Among urological diseases, anomalies of the bladder occupy a special place. These are congenital pathologies that develop during the formation of a child in the womb. The main causes of anomalies are considered to be a hereditary factor, poor ecology, infectious diseases suffered by the mother during pregnancy, the mother's use of alcohol and drugs, and occupational hazards. As a result, various defects develop. Some of them are incompatible with life.
Agenesis: an anomaly of congenital absence of a bladder in a newborn
Bladder defects are both congenital and acquired.
Agenesis refers to a deformity in which one or another organ is missing. Bladder agenesis is a rare pathology. According to statistics, out of 19,046 infants who were stillborn or died in early childhood, 7 had this anomaly discovered at autopsy. Pathology is formed due to incomplete development of the cloaca or allanthops. Accompanied by atresia of the rectum and vagina, absence of the urethra. This vice is incompatible with life. However, with further developments in medicine in the future, agenesis will be treated with bladder transplantation. Currently, the problem is solved by removing the ureters into the intestines.
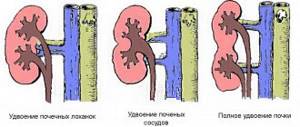
Bladder duplication
Duplication of the bladder is characterized by the division of the bladder into 2 parts by a septum, which can run in two planes (lengthwise or transversely). Pathology happens:
- Full. The urethra is divided into 2 compartments, independent of each other. Each of them has its own ureter, neck and separate urethra.
- Incomplete doubling. Both compartments open into a single cervix and urethra.
There is incomplete division of the organ. This phenomenon is called a two-chamber bladder. During ultrasound diagnostics, this defect can be mistaken for an extensive diverticulum. The main symptoms of the anomaly are urinary incontinence and chronic inflammatory processes, for example, cystitis, pyelonephritis. As part of the treatment, the septum is excised through surgery.
Diverticulum
A bulge in the wall of the bladder is called a diverticulum. Like any pathology, the disease disrupts the normal functioning of the bladder and provokes complications. The anomaly does not have pronounced symptoms, which is why it is difficult to diagnose. This is the danger of the disease: complications develop before the pathology is determined. Urine stagnates in the diverticulum, pathogenic microflora is formed, and the mucous membrane of the bladder is affected. All this contributes to the development of inflammatory processes. The pathology is eliminated surgically.
Any deviation from the norm in the structure of the bladder requires immediate treatment. Otherwise, serious complications develop with a poor prognosis.
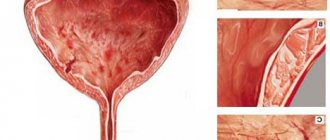
Diagnosis of benign and malignant bladder tumors
Through diagnostic measures that are carried out when this disease is suspected, the following points should be addressed:
- The fact of the presence of a tumor.
- Stage of development of the neoplasm.
- The structure of the mucous membrane in the area of pathological protrusion.
- Presence/absence of metastasis to neighboring organs.
In this regard, the examination should be comprehensive and cover not only the genitourinary system, but also other organs.
Various methods can be used to detect a bladder tumor:
- Bimanual palpation . It is performed under anesthesia with an empty bladder. Makes it possible to determine the presence of dense formations in the bladder area. If the pathological process involves the pelvic organs/bones, uterus, vagina/prostate gland, this diagnostic method will also be indicative.
- Cytological testing of urine. The sample taken is examined for the presence of atypical cells. Although a negative result in this analysis does not guarantee the absence of cancer.
- Cystoscopy. An instrumental diagnostic method, during which a special device is inserted directly into the bladder. This organ is carefully examined; if an atypical area is found, a small piece is plucked off from it and sent to the laboratory for histological examination. The type of research under consideration is the most reliable in diagnosing this cancer.
- Excretory urography, cystography. They are a type of x-ray examination methods. With their help, you can determine the degree of deformation of the walls of the bladder, the location of its neck, and thereby determine the nature of tumor growth.
- Ultrasound of the bladder, computed tomography, MRI. They make it possible to visualize a pathological neoplasm, evaluate its parameters and prevalence.
- Excretory urography. Helps determine the performance of the kidneys, examine their structure, as well as the structure of the ureters and bladder.
- Bone scintigraphy, lymphography , and some other methods are used to diagnose metastases.
Rate
—
Congenital detrusor hypertrophy
Detrusor hypertrophy is an enlargement of the bladder muscle that pushes urine out and allows urination to occur. Congenital pathology, in addition to the detrusor anomaly, does not have accompanying anomalies; the state of urodynamics, urethra, etc. is normal. To avoid subsequent complications, it is necessary to remove the underdeveloped muscle and replace it with a loop of intestine.
If left untreated, the child has difficulty urinating and the bladder does not empty completely. The newborn becomes restless and strains. Over time, a large volume of urine accumulates in the bladder because the detrusor is unable to cope with the load. As a result, the bladder stretches, atrophy occurs, followed by atony of the organ.
exstrophy
Exstrophy is underdevelopment of the genitourinary system. It is considered the most severe type of anomaly in urology. The disease is characterized by the absence of the abdominal wall and bladder wall. Determined immediately after the birth of the child. Due to the difference in pressure, the bladder turns outward, and urine flows out through the abdomen. There are often concomitant pathologies: epispadias (underdevelopment, dissection of the urethra), splitting of the pubic bone. Among 30-50 thousand newborns, only one is diagnosed with this pathology; girls are 2 times more likely than boys. If a woman’s first child was born with this anomaly, then the likelihood of having this problem in her second child increases (1:100).
Neoplasms in the urethral area
Urethral polyp. This is a type in which the connective tissue grows in large quantities and causes severe focal inflammation. Among the male half, the polyp prefers places closer to the prostatic area. In women, this is most often the urinary tract.
Urethral carbuncle. Girls and women are most susceptible to this disease. Most often, part of the mucous membrane falls out of the urethra, which leads to inflammation and the possibility of catching an infection, and blood circulation throughout the entire area is also disrupted.
Urethral papilloma is a common formation with many villi that can be located along the entire length of the urethra in both men and women.
If the tumor is benign and small, a person can live 80 years and not know that he has something similar. Since such a tumor does not show itself in any way and does not manifest itself in any way. As the formation grows, there may be discomfort, burning, and bleeding. In cases where the tumor appears externally, doctors perform simple resection and electrocoagulation. If the location is the inner surface, then doctors resort to urethroscopes and the TUR method.
Bladder neck contracture
This disease is called bladder neck stenosis or Marion's disease. A rare defect of the bladder, described back in 1935. A distinctive feature of the pathology is a violation of the development of connective tissue, as a result of which an abnormally large amount of fibrous tissue is formed under the mucous membrane and in the muscle layer of the bladder neck. There are cases where the disease affects a large area of an organ. Boys are more likely to suffer from this disease.
Main symptoms
The manifestation of the disease depends on the degree of damage and its duration:
- With mild contracture, the child experiences difficulty urinating or the disease does not manifest itself until concomitant diseases and complications arise.
- Severe degree of pathology and/or duration of the disease is characterized by difficulty urinating, residual urine remains in the bladder.
- Absence/delay of urination.
- Frequent urinary tract infections occur.
- If the pathology is complicated by hydronephrosis and this phenomenon is diagnosed in a child before birth, a difficult birth is predicted.
- If treatment is not started, renal failure develops.
Diagnosis of congenital diseases
To make a correct diagnosis, an instrumental examination is carried out:
- Cystoscopy identifies a trabecular bladder. The phenomenon occurs with difficulty urinating and is an abnormal development of some muscle fibers of the urinary tract, between which depressions are formed - false diverticula.
- Retrograde pyelography reveals tortuosity and dilation of the ureters, vesicoureteral reflux.
- The diagnosis is confirmed by uroflowmetry, demonstrating the condition of the urinary cervix.
Treatment methods
Treatment of the anomaly is possible only through surgery. The operation is carried out endoscopically, i.e. through the urethra. The affected bladder neck is dissected and plastic surgery is performed. Along with this, therapy for concomitant inflammatory processes that arise as a complication and elimination of intoxication are required.
Prevention
To prevent the development of cystitis of the bladder neck, you need to strengthen the body's defenses and monitor personal hygiene. Necessary:
- avoid prolonged exposure to the cold;
- treat infections, especially sexually transmitted ones;
- use barrier contraceptives;
- maintain genital hygiene;
- Healthy food;
- drink enough water;
- do not wear tight or constrictive clothing;
- give preference to linen made from natural fabrics;
- move more;
- undergo routine examinations with a urologist or gynecologist.
Diseases of the bladder neck bring discomfort to the patient, interfere with a full life and can cause the development of severe pathologies of the urinary tract. Treatment is usually carried out on an outpatient basis.
With a quick diagnosis and proper treatment, the prognosis for recovery is positive. In advanced situations, surgical intervention may be required. It is best to prevent the development of cystitis by observing good hygiene and increasing immunity.
Urachal anomalies
The urachus is a tube connecting the fetal bladder to the umbilical cord. Due to this, fetal urine is excreted into the amniotic fluid. In the fifth month of pregnancy, the process of forming a full-fledged urinary system of the child begins, and this duct becomes overgrown. Sometimes this does not happen and the child is born with a urachus anomaly. After the umbilical cord falls off, a fistula is discovered, from which urine oozes. Usually the pathology is diagnosed in children under 5 years of age, but there are cases when bladder pathology manifests itself in older people. It is less common in women. There are 2 types of this anomaly.
Complete non-union
When the urachus is fully opened, pathological changes in the structure of the child are noticeable immediately after birth, because urine is released from the navel. If the diameter of the duct is small, urine is mainly excreted through the urethra. If you press down on the baby's tummy, intense urine leaks from the navel. The disease is diagnosed through cystoscopy and cystography. A probe inserted into the bladder reveals the opening of an unclosed urachus. Another method is to inject a colored liquid into the bladder using a catheter. Its discharge from the navel confirms the type and characteristics of the defect.
Partial cleft
Depending on the location of the cleft, the defect is divided into 3 types:
- Umbilical fistula. Urachus does not overgrow from above. The problem is discovered after the child's umbilical cord falls off or at any other age. If the pathology manifests itself in an adult, it can be argued that the urachus is infected, which led to suppuration and its breakthrough through the navel.
- Cyst formation. Pathology of the middle duct. It is manifested by the presence of a neoplasm, which can be independent or related to the bladder or navel.
- Diverticulum. Non-union of the lower section. Appears after an infectious lesion. The patient complains of abdominal pain, painful urination with frequent urge. Through cystoscopy, a passage into an open duct (diverticulum) is detected in the upper part of the urinary tract. Suppuration is observed in the diverticulum, pus enters the bladder.
Treatment of bladder abnormalities is carried out only by surgery.
Treatment methods
When fully opened, the urachus is cut out. The operation is performed no later than a few months after the birth of the child to prevent infection. Basically, the procedure is performed a few days after birth. If there is partial opening in the first year of the baby's life, surgical intervention is not performed. There are cases of spontaneous closure of the fistula during the first months of the baby’s life.
If surgery is postponed, the child's mother carries out conservative therapy. At the hospital, the woman is given instructions. The goal of therapy is to prevent infection. The navel is systematically treated with antiseptic solutions. The baby is given baths with a solution of potassium permanganate. Surgery is performed when the child is strong enough and turns one year old. Depending on the situation, the navel and urachus are removed, but more often only the fistula itself.
Causes and triggers of the disease
The reasons for the development of the disease differ depending on the gender of the patient.
Women
Girls and young women (from 8 to 40 years old) are most susceptible to cystitis. Cervical cystitis in women is most often caused by poor hygiene and weakened immunity:
- Acute cervical cystitis can begin after hypothermia, especially in the area where the organs of the urinary and reproductive systems are located. This is caused by sitting on a cold surface for a long time and wearing too light clothes.
- The disease develops due to lack of hygiene (rarely taking a shower or bath, wearing dirty underwear, unprotected sexual intercourse). Bacteria from the genitals or intestines enter the urethra and then into the bladder.
- Risk factors include sexually transmitted infections (gonorrhea, chlamydia, candidiasis, trichomoniasis, herpes).
- Cervical cystitis can appear against the background of weak immunity due to any infectious processes in the body: colds, flu, caries.
- Lack of physical activity contributes to inflammation.
- Irritation of the organ neck is caused by the abuse of strong drinks and caffeine, bad eating habits (insufficient consumption of fiber, slow carbohydrates, excess sugar, flour, spicy and salty foods).
Men
In men, inflammation most often results from a narrowing of the cervix due to hardening of the bladder tissue. Scars form on the cervix, and the hole for the outflow of urine narrows, which interferes with emptying.
A person can be born with sclerosis of organ tissue, but more often scarring of the cervical walls appears in old age after prostate surgery. Long-term or repeated inflammatory processes in the prostate can also lead to cervical sclerosis.
Symptoms
The onset of the disease is usually acute: the main symptom of cervical cystitis is a frequent urge to urinate (every 15–20 minutes).
Symptoms of the disease:
- pain, burning in the lower abdomen, especially during bowel movements;
- pain during sexual intercourse;
- elevated temperature;
- nausea, vomiting;
- deterioration of general condition;
- urinary incontinence;
- a small amount of fluid released when visiting the toilet (often in the form of a thin stream or drops);
- bloody or purulent impurities in the urine, cloudiness, repulsive odor.
Sometimes cervical cystitis is asymptomatic or the symptoms are mild.
In this case, it can be recognized by urine, blood tests, and the results of instrumental examinations.
Sclerosis of the bladder neck in men has the following symptoms:
- At the first stage (lasts about 3 years), the patient complains of frequent visits to the toilet, especially at night. If the patient consults a urologist in time, the disease can be completely cured.
- In the second stage, due to scars on the bladder and a narrowed passage for fluid exit, unremoved urine begins to accumulate in the body of the organ. When you finish urinating, blood often appears. At this stage, incontinence or problems with urine flow develop. Pathogenic microorganisms multiply in the accumulated urine, causing inflammation to spread to the entire bladder and then to the kidneys. The result may be pyelonephritis or other serious kidney dysfunction.
- At the third stage, the patient loses the ability to urinate independently. It is necessary to install a stoma (an artificial opening for draining urine through a catheter) in the anterior wall of the abdomen.