A bladder diverticulum is a pathological formation in the form of a niche on the bladder wall that protrudes into the pelvic area. According to medical observations, it occurs equally often in both men and women. So, let’s understand the concept of what a bladder diverticulum is. There are two forms, primary and secondary.
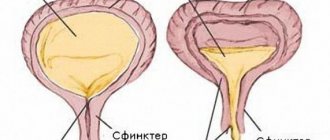
Primary ones, they are true, are formed during an abnormal development of the embryo and a violation of the formation of the urinary system. In this case, the diverticulum affects all the walls of the bladder. A neck extends from the walls and goes into a special pouch. Some people live for many years before discovering this disease. Due to the fact that a true diverticulum has a neck, it is more difficult for urine to exit through it from the niche into the lumen of the bladder.
Secondary, or false, occurs against the background of other diseases. When the walls are damaged, they become thinner, and a protrusion forms under the influence of increased intravesical pressure. In this case, hypertrophy of the bladder occurs, weakness of the muscle layer and as a result of all this - urinary retention and its chronic stagnation. If multiple protrusions are formed, then we are talking about diverticulosis.
The most common causes of pseudodiverticulum include:
- Inflammatory and infectious diseases.
- Prostate adenoma.
- Malignant neoplasms of the pelvic cavity.
- Muscle stretching.
- Injuries.
- Increased intravesical pressure.
Diverticulum as an independent nosological unit is not dangerous. The big problem is diseases that occur against the background of illness. Due to chronic stagnation of urine, a secondary bacterial infection occurs, which leads to the development of cystitis, pyelonephritis, and urethritis.
It is known that a niche appears on a thinned wall, therefore, if the bladder is injured, there is a risk of rupture of the walls and the development of peritonitis. This pathology requires urgent hospitalization and urgent surgery.
Bladder diverticulum - what is it?
Diverticulum is the formation of one or more additional cavities in an organ due to protrusion of its wall. The disease can be either congenital or acquired.
The pathology is especially common in men, which is associated with an enlarged prostate gland - a predisposing factor in the development of diverticulosis. The sizes of diverticula are quite varied - from small cavities to large sac-like formations.
Types of diverticula
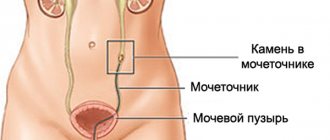
Diverticula predominantly form at the junction of the ureters. The formations communicate with the organ cavity through the neck of the diverticulum. Diverticula can be isolated formations. But several protrusions of the organ wall – diverticulosis – also occur.
Based on the structure of the walls of the formation, they are distinguished:
- True diverticulum . Its wall has a similar structure to the bladder and contains a mucous membrane, a muscular layer and a connective tissue membrane. It is more common in congenital forms of the disease.
- Bladder pseudodiverticula . They are formed by a mucous membrane that penetrates through all layers (muscle and connective tissue) of the organ. Thus, the wall of the formation is represented only by the mucous membrane. It is observed mainly in the acquired form of the pathology.
Use of conservative treatment methods
Protrusion of the bladder wall is irreversible.
Conservative methods do not have the expected positive effect in eliminating the problem. Preference is given to surgical interventions. Drug therapy provides symptomatic therapy and assistance in the rehabilitation of the patient.
The most common medications used in drug treatment during the rehabilitation period can be divided into several groups.
Such drugs include:
- antispasmodics;
- antibacterial agents;
- hemostatics;
- diuretics.
Antispasmodic drugs are used to relieve pain during acute manifestations of the disease. This group includes: Spazmalgon, No-shpa, Baralgin. In addition to antispasmodics, nonsteroidal anti-inflammatory drugs also have a broad analgesic effect. Their use is more typical in the postoperative period.
Antibacterial therapy is used during infection or for its prevention. The most commonly used are Ceftriaxone, Zovirax, Tuliside, and Levofloxacin.
Hemostatic drugs are needed to stop bleeding that develops against the background of complications of the disease, namely when the wall ruptures, ulcers form, and diverticulum ruptures. The most powerful therapeutic effect is found in: Aminocaproic acid, Vicasol, Vitamin K.
Diuretics are most often used when urinary retention develops. They help speed up the excretion of urine and prevent its stagnation.
Reasons for the development of pathology
Congenital forms of the disease are a malformation of an organ associated with a violation of its formation during embryogenesis.
The main cause of the acquired pathology is increased urine pressure in the urinary system. As a result of constant exposure to the wall of the organ, compensatory hypertrophy of its muscle layer occurs, but if the factor causing the increase in pressure is not eliminated, then atrophic processes develop. This leads to excessive stretching and disruption of the structure of the muscle layer, which is manifested by protrusion of the mucous membrane through the muscle fibers and connective tissue capsule.
The cause of impaired urine outflow is an obstruction localized in the urethra, the so-called infravesicular obstruction. The patient is forced to constantly strain when urinating, which leads to overstretching of the walls of the organ. This is observed in the following conditions:
- age-related hyperplasia (enlargement) of the prostate gland;
- benign and malignant prostate tumors;
- narrowing of the urethra;
- cicatricial change or sclerotic processes in the neck of the organ.
Reasons for education
Diseases that contribute to the development of the acquired form of diverticulum:
- Urethral stricture (the canal is narrowed and causes difficulty urinating).
- Prostate adenoma (proliferation of prostate tissue with the formation of nodes, tumors and pressure on the urethra).
- Sclerosis of the bladder neck (overgrowth of connective tissue causes narrowing of the lumen).
- Tumor of the urinary organs (creates high blood pressure).
- Various pathologies that complicate the natural physiological outflow of urine.
Diseases that provoke the development of acquired diverticula mostly affect the male gender due to their anatomy. This explains the fact why pathology is diagnosed in men more often than in the female population.
Causes of congenital disorder:
- Complications after infectious diseases during pregnancy.
- Bad habits of the mother before or during pregnancy.
- Cell mutation as a result of chemical or radiation exposure.
- Environmental factors.
Symptoms of the disease
The pathology can occur for a long time without disturbing the patient. Specific symptoms appear when the size of the protrusion increases, which leads to disruption and difficulty urinating.
The main symptoms suggesting the presence of a diverticulum:
Urinary disorders . Urine excretion occurs in 2 doses. First, the bladder is emptied, then the formation cavity. The duration of urination also increases. Patients complain of a feeling of incomplete emptying of the bladder.
Stagnation of urine . The protrusion cavity is a source of secondary infection of the urinary system. Regular stagnation of urine in a diverticulum leads to the development of chronic inflammation of the bladder (cystitis), as well as the formation itself (diverticulitis). Infections respond poorly to antibiotic therapy and are characterized by frequent exacerbations. Patients complain of cloudy urine, the appearance of blood and pus in it.
Kidney damage . If the protrusion of the wall is localized in the immediate vicinity of the confluence of the ureters, then a reverse flow of urine into the renal pelvis is formed - vesicoureteral reflux. This leads to increased pressure in the renal pelvicaliceal system, which leads to the development of pyelitis and pyelonephritis. In severe cases, diverticulosis is complicated by hydronephrosis and renal failure.
Clinical picture
The main symptoms of bladder diverticulum are associated with stagnation of urine. On a small scale, the disease can be asymptomatic. The pathology manifests itself with dysuric manifestations: miction is disrupted, fluid is released in several stages, and the flow is intermittent. As a rule, urine is first evacuated from the cystic cavity, and then from the diverticula. This lengthens the total time of urination; the patient has to push additionally for complete emptying.
In addition, the following symptoms may be observed:
- inflammatory processes;
- discharge of pus along with urine;
- unpleasant odor of urine;
- greenish tint to urine;
- pathological discharge from the urethra;
- hematuria.
True bladder diverticulum is often accompanied by inflammatory pathologies and, if not treated promptly, can develop into pyelonephritis, hydronephrosis or renal failure. The condition requires mandatory medical care; self-treatment, recipes from the Internet and from friends will not help in this case, but will only aggravate the situation.
Detection of bladder diverticulum on ultrasound
Ultrasound diagnostics is the main and most accessible way to identify diverticula, both true and pseudodiverticulosis. The examination is carried out through the anterior abdominal wall. The sensor of the device is located above the pubis. With transrectal access, the scanner is located in the rectum.
A bladder ultrasound takes 10 to 15 minutes. During the study, the patient may feel some discomfort when the sensor presses on a full bladder, since this involves holding back from urinating.
The pathological formation is visualized as a formation surrounded by a capsule with echo-negative content. Using ultrasound, the shape and size of the protrusion, the structure of its walls are determined, the diameter of the neck of the formation and the connection with the bladder are assessed. In addition, the presence of stones, tumors, cysts and kidney damage is determined.
An important condition for successful visualization of the bladder using ultrasound is proper preparation for the examination. The purpose of the preliminary procedures is to fill the cavity of the bladder, since only when the organ is in a straightened state can the doctor clearly see the features of its structure.
To do this, you should refrain from going to the toilet 4–6 hours before the test; you can also drink 1 liter of water about 2 hours before the test. If a transrectal examination is planned, a cleansing enema is necessary.
The main factors leading to diverticula
- Congenital anomalies. an additional bubble is formed after dysembryogenetic anomalies and is manifested by a weak detrusor.
- Disruption of the physiological dynamics of the urinary system. Which leads to an obstruction of the free outflow of processed physiological fluids. Physio-pathological changes in the structure of the bladder are the result of increased pressure inside it, which leads to overstretching of the walls and divergence of muscle fibers.
- Pathologies leading to diverticula. Infravesical obstruction by prostate adenoma, urethral strictures, sclerosis of the urinary canal, nephrolithiasis, polyps, malignant neoplasms.
- Mechanical injuries. Weakening of the bladder walls after blows, contusions or compressions.
- Poisoning of the body with poisons.
- Urological postoperative complications.
Can the intestines put pressure on the bladder? Of course, with pathologies such as rectal cancer, compression of the urinary organ from the intestine is observed. The larger the tumor, the more pronounced the symptom complex appears in the form of heaviness in the pelvic area and a constant feeling of a full bladder, as well as a frequent urge to urinate.
Treatment of this pathology is carried out in the oncology department. If stage 1 cancer is removed and the large intestine is removed, feces pass through the stoma. The bladder begins to function normally.
Disease Prevention
To prevent the appearance of congenital pathology, it is necessary to create satisfactory conditions for pregnancy: a pregnant woman should definitely get rid of bad habits, lead an active lifestyle, avoid injuries and promptly treat any inflammatory diseases that have arisen.
The formation of an acquired diverticulum is prevented by timely treatment of diseases that contribute to its occurrence.
Cervical sclerosis, prostate hyperplasia and some other diseases can pose a danger. Regular examination by a urologist will also prevent the appearance and development of bladder deformation.
How to recognize MP diverticulum
It is difficult to determine pathology at the beginning of development. It is possible to identify the problem at an early stage only through a preventive examination. Often the disease is discovered when a patient complains of recurring pyelonephritis or cystitis.
To make an accurate diagnosis, specialists carry out a number of diagnostic procedures.
The first diagnostic method is echography (ultrasound) of the MP. Ultrasound evaluates the location, shape and size of the diverticulum, and reveals the presence of stones and tumors.
In addition to ultrasound, there are diagnostic methods such as cystography and cystoscopy. During cystography, X-rays of the bladder filled with a special contrast liquid are taken.
Inspection of the inner surface of the bladder is called cystoscopy. This procedure identifies the neck connecting the main cavity with the formation and determines the type of pathology.
Diagnosis of the disease includes the need to conduct a complex of urodynamic studies. These studies help evaluate urinary function in full.
In men, diverticulum is accompanied by the following symptoms: discomfort with little need, tingling, aching pain in the lower abdomen, cloudy discharge, redness of the head of the penis.
In women, pathological protrusion of the bladder may be accompanied by cystitis. External signs of the disease: discharge similar to thrush, small sores on the labia and itching in the genital area.
In children, congenital MP deformity is more often detected. The abnormal formation is located according to the same principle as in adults; it is often localized near the junction of the ureter with the bladder.
Pain caused by abnormal protrusion of the bladder in a child is either weak or moderate. Most often the pain is aching in nature. As the disease progresses, the frequency of pain changes: at first it is periodic, later the discomfort and pain become constant. Localized pain in the lower abdomen becomes worse when urinating. Small children notify about this by crying for a long time before emptying the bladder or immediately after the end.
Diagnostics
Bladder diverticula may be suspected when a patient experiences symptoms such as recurrent urinary tract infections, chronic pelvic pain syndrome with signs of inflammation, abdominal fullness, incomplete emptying of the bladder, or bowel problems in general that suggest obstruction and stasis. urine. However, patients may not have specific symptoms, and diverticula may be discovered during testing for other problems. An excellent means of detecting bladder diverticula is the cystogram, which provides an x-ray image of the bladder using cystography by injecting a contrast dye.
A diverticulum can also be detected using cystoscopy, which is especially useful for checking for tumors in the diverticulum by inserting a flexible cystoscope through the urethra and into the bladder. Bladder function and the presence of bladder neck obstruction can be assessed using a bladder pressure test (urodynamic test). Finally, in some cases, it may be necessary to check the impact of obstruction on the kidneys by performing an ultrasound examination of the kidneys.
Classification
Smoking and other bad habits of a pregnant woman can provoke the formation of congenital bladder diverticulum.
Based on their origin, bladder diverticula are divided into primary (arising on their own) and secondary (developing as a consequence of some other urological pathology). Primary ones are also called congenital - with them a person is born, and secondary ones - acquired, which develop during his life.
Depending on the structure of the wall, true and false diverticula are distinguished:
- the wall of a true diverticulum consists of the same layers as the bladder itself - mucous, submucosal, muscular and the adventitia covering it; as a rule, primary, congenital diverticula are true;
- a false diverticulum is formed only by the mucous membrane, which protrudes through weakened fibers of the muscular wall of the bladder; Secondary, acquired diverticula usually have this structure.
Some patients have only one protrusion of the bladder wall, while others have several. Multiple diverticula are considered diverticulosis.
Types of disease
Pathology has 2 forms, which have their own characteristics.
Thus, it can be noted.
True diverticulum
This form of pathology is congenital and progresses simultaneously with the development of organs. As a result, the layers of the bladder septum are the same.
With such parallel development, the shape of the organs is disrupted. Pathology appears on the back wall and takes the shape of a bag.
Acquired pathology
The second form is a false and inherently acquired pathology. Occurs against a background of increased pressure inside the bladder and
with thinning and exhaustion of the walls.
In this case, during formation, the diverticulum protrudes through the muscle fibers and takes on the appearance of a hernia. It is connected to the bladder using a neck.
Often, when the disease occurs, the muscles hypertrophy, and as a result, problems with emptying appear. Taking into account that the outflow of urine is difficult, the organ begins to enlarge. At the same time, its shell becomes thinner, and the muscle fibers lose their former appearance and become loose.
As a result, deformation occurs and new pathologies arise.
False diverticula can have absolutely any size, and are located absolutely anywhere in the lining of the bladder. They can also be single or multiple.
Treatment tactics and prognosis
Treatment of a protruding small sac, which does not cause dynamic disorders, is carried out on an inpatient or outpatient basis; it is not operated on. The patient must be constantly monitored by a doctor, undergoing tests and performing ultrasounds.
All other types of large diverticula that impair the outflow of urine are subject to only surgical treatment, that is, endoscopic or open.
Endoscopic surgery is done in cases of true diverticulum, excising the canal and making adequate communication between the cavity and the bladder. Open surgery or diverticulectomy consists of complete removal of the communicating formation by incision of the suprapubic region and the anterior wall of the bladder. The wound is sutured in layers and drained. After the operation, the patient is rehabilitated in the shortest possible time, starting work and a full-fledged lifestyle.