The kidneys have a major impact on the menstrual cycle, and unhealthy kidneys can cause irregular or delayed menstrual cycles.
What is the connection between kidneys and menstruation?
Kidneys are an organ that is included in the list of important components for humans. They ensure the vital functions of the whole organism, and especially the reproductive system. Paired organ:
- Cleanses the blood of toxins.
- Converts one substance to another.
- Removes urine.
- Controls acid-base and water-electrolyte balance, blood composition.
- Participates in the production of various hormones - renin, erythropoietin, prostaglandins. They are responsible for water metabolism, blood circulation, and normalization of blood pressure.
Since the kidneys are involved in hormonal synthesis, and the functioning of the reproductive system depends on the level of hormones, we can say that any changes affect the menstrual cycle. It is worth noting that during menstruation, a woman loses blood and the body is more susceptible to infection.
Kidney pain is possible before menstruation
Sometimes the patient experiences pain in the kidney area before menstruation. Often along with this there is pain in the lower abdomen. This is normal, symptoms go away after 1-2 days.
If the pain is tolerable and does not cause other inconveniences, there is no reason to worry, thus the body is preparing for endometrial detachment.
Can a cold cause a delay in menstruation?
Any cold causes stress in the body. A stressful state weakens the immune system, resulting in disruption of the menstrual cycle.
In many situations, the failure goes away on its own and no additional therapy is required.
But for some women, the delay in menstruation due to a cold can be too long and requires special correction, which must be prescribed by a qualified specialist.
The relationship between the menstrual cycle and colds
A delay in menstruation due to colds has occurred at least once in almost every woman. The monthly cyclical process of the reproductive system depends on hormonal activity.
A stressful situation and weakened immunity affect the production of hormones. The hypothalamus and pituitary gland produce special substances that affect the formation and development of the follicle, as well as the production of progesterone, the ovulation mechanism. When there are not enough hormones, menstruation is delayed compared to the previous month.
- Flu and colds are among the stressful situations that the female body experiences during illness;
- Toxic waste products of viruses affect all organs, including the genitals, as well as the entire immune system;
- As a result, a woman does not have periods or experiences unusual duration, atypical volume and intensity of discharge.
In addition to the negative impact of viruses, the medications that a woman takes to treat a cold affect the monthly cycle. Medicines cause a delay in menstruation because they weaken the immune system and lead to hormonal imbalance. Monthly natural processes are disrupted.
What is considered normal?
Many women do not know what to do if their monthly cycle is disrupted due to a cold, and they begin to panic. First of all, you need to make sure there is no pregnancy. If the test is negative, the delay in menstruation is most likely due to the consequences of acute respiratory infections or influenza.
How many days can a cold last? Cycle disturbances during a cold or immediately after it are allowed, but not longer than a week.
When should you worry?
When you miss your period for more than 7 days, you need to find time to visit the gynecologist's office. After passing all the tests, the doctor will determine the presence or absence of inflammation.
It would be a good idea to check the condition of the uterus, tubes, and ovaries using an ultrasound diagnostic machine.
Such an examination will help identify pathology in the pelvis, which may have been caused by colds and flu.
What to do to restore the cycle?
Typically, gynecologists recommend the following therapy to restore the cycle:
- Medicines for general strengthening of the body;
- Vitamin complexes with mineral supplements;
- For serious disorders, hormonal drugs are prescribed.
If premenstrual syndrome (PMS) occurs, doctors recommend mild sedatives or corrective non-hormonal therapy to normalize the cycle.
We need comfortable conditions for recovery and the speedy restoration of menstruation. This requires a balanced diet, plenty of fluids, good sleep, and fresh air. You should refrain from physical activity, but quiet exercise is necessary to normalize blood circulation in the pelvic organs.
Delay in colds of the urinary system
When a woman has a cold, the organs of the excretory system often become inflamed: the kidneys and bladder. Can pathology cause delayed menstruation? The answer is yes. In this case, the delay occurs in various forms, depending on the severity of inflammation, the state of the immune system, and concomitant diseases.
Cystitis
A delay in a cold in the bladder is associated with an inflammatory process, since the infection spreads to the genitals, including, which leads to a cycle failure.
Chronic cystitis is difficult to treat; it provokes infection into the ovaries, which disrupts the functioning of female sex hormones and disrupts the menstrual cycle. The production of estrogen decreases, hormone deficiency thins the inner lining of the bladder, the mucous membrane is more easily injured, and any hypothermia provokes the proliferation of bacteria.
An advanced infection causes pain and burning when urinating. Lack of treatment has a negative impact on a woman’s health; the infection can move through the ureters and affect the kidneys.
Nephritis
Any ailments that appear during a kidney cold do not go unnoticed in the female cycle. It is quite possible that kidney inflammation will cause a prolonged absence of menstruation, since the cycle reacts to almost all problems in the body.
The anatomical features of a woman contribute to the fact that the infection easily penetrates from the urinary system to the reproductive system. The woman must undergo a full examination. Therapy is prescribed according to the diagnosis. Choosing treatment on your own is unacceptable due to the seriousness of the problem.
Delay in genital colds
Monthly bleeding on time indicates the normal functioning of the female body. When the genitals are exposed to disease and inflammation, the physiological process is disrupted.
Additionally, girls may feel severe pain in the lower abdomen, extending to the lower back, and unpleasant discharge.
When inflammation of the female genital area is diagnosed, menstruation is disrupted.
Inflammation in the pipes
If you have a cold in the appendages, you must find out the reason for the delay in menstruation. The disorder sometimes lasts 7 days or more. In this case, you should pay attention to additional symptoms:
- The appearance of purulent, bloody, mucous discharge;
- Pain in the abdomen above the pubis;
- High body temperature.
With temperature, the blood becomes thicker and its fluidity decreases, which also affects the menstrual cycle.
The causes of ovarian inflammation can be pathogenic or conditionally pathogenic bacteria, as well as factors that are quite harmless at first glance, such as intrauterine devices, hypothermia, the use of sanitary tampons and panty liners.
Due to frequent colds, the fallopian tubes become denser, longer, pus begins to be released from them, and adhesions develop. Delayed treatment leads to the infection spreading further.
What diseases can be caused by pain in the kidney?
Discomfort and pain do not always occur in women. There are people who do without these symptoms during menstruation. The table lists the causes of pain in the kidneys.
| Cause of pain | Description |
| Uterine diseases | Painful sensations in the kidneys appear due to the fact that the organ is located next to the uterus |
| Inflammation of the lumbar region | Diseases of the spine, joints or injuries are the cause of pain in the kidneys |
| Disturbance of the uterus | The uterus can affect the nerves in the lower back. The symptom appears during menstruation and is perceived as pain in the kidneys |
| Inflammations of the genitourinary system or sexually transmitted diseases | May cause pain in the kidney area |
| Edema of the uterus | Appears during menstruation. The uterus increases in size and comes into contact with nearby organs. There is discomfort and slight pain during menstruation |
| Large amounts of estrogen | May increase menstruation and place additional stress on the kidneys |
| Pyelonephritis or urolithiasis in an acute state | Diseases can become acute during menstruation due to a weakened immune system or increased contractions of the uterus. During menstruation, the uterus begins to move and puts pressure on nearby organs, causing pain in the kidneys |
Menstruation with pyelonephritis
- watch advertisements
PYELONEPHRITIS is a nonspecific infectious disease of the kidneys that affects the renal parenchyma, mainly interstitial tissue, pelvis and calyces. Pyelonephritis can be unilateral or bilateral, primary and secondary, acute (serous or purulent), chronic or recurrent.Etiology, pathogenesis. Most often, pyelonephritis is caused by intestinal Escherichia, Enterococcus, Proteus, staphylococci, streptococci. In one third of patients with acute pyelonephritis and in 2/3 of patients with chronic pyelonephritis, the microflora is mixed.
During treatment, the microflora and its sensitivity to antibiotics change, which requires repeated urine cultures to determine adequate urinary antiseptics. It is necessary to remember the role of protoplasts and L-forms of bacteria in the occurrence of relapses of pyelonephritis. If the infection in the kidney is supported by protoplasts, then urine culture will not detect them.
The development of pyelonephritis largely depends on the general condition of the macroorganism and a decrease in its immunobiological reactivity. The infection penetrates the kidney, pelvis and its calyces by hematogenous or lymphogenous route, from the lower urinary tract along the wall of the ureter, along its lumen - in the presence of retrograde reflux.
Urinary stasis and disturbances of venous and lymphatic outflow from the kidney are important in the development of pyelonephritis. Pyelonephritis is often preceded by latent interstitial nephritis.
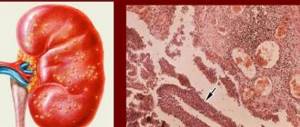
Acute pyelonephritis can be interstitial, serous or purulent. Apostematous nephritis and renal carbuncle are possible subsequent stages of acute purulent pyelonephritis.
Symptoms, course. The disease begins acutely, high temperatures (up to 40 grams) appear.
C) fever, chills, drenching sweat, pain in the lumbar region; on the side of the affected kidney - tension in the anterior abdominal wall, sharp pain in the costovertebral angle; general malaise, thirst, dysuria or pollakiuria.
Additional headache, nausea, and vomiting indicate rapidly increasing intoxication. Neutrophilic leukocytosis, aneosinophilia, pyuria with moderate proteinuria and hematuria are noted.
Sometimes, as the condition of patients worsens, leukocytosis gives way to leukopenia, which is a poor prognostic sign. Pasternatsky's symptom is usually positive. With bilateral acute pyelonephritis, signs of renal failure often appear. Acute pyelonephritis can be complicated by paranephritis and necrosis of the renal papillae.
Diagnosis. An important role in diagnosis is played by indications in the anamnesis of a recent acute purulent process or the presence of chronic diseases (subacute septic endocarditis, gynecological diseases, etc.).
A combination of fever with dysuria, pain in the lumbar region, oliguria, pyuria, proteinuria, hematuria, bacteriuria with a high relative density of urine is typical.
It should be remembered that pathological elements in the urine can be observed in any acute purulent disease and that pyuria can be of extrarenal origin (prostate gland, lower urinary tract).
A survey X-ray reveals an increase in volume of one of the kidneys; excretory urography reveals a sharp limitation of the mobility of the affected kidney during breathing, the absence or later appearance of a shadow of the urinary tract on the affected side. Compression of the calyces and pelvis, amputation of one or more calyces indicate the presence of a carbuncle.
Treatment. In the acute period, table No. 7a is prescribed, consumption of up to 2-2.5 liters of liquid per day. Then the diet is expanded, increasing its protein and fat content.
With the development of metabolic acidosis, sodium bicarbonate is prescribed orally 3-5 g or intravenously 40-60 ml of a 3-5% solution. To improve local blood circulation and reduce pain, thermal procedures are prescribed (warming compresses, heating pads, diathermy of the lumbar region).
If the pain does not subside, then antispasmodics are used (platiphylline, papaverine, belladonna extract, etc.).
Antibacterial therapy is carried out with nalidixic acid (nevigramon, negram), the course of treatment of which should last at least 7 days (0.5-1 g 4 times a day), nitrofuran derivatives (furadonin 0.15 g 3-4 times a day, course of treatment is 5-8 days), nitroxoline (5-NOK), prescribed 0.1-0.2 g 4 times a day for 2-3 weeks.
The use of these drugs should be alternate. Nalidixic acid and nitrofuran derivatives should not be prescribed simultaneously, as this weakens the antibacterial effect.
During the first 5-6 days, especially with an infection resistant to antibiotics, hexamethylenetetramine (urotropine) can be used orally 0.5-1 g 3-4 times a day or intravenously 5-10 ml of a 40% solution daily.
Combined treatment with antibiotics and sulfonamides is very effective. The selection of antibiotics is carried out depending on the sensitivity of the microflora to them.
Prescribe drugs from the penicillin group (benzylpenicillin 1,000,000-2,000,000 units/day, oxacillin orally or intramuscularly 2-3 g/day, ampicillin orally up to 6-10 g/day, ampicillin sodium salt intramuscularly or intramuscularly). /at least 2-3 g/day, etc.) or together with streptomycin (0.25-0.5 g IM 2 times a day).
Tetracyclines are also used (tetracycline orally 0.2-0.3 g 4-6 times a day; its derivatives - morphocycline, metacycline, etc.
), macrolide antibiotics (oletetrin, tetraolean orally 0.25 g 4-6 times a day), aminoglycoside antibiotics (kanamycin intramuscularly 0.5 g 2-3 times a day, gentamicin intramuscularly 0, 4 mg/kg 2-3 times a day), cephalosporin antibiotics (cephaloridine, ceporin IM or IV 1.5-2 g per day), etc. You should remember the need to change antibiotics every 5-7 10 days and use them in moderate doses with caution in case of functional renal failure.
Of the sulfonamide drugs, urosulfan and etazol (1 g 6 times a day), long-acting sulfonamides (sulfapyridazine 1-2 g on the first day, then 1 g for 2 weeks; sulfamonomethoxine, sulfadimethoxine) are prescribed.
In most patients, changes in urine disappear within a few days, but antibiotic therapy must be continued (usually the course of treatment lasts 4 weeks).
If conservative therapy is ineffective (usually with apostematous nephritis and renal carbuncle), surgical intervention is indicated.
Chronic pyelonephritis can be a consequence of untreated acute pyelonephritis (more often) or primary chronic, that is, it can occur without acute phenomena from the onset of the disease. In most patients, chronic pyelonephritis occurs in childhood, especially in girls.
In 1/3 of patients, a routine examination fails to identify undoubted signs of pyelonephritis. Often, only periods of unexplained fever indicate an exacerbation of the disease.
In recent years, cases of combined disease with chronic glomerulonephritis and pyelonephritis have been increasingly reported.
Symptoms, course. Unilateral chronic pyelonephritis is characterized by dull, constant pain in the lumbar region on the side of the affected kidney. There are no dysuric phenomena in most patients. During an exacerbation, only 20% of patients have a fever. In urine sediment, the predominance of leukocytes over other formed elements of urine is determined. However, as
shrinkage of the pyelonephritic kidney, the severity of urinary syndrome decreases. The relative density of urine remains normal. For diagnosis, the detection of active leukocytes in the urine is essential.
In case of latent pyelonephritis, it is advisable to carry out a pyrogenal or prednisolone test (30 mg of prednisolone, dissolved in 10 ml of isotonic sodium chloride solution, administered intravenously over 5 minutes; after 1, 2, 3 hours, and 24 hours after this, urine is collected for examination) . The prednisolone test is positive if, after administration of prednisolone, more than 400,000 leukocytes are excreted in the urine within 1 hour, a significant portion of which are active. The detection of Sternheimer-Malbin cells in the urine only indicates the presence of an inflammatory process in the urinary system, but does not yet prove the existence of pyelonephritis.
One of the symptoms of the disease in most patients is bacteriuria. If the number of bacteria in 1 ml of urine exceeds 100,000, then it is necessary to determine their sensitivity to antibiotics and chemotherapy. Arterial hypertension is a common symptom of chronic pyelonephritis, especially bilateral.
The functional state of the kidneys is examined using chromocystoscopy, excretory urography, clearance methods (for example, determining the purification coefficient of endogenous creatine in each kidney separately), radionuclide methods (renography with hippuran labeled 1311, kidney scanning).
In chronic pyelonephritis, the concentrating ability of the kidneys is impaired early, while the nitrogen excretory function is preserved for many years.
Acidosis developing as a result of dysfunction of the tubules, as well as renal loss of calcium and phosphate, sometimes lead to secondary parathyroidism with renal osteodystrophy.
With infusion urography, a decrease in the concentrating ability of the kidneys, delayed release of a radiopaque substance, local spasms and deformations of the calyces and pelvis are initially determined. Subsequently, the spastic phase is replaced by atony, the calyces and pelvis dilate.
Then the edges of the cups take on a mushroom shape, and the cups themselves move closer together. Infusion urography is informative only in patients with blood urea levels below 1 g/l. In diagnostically unclear cases, a kidney biopsy is resorted to.
However, with focal lesions of the kidney during pyelonephritis, negative biopsy data do not exclude the current process, since it is possible that unaffected tissue may enter the biopsy sample.
With the development of renal failure, pale and dry skin, nausea and vomiting, and nosebleeds appear. Patients lose weight and anemia increases. Pathological elements disappear from urine. Complications of pyelonephritis: nephrolithiasis, pyonephrosis, necrosis of the renal papillae.
The diagnosis is often very difficult.
In the differential diagnosis of chronic glomerulonephritis, the nature of the urinary syndrome (the predominance of leukocyturia over hematuria, the presence of active leukocytes and Sternheimer-Malbin cells, significant bacteriuria in pyelonephritis), data from excretory urography, and radionuclide renography are important. Nephrotic syndrome indicates the presence of glomerulonephritis. In case of arterial hypertension, differential diagnosis should be made between pyelonephritis, hypertension and vasorenal hypertension. A characteristic anamnesis characteristic of pyelonephritis, urinary syndrome, the results of X-ray and radionuclide studies, and the asymmetry of dye excretion detected using chromocystoscopy in the vast majority of cases make it possible to recognize the disease.
The question of the presence of renovascular hypertension is resolved using intravenous urography, radionuclide renography and aortoarteriography.
Treatment of chronic pyelonephritis should be carried out over a long period of time (years). Treatment should begin with the appointment of nitrofurans (furadonin, furadantin, etc.), nalidixic acid (negram, nevigramon), 5-NOK, sulfonamides (urosulfan, atazole, etc.), alternating them.
At the same time, it is advisable to treat with cranberry extract. In case of ineffectiveness of these drugs or exacerbations of the disease, broad-spectrum antibiotics are used. The prescription of an antibiotic should each time be preceded by determining the sensitivity of the microflora to it.
For most patients, monthly 10-day courses of treatment are sufficient. However, in some patients with such therapeutic tactics, virulent microflora continues to be sown from the urine.
In such cases, long-term continuous antibiotic therapy is recommended, changing drugs every 5-7 days.
With the development of renal failure, the effectiveness of antibacterial therapy decreases (due to a decrease in the concentration of antibacterial drugs in the urine).
When the residual nitrogen content in the blood serum is more than 0.7 g/l, it is practically impossible to achieve a therapeutically effective concentration of antibacterial drugs in the urine.
In the absence of renal failure, resort treatment is indicated in Truskavets, Essentuki, Zheleznovodsk, Sairm, Bayram-Ali.
Source: https://entsefalopatiya.ru/venerologija/mesjachnye-pri-pielonefrite/
What other causes of pain
There are cases when a woman does not have diseases of the genitourinary system, but still experiences pain in the lumbar region during menstruation. This may occur due to:
- Poor nutrition. Eating unhealthy, fried, smoked, salty foods. Pain can occur with excessive drinking and smoking, as this puts additional strain on the kidneys.
Taking medications often causes kidney pain
- Taking medications. With long-term use of certain medications, kidney function is impaired.
- Use of hormonal drugs. Oral contraceptives increase the load on many organs, including the kidneys. It is necessary to change the method of contraception to reduce pain.
When to worry
Most women keep a menstrual calendar. They notice any abnormalities in the cycle and, asking whether there may be a delay after cystitis, visit the doctor on the second day after the pathology is detected.
Deviations of 5-7 days are considered normal. Some women have irregular periods all the time. In this case, it is even more difficult to understand how many days the delay lasts and whether there is cause for concern.
You should consult a doctor if the delay is more than 10 days. It is necessary to visit an antenatal clinic if delays occur constantly. Sometimes an irregular cycle is not an individual feature or a one-time deviation caused by cystitis.
Most often, a violation of the monthly cycle is a sign of severe pathologies of the endocrine or reproductive system.
How is the diagnosis carried out?
In order to determine the cause of pain in the kidney area, you need to consult a gynecologist. The specialist may ask questions about the nature of the discharge and symptoms.
If necessary, the gynecologist will send the woman to a urologist and other doctors.
To diagnose diseases, urine and blood are taken for analysis. Additionally, ultrasound diagnostics of the abdominal cavity is performed. The doctor makes an accurate diagnosis based on the examination results.
This video will tell you about different pains during menstruation:
Delayed menstruation and cystitis: is there a relationship?
A menstrual disorder indicates health problems. The reasons for missed periods (except pregnancy) are hormonal imbalance, stress, gynecological problems, and so on. Cystitis and delayed menstruation are interrelated when inflammation spreads to the ovaries.
Menstrual irregularities are the result of a malfunction of the appendages. Changes in hormonal levels lead to a decrease in bladder tone and the development of cystitis.
The inflammatory process affects the pelvic organs, so for this infection, doctors recommend, in addition to the urologist, making an appointment with a gynecologist.
Cystitis in young women occurs due to sexual activity. IUDs and contraceptive gels can disrupt the microflora.
Women during menopause suffer from cystitis, because there is a relationship between hormonal levels and inflammation of the bladder. During this period, a woman’s pelvic organs descend, which makes it easier for infection to occur. If you have ovarian dysfunction, you should visit your doctor to rule out menopause.
It cannot be said that inflammation in the bladder may be the only cause of cycle disruption. Lack of menstruation is a symptom of physiological, biochemical, genetic, anatomical disorders. The problem lies not only in inflammation of the bladder.
After treatment for cystitis, a woman may experience a delay. The failure occurs due to incompletely cured inflammation, which turns into a chronic disease. Disruption of hormone production also causes a delay in menstruation.
What to do if there is a delay?
In order to establish the cause of menstrual irregularities, a consultation with a gynecologist is necessary. The doctor will select antibacterial medications that have a targeted effect.
If the cause is not pregnancy, the following examinations are prescribed:
- Ultrasound of the genitourinary organs;
- blood analysis;
- PCR diagnostics;
- urine analysis (general and Nechiporenko);
- biopsy.
To exclude pathology in the pituitary gland, a CT scan of the brain and an MRI are prescribed. Other examinations may be provided. In order to exclude sexually transmitted infections, a flora culture is done. The doctor develops further treatment tactics. The restoration of the menstrual cycle is considered a positive result.
How to restore the menstrual cycle?
Medical procedures alone do not normalize the cycle. The functioning of the ovaries is restored by a whole range of measures:
- physical education classes;
- balanced diet;
- vitamin therapy;
- work and rest schedule.
Consequences
Advanced cystitis will cause inflammation to spread to other organs. The infection penetrates the appendages and kidneys, so cystitis is treated at an early stage. Sometimes inflammatory diseases occur in a latent form. The patient may not even know that she has a sexually transmitted disease.
If a woman has a delay due to cystitis, she should immediately consult a doctor. The neglected inflammatory process leads to infertility.
After the examinations, the doctor will prescribe a comprehensive treatment. The inflammatory process is stopped if it is not started. The doctor finds out the nature of the pathogenic organisms. The success of treatment depends on how correctly the antibacterial agent is selected.
The following drugs are prescribed:
- Monural;
- Nolitsin;
- Palin;
- 5-NOK and others.
The doctor prescribes non-steroidal anti-inflammatory drugs if the pain syndrome is severe. Indomethacin, Nurofen, Diclofenac and others are prescribed. If cystitis is discovered before menstruation, treatment should be started immediately. During this period, drinking plenty of fluids is recommended.
Prevention
The mucous membrane of the urinary system is resistant to microbes, but sometimes the defense mechanisms fail. Preventive measures:
- Cystitis develops in the cold season, so you should not get too cold.
- Women should treat infections, including sore teeth.
- It is important to maintain a urination schedule (4–7 times a day).
- You should empty your bladder before and after sexual intercourse.
- Underwear should not restrict movement.
- Following good hygiene reduces the risk of infection.
- You need to drink 2 liters of water per day.
- Salty, sour, spicy and alcoholic drinks cause inflammation of the bladder.
- It is necessary to engage in physical education. This is important when working sedentarily.
Menstrual irregularities due to inflammation of the bladder are possible if the infection penetrates into the appendages.
Source: https://MedLab.expert/cistit/zaerzhka-mesyachnyh-i-cistit-est-li-vzaimosvyaz
How is pain treated?
If severe pain occurs, you can take painkillers. For example: Baralgin, No-shpa, Spazmalgon. It is necessary to visit a specialist and not self-medicate.
The doctor prescribes medications not only to relieve symptoms, but also to get rid of the cause of the pain. Antibacterial and anti-inflammatory drugs reduce inflammation. Analgesics relieve pain. In addition, decoctions of herbs may additionally be prescribed. The course of medication depends on the manifestation of the disease.
If the examination does not reveal any abnormalities in the woman’s health, it is recommended to follow traditional methods: a warm bath and rest.
It is very important to monitor your diet; it is best to eat foods that have a diuretic effect (watermelon, melon, berry fruit juice). A woman needs to do yoga, listen to pleasant music, and walk more in nature. Physiotherapy methods such as acupuncture and massage can be used.
Food should be healthy
Diet
The first thing to do is exclude fried, fatty, spicy foods from the diet. Broths made from mushrooms and fish are prohibited, as they contain many extractive substances that can provoke an exacerbation of the disease.
The menu is enriched with:
- dietary products made from flour (pasta, day-old black bread);
- vegetables and fruits;
- dairy products;
- juices, fruit drinks.
The attending physician can prescribe alkaline mineral waters in courses with a specific dose depending on individual needs.
Meat and fish dishes must be boiled.
Eating foods that have a slight laxative effect, such as beets and prunes, will reduce the risk of constipation.
As for the use of salt, it all depends on the complexity of the process. Basically, salt is excluded in case of severe pyelonephritis.
Gallery of approved products
Dairy
Prunes
Beet
Fruits
Vegetables
What is pain prevention?
To prevent the development of certain diseases, it is recommended to follow the following rules:
- Maintain personal hygiene. It is necessary to carefully care for the intimate area.
- Do not get carried away with taking medications. It's best to use them only when necessary.
- Stop using hormonal contraceptives.
- Avoid hypothermia of the body. Choose clothes and shoes according to the weather.
- Avoid frequent changes of sexual partners and use protection.
- On the eve of menstruation, do not eat unhealthy, salty, fried, spicy, fatty foods. It is better to eat light foods.
- Do exercises in the morning, walk in the fresh air.
- Visit a gynecologist once a year.
The kidneys are located close to the genitals, so it is necessary to take into account that the occurrence of painful sensations is not always associated with diseases of the renal system. To identify the cause, you need to contact a gynecologist who will conduct an examination and prescribe the necessary treatment.
Main symptoms and signs of kidney disease in women
July 22, 2020
The functional ability of the kidneys is an important component of the health of the body as a whole, as these organs filter the blood from toxins and harmful substances. Any damage to an internal organ leads to insufficient cleansing. In this case, the symptoms of kidney disease in a woman will be expressed not only by pain in the lumbar region, but also by discomfort in the genitourinary system.
Causes
The main cause of kidney disease in women is a weakened immune system. A harmful bacterium entering the body, most often through the urethra (along the ascending route), travels through the genitourinary system to the kidney, thereby provoking inflammation.
The causes of intoxication of the body caused by improper functioning of the kidneys can be associated with various factors:
- lack of a balanced diet, the predominance of protein foods creates excessive stress on the internal organs;
- abuse of alcoholic beverages provokes the kidneys to increase filtration in order to remove harmful substances;
- stagnation of urine in the urinary system contributes to the return of urine to the ureter, subsequent infection and expansion of the pyelocaliceal region;
- uncontrolled use of medications increases the load on the kidneys;
- poor environmental situation, contaminated drinking water causes many kidney diseases;
- congenital diseases.
Symptoms and development
Often the development of kidney diseases at the initial stage is asymptomatic; as the pathology progresses, signs appear that directly or indirectly indicate the disease in women:
- renal colic of varying intensity, which can be either unilateral or bilateral;
- discomfort when urinating, often accompanied by pain;
- frequent urge to urinate, with occasional urine discharge;
- hematuria – bloody spots in the urine;
- high temperature indicates the presence of an infectious process;
- persistent hypertension;
- general weakness, headache, chills, increased fatigue, decreased appetite, possible feeling of nausea, vomiting.
Along with symptoms caused by internal processes, there are external signs that can be used to suspect kidney disease in women:
- swelling reactions on the eyelids (bags under the eyes) or face (puffiness), appearing in the morning;
- dry, pale skin;
- brittle hair and nails;
- anemia;
- shortness of breath without any physical activity.
The detection of several of the above symptoms in a patient indicates the development of the disease, so it is worth consulting a nephrologist or urologist to make an accurate diagnosis.
Major kidney diseases
There are kidney diseases that have the highest prevalence according to statistical data.
Pyelonephritis is infectious in nature, the disease is caused by an acute or chronic stage of development. The harmful microorganism enters the body through any source of infection (tonsillitis, caries, cystitis, less often through the blood), after which it begins an inflammatory reaction in the kidney tissue and pelvic area.
The disease can worsen if there are large stones that block the flow of urine. Stagnation of urine and subsequent infection occurs. The acute stage of pyelonephritis is characterized by pronounced symptoms, in contrast to the chronic course of the disease, in which the signs of the disease are sluggish.
Glomerulonephritis is an inflammatory disease of the renal glomeruli, in which the symptoms are very mild, due not only to the presence of infection, but also to an allergic reaction of the body.
A urine test indicates all the signs of glomerulonephritis:
- hematuria;
- the density and color of urine are not normal;
- leukocyturia;
- proteinuria.
The main and main symptom of the disease is a persistent increase in blood pressure, which is difficult to reduce even after taking appropriate medications. An additional sign of pathology can be a violation of the water-electrolyte balance, with fluid retention and edematous reactions.
Urolithiasis (UCD) is the formation of stones in the renal pelvis and other organs of the urinary system (ureters, bladder). Crystallization of stones can be triggered by various factors, ranging from contaminated drinking water to disturbances in the internal processes of the body.
Symptoms of ICD have a pronounced characteristic color:
- colic in the lumbar region;
- pain syndrome radiating to the groin area;
- presence of blood or pus in the urine.
Diagnostic measures
Making a diagnosis involves the use of a number of examinations, since the symptoms of the disease may indicate not only kidney disease:
- Ultrasound is the most popular method for diagnosing diseases of internal organs not only in women, but also in men. The examination is effective in the presence of signs of an inflammatory process, to detect abnormal enlargements or shifts of the kidneys.
- CT scan of the kidneys is used for a more detailed study of the pathological processes occurring inside the organ.
- Excretory urography is used to understand the functional state of the kidneys and their ability to fulfill their intended purpose.
- Magnetic resonance imaging is a method that allows you to most accurately determine the disease, and is especially effective when tumor tumors are suspected.
- Angiography – determines pathologies associated with the renal vessels.
- Kidney biopsy is used only when the diagnosis is unclear.
Laboratory tests of urine and blood are also used to understand the dynamics and severity of the disease.
Treatment and prevention
Depending on the stage of the disease, therapy may be prescribed, which includes medications and dietary changes to reduce unnecessary stress on the kidneys. First of all, treatment involves eliminating the infection with antibacterial agents and relieving symptoms with pain medications.
A preventive or therapeutic diet provides for the following conditions:
- eliminating salt from the diet in order to reduce fluid retention in the body;
- try to eat fresh food. Limit spicy, salty, canned and fried foods;
- eat small meals - several times a day;
- give up bad habits (alcohol, smoking);
- the diet should contain the maximum amount of fiber;
- observe the drinking regime.
The female body is more susceptible to kidney diseases due to physiological characteristics. Therefore, if you have symptoms of urinary disorders, you should immediately consult a doctor to avoid the development of chronic pathologies and infection of the reproductive system.