During the period of bearing a child, as well as in the postpartum period, many women experience exacerbation of chronic diseases that were diagnosed before pregnancy. In order for a woman to safely bear and give birth to a child, from the moment of pregnancy a whole list of sequential reactions is launched in her body, one of which is suppression of the immune system.
In the postpartum period, a woman’s immunity continues to remain at a relatively low level, which is why a young mother runs the risk of encountering certain pathologies of an infectious and non-infectious nature. A striking example is pyelonephritis after childbirth, the characteristics and features of which will be discussed in detail below.
Why do my kidneys hurt when breastfeeding?
Kidneys are an important organ in the human body. Its main function is to filter the blood in special glomeruli, cleansing it of toxins. In a few minutes, the kidneys pass through their entire volume.
Disruption of this organ leads to serious changes throughout the body. Therefore, it is extremely important to promptly identify and treat renal pathology. Unpleasant sensations and discomfort may appear when swelling of the tissue under the capsule occurs or the urinary tract is irritated, for example, by salt crystals, etc.
This may be caused by the following conditions:
- Inflammation of all organ structures – pyelonephritis. In this case, swelling of the perinephric tissue occurs, which causes nagging pain in the back.
- Urolithiasis disease. Pain in this case occurs due to the fact that small stones begin to move along the renal pelvis and ureters, causing irritation of the mucous membrane and severe pain.
- Thrombosis of renal vessels. In this case, swelling of the kidney occurs due to the fact that blood flows in, but its outflow is impaired due to vascular thrombosis. This happens extremely rarely after childbirth.
- Glomeluronephritis is a disorder of the kidneys due to changes in the glomeruli - the glomeruli.
- Hydronephrosis is the accumulation of fluid in the pelvis if the outflow of urine is disrupted, for example, with urolithiasis or with a tumor. Stretching of the kidney capsule causes pain.
- Injuries, bruises in the lumbar region.
But it should be noted that most often pain in the lumbar region is caused not by kidney pathology, but by problems with the spine (osteochondrosis) and muscles (myositis).
The following conditions do not lead to severe pain:
- benign (cysts, etc.) and malignant tumors in the early stages;
- acute or chronic renal failure;
- malformations of this organ.
When renal pathology is confirmed after childbirth, in more than 90% of cases it is pyelonephritis. This is due to the fact that during this period the woman’s immunity is significantly weakened. And sometimes a young mother does not even suspect that she has a hidden infection in her kidneys. Accordingly, against the background of weakened immunity, microbes begin to become more active and cause illness. It can begin to appear immediately after birth or after a few weeks.
What diuretics are allowed for breastfeeding?
When breastfeeding, accompanied by edema, it is advisable to avoid any diuretics. If the swelling is severe, and the kidneys excrete urine slowly or are affected by pyelonephritis, diuretics cannot be avoided. You can choose a suitable medicine from herbal preparations, tablets based on herbal ingredients, traditional medicine or pharmacological drugs. The main thing is to consult with your doctor about the chosen diuretic and its dosage, which will not harm the newborn.
Diuretics should be taken after breastfeeding to ensure they have minimal effect on breast milk.
Herbs and herbal infusions
For breastfeeding, you can drink diuretic decoctions of chamomile, parsley roots, bearberry leaves, centaury, rosemary leaves, lovage roots, birch leaves, lingonberry leaves, knotweed grass, yarrow, corn silk and wheatgrass rhizomes. In addition to removing excess fluid from the body, diuretics for nursing mothers have a persistent antimicrobial, anti-inflammatory, antispasmodic and analgesic effect.
A diuretic herbal mixture for breastfeeding is prepared from rose hips, lingonberry leaves, bearberry leaves, string and St. John's wort. It is recommended to discard other herbal mixtures during this period, since the combination of many medicinal herbs in one collection is contraindicated during breastfeeding.
Diuretics based on herbal ingredients
Of the herbal diuretics for breastfeeding, Canephron, Urolesan and Fitolysin are allowed. These natural herbal remedies have a good diuretic effect, destroy bacteria in the kidneys and urinary tract, dissolve stones in urolithiasis, relieve inflammation and spasms of smooth muscles. They do not have a negative effect on lactation and practically do not inhibit milk production, but before using them you should consult a urologist.
Folk remedies
Traditional medicine recommends using watermelons to get rid of edema during breastfeeding. It is prohibited to consume melons during breastfeeding, since the child’s gastrointestinal tract is not yet able to digest them. Cranberry and lingonberry fruit drinks, decoctions and compotes, infusions of dried apricots, raisins and prunes, freshly squeezed carrot, cucumber and pumpkin juices effectively eliminate swelling. Fresh apples, celery, green onions and grapes will help remove excess fluid from tissues.
To prevent swelling from returning, a nursing mother needs to follow a salt-free diet, eat right and move more.
Causes
The infection can be in the body and lie dormant for the time being, without showing any symptoms. Pregnancy and childbirth often provoke the activation of chronic diseases. It may start with cystitis, but very quickly the bacteria will reach the kidney and pyelonephritis will develop.
In some cases, pyelonephritis begins to develop in the last weeks of pregnancy. Due to the growing uterus and increased intra-abdominal pressure, the outflow of urine becomes difficult and this leads to the development of the disease.
Composition and effect of the drug
Canephron is available in tablets or drops. During breastfeeding, women are more often prescribed tablets, since the drops contain alcohol.
This medicine contains:
- rosemary;
- rose hip;
- centaury;
- lovage
All plants that are used in the production of Canephron have been used for many years to treat inflammatory processes in the genitourinary system. This drug has the following therapeutic effects:
- helps improve the functioning of the kidneys and urinary tract;
- relieves swelling by removing excess water from the body;
- relieves spasms;
- increases the effectiveness of antibiotics during the treatment of infections;
- relaxes the vessels of the genitourinary system;
- improves blood flow in renal tissues.
Excipients of Canephron are: riboflavin, castor oil, lactose, etc.
When breastfeeding, women can take this medicine not only for primary treatment, but also in combination with other drugs. Due to the absence of side effects, Canephron is very well accepted by the body, as evidenced by numerous positive reviews about this drug. Already from the first days of taking it, you can feel the pain subsiding and concerns from the genitourinary system disappear.
How to identify and diagnose an infection?
Urinary tract infection (cystitis) is often confused with pyelonephritis. However, in the case of cystitis, the woman’s general condition deteriorates slightly. And the clinical picture of pyelonephritis looks very bright.
The symptoms of the disease are difficult to miss:
- Increase in body temperature to 39-40°.
- Back pain just above the lower back (can be unilateral, if one of the kidneys is affected, or bilateral).
- Symptoms of general intoxication: chills, general weakness, nausea.
- Painful urination.
If the body temperature is elevated in the postpartum period, a woman must undergo a general urine test in addition to a clinical blood test. Which, with pyelonephritis, will most likely show an increased content of leukocytes and protein. To accurately diagnose the disease, an ultrasound of the kidneys is performed.
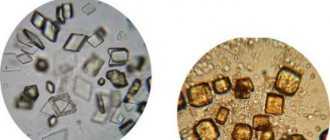
This is what a kidney affected by pyelonephritis looks like
How to treat childhood cystitis in girls
Cystitis is observed much more often in girls than in boys. This is facilitated by a slightly different structure and location of the genitourinary organs - the urethra is shorter and wider, which allows infections to easily penetrate inside the body. In addition, in childhood, girls’ ovaries are not yet sufficiently formed, which perform the protective function of the mucous membrane from viruses and infections.
Causes of occurrence and risk groups
Multiple factors can contribute to the development of childhood cystitis. First of all, this is determined by the general condition of the body and the presence of certain diseases, in particular:
- congenital defects of the urinary system;
- chronic infectious foci in the body;
- urinary incontinence;
- diabetes;
- neurogenic bladder dysfunction;
- calcium oxalate crystalluria.
In addition, external provocateurs can also cause the development of pathology. These include:
- infections acquired from outside;
- invasive methods of diagnosis and therapy (surgery or cystoscopy);
- foreign body in the urinary organs;
- treatment with medications that irritate the bladder mucosa;
- radiation and toxic agents.
When an infection occurs, cystitis does not appear immediately, but only after a decrease in immunity, which may be caused by a cold, lack of vitamins and other factors.
Urinary tract infections occur in different ways. Doctors identify several methods: The folk method of cleansing the kidneys! Our grandmothers were treated using this recipe...
Cleaning your kidneys is easy! You need to add it during meals...
- Descending - the infection can come from the kidneys, against the background of pyelonephritis.
- Ascending – penetration of bacteria from the anal or genital area.
- Hematogenous - with blood, with sepsis.
- Contact – infection occurs through the wall of the bladder.
- Lymphogenic - along the lymph flow.
In the case when the girl is not yet two years old, the infection enters the body in an ascending manner. If hygiene is not observed, remains of feces or urine enter the vagina, which provokes the development of an inflammatory process. Microorganisms multiply, causing cystitis to appear.
The main causative agents of the disease:
- chlamydia;
- coli;
- ureaplasma;
- staphylococci;
- streptococci.
Girls who have:
- dysbacteriosis;
- poor nutrition;
- urolithiasis disease;
- various types of genital injuries;
- chronic pathologies of internal organs (colitis, pancreatitis and others).
Factors that can cause the appearance of cystitis in children:
- Wearing tight underwear.
- Failure to comply with or lack of hygiene measures in the intimate area.
- Hypothermia.
- Frequent infectious diseases.
- Incomplete emptying of the bladder.
Normally, at the age of 8 years, girls should urinate about 7 times a day.
Forms and signs of cystitis
Characteristic symptoms and further treatment of cystitis in girls will depend primarily on the form of development of the pathology.
- Acute cystitis. The manifestation of the disease occurs several hours or days after exposure to the infectious pathogen. The development of a superficial inflammatory process on the mucous membrane is noted. If the disease is diagnosed on time and the correct treatment tactics are chosen, then the complete disappearance of symptoms occurs after 7–10 days.
- Chronic cystitis. It occurs against the background of frequent inflammation of the bladder mucosa and in most cases is observed in children with other diseases. As a rule, in the presence of other pathologies, inflammation occurs. This form of cystitis is difficult to treat and lasts a long time. As a result of the disease, the deep layers of the bladder are affected. In severe cases, inflammatory processes also affect the outer layers of the organ.
The first symptoms of cystitis are a burning sensation and stabbing pain in the pubic area.
Since infants are not yet able to tell what is causing them concern. Symptoms that may indicate a urinary tract infection include:
- increased body temperature (up to 39 degrees);
- frequent urination;
- crying and worrying;
- dark color of urine.
In addition, older adults receive complaints about:
pain that occurs when going to the toilet in the lower abdomen;
- pain in the perineum;
- urinary incontinence;
- presence of blood impurities in the liquid.
With chronic cystitis, such manifestations will be less pronounced. Their intensification is observed during exacerbations.
Diagnostic methods
At the first suspicion of cystitis, the child must be immediately shown to a specialist. The doctor will conduct an examination and, in accordance with the results obtained, prescribe a course of treatment.
Diagnosis of cystitis includes:
- general analysis of urine and blood;
- tank culture, which allows you to determine the type and level of sensitivity of pathogenic microorganisms;
- biochemical analysis;
- Ultrasound of the urinary system.
The determining method of research confirming the diagnosis will be a urine test. To obtain the most reliable data, it is important to adhere to certain rules:
- before collecting urine, perform thorough hygiene of the genitals using soap and warm water;
- urine is submitted to the laboratory no later than an hour and a half after collection;
- It is recommended to use only a sterile container.
To collect tests from a newborn, you can buy a special device - a urine collector.
Before performing an ultrasound examination, it is necessary that the bladder is full. This method allows us to identify the presence or absence of thickening of the mucous membrane of the urinary organ, uneven contours and jaggedness.
Therapeutic measures
In order for the treatment of cystitis in girls to be as effective as possible, it is necessary to take an integrated approach. It is important to follow the following recommendations:
- The child should be provided with bed rest at least for the first 3–4 days from the onset of the disease.
- Warm foot baths can be used as symptomatic therapy at home. They help relieve pain in the abdominal area by redistributing blood flow in the body.
- The patient should be provided with plenty of fluids. This will prevent intoxication.
- If the child is under 1 year old and is breastfed, then his mother should review his diet.
- Proper hygiene of the genital organs is necessary - frequent diaper changes for infants, spacious underwear made of natural fabrics.
- If treatment at home is meant using traditional medicine, then this must be discussed with the attending physician, since some plants can provoke an allergic reaction.
Treatment with medications
How to treat cystitis with medications is determined by the doctor. Since the disease mainly occurs under the influence of bacterial pathogens, antibiotics must be used. Usually prescribed:
- Augmentin - can be used at any age.
- Cefuroxime - the dose is calculated depending on the age category of the small patient and her weight. For example, at 6 years old it is recommended to administer 5 ml of the drug in the morning, lunch and evening.
- Monural – can be used one-time from the age of 5 years.
In addition, the doctor prescribes medications from groups such as:
- Anti-inflammatory and antibacterial agents - Canephron, Cyston.
- Lacto- and bifidobacteria – Acipol, Hilakforte, Linex.
- Antiviral medications – Kagocel, Cycloferon.
- Antipyretic drugs – Ibuprofen or Paracetamol. For illness in newborns and young children, it is recommended to use rectal suppositories. At older ages, medications are given in tablet form.
Phytotherapy
As a supplement, you can give your child infusions and decoctions prepared from medicinal plants. It is important to remember that this method will not replace antibiotics, but will reduce the inflammation process and ensure remission for a long time.
If the treatment of acute cystitis is chosen correctly, then recovery occurs quickly. In case of chronic pathology, it is necessary to periodically be observed by a specialist.
To prevent the occurrence of a disease such as childhood cystitis, you need to try not to overcool the body and strictly follow the rules of hygiene.
Symptoms of pyelonephritis during lactation
During pregnancy and after childbirth, urinary tract infections (UTIs) are common. This condition is not accompanied by any symptoms; the pathology is diagnosed by inflammatory changes in urine tests. If a UTI is missed, the infection will progress to pyelonephritis. Therefore, it is important to regularly take at least general urine tests during pregnancy and for some time after childbirth.
Pyelonephritis can occur in acute and chronic forms. The course of the disease largely determines the severity of symptoms. Accordingly, acute pyelonephritis will have a clear clinical picture, while chronic pyelonephritis will have a blurred clinical picture. Symptoms of the disease include the following:
- Increased body temperature, most often up to 38 and above. This is due to intoxication of the body and activation of infection.
- Along with this, weakness, lethargy, and headaches appear.
- There may be digestive disorders - diarrhea, nausea or vomiting.
- The main symptom is pain in the area of the projection of the kidneys. Usually this is in the lumbar region or a little higher, almost under the very ribs on the back. The pain can be sharp and unbearable, but more often it is a dull and aching discomfort.
- Often pyelonephritis is accompanied by the involvement of other parts of the urinary system (bladder, urethra, etc.) in the inflammatory process. This will add symptoms such as pain and cramps when urinating, frequent urges, and others.
Prevention of pyelonephritis
Pyelonephritis is easier to prevent than to treat. Basic methods of preventing pyelonephritis in women:
1. Timely and complete treatment of infectious diseases, such as:
- caries;
- tonsillitis;
- sinusitis;
- cholecystitis;
- appendicitis;
- pneumonia;
- colitis;
- cystitis.
2. Prevention of constipation.
3. Compliance with hygiene rules.
4. Monitoring urine during pregnancy and during routine medical examinations (for example, during medical examinations of the population).
5. Avoiding severe physical and mental fatigue.
6. Avoiding prolonged stressful conditions.
7. Avoiding hypothermia and places with high humidity levels.
8. Conducting preventive courses of herbal therapy.
9. Comprehensive examination of the urinary system during pregnancy planning.
10. Performing special exercises for pregnant women that ease the load on the kidneys and restore the natural flow of urine.
11. Maintaining plenty of fluids during pregnancy.
Forms of pyelonephritis and their features
Depending on the clinical manifestation and course of the disease, there are two forms of pyelonephritis - acute and chronic. Each of them has its own treatment principles and prognosis.
Acute
The acute form always begins suddenly, usually with an increase in body temperature. All other clinical symptoms are also pronounced, so there are no special problems in diagnosing the condition. But acute pyelonephritis requires serious treatment, despite breastfeeding. Sometimes you have to resort to surgery, for example, installing stands in the ureters to normalize the outflow of urine, etc.
Acute pyelonephritis can lead to various types of complications, for example, to the formation of multiple ulcers in the kidney (apostematous nephritis) or to an abscess.
Chronic
Chronic pyelonephritis can form for several reasons. Namely:
- If antibacterial drugs are taken incorrectly (incomplete regimens, incorrect doses, etc.). This leads to the development of drug resistance in bacteria.
- With a weak immune response to inflammation, some of the microbes eventually enter a latent form.
- If there are any structural features of the organs of the urinary system. They can be congenital or acquired (after operations, injuries, etc.).
Chronic pyelonephritis can occur with rare periods of exacerbation. In this case, the woman has no idea about the source of latent infection in her body for a long time. Any weakening of the immune system (childbirth, pregnancy, etc.) leads to the activation of microbes.
A long course of chronic pyelonephritis can lead to shrinkage of the kidney, it decreases in size and ceases to function. The risks of urolithiasis, hydronephrosis, kidney failure and other problems also increase.
What is pyelonephritis, its types
Pyelonephritis is an inflammatory kidney disease, which is characterized by a nonspecific pattern of origin. The pathological condition first spreads to individual parts of the kidneys: the cups and pelvis, and then spreads to the entire organ, including the renal tubules and vessels.
Pyelonephritis in medicine is distinguished as an independent disease, and as a developed consequence of other conditions of the human body (for example, pregnancy, inflammatory diseases of the peritoneal organs). This disease is the most common among nephrological pathologies; according to statistics, every tenth person is diagnosed with pyelonephritis.
Women suffer from this problem 3-4 times more often than men. This is explained by the structure of the female genitourinary system (short urination channel, close location of the ovaries) and the reproductive function, which disrupts the natural flow of urine.
In medicine, pyelonephritis is classified very thoroughly; there are more than a dozen varieties of the disease, divided according to criteria and subtypes (for example, depending on the penetration of the infection, its spread).
The general type picture of pyelonephritis can be presented as follows:
1. According to the course of the inflammatory process:
- chronic;
- spicy.
2. By the number of foci of infection:
- unilateral;
- bilateral.
3. According to the patency of the urinary canals:
- obstructive;
- non-obstructive.
4. According to the nature of the origin of the infection:
- primary;
- secondary.
Manifestation of the clinical picture
With pyelonephritis during breastfeeding, the following symptoms are often observed:
- fever;
- muscle pain;
- increase in temperature;
- urine becomes cloudy in color;
- lower back pain;
- discomfort in the lower abdominal cavity.
Symptoms appear quite quickly, and the woman is not able to adequately assess her own well-being. If you have intense pain, you should consult a doctor.
Stages of flow
There are primary and secondary stages of the disease:
- the primary is the inflammatory process, during which there are no disruptions in urodynamics and other kidney pathologies;
- secondary inflammation that occurs in various diseases of the genitourinary system.
Having established the stage of the disease, it is possible to begin appropriate therapy.
Basic principles of treatment
If a woman has the first signs of pyelonephritis, she should immediately seek advice from a specialist who can correctly and promptly diagnose the pathological condition, and then prescribe appropriate treatment. In most cases, the doctor will insist on hospitalization. This decision is not without meaning, because in a hospital setting it is much easier to control the dynamics of the patient’s condition and it is possible to use a complex of the most effective medications.
However, postpartum pyelonephritis in a nursing mother is complicated by the woman’s reluctance to be separated from the baby and interrupt breastfeeding. In this case, the doctor is forced to decide on hospitalization of the woman in the event of a sharp deterioration in the patient’s condition or prescribe appropriate medications that can be used at home.
How to treat pyelonephritis? Of course, antibiotics will be the basis of the therapeutic complex. And on this basis many questions arise.
Antibiotics and breastfeeding
So, how to treat pyelonephritis of both kidneys during breastfeeding? The answer from a competent and qualified specialist will be unequivocal: antibiotics. After all, the pathological process can affect not only the pelvis and tubules, but also affect the entire kidney.
The worries of many mothers associated with the prescription of antibiotics are often not without meaning. Depending on the severity of the disease, the doctor prescribes medications that may not be compatible with breastfeeding. However, this is not a reason to refuse treatment. During this period of time, the baby should be switched to artificial feeding, and the mother should follow the specialist’s instructions flawlessly.
This video explains how to combine medication and breastfeeding without harming the baby:
A nursing mother will have to work hard to maintain lactation. You will have to express milk several times a day (6-9). The main antibacterial drugs that are most effective during this period include Amoxicillin. Doctors immediately warn that its use has a negative effect on the baby. Nevertheless, Amoxicillin very effectively fights the causes of the disease, and therefore is widely popular among many specialists.
But the latest generations of antibiotics act selectively, so there is a high probability that a nursing mother will be treated without recommendations to stop breastfeeding. The annotations of many modern drugs indicate that they can be used during breastfeeding or lactation. In this case, you don’t have to worry about the fact that antibiotics threaten the baby and can cause any negative consequences. However, not all of them will be effective; in any case, the choice of drug for therapy will be strictly individual and based on the severity of the patient’s condition.
How to treat pyelonephritis besides using antibacterial drugs? Experts recommend drinking plenty of warm drinks to help remove toxins and waste products from the body. Bed rest will also be an important factor promoting recovery. Only full compliance with all the doctor’s recommendations will be the key to a complete recovery and a return to full breastfeeding of the baby.
Complete collection and description: tablets for kidneys during lactation and other information for human treatment.
Many women experience bladder problems during pregnancy. Doctors often prescribe Canephron in such cases. After childbirth, urinary tract diseases may recur. But with breastfeeding, you need to be careful when using medications so as not to harm your baby. Therefore, it would be fair to find out whether Canephron can be taken while breastfeeding.
Diagnosis of pyelonephritis in a nursing mother
Signs of pyelonephritis can be identified when examining a woman. When tapping on the back, pain will be felt in the area where the kidneys are projected. You also need to do the following to confirm:
- General urine analysis. It will contain an increased amount of protein and, most importantly, leukocytes.
- A general blood test, which will show clear signs of inflammation. This is a decrease in hemoglobin levels, an increase in ESR, leukocytes, and a change in the leukocyte formula.
- Urine according to Nechiporenko, the study is aimed specifically at identifying inflammation in the kidneys.
- Sometimes a three-glass test is performed with separate urine collection, alternately in three portions during one act of urination. This way you can identify the site of inflammation - kidneys, bladder, urethra, etc.
- Urine according to Zimnitsky will show how this organ functions. This is especially true for chronic pyelonephritis.
- Urine culture for flora and sensitivity to antibiotics helps determine the most effective treatment regimens.
- An ultrasound examination of the kidneys will reveal signs of inflammation (swelling, changes in kidney density, etc.), as well as stones and other possible formations in them (cysts, tumors, etc.).
- Various radiological methods are used for complicated forms of pyelonephritis and combination with urolithiasis. These are excretory, retrograde urography and others.
- A CT or MRI is performed if a kidney tumor is suspected.
Diagnosis of the disease
A doctor may suspect pyelonephritis based on complaints, examination and medical history. To clarify and determine the extent of the process, a more in-depth examination is necessary. Urine is thoroughly analyzed. The following tests are performed with it:
| Type of study | Features of the event |
| General research | With pyelonephritis, the TAM will have increased leukocytes, protein, possibly casts and bacteria. |
| Bacteriological culture of urine for flora | It is important to do this test before starting antibiotics. Otherwise, the results may not reflect the true process. |
| Urine according to Nechiporenko | Gives a more detailed result on the content of leukocytes. |
| Research on Zimnitsky | It is carried out to identify kidney dysfunctions, which may be the first signals on the path to renal failure. |
| Three-glass sample | It is carried out to determine the location of inflammation (kidneys, bladder or urethra). In this case, it is necessary to collect urine sequentially into three containers during one act of urination. |
Instrumental diagnostic methods are used. Most often this is:
- Ultrasound examination of the kidneys. In this case, you can see signs of inflammation, an increase in size, accumulation of fluid in the pelvis and ureters, etc.
- X-ray methods are widely used - various types of urography and others. In this case, the urinary system is filled with a contrast agent and a series of images is taken. They can be used to judge some serious changes in the kidneys.
- CT and MRI are often performed in case of tumor processes or suspicion of them.
Is it possible to relieve kidney pain at home?
If pain occurs in the kidney area, you should first make sure that it is they that are bothering you. Often these are myositis (inflammation of muscles), radiculitis of the lumbar region, etc. If a young mother is sure that her back hurts precisely because of her kidneys, she can do the following:
- Take an antispasmodic drug (no-shpu, drotaverine and the like).
- Additionally, you can relieve pain with the help of NSAIDs (diclofenac, ketorolac and others).
- For fever - antipyretics.
After this, you should consult a doctor. After a minimal examination and examination (at least a general urine test and Nechiporenko test), the specialist will prescribe additional medications. These will most likely include antibiotic therapy. For exacerbation of pyelonephritis, this is the main treatment.
You should not start taking antibiotics on your own, only in extreme cases when it is not possible to visit a doctor.
This may cause the following:
- Incorrect regimens will contribute to the development of microbial resistance to drugs.
- If you first start treatment with antibiotics and then take tests, the results will not be entirely reliable. This is especially true for urine culture for flora.
Treatment of pyelonephritis after childbirth
Treatment of pyelonephritis after childbirth should only be carried out by a specialist. Self-prescription of drugs and thoughtless use of traditional medicine can only aggravate the situation and cause harm not only to the mother, but also to the baby. Therefore, everything must be agreed with the doctor.
General recommendations for a nursing mother will be as follows:
- It is useful to take the knee-elbow position several times a day to improve the flow of urine. For the same purpose, it is recommended to sleep on the “healthy” side.
- Bowel movements should be monitored and laxatives taken if necessary.
- It is recommended to limit the consumption of table salt, as it retains fluid and will aggravate the disease.
Drug therapy
The directions of treatment are as follows:
- Antibacterial therapy taking into account the expected flora and its sensitivity to drugs. The following drugs are often prescribed: Amoclav, Cefotaxime, Cefepime and others. If a woman supports lactation, those products are chosen that are safe at this time.
- Antispasmodics, anti-inflammatory and painkillers.
- Detoxification therapy is carried out at high temperatures. For this, intravenous infusions of saline, glucose, Ringer and others are used. This allows you to quickly remove microbial toxins from the body, which will contribute to a speedy recovery.
- Immunomodulatory agents, for example, Viferon, Ruferon and others.
Folk remedies
It is useful to combine herbal medicine from ready-made mixtures or create compositions yourself. The following herbs are recommended:
- bearberry leaves,
- cowberry,
- fennel,
- parsley,
- dill,
- rosehip and others.
You can make tea, fruit drinks or just infusions. During treatment of pyelonephritis, it is very important to maintain a drinking regime, since microbial toxins will be released along with urine, and the disease will recede.
When using herbal preparations, you should carefully monitor the baby's reaction if he is breastfed. Any rashes, swelling and other complications in the baby should cause immediate cancellation.
Possible complications
The most common adverse effects in women during the postpartum period include:
- Breast engorgement . It occurs at the initial stage of breastfeeding and lasts for 2 days, and is minimized by early frequent breastfeeding. In some situations, a comfortable bra for mothers during lactation helps. It must be worn all day. In addition, use a cool compress on the chest after feeding, and mild analgesics (for example, Ibuprofen). Sometimes massage and a warm compress help. Additional pumping of milk reduces engorgement. A certain amount of milk is expressed, which eliminates discomfort.
- Mastitis . It is observed quite often and manifests itself as a painful, swollen part of the breast. It is formed when the gland becomes engorged and the ducts are blocked.
- Mother's concern . Frustration and dissatisfaction develops as a result of a lack of lactation experience, technical difficulties in the feeding process, fatigue and difficulty in determining a sufficient volume of milk, as well as physiological changes after childbirth.
Compliance with preventive measures helps prevent adverse consequences.
Treatment of children
This medicine is good not only for adults. Doctors often prescribe it to treat children. And even in infancy.
Usually children are prescribed an alcohol solution. Despite the fact that it contains alcohol, studies have shown that a tiny amount of it cannot harm a growing child's body.
Latest discussions:
The female genital organs are located close to the bladder, so pregnancy can lead to urinary tract problems. After childbirth, urinary tract diseases will prevent a young mother who is breastfeeding from fully enjoying motherhood. During lactation, not all medications are allowed to be taken, since they can affect the baby through milk. But some drugs, which include Canephron, are recommended for use even by nursing mothers.
After childbirth, there is a high risk of a woman developing a urinary tract infection.
A woman's body before and after childbirth
During pregnancy, many women suffer from edema. This is not something to be afraid of. Swelling is a normal phenomenon due to hormonal changes. They will go away a few days after giving birth. Excess fluid will be eliminated through urination.
Women who have recently given birth begin to go to the toilet frequently. This is the process of removing excess fluid. If the health condition is not aggravated by hypertension, blood pressure, heart or kidney pathology, special medications to combat edema are not prescribed. To alleviate the condition, it makes sense to drink birch sap or diuretic decoctions, which are recommended by the doctor.
During childbirth, the genitourinary organs take on a large load and experience stress. A woman’s immunity declines, and bladder diseases develop against this background. At the current level of development of medicine, these diseases respond well to treatment, but not all medications can be taken orally without harming the health of the baby.
Diseases of the genitourinary system are accompanied by swelling, pain, nausea and vomiting, and fever. Often a woman develops cystitis, which is caused by E. coli entering the urinary ducts. A popular treatment for kidney and bladder diseases is the drug Canephron. Let's figure out whether it can be consumed during lactation.
Composition of Canephron
The alcohol version of the drug is contraindicated in nursing women, so Canephron is recommended to be taken in tablet form
Canephron is a herbal medicine. It includes herbs such as centaury, rosemary leaves, rose hips and lovage roots. The composition also includes additives: plain and modified corn starch, silicon dioxide, povidone, riboflavin, calcium carbonate, lactose monohydrate, titanium dioxide, talc, dextrose, shellac, corn oil, red iron oxide and rock wax.
The drug in drops contains a hydroalcoholic extract, so drops are not prescribed to young mothers while breastfeeding. Canephron tablets are yellow in color. They are small, packaged in cellular plates of 20 pieces each. There are 3 such plates in a package.
Action of Canephron
Main properties of the drug:
- The drug has an antispasmodic and diuretic effect. It normalizes the process of urination. The diuretic property helps relieve edema, the antispasmodic property improves blood flow in the renal tissues.
- Canephron increases the effectiveness of antibiotic treatment. It should be noted that antibiotics are prescribed to nursing women as a last resort, and breastfeeding is prohibited.
- It has antimicrobial and anti-inflammatory effects. It is prescribed to patients with chronic inflammatory processes, since the drug is well tolerated.
- The biologically active substances included in the drug determine its antiseptic effect.
- The drug reduces the excretion of protein from the body, which is used in the treatment of certain diseases.
Breastfeeding is not canceled when taking Canephron, since the herbal composition of the drug allows you to treat inflammation without harming the newborn.
Women are prescribed Canephron while breastfeeding, usually in tablets. From the first days of taking the drug, the patient feels relief. The medicine is also used for complex therapy in combination with other drugs.
For what diseases is Canephron prescribed?
Currently, urolithiasis is becoming a disease of increasingly younger women. At the same time, pregnancy and feeding often aggravate its course. Therefore, the doctor may suggest taking a course of Canephron during lactation for preventive purposes, since the medicine prevents the formation of stones in the kidneys and bladder.
Childbirth takes a lot of strength and health from a woman. A weakened body needs support with medications, so doctors sometimes prescribe a number of medications to mothers who have recently given birth to help the body recover. Diseases for which Canephron is indicated:
- if symptoms (back pain, blood in the urine, uncomfortable urination) indicate the presence of kidney stones;
- pain when urinating, indicating possible cystitis;
- back pain at the lumbar level, which is a sign of inflammation of the renal pelvis;
- inflammation of the renal glomeruli;
- inflammation of the kidney calyces.
If a woman experiences one of the symptoms of a urinary tract infection, she should seek help from a doctor.
Self-treatment is not allowed due to the danger of harming not only yourself, but also the baby’s body. Before deciding to prescribe the drug, the doctor prescribes an examination, which includes tests and an ultrasound. Once a diagnosis has been made and medication has been prescribed, treatment must be started as quickly as possible. An advanced disease causes a serious complication - inflammation can spread to other organs of the body.
There are no obvious contraindications to taking Canephron. The limitation is individual intolerance to the drug. It can only be detected during treatment. Carefully monitor your feelings and your child’s when you start using the drug. If your newborn develops allergies, diarrhea, fever, restlessness, sleep disturbances, or other signs of unwellness, stop treatment and consult a doctor.
How to take Canephron during lactation?
A detailed regimen for using the drug is contained in the instructions included with the package. Despite this, you should not take Canephron on your own. The medicine must be prescribed by a doctor who will determine your dosage based on the patient’s personal characteristics and health status.
As a rule, Canephron during breastfeeding is prescribed 2 tablets 3 times a day. Treatment usually lasts 1 month, but the doctor may extend it for another 2 weeks. Drops are taken 50 drops in one dose 3 times a day.
The doctor will prescribe the required form of release of the drug and dosage. In this case, it is necessary to strictly follow the instructions for the drug, as well as monitor the health of the woman and child.
Canephron is prescribed in tablets during lactation. Due to the natural composition of Canephron, it is indicated for breastfeeding women. There is no need to interrupt breastfeeding. The drug will not harm either the mother or the infant. Since antibiotics cannot be taken during lactation, at the very beginning of urinary tract inflammation, women are prescribed this drug, which successfully fights the disease.
For the treatment of children, Canephron for children, which has a different dosage, can be used. Individual intolerance to the drug may also be a contraindication. Canephron is a unique drug that has no analogues. Its herbal composition allows it to be prescribed to people of different ages and health conditions.
Is it possible to take medicine without a doctor's prescription?
Let us note once again that self-treatment without examination by a specialist is unacceptable. Only a doctor can decide which medicine you should take and minimize the risk of side effects. In recent years, almost all drugs can be purchased in pharmacies without a doctor's prescription. In this regard, the number of cases of complications from taking medications has sharply increased, including among young children. Adults and children are admitted to hospitals in serious condition after self-administration of medications that caused serious health complications. The drug can only be prescribed by the attending physician. If you decide to be treated with traditional medicine, you still need to consult a specialist.
https://youtu.be/7-7jkH56WzA
Pyelonephritis is characterized by the development of an inflammatory process in the kidneys, caused by various bacteria, with damage to the pyelocaliceal system. This disease is quite common in nursing mothers.
Often, symptoms begin to appear a short period of time after childbirth, when the weakened body cannot fully fight the infectious agents - streptococci, Proteus, Escherichia and enterococci.
The development of the disease can lead to a number of adverse consequences, including chronic renal failure.
How to alleviate the condition?
Relying on traditional methods of self-medication for pyelonephritis after childbirth is strictly prohibited. But you can use some tips to ease your condition during illness:
- You can stand in the knee-elbow position several times a day. This improves urine flow.
- Eat easily digestible foods so as not to provoke constipation and stimulate easy and timely bowel movements.
- Limit the consumption of salt, which retains water in the body.
- Maintain plenty of fluids. You can drink fruit drinks, clean warm water, and lemon water. Microbial toxins will be eliminated from the body along with urine.
Therapy methods
Treatment of pyelonephritis after the birth of a child is complex. The most rational and harmless means during lactation are prescribed only by a doctor. Self-treatment can only make you feel worse. Mostly therapy involves:
- medications;
- herbal medicine;
- physiotherapy.
He will properly and in the shortest possible time diagnose the pathological process, and then prescribe appropriate therapy.
Traditional remedies
During lactation, it is optimal to limit the use of medications. Required admission will be:
- Antibiotics. They should be selected taking into account the susceptibility of the flora, but this is not possible in all cases. Often, drugs from the cephalosporin subgroup (Cefepime, Cefotaxime) and the penicillin series (Amoclav, Amoxiclav) are used.
- If necessary, take anesthetics and antispasmodics.
During treatment, you need to maintain a drinking regime and not interfere with urination. For these purposes, it is recommended to sleep on the opposite side, take a knee-elbow position 3-4 times a day, and prevent constipation.
ethnoscience
For the treatment and prevention of the disease, preparations with diuretic, antiseptic and antibacterial effects are used. They can be complex compositions or single-component ones. It is recommended to make tinctures and decoctions from the following medicinal herbs:
However, you need to be careful and observe the baby’s reaction to new components.
Nutrition rules
If inflammation is detected in the kidneys, women after childbirth are advised to follow a special diet.
For example, during acute pyelonephritis you need to drink more fluid.
Spicy, fatty and fried foods are excluded from the menu. It is recommended to take as many vegetables and fruits as possible.
- reducing the consumption of meat products, fish broths, spices;
- increasing the amount of fluid taken (at least 2 liters per day);
- reducing salt intake;
- increased intake of vitamins into the body.
You need to consult a doctor who can choose your diet during the postpartum period.
Introduction
Nephroptosis
, or omission
kidneys
, is a condition in which the mobility of the kidney exceeds the physiological norm. Normally, when changing body position and breathing, the kidney can move from the renal bed in the vertical direction up to 2 cm. With nephroptosis, the kidney can move up to 10 cm. Sometimes it can descend into the small pelvis. Such a mobile bud is also called
"wandering" kidney
The kidney is held at the physiological level by ligaments, fascia that form the renal bed, intra-abdominal pressure (created by the muscles of the anterior abdominal wall and the diaphragm), the fascial-fatty capsule of the kidney and the fatty tissue between
adrenal gland
and kidney.
According to statistics, nephroptosis is currently observed in 1.5% of women and 0.1% of men. The predominant age for this pathology is 25-40 years. Nephroptosis is observed predominantly on the right. This is explained by the fact that the left kidney has a stronger ligamentous apparatus and the fact that the right kidney is normally located lower than the left. In some cases, there is bilateral prolapse ( ptosis
) kidney.
Does breastfeeding affect the removal of kidney stones?
As for whether breastfeeding affects the removal of kidney stones
, we can say that yes, it does, and in a positive sense. To produce a sufficient amount of milk, you need to drink a lot, and the liquid, passing through the kidneys, flushes them, accelerating the passage of possible stones. Very often, stones are washed away at the sand stage, causing discomfort, but this is still better than the possibility of them being compressed into larger formations, the removal of which may require surgery.
After pregnancy and childbirth, exacerbation of a large number of chronic pathologies is likely.
Significant stress on internal organs increases, which is why many patients after childbirth turn to doctors with various pathological processes.
One of them will be pyelonephritis in the postpartum period during lactation.