Often occurs in various stressful situations with latently existing hypofunction of the adrenal glands - acute adrenal insufficiency in children. In this article we will look at the main causes and symptoms of acute adrenal insufficiency in children, as well as how acute adrenal insufficiency in a child is treated.
Symptoms of acute adrenal insufficiency in children
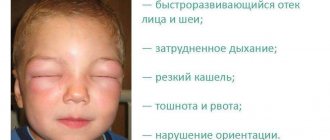
Clinical symptoms of sudden onset adrenal insufficiency depend on the age of the child. In newborns and infants, the first signs of adrenal insufficiency are:
- regurgitation, turning into “fountain” vomiting,
- diarrhea and polyuria with the development of exicosis,
- blood pressure drops quickly,
- dullness of heart sounds is detected,
- peripheral circulation is disrupted until hypostatic (“cadaveric”) spots appear,
- collapse develops.
Before the onset of acute vascular insufficiency, older children may complain of the following symptoms: headache and abdominal pain. As collapse develops, diuresis stops until anuria occurs.
Diagnostics
Addison's pathology can be confirmed by monitoring the dynamics of changes in the level of hydrocortisone in the blood serum.
In a healthy person, there is a sharp jump in the level of cortisol in the blood in the morning upon awakening, and in patients with adrenal insufficiency, the level of this hormone is constantly in the lower values.
At the same time, low readings of aldosterone and renin concentrations are monitored. High concentrations of potassium, together with pathologically low blood sugar levels, are observed during a disease crisis. In daily urine, a decrease in the total level of 17-hydroxycorticosteroids can be noted, although such a study is not highly effective.
When the patient's blood is taken on an empty stomach, low blood sugar levels are noted, as well as a flat shape of the glycemic curve.
Tests using the drug prednisolone have almost no effect on increasing cortisol levels.
A combined method for diagnosing adrenal insufficiency is carried out together with intestinal infections, helminthic infestations, and intoxications.
Adcison's disease in infants must be differentiated from pyloric stenosis and pylorospasm, as well as the adrenogenital symptomatic complex, accompanied by loss of mineral salts.
At the same time, it is necessary to differentiate acute adrenal failure from various infections, as well as from intestinal neuroinfections.
When diagnosing the disease in older children, it is necessary to initially exclude sepsis, encephalitis and meningitis.
Methods of treating the disease
When a crisis of adrenal insufficiency occurs, it is common to use a combination of methods such as:
- suppression of shock;
- returning fluid levels, as well as mineral levels, to normal levels;
- replenishment of hormone deficiencies.
The patient is prescribed droppers of an isotonic sodium solution with 5 percent glucose to which 100 milligrams of cortisol are added. This dropper is repeated every 4-8 hours.
In addition, doctors most often prescribe the use of adrenaline, corglycone, and vitamin C. 1-3 milliliters of DOX oil solution is injected intramuscularly once a day.
The main guidelines in the process of bringing a patient out of a crisis are:
- patient dehydration;
- content of basic mineral compounds in the blood;
- CBS;
- blood sugar level.
The duration of therapy using a dropper depends on the severity of the patient’s condition, which can last up to 5 days. As the patient's general condition improves, the dose of cortisone in the dropper is reduced when switching to intramuscular administration of this drug.
In the chronic form of the disease, constant therapy is used throughout the patient's life using prednisolone and cortisone. When observing vomiting in a patient, it is customary to replace prednisolone with intramuscular cortisone.
Parents of children diagnosed with chronic adrenal insufficiency should know the basic principles of lifelong replacement therapy. If you follow simple rules and constantly use medications prescribed by doctors, the life of a patient with chronic adrenal insufficiency will be complete.
Neonatal endocrinopathies in newborns
Adrenal insufficiency. During the neonatal period, various diseases associated with dysfunction of endocrine organs are observed. Among them, adrenal insufficiency is the most common. Its causes may be congenital virilizing hyperplasia of the adrenal cortex, hypoaldosteronism, hemorrhages in the adrenal glands, congenital hypoplasia of the adrenal cortex, and infectious diseases.
Congenital virilizing hyperplasia of the adrenal cortex (congenital dysfunction of the adrenal cortex, congenital adrenogenital syndrome, female pseudohermaphroditism) is a hereditary disease that, according to various authors, occurs in 1 case per 5000 births with the same frequency in boys and girls. Inherited in an autosomal recessive manner. The disease often recurs in several children in a family in the same form.
The pathogenesis of congenital virilizing adrenal hyperplasia is based on a violation of the biosynthesis of corticosteroids as a result of a deficiency of enzymes involved in its synthesis. A constant deficiency of cortisol in the body of patients causes increased production of ACTH by the hypothalamus-pituitary gland system. ACTH intensely stimulates the adrenal glands and leads to hyperplasia of their cortex, which, however, is not accompanied by an increase in the production of glucocorticoids and mineralocorticoids. At the same time, in the adrenal cortex, intermediate biosynthesis products (progesterone, 17-hydroxyprogesterone, deoxycorticosterone) and androgens are formed in large quantities, in the synthesis of which the enzymes 21- and 11-p-hydroxylase do not participate. With congenital hyperplasia of the adrenal cortex, due to increased production of androgens, the external genitalia in girls are formed incorrectly (pseudogermaphroditism). After the birth of a child, excessive production of androgens by the adrenal cortex leads to increased symptoms of virilization in girls, accelerated physical development of children of both sexes and premature puberty in boys according to the isosexual type, and girls - according to the heterosexual type.
There are 3 clinical forms of the disease depending on the degree of deficiency of gluco- and mineralocorticoids. With partial deficiency of the 21-hydroxylase enzyme (viril form - 57% of all forms), the lack of cortisol production is compensated by hyperplasia of the adrenal cortex. The amount of hormones sufficient for everyday life enters the blood. With a more profound deficiency of the enzyme 21-hydroxylase, the synthesis of not only cortisol, but also mineralocorticoids is impaired. The salt-wasting form of the disease develops (38%). This form of congenital dysfunction of the adrenal cortex is accompanied by severe metabolic disorders. A lack of aldosterone in the body leads to impaired potassium secretion with its retention in the body and sodium reabsorption with its excessive release by the renal tubules. Cortisol deficiency, which normally contributes to sodium retention in the body, also predisposes to sodium loss. The body's loss of sodium is accompanied by the release of large amounts of extracellular fluid with the rapid development of dehydration. Potassium retention in the body leads to an increase in intracellular osmolarity, the movement of fluid from the extracellular space with the development of intracellular edema, which can cause cerebral edema with convulsive syndrome. Vomiting and loose stools characteristic of adrenal insufficiency worsen the disturbance of water-electrolyte metabolism and lead to shock from dehydration. Altered sodium reabsorption is associated with impaired secretion of hydrogen ions—metabolic acidosis. Dehydration, hyperkalemia, hyponatremia and metabolic acidosis cause severe dysfunction of the central nervous system and cardiovascular system, kidneys, gastrointestinal tract and other organs.
In addition to severe deficiency of 21-hydroxylase, the salt-wasting form of the disease can be caused by a deficiency of the enzyme 3-β-hydroxydehydrogenase. This form of the disease is rare (1%). Since the 3-B-hydroxydehydrogenase enzyme system is involved in the synthesis of sex hormones, disruption of the synthesis of the latter in the fetal testicles leads to abnormal structure of the external genitalia in boys: hypospadias, cryptorchidism, and splitting of the scrotum. Patients with this enzyme deficiency experience severe disturbances in electrolyte metabolism.
The hypertensive form of congenital adrenal hyperplasia (3%) develops as a result of deficiency of the enzyme 11-B-hydroxylase. The synthesis of mineralocorticoids in conditions of 11-B-hydroxylase deficiency is characterized by the accumulation of deoxycorticosterone, which causes an increase in blood pressure. Rare forms of the disease (salt-wasting form without pronounced virilization, periodic etiocholanolone fever, etc.) account for about 1%.
Clinical symptoms of congenital virilizing adrenal hyperplasia depend on the form of the disease. A simple, uncomplicated form can be suspected in a newborn girl due to virilization of the genital organs, and it is very difficult to diagnose a boy, since his symptoms of the disease appear 2-3 years later in the form of premature puberty. However, in severe stressful situations (illness, surgical interventions, intense physical activity), when the need for hormones increases sharply, children with an uncomplicated form of the disease develop crises of adrenal insufficiency (adynamia, hypotension, dyspeptic disorders, dehydration, decreased blood pressure). Without hormonal therapy, blood pressure reaches zero, loss of consciousness and death occur.
Clinical manifestations of the salt-wasting form usually develop in the first days of life. Children experience sluggishness in sucking, regurgitation, vomiting, significant loss of body weight, insufficient weight gain, and polyuria. A sharp deterioration in condition (crisis of acute adrenal insufficiency) most often develops in the 3rd week of life. Its occurrence may be precipitated by intercurrent illness. Characterized by severe lethargy, adynamia, cold sweat, breast refusal, persistent vomiting, dyspeptic disorders, frequent and profuse urination. When examining children, pallor or cyanosis of the skin, emphasized marbled skin pattern, muscle hypotonia, symptoms of dehydration of the II and III degrees are revealed (sharpened facial features, decreased tissue turgor, dry mucous membranes, shortness of breath, tachycardia, muffled heart sounds). Some children experience increased gastric motility, reminiscent of an “hourglass” symptom. In the absence of urgent treatment, loss of consciousness, convulsions, and cardiopulmonary failure may occur. Without active treatment, crises of adrenal insufficiency in children with a salt-wasting form of congenital dysfunction of the adrenal cortex end in death.
A quick diagnosis is of great importance for effective treatment. The diagnosis is made when girls have abnormal genital structure; During a crisis in boys, an important diagnostic sign is polyuria against the background of severe symptoms of dehydration. Laboratory tests help establish an accurate diagnosis, since a crisis of adrenal insufficiency is always accompanied by hyponatremia, hyperkalemia, metabolic acidosis with severe base deficiency, signs of hyperkalemia on the ECG, and increased excretion of sodium and chlorine in the urine. An important diagnostic method is to determine the content of 17-KS in daily urine: normally, in the first 10-14 days of life, from 4.6 to 8.67 µmol/l 17-KS is excreted in the urine per day, in the 3-4th week of life - from 0.693 to 1.73 µmol/l. With congenital adrenal hyperplasia, urinary excretion of 17-CS can be increased by 34.67 μmol/L per day or more. To clarify the depth of deficiency of enzyme systems and the localization of the block in the biosynthesis of steroid hormones, a chromatographic study of corticosteroids in daily urine is indicated. When making a diagnosis, family history may be important: the birth of children with a similar clinical picture, their early death from acute adrenal insufficiency.
Differential diagnosis in girls is made with malformations of the male genital organs, intersexism, and female pseudohermaphroditism of a different origin. In boys during a crisis of adrenal insufficiency, hypoaldosteronism, pyloric stenosis, gastroenterocolitis, sepsis, pneumonia, and meningitis are excluded.
With pyloric stenosis, the deterioration of the child’s condition develops less acutely, there is no anorexia, cyanosis, marbling of the skin, muscle hypotension, excessive urination, or dyspeptic stool; on the contrary, there is a tendency to constipation. In the blood with pyloric stenosis, metabolic alkalosis, hyponatremia and hypokalemia occur. Palpation of the hypertrophied pylorus has important diagnostic value. X-ray examination of the lungs helps to exclude pneumonia, meningitis - a spinal puncture, sepsis - the absence of purulent foci and normal blood tests.
The characteristic appearance of the genital organs helps determine the correct sex in girls with congenital adrenal hyperplasia. There are 5 types of virilization of the external genitalia. What they have in common is the presence of an enlarged clitoris with a glans and foreskin, reminiscent of a hypospadiastic male penis. Type I is characterized by a normal structure of the female genital area. In type II, the vestibule of the vagina is deepened and funnel-shaped. With types I and II of the structure of the external genitalia, there are 2 openings - the urethra and the vagina, but they are located close to each other. In types III and IV, there is a common urogenital opening at the base of the penis-shaped clitoris. The labia minora are absent, the labia majora are fused and scrotal-shaped. In patients with type V, the urogenital opening is located at the top of the penis-shaped clitoris and the structure of the external genitalia corresponds to the male, but there are no testicles. In difficult cases, to establish the true gender of the child, they resort to the study of sex chromatin.
In addition to adrenogenital syndrome, signs of female pseudohermaphroditism in fetuses appear with androgen-producing tumors in the ovaries and adrenal glands of a pregnant woman or when she is treated with hormones (progesterone, testosterone, stilbestrol). Anamnesis, symptoms of virilization in the mother, and disappearance of symptoms of virilization in the child without treatment help to establish the diagnosis.
Treatment of congenital dysfunction of the adrenal cortex is of a replacement nature. Children are prescribed glucocorticoid drugs to eliminate cortisol deficiency, normalize the secretion of ACTH by the pituitary gland, and reduce the synthesis of androgens to normal amounts. An adequate dose of hormones normalizes the physical development of children, prevents premature puberty, reduces the tendency to intercurrent diseases and eliminates the symptoms of virilization in girls.
Treatment of an uncomplicated form of congenital adrenal hyperplasia begins with a glucocorticoid test, which is both diagnostic and the beginning of therapy. Using the test, you can differentiate congenital adrenal hyperplasia from a tumor - androsteroma. Test technique: after determining 17-KS in daily urine, the child is administered hydrocortisone 25 mg (1 ml) intramuscularly for 5 days. Then daily urine is collected again at 17-KS. Hydrocortisone blocks the release of ACTH, resulting in decreased androgen synthesis. The sample is considered positive if the release of 17-KS is reduced by 50% or more. A negative test indicates a tumor of the adrenal cortex.
After confirmation of the diagnosis, intramuscular administration of glucocorticoids is replaced by medications (prednisolone). The therapeutic dose is selected under the control of urinary excretion of 17-KS. Patients should receive glucocorticoid drugs for life. If stressful conditions occur (illness, injury, surgery), the dose of glucocorticoids should be increased by 1.5 times and oral administration of hormones should be replaced with parenteral administration.
In children with a salt-wasting form of the disease, therapy is always carried out according to vital indications. After the diagnosis is established, treatment begins with intravenous or intramuscular injections of hydrocortisone at a rate of 3-5 mg per 1 kg of body weight 2-3 times a day. According to indications, the dose is increased to 25-100 mg per day. The drug is administered parenterally until the general condition improves - on average 3-5 days. However, in most patients, administration of glucocorticoid drugs and salt alone does not eliminate electrolyte disturbances. They are shown intramuscular administration of mineralocorticoids - deoxycorticosterone acetate (DOXA); During periods of adrenal insufficiency crisis, 5 mg of this drug is administered subcutaneously.
Simultaneously with hormonal medications, intravenous drips of fluid in the form of colloidal solutions (plasma, albumin, polyglucin, rheopolyglucin) and 10% glucose solution with isotonic or hypertonic sodium chloride solution are required to quickly eliminate BCC deficiency and dehydration. It is impossible to administer potassium preparations or liquids containing potassium (hemodez, polyionic solution, etc.) due to hyperkalemia in this disease.
The total amount of fluid for infusion therapy depends on the degree of dehydration and the depth of electrolyte disturbances. On average, it should be at least 200-300 ml per 1 kg of body weight per day. The duration of intravenous drips of fluid is determined based on the elimination of symptoms of dehydration and normalization of the content of electrolytes in the blood serum. With the introduction of a sufficient amount of fluid, hormones and salt, the general condition of patients noticeably improves: the child becomes more active, vomiting stops, appetite appears, and body weight regularly increases. After recovery from the adrenal insufficiency crisis, the dose of glucocorticoid drugs is gradually reduced under the control of the concentration of 17-KS in the urine. It is advisable to replace DOX injections by implanting a DOX crystal tablet (100 mg) under the skin. Its effect lasts 6-8 months. Children with congenital virilizing adrenal hyperplasia require constant monitoring by a pediatrician and endocrinologist.
Hypoaldosteronism is an isolated violation of the mineralocorticoid function of the adrenal cortex. It is extremely rare. There is a hereditary form, which is based on an enzymatic block in the synthesis of aldosterone (18-oxidase deficiency), and transient hypoaldosteronism, in which a decrease in aldosterone secretion is caused by a delay in the maturation of the zona glomerulosa of the adrenal cortex. Both forms are characterized by anorexia, regurgitation and vomiting, increased intestinal motility, the development of severe degrees of dehydration against the background of hyponatremia, hyperkalemia, loss of a significant amount of salt in the urine, and reduced aldosterone excretion. In contrast to congenital hyperplasia of the adrenal cortex with hypoaldosteronism, the genital organs in girls are formed correctly, there is no skin pigmentation, and the size of the adrenal glands is normal. The levels of glucose in the blood and 17-KS in the urine are within normal limits.
Treatment of hypoaldosteronism is reduced to the administration of mineralocorticoids (DOXA) and saline solutions until the electrolyte composition of the blood is normalized.
Acute adrenal insufficiency in newborns can result from damage to the normally formed adrenal gland. In the first days of life, it is often observed in children who have suffered asphyxia or birth trauma, as well as with intrauterine infection and the addition of intercurrent diseases - sepsis, pneumonia, ARVI. The cause of acute adrenal insufficiency in these children is hemorrhage into the adrenal glands.
In the pathogenesis of hemorrhages in the adrenal glands, the main role is played by disturbances of the uteroplacental circulation, intrauterine fetal hypoxia, increased fibrinolytic activity of the blood, the occurrence of diapedetic hemorrhages, and thromboembolic vascular lesions. Predisposing factors are physiological hypothrombinemia in newborns, increased fragility of the adrenal vessels, their relatively large size and location in an easily vulnerable area, features of the venous outflow of blood from the adrenal glands and the structure of the wall of the central adrenal vein and its medullary branches. Massive hemorrhages in the adrenal glands are often a consequence of disseminated intravascular coagulation syndrome as a result of bacterial shock.
The leading clinical symptoms of hemorrhage into the adrenal glands are lethargy, adynamia, vomiting, hyporeflexia, hypotonia of the muscles of the trunk and limbs, cyanosis, tachypnea. With traumatic injury to the adrenal glands, from the first hours of life the child develops progressive anemia without visible external bleeding. Sometimes there is a two-phase clinical picture. In the first 1-2 days, less often until the 5th day, the condition remains satisfactory. Then a sudden deterioration occurs (drowsiness, cyanosis, pallor of the skin and mucous membranes, arrhythmic shallow breathing, apnea attacks, muffled heart sounds, bradycardia, hyporeflexia, and sometimes an “acute abdomen”) appear. When palpating the abdomen, a tumor-like formation is determined at the site of the hematoma. As the disease progresses, intense jaundice may appear due to resorption of the hematoma. In some cases, calcification of the hematoma is observed, which persists for life. Additional studies include a blood test for hemoglobin, potassium and sodium, blood pressure measurement, intravenous pyelography (downward displacement of the kidney, impaired excretory function), and an x-ray of the abdominal cavity in two projections.
Therapy for acute adrenal insufficiency is aimed at combating shock, anemia, electrolyte disturbances and increasing blood clotting. For this purpose, hydrocortisone 10-15 mg/kg per day (in 4 doses) is prescribed intravenously or intramuscularly for 7-10 days, DOXA 0.5-1 ml intramuscularly 1 time per day for 10 days to 1 month. When the condition improves, hydrocortisone is replaced with prednisolone. Blood, plasma, 10% glucose solution, isotonic sodium chloride solution are injected intravenously in volumes calculated individually according to the severity of the patient (see Chapter 24, section “Infusion therapy”). At the same time, antibiotics, Vicasol, vitamins C and group B are administered according to indications. If necessary, surgical intervention is performed.
The literature describes observations of the death of newborns from acute adrenal insufficiency as a result of congenital hypoplasia of the adrenal cortex. It may be caused by an intrauterine infection (cytomegaly, destructive processes in the adrenal cortex after involution of the germinal zone, pathology of the hypothalamic-pituitary system with insufficient secretion of ACTH and STH).
Diseases of the parathyroid glands. Hypoparathyroidism can develop as a result of maternal hyperparathyroidism during pregnancy. After birth, the child quickly develops hypocalcemia, which is not accompanied by an increase in PTH levels in the blood due to temporary inhibition of the function of the parathyroid glands. Observations of congenital transient idiopathic hypoparathyroidism are described, in which, in addition to hypocalcemia, hyperphosphatemia is observed. The disease is associated either with impaired renal excretion of phosphates or with early hypovitaminosis D. Hereditary forms of hypoparathyroidism are known in combination with a severe immune defect due to simultaneous aplasia of the parathyroid glands and thymus gland.
Clinically, the symptoms of hypoparathyroidism are manifested by increased neuromuscular excitability, increased physiological reflexes, tremor of the limbs and chin, convulsive readiness and convulsions. Symptoms of transient hypoparathyroidism last for 1-3 weeks; hereditary forms are accompanied by persistent changes in the nervous system (convulsive seizures) and impaired physical development.
Treatment of transient forms of hypoparathyroidism is carried out by intravenous administration of calcium solutions with glucose, and the administration of calcium preparations orally. According to V. Blunk, simultaneous administration of PTH during the 1st week of life has a good effect. If the symptoms of hypoparathyroidism persist, the administration of calcium supplements is combined with high doses of vitamin D—up to 20,000 IU daily. Indications for discontinuation of treatment are the disappearance of symptoms of hypoparathyroidism and normalization of biochemical parameters. Hereditary forms of hypoparathyroidism require long-term treatment by endocrinologists.
Hyperparathyroidism in newborns is extremely rare. At birth, the child has muscle hypotonia, rickets-like skeletal deformation, and a high concentration of calcium in the blood. The prognosis is unfavorable.
Diabetic fetopathy of newborns is a consequence of severe endocrine and metabolic disorders in fetuses from mothers with diabetes. The degree of damage to the fetus depends on the duration of the mother's illness and the severity of its course. Most children are born premature, with a large body weight with a disproportionate build, with an overdeveloped subcutaneous fat layer, pastosity, and cardiomegaly. The severity of the condition at birth and in the first days of life is due to intrauterine and postnatal hypoxia, birth trauma, severe and prolonged hypoglycemia, a decrease in blood sugar to 0.555-1.665 mmol/l, and functional immaturity of a number of systems. Neonatal adaptation disorders include changes in the central nervous system (lethargy, restlessness, weak cry with a groan, decreased motor activity, muscle hypotonia, hyporeflexia, tremor of the limbs, paresis, clavicle fracture, etc.), the development of varying degrees of respiratory and heart failure (tachypnea or a detailed picture of SDR , expansion of the borders of the heart, tachycardia, muffled tones, enlarged liver), symptoms of adrenal insufficiency. Over time, half of the children experience a significant (10-15%) decrease in body weight and long-term recovery, conjugative hyperbilirubinemia, aseptic necrosis of the subcutaneous fat layer, retardation in neuropsychic development, and the formation of hydrocephalus.
Intensive therapy does not always lead to the desired result. The causes of death in children with severe forms of the disease are hyaline membrane disease, edematous hemorrhagic syndrome, and hemorrhages in the brain and adrenal gland.
Newborns with diabetic fetopathy require intensive care from the first hours of life. Therapeutic measures include intravenous administration of 5-10% glucose solutions (without insulin) until a persistent increase in blood sugar, the administration of cardiac glycosides until the symptoms of heart failure disappear, complex therapy for hemolytic fluid dynamics disorders and SDR, and hormonal therapy in the presence of symptoms of adrenal insufficiency.
Rare forms of endocrinopathies in newborns include intersexism (true hermaphroditism, gonadal dysgenesis) - the presence of ovarian and testicular tissue in a child that disrupts sexual differentiation. The fetus develops both testes and ovaries. The external genitalia can be formed according to the female type, but the testicles are palpable in the thickness of the labia majora. More often, however, there is a developed penis with elements of hypospadias and the newborn is classified as female. When making a diagnosis, determination of the karyotype, sex chromatin, and the absence of an increase in 17-KS in the urine help. A consultation with an endocrinologist is indicated.
Newborns with male pneudohermaphroditism (with a purely male karyotype have intersex or female genital organs) are more often assigned female gender. The need to clarify gender arises at puberty, when a “girl” has amenorrhea, impaired pubic hair growth, and testicles are detected due to a strangulated inguinal hernia.
The diagnosis of hypogonadism in the neonatal period is questionable due to the lack of gonadal function.
Information
Sources and literature
- Minutes of meetings of the Joint Commission on the quality of medical services of the Ministry of Health of the Republic of Kazakhstan, 2020 1) Federal clinical recommendations for the management of children with endocrine diseases, under the general editorship of Dedov I.I., and Peterkova V.A., M, 2014. 2) Clinical protocol for diagnostics and treatment of acute adrenal insufficiency, 2014 3) Pediatric endocrinology. Atlas (edited by I.I. Dedov, V.A. Peterkova. - M.: GEOTAR-Media, 2020 -240 pp.). 4) Bazarbekova R.B. Guide to endocrinology of childhood and adolescence - Almaty, 2014 -252 p. 5) Stefan R. Bornstein, Bruno Allolio, Wiebke Arlt et all Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline // J Clin Endocrinol Metab ( 2016) 101 (2): 364-389. 6) M.B. Runke, P.E. Mullis Diagnostics of Endocrine function in Children and Adolescence. 4th, revised and extended edition, 2011.
Information
ORGANIZATIONAL ASPECTS OF THE PROTOCOL
List of protocol developers with qualification information:
1) Dosanova Ainur Kasimbekovna - Candidate of Medical Sciences, Associate Professor of the Department of Endocrinology of JSC “Kazakh Medical University of Continuing Education”, Secretary of the RPO “Association of Endocrinologists of Kazakhstan”; 2) Rimma Bazarbekovna Bazarbekova - Doctor of Medical Sciences, Professor, Head of the Department of Endocrinology of JSC “Kazakh Medical University of Continuing Education”, Chairman of the RPO “Association of Endocrinologists of Kazakhstan”; 3) Smagulova Gaziza Azhmagievna - Candidate of Medical Sciences, Associate Professor, Head of the Department of Propaedeutics of Internal Diseases and Clinical Pharmacology of the Republican State Enterprise at the West Kazakhstan State Medical University named after. M. Ospanova."
Disclosure of no conflict of interest:
No.
Reviewers:
Nurbekova Akmaral Asylovna - Doctor of Medical Sciences, Professor of the Department of Therapy No. 2 of the RSE at the RSE "Kazakh Medical University named after. S.D. Asfendiyarov.
Indication of the conditions for reviewing the protocol:
review of the protocol 5 years after its publication and from the date of its entry into force or in the presence of new methods with a level of evidence.
Therapeutic measures
- With severe arterial hypotension:
- Anti-shock position or
- A combination of an anti-shock position with an elevated position of the upper half of the body;
- Inhalation administration of 100% O2 on a constant flow through nasal catheters (mask) or IVL with an “Ambu” bag with oxygenation of 100% O2 on a constant flow;
- Catheterization of the cubital or other peripheral veins or installation of intraosseous access or, and for anesthesiologists and resuscitators - catheterization of the subclavian or other central veins (according to indications);
- Hydrocortisone – 100 mg IM (IV (intraosseous) bolus slowly);
In the absence of hydrocortisone:
- Prednisolone – 60 mg IV (intraosseous) bolus slowly +
- Dexamethasone – 8 mg IV (intraosseous) slow bolus;
- If there is vomiting :
- Metoclopramide -10 mg IV (intraosseous) slow bolus (IM);
- For hypoglycemia :
- Glucose 40% – 20-80 ml, IV (intraosseous) in fractional 20 ml bolus doses;
- Sodium chloride 0.9% – intraosseous drip, at a rate of 10 ml/kg/hour, under auscultatory control of the lungs, on site and during medical evacuation;
- With persistent arterial hypotension (SBP < 90 mmHg):
- Catheterization of the 2nd peripheral vein or installation of intraosseous access or for anesthesiologists-resuscitators - subclavian or other central veins (according to indications);
- Colloids – 500 ml IV (intraosseous) at a rate of 10 ml/kg/hour, under auscultatory control of the lungs, on site and during medical evacuation;
- With persistent arterial hypotension (SBP < 90 mmHg):
- Dopamine – 200 mg IV (intraosseous) by drip or infusion pump, at a rate of 5 to 20 m kg/kg/min., on site and during medical evacuation or, and
- Adrenaline -1-3 mg IV (intraosseous) drip or infusion pump, at a rate of 2 to 10 mcg/min., on site and during medical evacuation or, and
- Norepinephrine – 4 mg IV (intraosseous), drip or infusion pump, at a rate of 2 mcg/min., on site and during medical evacuation;
- For anesthesiologists and resuscitators:
With a SpO2 level <90% against the background of oxygenation of 100% O2 or, and with a level of consciousness <9 points on the Glasgow Coma Scale or, and with persistent arterial hypotension (SBP <90 mmHg):
- Transfer to mechanical ventilation;
- Mechanical ventilation in normal ventilation mode;
- Probe into the stomach;
- Medical evacuation (see “General tactical measures”).
Pathogenesis
Acute adrenal insufficiency is accompanied by a lack of production of mineralocorticoids and glucocorticoids.
As a result, dehydration is observed due to the loss of sodium ions, chlorides and deterioration of their absorption in the intestine.
Dehydration leads to a decrease in circulating blood volume and the development of shock.
Due to an increase in potassium concentration in cells, intercellular fluid and blood serum, the ability of the myocardium to contract is impaired.
The absence of glucocorticoids leads to hypoglycemia and a decrease in the concentration of glycogen in the muscles and liver. The reabsorption and filtration capacity of the kidneys decreases.
In fulminant meningococcal sepsis, bacterial shock causes acute vasospasm, hemorrhage and necrosis of the medulla and cortex of the adrenal glands.
Etiology
Adrenal hemorrhage usually has 2 causes:
- Infection . Infectious diseases such as scarlet fever, measles, typhus cause damage to blood vessels, or rather their inner layer, by toxins. This leads to increased blood clotting, platelet aggregation, and thrombosis of the adrenal glands. This causes numerous hemorrhages in 60% of cases of Waterhouse-Friderichsen syndrome. The situation is aggravated by the fact that the affected vessels cannot carry oxygen, which means that the cells of all tissues are affected.
- Medical errors at the time of adoption of a child . Difficult childbirth and incorrect actions by the doctor lead to oxygen starvation. As a result, breakdown products accumulate in the body, affecting the adrenal glands. The result is the appearance of a hematoma. At risk are newborns with entanglement, diabetes mellitus, as well as those whose umbilical cord was cut too early (before the pulsation stops).
Classification
Acute pathology occurs as a result of a sharp decrease or cessation of hormone synthesis by the adrenal cortex. Chronic pathology develops with a lack of cortisol and aldosterone (hormones of the adrenal cortex), and can be congenital or acquired.
Chronic pathology is divided into:
- primary (occurs when adrenal tissue is damaged);
- secondary (the pathological process affects the anterior lobe of the pituitary gland, the production of ACTH is disrupted);
- tertiary (develops as a result of damage to the hypothalamus by a pathological process, characterized by insufficient production of corticotropin-releasing hormone).
In 95% of cases, Addison's disease (primary chronic adrenal insufficiency) is observed.
Causes
Up to 3 years of age, the adrenal glands in children are characterized by physiological immaturity.
Acute adrenal insufficiency can lead to:
- some infectious diseases caused by bacteria, viruses, parasites, fungi;
- autoimmune processes (destruction of the adrenal glands as a result of exposure to one’s own antibodies);
- stress;
- hemorrhage in the adrenal glands (caused by injury, meningococcal infection).
The cause of primary failure was previously considered to be tuberculosis of the adrenal glands. Now most cases are due to hereditary diseases. The risk of pathology increases in children:
- If one of the hereditary diseases is detected, characterized by adrenal insufficiency, which currently has no symptoms.
- If there is a patient in the family with adrenal insufficiency or any inherited disease.
- In the case of any autoimmune pathology of the endocrine system (especially Graves' disease, hypoparathyroidism).
- After radiation therapy sessions, surgery in the area of the hypothalamus, pituitary gland.
- With congenital hypopituitarism.