During pregnancy, women face various diseases due to the hormonal changes that occur. In addition, pregnant women often have a weakened immune system. All this affects the overall functioning of the body, and some of its functions may fail, resulting in the appearance and development of some disease that the woman had never even heard of before pregnancy. Gestational pyelonephritis is one such disease.
How do the symptoms of the disease manifest themselves?
Pyelonephritis in pregnant women gives pronounced symptoms at the end of the second trimester. Their intensity depends on the type and stage of development of the pathology. During an exacerbation, women exhibit the following symptoms:
- Hyperthermia;
- Loss of appetite;
- Weakness throughout the body;
- Vomiting, nausea;
- Lethargy;
- Pain in muscles and head;
- Chills.
During remission, most symptoms disappear. The only signs of chronic pyelonephritis during pregnancy are aching painful sensations. They are localized in the lumbar spine on the side where the affected organ is located. If a pregnant woman follows the recommendations of her doctor, the likelihood of complications is significantly reduced.
The asymptomatic form of renal disease is classified into a separate group. In this case, symptoms are almost completely absent, which greatly complicates the differential diagnosis.
Diagnostic measures
A wide range of different techniques are used to diagnose pyelonephritis. The examination usually begins with laboratory tests, which every woman regularly undergoes at the clinic. If pyelonephritis is suspected, instrumental diagnostic methods are used to differentiate it from other ailments. Most often, kidney inflammation is confused with the following diseases:
- glomerulonephritis;
- appendicitis;
- gastritis;
- peptic ulcer;
- colitis and enterocolitis;
- intestinal infection;
- pancreatitis.
Laboratory methods
Laboratory methods for diagnosing pyelonephritis are divided into primary and secondary. Typically, for safety reasons, the following range of studies is used:
- General blood analysis. An increased number of white blood cells and an increased erythrocyte sedimentation rate (ESR) will indicate the presence of an inflammatory process in the body.
- General urine analysis. It is taken to identify changes in its composition. The density, quantity, and main cellular components are assessed. With pyelonephritis, the urine will be cloudy and contain a high content of white blood cells.
- Bacteriological culture of urine. It will allow you to identify the causative agent of the infection within a few days, which will help you choose the right antibiotic.
For analysis, several tubes with biological contents are usually taken
Instrumental methods
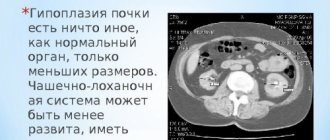
Preference in identifying pyelonephritis is traditionally given to instrumental techniques. For pregnant women, the safest test method is ultrasound diagnostics (ultrasound). With its help, you can examine the structure of the pyelocaliceal system, the condition of the tubules and find out the cause of the pathology.
Ultrasound is the safest method for detecting pyelonephritis in pregnant women
Causes
Gestational pyelonephritis in a pregnant woman most often develops due to mechanical impact. This effect is explained by compression of the kidneys by the uterus. Chronic pyelonephritis can go into an acute phase during the third trimester of pregnancy, it is during this period that the impact on internal organs increases to its maximum. Not only the kidneys suffer, but the functionality of the bladder and ureters decreases due to pressure.
Before you do anything, you need to find out the possible risk factors. In addition to uterine enlargement, the causes of pathology include:
- Hormonal changes in the body;
- A history of chronic diseases of the genitourinary system;
- Weakening of the protective function;
- Insufficient physical activity;
- The influence of low temperatures;
- Infectious infection;
- Failure to comply with personal hygiene rules;
- Malformations of the urinary tract;
- Promiscuous sex life.
Inflammation of the renal pelvis negatively affects both the health of the expectant mother and the condition of the fetus.
Pyelonephritis during pregnancy
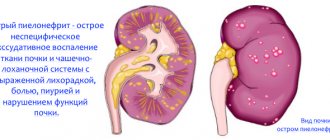
Pyelonephritis is an infectious disease characterized by inflammation of interstitial tissue involving the calyces and pelvis. The prevalence of this pathology among pregnant women reaches 7%. There are 3 degrees of severity of pyelonephritis. In mild forms, acute inflammation develops. There are no complications. With timely treatment, pregnancy and childbirth proceed without complications.
Pyelonephritis of 2nd severity often occurs in a chronic form. In 20–30% of cases it leads to complications. The most severe is gestational pyelonephritis of the 3rd degree. Against this background, secondary (symptomatic) arterial hypertension and renal failure develop. In this situation there is a risk for the child. If the disease is detected before the child is conceived, then pregnancy is not recommended due to the high risk.
Main etiological factors
Gestational pyelonephritis during pregnancy develops for several reasons. The main predisposing factors are:
- stagnation of urine;
- reflux as a result of decreased tone of the bladder and ureters;
- penetration of infection;
- hormonal changes;
- compression of the ureters by an enlarged uterus;
- urolithiasis disease;
- impaired blood circulation;
- cystitis;
- urethritis;
- presence of diabetes mellitus;
- immunodeficiency;
- dystopia;
- catheterization
In most cases, kidney inflammation is detected in the 2nd and 3rd trimesters. Most often, bacteria (Escherichia coli, cocci) are the causative agents of pyelonephritis. Their active spread is facilitated by an increase in the level of progesterone in the blood. This hormone reduces the tone of the ureters and bladder.
Urinary excretion becomes difficult. Defense mechanisms do not work, and microbes accumulate, penetrating the kidneys through the ascending route. Sometimes bacteria spread through the blood and lymph. This is possible in the presence of other infectious diseases. Pyelonephritis in pregnant women occurs when the kidney tissue is compressed by the enlarged uterus.
Less commonly, the disease is caused by viruses and fungi. Infection is possible during catheterization. Pyelonephritis often develops in women who do not follow the rules of intimate hygiene, drink little, have STIs and endocrine diseases. The risk group includes women 18–30 years old who have never given birth before.
Pathogenesis of disease development
Inflammation of the kidneys like pyelonephritis has a complex mechanism. The basis is a violation of urodynamics (normal urine flow). This is facilitated by compression and hormonal factors. At the beginning of pregnancy, the body undergoes restructuring. The ratio of estrogen and progesterone changes.
The latter acts on the adrenergic receptors of the upper urinary organs. This leads to hypotension. The consequence is stagnation of urine. On days 7–13, estradiol production increases. It disrupts alpha receptor activity. In the later stages of gestation, the main link in the pathogenesis of the development of pyelonephritis is compression of the kidney tissue by the uterus. The following factors play an important role:
- hereditary predisposition;
- decreased immune status;
- Vesicoureteral reflux.
During pregnancy, lymphocyte activity decreases. Initially, bacteriuria develops, which, if left untreated, leads to kidney damage. The disease is more often detected in women with cephalic presentation of the fetus. If there is right ovarian vein syndrome, then compression of the middle third of the right ureter occurs. In this case, acute pyelonephritis develops.
Signs of pyelonephritis in pregnant women
The disease most often begins acutely. With pyelonephritis before the 12th week of pregnancy, the following symptoms are observed:
- fever;
- increased sweating;
- chills;
- tachycardia;
- adynamia;
- weakness;
- unilateral or bilateral lower back pain;
- strangury;
- feeling of bladder fullness.
Very often, kidney inflammation is combined with cystitis and urethritis. Pain with gestational pyelonephritis is one-sided. Only sometimes both kidneys are involved in the process. The pain radiates to the genitals, groin area and upper abdomen. It varies in intensity. Infection always provokes the appearance of symptoms of intoxication.
The purulent-destructive form of the disease occurs most rapidly. It is characterized by hectic fever. The temperature rises after a certain time. Tapping along the edge of the costal arch reveals a positive Pasternatsky sign. Sometimes nausea and vomiting occur. Women's appetite worsens.
Urine takes on a reddish tint. This sign is not always observed. It indicates the appearance of blood in the urine. Urine becomes cloudy. When pyelonephritis is combined with cystitis, mictions become frequent. Pubic pain may occur. The chronic form of the disease is asymptomatic or with a poor clinical picture.
Danger of pyelonephritis for the fetus
Not everyone knows what effect this disease has on the fetus. Advanced pyelonephritis can cause sepsis. This is a dangerous complication in which bacteria and their toxins spread and affect all organs and systems. Microbes penetrate the placental barrier and can cause miscarriage.
Other negative consequences include intrauterine infection and premature birth. The most dangerous complication is infectious-toxic shock. It develops very rarely. Preeclampsia may be the cause of a developmental disorder in the baby. This is a complication of pregnancy, characterized by edema, high blood pressure and proteinuria. Children born to mothers with pyelonephritis may be weak and premature.
Types of pathology
Gestational pyelonephritis is classified according to several criteria, including:
- Pathogenesis;
- The nature of the current;
- Stage of development;
- Impact area;
- Preservation of functionality.
The condition of the kidneys in pregnant women is of great importance; women who have both kidneys affected are most at risk. Tubulointerstitial nephritis can be primary or secondary. The appearance of the latter is explained by a relapse of a disease that the patient had previously suffered from. Acute pyelonephritis in pregnant women can become chronic. In this case, the functionality of parenchymal organs suffers. Chronic pyelonephritis, worsened during pregnancy, provokes disturbances in the filtration mechanism.
Gestational
Gestational pyelonephritis can appear during pregnancy and after childbirth. According to statistics, in 10% of all patients, this pathology is accompanied by the development of purulent-destructive foci. The cause of their occurrence is carbuncles, abscesses and apostemes. The acute type of gestational pyelonephritis occupies second position in the list of the most common extragenital diseases. Women who become pregnant for the first time are at risk. Among the factors predisposing to gestational damage to parenchymal organs are hormonal and immunological changes in the body.
Tubulointerstitial nephritis most often develops in the second or third trimester of pregnancy. At 34-36 weeks, the risk of developing pathology reaches a critical level. In some cases, gestational kidney damage manifests itself during or immediately after childbirth (4-12 days). The sooner treatment is started, the fewer consequences. Pyelonephritis during pregnancy affects the fetus, so if alarming signs appear, you should visit a doctor.
Chronic
During pregnancy and the postpartum period, chronic pyelonephritis of two types can occur. The primary develops secretly. The acute phase proceeds without visible manifestations, the transition to the next stage is also not burdened by external symptoms. After the first signs appear, chronic tubulointerstitial nephritis is diagnosed.
Treatment of chronic pyelonephritis of the second type is complicated by urolithiasis, urethritis, developmental abnormalities or cystitis. These disorders are the root cause of the pathology, which is most dangerous for a woman expecting a child. The primary exacerbation of a chronic disease is characterized by the rapid onset of symptoms of infectious infection; the secondary exacerbation can slowly progress over several years. An obstructive disease is much more difficult to cure than its non-obstructive variety. The situation is aggravated by excessive stress on the kidneys and decreased immunity.
Spicy
The development of acute pyelonephritis during pregnancy is fraught with the appearance of symptoms such as:
- Change in urine color;
- Increased body temperature;
- Dyspeptic disorder;
- Unpleasant odor;
- Pain that occurs with sudden movements and physical activity.
This type of pathology is a form of secondary obstructive pyelonephritis. Clinical manifestations occur suddenly. Due to hormonal imbalance, the tone of the urinary tract changes. The result of such an effect is a violation of the outflow of urine.
Main causes
Pyelonephritis is an inflammatory disease that occurs when a pathogen enters the kidney tissue. The most common routes of infection are:
- through blood;
- through lymphatic vessels;
- with a stream of urine.
Predisposing factors include:
- acclimatization;
- sudden changes in ambient temperature;
- cooling;
- frequent ARVI and influenza;
- passive lifestyle;
- bad habits;
- poor nutrition;
- genetic predisposition;
- changes during pregnancy in the genitourinary system;
- traumatic kidney damage;
- work in hazardous production.
Pyelonephritis is not a disease that disrupts the processes of conception. Many women were able to get pregnant after successful treatment and bear healthy children without problems for their own health.
Diagnostics
Gestational pyelonephritis in pregnant women is diagnosed through instrumental and laboratory tests. An examination is necessary to identify the exact cause of the malaise. Urine and blood tests, which a woman takes in the first and second trimester of pregnancy, allow acute and chronic pyelonephritis to be identified in a timely manner.
The patient is prescribed OAC, OAM, biochemical blood test, urine test according to Zimnitsky and Nechiporenko, and bacteriological culture. Among the hardware diagnostic methods include ultrasound, chromocystoscopy, and catheterization of the urinary tract.
Your doctor will help you get rid of the root cause of the disease and relieve its symptoms. The effectiveness of therapy is checked through control tests. X-rays, excretory urography, as well as other radioisotope research methods are strictly prohibited during pregnancy.
What tests need to be taken
X-ray examinations are not performed during pregnancy to avoid radiation exposure to the body of the expectant mother and child. When making a diagnosis, the results of the following examinations are taken into account:
- general clinical blood test;
- general urine analysis;
- Ultrasound of the kidneys;
- urine culture for microflora;
- blood chemistry.
To prevent vertical spread of infection, cystoscopy and urinary catheterization are not performed.
If the clinical picture is unclear, a Zimnitsky test is additionally performed, which evaluates the functional state of the kidneys. If necessary, consult with an infectious disease specialist or hepatologist.
Treatment
Gestational pyelonephritis is treated in an inpatient setting. At the first stage, the passage of urine is restored. For this, positional therapy is prescribed:
- The woman lies on her side (on the side where the healthy kidney is located);
- Takes a knee-elbow position;
- The end of the bed is raised.
As a result of these manipulations, the pressure of the uterus on the parenchymal organs decreases, the outflow of urine occurs normally, and the patient’s condition improves. If there are no positive results after such therapy, catheterization or puncture nephrostomy is performed. Treatment of pyelonephritis during pregnancy is carried out with the help of drug therapy, physiotherapy and homeopathy. As a last resort, surgery is used. The sooner treatment begins, the greater the chance of a favorable outcome. Kidney damage in the 1st or 2nd trimester can lead to missed abortion. Ignoring the doctor’s clinical recommendations can lead to acute renal failure.
Medicines
If pyelonephritis is detected during pregnancy, the selection of medications is based on the diagnosis, the individual characteristics of the patient and the trimester. Antibiotics can not only get rid of pathology, but also harm the child. The safest drugs include:
- Ampicillin;
- Erythromycin;
- Oxacillin;
- Netilmicin;
- Tseporin;
- Suprax.
The prescribed dosage regimen and dosage cannot be changed. Increasing the duration of drug therapy is harmful to the fetus. Antibiotic drugs are prescribed only after laboratory tests. Infusion medicinal formulations, antispasmodics, vitamin-mineral complexes, and sedatives have a good effect.
When treating a woman during lactation, caution should also be exercised. All drugs that enter the mother's body pass into breast milk. Only the doctor decides how to treat a woman. Selecting medications on your own is strictly prohibited.
Surgery
If inflammation of the pyelocaliceal system is accompanied by suppuration, surgery is performed. How to treat purulent-destructive changes localized in several segments of a parenchymal organ is decided after a full diagnostic examination. To get rid of the clinical manifestations of the pathology, nephrostomy, kidney decapsulation and nephrectomy are performed. The latter is necessary if pyelonephritis worsens or severe intoxication is added to other symptoms of the disease.
Indications for surgical intervention may be:
- Lack of positive results from conservative therapy;
- The appearance of an abscess, apostematous nephritis and carbuncle.
To avoid having to undergo surgery, you must follow all the doctor’s recommendations.
Plasmapheresis
This extracorporeal detoxification method is used to treat complicated kidney pathologies during pregnancy. Pregnant women have no contraindications to its use. Additional advantages of this method include simplicity, absence of adverse reactions and effectiveness.
Thanks to this method, you can get rid of problems with humoral and cellular immunity; reduce body temperature; remove intoxication; improve the patient's general condition. Plasmapheresis is usually performed before surgery. The positive effect of this procedure reduces the risk of complications.
Physiotherapy
Complex therapy prescribed when foci of inflammation are identified often includes ultraviolet radiation of autologous blood, electrophoresis, SMV therapy, and UHF. This treatment tactic helps alleviate the patient’s condition. The use of these physiotherapy procedures occurs over a certain period of time. A positive result can be obtained only after completing the full course.
Diet
Diet is an integral part of therapy prescribed for pyelonephritis in pregnant women. Pickles, marinades, smoked and fried foods must be excluded from the diet. It is necessary to increase the amount of vegetables and fruits consumed, and monitor the amount of fluid in the body. Excesses negatively affect the condition of parenchymal organs.
The diet menu is supplemented with compotes, diuretic tea, fruit drinks, and juices. You need to eat fractionally, that is, the number of meals increases, and the portion decreases. The basis is products that prevent constipation and other gastrointestinal disorders. First courses must be vegetarian. Meat and fish should be introduced into the diet with caution. Before doing this, it is advisable to consult with your doctor.
Folk remedies
During pregnancy and breastfeeding, it is not recommended to take herbal medicines that are not approved by the doctor. Treatment at home should occur under the supervision of a specialist. The body of the expectant mother is vulnerable; everything she consumes affects the fetus.
Folk remedies that you can drink while in an interesting situation are prepared from:
- Lingonberries;
- Motherwort;
- Honey (if there is no allergy);
- Parsley;
- Sea buckthorn.
There are many options, the main thing is to follow the recommended proportions and dosage regimen.
Treatment of pyelonephritis in pregnant women
Elimination of infection and restoration of urination are the main tasks of treating pyelonephritis in pregnant patients. Medicines are selected taking into account the sensitivity of bacteria and the trimester of pregnancy.
Antibiotics
In early pregnancy, bacterial infections are treated with protected penicillins. Low-toxic antibiotics do not affect the intrauterine development of the fetus. In the first trimester of gestation the following are used:
- Augmentin;
- Amoxi-apo-clav;
- Klavam;
- Betaclave;
- Theraclave.
Starting from the fourth month of pregnancy, it is allowed to use macrolides and cephalosporins:
- Spiramycin;
- Cefotaxime;
- Abithrax;
- Ceftriaxone;
- Loraxim.
Fluoroquinolone antibiotics are not used during pregnancy. Sulfonamides should not be used in the first and last trimesters.
Auxiliary medications
To relieve the symptoms of pyelonephritis, strengthen the immune system and eliminate intoxication, the following are used:
- analgesics (Bofen, Nurofen) – relieve renal colic, discomfort in the lower back;
- uroseptics (Fitolysin, Canephron) – destroy infection in the urinary tract, prevent cystitis and urethritis;
- antispasmodics (Spazoverin, No-Shpa) - relax smooth muscles, preventing increased uterine tone and premature birth;
- vitamins (Elevit Pronatal, Pregnavit) – replenish the deficiency of bioactive substances, stimulate the body to fight infection.
Before treating pyelonephritis with medications, consult an obstetrician-gynecologist or nephrologist. Irrational therapy is fraught with disturbances in fetal development.
Diet and drink
A diet is prescribed in conjunction with drug therapy. In the first and second trimester you need to eat more fortified fruits and vegetables:
- gooseberry;
- currants;
- cucumbers;
- carrot;
- melon;
- beets;
- pears;
- apples;
- watermelons;
- grape.
Vinegar, spices and fatty foods are excluded from the diet. In the last trimester, fermented milk products, fruit drinks and compotes are recommended. To reduce swelling and the severity of hypertension, avoid table salt.
Bed rest
Pyelonephritis in pregnant women occurs in severe form. To prevent complications and improve well-being, patients should adhere to bed rest:
- in case of kidney inflammation, complete rest for 7 days is indicated;
- to avoid fluid stagnation, sleep on the healthy side;
- To prevent swelling, place a pillow under your feet.
In a horizontal position, blood circulation in the pelvic organs is restored, which promotes recovery.
When is surgery necessary?
Surgery is required for purulent inflammation of the renal parenchyma and the formation of carbuncles. During pregnancy, preference is given to organ-preserving operations:
- kidney decapsulation - removal of the outer shell of the organ in order to reduce pressure on the inflamed parenchyma;
- abscess drainage - opening the abscess with subsequent removal of purulent contents from the lesion.
If pyelonephritis is severe and threatens termination of pregnancy, nephrectomy is resorted to - removal of the affected kidney.
Prevention
What can be done to prevent inflammation of the calyces and pelvis of the kidney in women who are expecting a baby? The disease is prevented through a healthy lifestyle, strengthening the immune system, proper nutrition, and regular physical activity. You should also pay attention to your drinking regime.
Excessive amounts of fluid negatively affect the patient's condition. Changes in immunity can be triggered by hypothermia and other negative external factors. Prevention of pyelonephritis during pregnancy is especially necessary if the woman has already suffered from this pathology.
What medications can the doctor prescribe?
Therapy for gestational pyelonephritis includes antibacterial and anti-inflammatory treatment. The use of many antibiotics and some uroseptics during pregnancy is strictly contraindicated, which significantly complicates the choice of medications. In any case, the tactics to combat this disease are chosen by the doctor in the hospital, since all women with this diagnosis are required to be hospitalized.
In the first trimester, the so-called barrier function of the placenta is usually not fully formed. At this time, an important stage in the formation of the child’s main organ systems occurs, so drug exposure is undesirable. If changes are detected only in urine tests, most likely, you will be able to limit yourself to the above recommendations. In case of active inflammation, which is accompanied by fever and pain, the use of penicillins (drugs Amoxicillin, Amoxiclav) is allowed.
From the second trimester, it is allowed to take antibiotics of the cephalosporin group (Suprax, Cefazolin), macrolides (Vilprafen, Sumamed). From the fifth month (with an active inflammatory process), Gentamicin is used strictly as prescribed by the doctor.
Treatment of gestational pyelonephritis also involves detoxification therapy, the use of vitamin complexes and sedatives. Particular attention is paid to the prevention of fetal hypoxia. In case of urgent need, urine flow is restored through catheterization and stenting of the ureter.
What are the dangers during pregnancy?
Why is pyelonephritis dangerous during pregnancy and breastfeeding? Advanced kidney inflammation is fraught with serious consequences for the expectant mother and baby. Ignoring symptoms often leads to intrauterine fetal death and spontaneous abortion.
During an exacerbation, the woman herself may suffer from severe intoxication, purulent-necrotic damage to parenchymal organs, arterial hypertension, and sepsis. The risk of premature birth increases. In some cases, termination of pregnancy is prescribed. It is performed due to fetal hypoxia or severe gestosis. The latter pathology is dealt with within 2 weeks.
Forecasts and long-term consequences
The danger of pyelonephritis lies not only in the discomfort it causes, but also in the long-term consequences. They can negatively affect both the health of the mother and the unborn baby. That is why the country's leading obstetricians and gynecologists advise getting rid of the disease before planning a pregnancy. It is advisable to take a course of preventive measures and completely change your lifestyle six months before conceiving a child. This way you can avoid an unexpected relapse of the disease and completely protect yourself and your baby from the action of pathogenic microorganisms that can enter the fetus’s body through the bloodstream.
Consequences for women
Pyelonephritis is a disease that can cause kidney failure in a completely healthy person. The body of a pregnant woman is a rather vulnerable target for various types of infections. When the first signs of pyelonephritis appear, you should go to the hospital, because if surgical intervention is necessary, you will need to undergo many examinations, as well as choose a method for quickly solving the problem.
The formation of purulent foci is often found in pyelonephritis
The main complications of pyelonephritis in pregnant women:
- small pustular formations in the kidney tissue;
- carbuncles and perinephric phlegmon;
- purulent melting of the tissue of the pelvic organs;
- gestosis and toxicosis;
- hypertensive crisis;
- edema syndrome;
- infectious-toxic shock;
- septic intoxication of the body;
- acute renal failure;
- miscarriage;
- premature birth.
Threat to baby
The child remains in the mother's body throughout the entire period of intrauterine development. Accordingly, everything that happens to a woman affects her baby in one way or another. The consequences of the disease are very dangerous: systems and organs are underdeveloped, the child does not gain weight, and at birth cannot breathe on his own. Most often the cardiovascular and bronchopulmonary systems and the brain are affected. Such children must be kept in the neonatal intensive care unit for a long time.
In intensive care, the child’s condition can be stabilized
The main consequences of pyelonephritis during pregnancy for the fetus:
- hypoxia: lack of oxygen negatively affects the formation of the nervous system;
- growth retardation: due to insufficient tissue nutrition, the child grows much slower than the established norm;
- yellowness of the skin: yellow-orange color of the skin and mucous membranes indicates disturbances in the hematopoietic system;
- infection of amniotic fluid: leads to infection of the child with pathogenic microorganisms;
- premature birth with a long anhydrous period: broken water no longer creates a favorable environment for the baby;
- intrauterine fetal death.
Jaundice of newborns is a common consequence of pyelonephritis
Management of pregnancy and childbirth with pyelonephritis
The diagnosis of pyelonephritis during pregnancy is not a death sentence. If you take medications correctly and in a timely manner, it is possible to recover or enter remission in a few weeks. Physiotherapy also helps improve the functioning of the genitourinary system. The expectant mother should regularly undergo the following tests at the clinic:
- general blood and urine tests;
- bacterioscopic stool culture;
- biochemical urine analysis;
- bacterioscopic urine culture.
In uncomplicated pregnancy with mild pyelonephritis, women can give birth on their own and carry the fetus to term. If the condition of the expectant mother rapidly deteriorates, it is possible to induce premature labor within the acceptable period by stimulating the uterus with oxytocin injections. Caesarean section for pyelonephritis is performed only in emergency cases of acute renal failure, since there is a high risk of intrauterine infection of the fetus during abdominal surgery.
Caesarean section for pyelonephritis is practically not used
Hospitalization during early and late pregnancy
Chronic pyelonephritis detected in early pregnancy is not a reason for hospitalization. They may insist on hospitalization if a urine test and the woman’s general condition indicate an exacerbation of the pathology. The malaise lasts for 1-3 weeks.
In any case, the patient will have to follow the correct lifestyle and the prescribed diet. This is necessary to prevent further progression of the disease. In later stages, bed rest is prescribed only during the acute phase. During the period of remission, the expectant mother should be active. Physical inactivity can worsen her situation; the risks are already quite high.
Preventive actions
To prevent the development of gestational pyelonephritis, it is extremely important for expectant mothers to include several points in their daily routine:
- Moderate physical activity. Doctors recommend taking short walks (about 1 hour) every day.
- Special gymnastics for pregnant women. Today, many sports centers conduct classes for women in position, thanks to which the back muscles are strengthened and the tone of all internal organ systems is improved.
- If you have a history of diseases of the urinary system, you must follow a special diet that promotes the outflow of urine.
- It is recommended to drink plenty of fluids per day.
- You should empty your bladder at least every three to four hours.
Paying attention to your own health and preventing gestational pyelonephritis is the key to giving birth to a strong baby. Such an insidious disease should not be neglected. If primary symptoms appear, it is better to consult a doctor and take all necessary measures to eliminate the pathology. Be healthy!
Sources:
https://studfiles.net/preview/1563572/ https://yandex.ru/health/turbo/articles?id=2463 https://fb.ru/article/201069/gestatsionnyiy-pielonefrit-pri-beremennosti-lechenie -gestationnogo-pielonefrita
Childbirth
Pathological changes in the kidneys do not affect conception. A woman can get pregnant if she has no problems with the reproductive system. Childbirth with pyelonephritis does not always take place by caesarean section. This diagnosis cannot be considered an indication for surgery.
In this case, everything depends on the general condition of the woman in labor, the physiological parameters of the fetus and the stage of the pathology. The decision regarding this issue is made by the doctor. Immediately after childbirth, the disease can enter the acute phase. The likelihood of such a phenomenon is extremely high in chronic pyelonephritis, even 14 days after the birth of the child. Clinical manifestations are similar to those of appendicitis, endometritis, sepsis and perimetritis.
Types of kidney inflammation
Pyelonephritis in pregnant women is classified according to different criteria - clinical manifestations, mechanism and period of onset. An accurate diagnosis makes it easier to choose treatment tactics and predict the further course of the disease.
During pregnancy, in 76% of women, foci of infection occur in the right kidney. Much less often, gestational pyelonephritis is left-sided or bilateral.
Nephrologists and obstetricians-gynecologists distinguish the following types of pyelonephritis:
- According to the course – acute and sluggish (chronic). The acute form occurs in 10% of women during primary pregnancy. It is characterized by a rapid course with severe pain. Sluggish pyelonephritis occurs against the background of acute. During periods of remission, it has almost no effect on a woman’s quality of life.
- By origin – primary and secondary. Pyelonephritis is called primary if the infection of the kidneys was not caused by external or internal factors. Secondary occurs against the background of urogenital infections, anatomical defects, and narrowing of the urinary tract.
- By period – relapses, partial or complete remission. During exacerbation, the symptoms are pronounced. With partial subsidence of symptoms, patients feel satisfactory, and with complete subsidence, laboratory signs of pyelonephritis are not detected.
According to the nature of the pathological changes, pyelonephritis can be serous, purulent, widespread (diffuse) and apostematous, when multiple ulcers appear in the renal parenchyma.
Consequences for the child
Pyelonephritis after childbirth can provoke purulent-septic complications, which can be fatal. Infection during fetal development can cause conjunctivitis or diseases of the internal organs. The outcome is impossible to predict. The consequences for the child may be irreversible. Therefore, doctors insist on early registration in antenatal clinics. Regular monitoring of the fetus’s condition is a real opportunity to save its life if any disturbances occur.
Main symptoms
The onset of gestational pyelonephritis is almost always sudden (with the exception of an erased prodromal period in the case of chronic cystitis or bacteriuria before pregnancy). Characteristic signs of the onset of the disease are:
- high body temperature up to 38–39 degrees and above;
- pain in the lumbar region;
- dysuria (impaired urination);
- change in urine color.
General weakness, nausea and other manifestations of intoxication of the body may also appear.
Regime and diet
Losing time during gestational pyelonephritis can be fraught with complications; urgent hospitalization, adequate examination and selection of the correct regimen are necessary. Depending on the severity of the disease, bed rest or strict bed rest is prescribed. You need to drink enough liquid to enhance urine flow and cleanse (cranberry juice, lingonberry tea, etc.). You can focus on the color of the urine - the more transparent it is, the better.
It is recommended to limit or completely eliminate table salt, especially if the disease occurs with hypertension. Do not consume coffee, spicy foods, marinades, or vinegar. Lactic acid products are useful - yogurt, kefir, as well as fruits and vegetables.
Development mechanism
Pyelonephritis is a nonspecific inflammatory process of bacterial etiology, characterized by damage to the renal tubules. If the pathology develops during pregnancy, then doctors use the term “gestational pyelonephritis.” The disease occurs against the background of damage to the renal pelvis, calyces and interstitial parenchyma tissue.
Pyelonephritis during pregnancy occurs when there is an infectious focus in a woman’s body (mainly in the urinary system), as well as as a result of disturbances in the outflow of urine through the urinary tract. Pathogenic microorganisms that penetrate the bloodstream from the environment act as agents of inflammation. These include:
- coli;
- enterococci;
- Pseudomonas aeruginosa;
- proteas;
- staphylococci.
Pyelonephritis in pregnant women is provoked by Escherichia coli and Proteus due to the anatomical proximity and general circulatory system of the urinary system, genitals and intestines. High resistance of the body to infectious pathogens will prevent the disease. With a low immune status, the likelihood of the formation of an inflammatory focus is extremely high.
Bacteria that have already been exposed to T-lymphocytes and leukocytes are especially dangerous. They have lost part of the cell wall, but have acquired resistance to external factors. Such microorganisms, when favorable conditions arise, form full-fledged strains. Pyelonephritis in early pregnancy most often develops after the emergence of several stable colonies of vegetative forms of microbes.
The main symptom of pyelonephritis during pregnancy is lower back pain
General information
Pyelonephritis is an inflammatory process in the kidney that develops as a result of infection.
Pregnant women are more predisposed to this disease due to poor urine flow and compression of the drainage canal by the growing uterus. Pyelonephritis is manifested by a sharp increase in temperature and painful discomfort in the lumbar region. To fight the infection, doctors usually recommend antibiotic therapy. With proper treatment, the expectant mother has every chance of giving birth to a healthy baby. What is the difference between gestational pyelonephritis? During pregnancy, the uterus, which grows every day, puts pressure on surrounding organs. Very often the ureter itself is compressed. This is the channel through which urine flows from the kidney directly to the bladder. Slowing down the process provokes stagnation and expansion of the kidney.
If the expectant mother was diagnosed with chronic pyelonephritis before pregnancy, and now has developed gestational pyelonephritis, the risk of complications is quite high. Such women should be constantly monitored by a doctor and strictly follow all his instructions.
What is the cause of pyelonephritis
Urologists believe that sitting on a cold stone or wet feet cannot cause pyelonephritis; this disease is always caused by microorganisms that normally live in the human body. They are called opportunistic.
In 90% of cases, the culprit is a group of enterobacteria. These are bacteria such as Escherichia coli (E. Coli), Klebsiella, Protea. The kidneys themselves are sterile. However, infectious agents can be introduced through the blood (hematogenous route) or through the ureters through the urethra (ascending route). There are, although rare, chlamydial, ureaplasma and viral pyelonephritis.
What harms urological health:
- frequent cystitis or acute pyelonephritis before pregnancy;
- hypothermia;
- bacteria in urine before or during pregnancy;
- diabetes;
- hereditary kidney diseases;
- kidney development abnormalities;
- inflammation of a single kidney;
- chronic pyelonephritis during pregnancy.
Causes of kidney inflammation during gestation
Here are the main factors for the development of inflammation in a pregnant woman:
- The growing uterus puts pressure on the ureters—urine passage is disrupted.
- A constant, sluggish inflammatory process - caries, tonsillitis - can contribute to the spread of infection in the genitourinary tract.
- Elevated levels of progesterone relax the smooth muscles of the ureters and bladder, impairing the movement of urine, promoting infection to the kidneys.
- The presence of even small kidney stones makes it easier for the infection to spread.
- Urinary reflux, due to tortuosity of the ureters or other causes, promotes the spread of bacteria from the lower third of the urethra into the kidney tissue.
As a result, inflammation of the kidney leads to sclerosis of the interstitial tissue and compression of the tubules. This is manifested by a deterioration in urine concentration function. Due to tissue sclerosis, renal arterial hypertension may develop. It occurs in 20% of women who have had pyelonephritis during pregnancy.
Of course, inflammation of the kidneys during pregnancy worsens its course, and the well-being of both the woman and the fetus suffers. The urologist and gynecologist pay due attention not only to the health of the expectant mother, but also to the baby in the womb. To check its condition, fetal CTG, ultrasound and Doppler ultrasound are performed.
How are urinary tract infections treated during pregnancy?
Kidney inflammation, as prescribed by a doctor, can be treated with antibiotics during pregnancy. Usually a 7-10 day course of antibiotics is prescribed, which is safe for you and the baby. Pyelonephritis is treated by a urologist or an obstetrician-gynecologist who manages the pregnancy. Let's talk in more detail about how to treat such inflammation.
Basic principles of therapy for exacerbation of gestational pyelonephritis:
- Timely therapy, first with a broad-spectrum antibiotic, then prescribing the drug based on the results of culture of the material.
- The use of herbal medicines - herbal based, kidney preparations.
- Restoring normal urine flow in the ureters.
- Monitoring the course of pregnancy, fetal well-being, correction of anemia.
- Drinking regimen: 1.5-2 l. water per day.
- The first 48 hours are parenteral administration of drugs, the following days are a transition to the oral route.
The harm of gestational pyelonephritis is greater than the harm of antibiotic therapy.
Features of the use of antibiotics in pregnant women
- In the first trimester of pregnancy, organogenesis occurs, that is, the formation of tissues and organs. During this period, only penicillins are safe. The use of other antibiotics can lead to various developmental defects, such as deafness.
- In the second and third trimesters of pregnancy, fetal organogenesis is completed, the placenta functions, protecting the fetus from many medications. The range of antibacterial drugs is expanding: semi-synthetic penicillins, cephalosporins, macrolides are being added, and, if necessary, nitrofurans. For example, E. coli is most sensitive to them.
- Fluoroquinolones are allowed in the postpartum period. At the same time, breastfeeding is prohibited during the period of antibacterial therapy. Treatment lasts 7–10 days. In the first 2 days, the method of administration of the drug is intramuscular, after which it is replaced with tablets.
The Russian Society of Urology considers the following antibiotics optimal.
Antibacterial drugs of choice:
- Amoxicillin/Clavulanate (1.2 g IV) (protected).
- Ampicillin (0.5–1.0 g IM, IV).
- Carbenicillin (1.0 g IM).
- Cephalosporins of various generations (1.0 g intravenously).
Pyelonephritis in pregnant women: causes, symptoms and treatment
Pyelonephritis is an inflammatory process that occurs as a result of infection in the kidneys. The most common pathogens are Escherichia coli, Staphylococcus, Enterococcus, and Proteus.
Sometimes on the card, instead of a diagnosis, the doctor writes down a disease code, which is taken from the International Classification of Diseases, Tenth Revision.
ICD-10 code for gestational pyelonephritis: O23.0 Kidney infection during pregnancy
What is gestational pyelonephritis?
It is called gestational when the cause is pregnancy. During the entire gestation period, the size of the uterus continuously increases, putting excessive pressure on the ureters (especially the right one), as a result of which the upper urinary tract (renal pelvis and ureters) expands.
The pathological process of dilation begins in the second half of gestation, reaching a peak in the first weeks of the third trimester, and stopping soon after birth.
Under the influence of pregnancy hormones (progesterone and hCG), in addition to the expansion of the renal pelvis and ureter, the motor ability of the urinary tract deteriorates, causing the outflow of urine (urine) to be disrupted.
Stagnant urine is a favorable environment for infection to enter and multiply in the urinary tract.
Paths of penetration of pathogenic microbes:
- hematogenous route (due to bacteremia) . If there is a focus of infection in any part of the body, pathogenic bacteria penetrate into the bloodstream. Bacteria travel through the blood throughout the body and, once in suitable conditions, begin to multiply.
- ascending tract (through the urinary tract) . From an infected urethra or bladder (with urethritis, cystitis), pathogenic microorganisms move up the urinary system, affecting the renal pelvis. Thus, untreated cystitis can cause the development of this disease.
If there is a focus of infection in the vagina (for example, with vaginitis), over time, bacteria are transferred from the vagina to the urethra, urethritis occurs, which can develop into pyelonephritis.
The risk of developing the disease increases if, before or during pregnancy, a woman had cystitis, asymptomatic bacteriuria, impaired urine outflow or other problems with the urinary system.
If you walk barefoot on a cold floor, sit on a cold floor, or swim in cold water, you will catch a cold!
Let's dispel the myth! The nature of colds is infectious. Opportunistic bacteria can be present in the human body in small quantities without causing any disease. And as soon as immunity decreases, pathogenic microorganisms begin to multiply at high speed.
Hypothermia causes a decrease in the body's defenses, as a result of which the human immune system is not able to overcome pathogens. Thus, cold itself cannot cause inflammation! This is why medicine recommends hardening the body.
How does the disease manifest itself?
Gestational pyelonephritis during pregnancy manifests itself differently depending on the form of the disease. There are acute and chronic forms of the disease.
Primiparous women are first overcome by acute gestational pyelonephritis at 4-5 months, and multiparous women at 6-8 months.
The chronic form of the disease is the most common: it appears even before conception, is practically asymptomatic for the woman, and during pregnancy a relapse occurs due to pregnancy.
Often gestational pyelonephritis in pregnant women (chronic, not acute) is confused with influenza or acute respiratory infections, because symptoms erased.
First, the disease manifests itself as a syndrome of general intoxication of the body (temperature rises slightly, fever, headache, body aches are observed). As a result, antiviral drugs relieve symptoms, and the disease continues to progress hidden.
During exacerbation of the chronic form
- in the first trimester, dull, aching pain occurs in the lumbar region, radiating to the perineum; body temperature rises (up to 37.9 °C). The woman takes a position “lying on her side”, bending her knees, pressing them to her stomach. This body position relieves pain.
- in the second and third trimesters, the disease is characterized by dull lumbar pain in combination with a mild headache, a slight increase in body temperature (up to 37.9 ° C), loss of appetite, weakness, fatigue, and disruption of the urinary process. A pregnant woman may complain of pain when urinating, incomplete emptying of the bladder, or difficulty urinating.
The disease is sometimes aggravated by increased blood pressure.
Acute gestational pyelonephritis is characterized by:
- the presence of severe pain in the lumbar region, radiating to the groin or thigh;
- sudden increase in body temperature (about 38-39 °C);
- malaise, chills, sweating;
- feeling of discomfort when urinating.
Why is gestational pyelonephritis dangerous?
- The presence of a chronic form of the disease and urinary tract infection in a pregnant woman increases the risk of intrauterine infection of the fetus, and for the mother, the disease carries the risk of infectious-toxic shock and the development of sepsis.
- Pain in the affected organ, fever and toxic waste products of infectious agents increase the excitability of the uterus, which increases the risk of spontaneous abortion.
- The infection has a negative impact on the child.
The baby is at risk of hypoxia, developmental delay, underweight, and breathing problems. - Gestational pyelonephritis during pregnancy provokes the appearance of gestosis, and their combination in 90% of cases is complicated by edema and increased blood pressure.
- The presence of inflammation increases the incidence of chronic fetoplacental insufficiency and premature birth.
Taking the necessary antibiotics in a timely manner can reduce the risk of premature birth from 50 to 5%. - Often, gestational pyelonephritis during pregnancy is accompanied by anemia, which complicates pregnancy, childbirth and the postpartum period.
Treatment tactics for pyelonephritis during pregnancy
1. Determination of the type of infectious agent and its sensitivity to antibiotics of various groups, by submitting urine for analysis for bacterial culture.
According to the results obtained, the pregnant woman is prescribed antibiotics that do not provoke the development of severe birth defects in the baby. Therapeutic course - up to 14 days.
A woman carrying a child needs to remember the following: whether she wants it or not, the inflammation must be treated! Let expectant mothers not be scared by the word “antibiotic”, because infection causes much more significant harm to the baby than this drug.
Antispasmodics are also prescribed to relieve pain, combined anti-inflammatory and antimicrobial agents, for example, the drug Canephron N.
It is recommended to take Phytolysin. It helps remove bacteria from the source of their reproduction, relieves inflammation, and improves the excretion of urine from the body. The drug is made on a natural basis and is approved for use during pregnancy.
As a complex therapy, pregnant women are often prescribed Cyston tablets. They have antispasmodic, bactericidal, anti-inflammatory effects, and also provide a mild diuretic effect.
Until the culture results are obtained, the pregnant woman may be prescribed broad-spectrum antibiotics (for example, Ampicillin, Amoxicillin, Ceftriaxone, Erythromycin, Spiramycin).
If taking antibiotics does not give the desired result, then alternative treatment is carried out using bacteriophages. Bacteriophages are “good” viruses that destroy a certain type of pathogenic bacteria. Depending on the type of pathogen, streptococcal, staphylococcal, coli, Proteus, Klebsiella bacteriophages, etc. are distinguished.
Bacteriophages are taken orally (swallowed) or introduced through a catheter or drain into the kidney.
2. Observance of strict bed rest.
In case of unilateral damage, sleep should be exclusively on the “healthy” side!
3. Drink plenty of non-carbonated water of low mineralization (it is advisable to drink a glass of water on an empty stomach), cranberry juice. Taking diuretics, for example, kidney tea or Brusniver collection.
In summer, it is recommended to eat ripe watermelons and melons. Black currants (if you are not allergic to vitamin C), peach, grapes, and pear are also useful. And a fresh cucumber should be the main ingredient in a salad for lunch.
4. Adhere to a therapeutic diet. During an exacerbation of the disease, you should eat food without salt, and hot, spicy, pickled and fried foods should be completely excluded from the menu.
Drinking coffee is not recommended! Chicory is a useful alternative.
5. Adopting the knee-elbow position for 15-20 minutes 3-5 times a day. This position helps improve the outflow of urine when urinating is difficult.
Throughout treatment, the child’s condition should be carefully monitored for early detection of possible hypoxia and delay in its development.
In case of repeated pyelonephritis, a catheter is inserted into the ureter through the urethra to drain urine, and antibacterial therapy is prescribed.
Surgical intervention is necessary only if taking medications does not produce the expected results or the inflammation is aggravated by a purulent process in combination with the destruction of kidney cells. In severe cases, due to the lack of proper treatment, the disease can cause kidney failure, the development of a kidney abscess, and threaten the woman with death.
Qualified medical care will help you avoid negative consequences. If hospitalization is offered, you should not refuse!
After treatment, it is necessary to submit urine for general analysis once every 2 weeks until the end of gestation, and monthly for bacterial culture. The probability of re-exacerbation of the disease before childbirth is about 20%.
Disease prevention
A pregnant woman should have her urine tested at every scheduled visit to the gynecologist, because prevention of the disease comes down to the timely detection of asymptomatic bacteriuria.
Is it possible to avoid exacerbation of pyelonephritis during pregnancy? To prevent remission of the chronic form of the disease, from the end of the first trimester you should take urological herbal medicines, for example, Canephron N, Brusniver collection, and systematically perform exercises to improve the functioning of the urinary system.
It is also important to maintain a drinking regime, consuming a sufficient amount of clean water without gas (at least 1.5 l/day).