Bilateral hemorrhage into the adrenal glands is the cause of acute adrenal insufficiency. In medical practice, this pathological condition is called Waterhouse-Friderichsen syndrome. Hemorrhage, or hemorrhagic infarction of the adrenal glands, often occurs against the background of a progressive infectious disease in the stage of decompensation.
Acute disruption of the blood supply to the adrenal glands leads to a complete or partial cessation of the formation of gluco- and mineralocorticoid hormones, which regulate water-salt, carbohydrate, immune metabolism and, in general, the homeostasis of the whole organism. Severe dehydration, collapse, neuropsychic and gastrointestinal disorders occur. If assistance is not provided at this stage, acute adrenal insufficiency develops into a coma, which ends in death.
The adrenal glands synthesize a large number of hormones that regulate important parameters of human life.
Etiology
Adrenal hemorrhage usually has 2 causes:
- Infection . Infectious diseases such as scarlet fever, measles, typhus cause damage to blood vessels, or rather their inner layer, by toxins. This leads to increased blood clotting, platelet aggregation, and thrombosis of the adrenal glands. This causes numerous hemorrhages in 60% of cases of Waterhouse-Friderichsen syndrome. The situation is aggravated by the fact that the affected vessels cannot carry oxygen, which means that the cells of all tissues are affected.
- Medical errors at the time of adoption of a child . Difficult childbirth and incorrect actions by the doctor lead to oxygen starvation. As a result, breakdown products accumulate in the body, affecting the adrenal glands. The result is the appearance of a hematoma. At risk are newborns with entanglement, diabetes mellitus, as well as those whose umbilical cord was cut too early (before the pulsation stops).
How long does it take for a hematoma to resolve?
This page contains the most popular posts and comments from our users on the topic “How long does it take for a hematoma to resolve.” This will help you quickly get an answer to your question, and you can also take part in the discussion.
I'm 10 weeks... a week ago there was a small detachment... today they did an ultrasound and they said there is a threat of miscarriage... the hematoma is not resolving
Girls, how long does it take for a hematoma to resolve, today I went for an ultrasound and it’s almost 30 mm, they said the baby is fine and to lie down more, they’ll discharge me on Monday
I popped the pills for two weeks, lay flat, went for an ultrasound, the doll is developing according to the schedule... the doctor said the hematoma has become smaller, but now I see that it is even a little larger in size than 6 weeks. Although according to the photo it’s not so dark anymore... at the 6th week there was actually a black spot all over the photo... but here it’s pale... I was treated for two weeks... the ultrasound specialist says that if there was tone or the cervix was slightly opened, it would.
I also have a hematoma... three weeks ago I was taken to the hospital with it, now I have been discharged, but the hematoma remains... sometimes it is smeared... the doctor at the residential complex said that this is normal, the hematoma is coming out, that it will take a long time to go away... it takes time... and more rest.
I came across it. They discovered it at 7 weeks and told me to wait. Up to 12 weeks, in most cases it resolves on its own. It hasn't resolved for me. At 14 weeks she was prescribed magnesium injections, no-shpu and vitamins. On the 8th or 9th day of treatment, I went to the toilet, and a piece of mucus with red streaks came out. There was nothing left on the ultrasound.
No, no blood, no pain
Source
Clinical picture
With hemorrhage into the adrenal glands, symptoms depend on the stage of the lesion.
First of all, the following signs appear:
- Changes (hyperpigmentation) of the skin and mucous membranes.
- Fall in blood pressure.
- Decreased appetite.
It is possible to normalize blood pressure by introducing adrenal hormones, the natural synthesis of which stops during hemorrhage.
If this is not done, the next stage of the lesion develops, which is characterized by a clinical picture:
- Increased body temperature.
- The appearance of vomiting.
This, in turn, leads to dehydration of the newborn's body. The child is lethargic, has scanty urination, and convulsions are possible.
Following the second stage comes the third stage, which is characterized by symptoms such as:
- Lack of urination.
- Decrease in temperature.
The child develops shock and falls into a coma.
With the development of bilateral hemorrhage, signs of acute adrenal insufficiency occur. First of all, these are shortness of breath, diarrhea, vomiting with blood, petechial skin rashes, tachycardia. Blood pressure drops sharply, convulsions and stupor appear.
If the hemorrhages are minor, they often go unnoticed, and in the future a small compaction forms at the site of the hematoma. In some cases, the adrenal gland can recover completely, although the formation of a tumor at the site of compaction is also possible.
Excision of the hematoma may require surgery, which may result in chronic adrenal insufficiency.
Anatomical and physiological features and functions of the adrenal glands in children
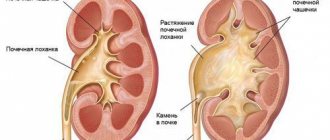
In the structure of small-sized organs, it is worth noting the presence of two different layers. Each layer performs specific functions. They are:
- Outer cortex;
- Medulla.
The outer layer is called the cortex, and the inner layer is the medulla. The structure of the medulla involves nerve and glandular cells, as well as nerve fibers. The medulla plays a secondary role, in contrast to the cortex. Removing the brain matter does not pose a threat to the child's life.
The function of the cortex is to process steroids and is responsible for the production of hormones, the main task of which is to regulate the process of substances throughout the body. In a newborn child, the mass of one adrenal gland is seven grams, and the size is slightly less than the size of the kidney. It is customary to separate the two adrenal cortexes. The cortex, in turn, has two zones:
- Fetal;
- Definitive.
During the initial formation, the adrenal glands undergo a number of functional changes. In the first month of a child’s life, their mass decreases by half; changes in the cortical zone are significant. At the age of about one year, the main role is assigned to the definitive zone, which performs the main functions in the child’s body.
During this period, the appearance of the glomerular, fascicular and reticular zones is noted. The cortical part is formed in a child between the ages of 11 and 14. The medulla increases in size. The end of its growth occurs in a period of 10-12 years. The organ enlarges by the age of 20. By this period, their work can be compared with the work of the adrenal glands of an adult.
Symptoms of the disease in children include:
- Muscle weakness;
- Fatigue;
- Cardiopalmus.
Manifestation of weakness, loss of appetite, nervous overexcitation are the causes of many diseases and require diagnosis, but many parents wonder how to check the functioning of the child’s adrenal glands. In this case, doctors recommend taking tests to determine the amount of hormones. The test results will reliably confirm the existence of a certain number of hormones in the child’s blood. Based on their results, you will be able to draw appropriate conclusions.
Diagnostic methods
Diagnosis begins with a visual examination of the child, during which the condition of the skin is assessed - they are bluish, moist and cold. There is also a decrease in blood pressure, which cannot be optimized even by taking medications.
A blood test allows you to determine the level of adrenal hormones and sugar . In case of hemorrhage, the former are reduced, while the sugar content coefficient significantly exceeds the norm.
To visualize the condition of the adrenal glands, they resort to ultrasound examination, thanks to which it is possible to see the part of the organ where the blood has leaked. When performing an x-ray of the adrenal glands, hematomas appear as dark spots on the image.
If adrenal hemorrhage is suspected, there is a risk of developing heart failure, therefore, among other diagnostic measures, an ECG is performed to assess the state of the cardiovascular system.
How is the diagnosis made?
To determine what kind of adrenal insufficiency we are talking about - primary, secondary or tertiary, perform:
Ultrasound of the adrenal glands, which may not show the organ at all, even if there is a tuberculosis or tumor process in it. In this case, an additional CT scan of the adrenal glands is performed; MRI of the brain with a targeted examination of the hypothalamus and pituitary gland.
But the main diagnosis of the disease is laboratory. In order to find out which hormone deficiency has occurred and how pronounced it is, the following are studied:
cortisol level in the blood: it is reduced in any type of deficiency; 17-OX and 17-KS in urine collected per day: these cortisol metabolites are also reduced in primary and secondary types of hypocortisolism; ACTH in the blood: it decreases with secondary-tertiary insufficiency, increases with disease of the adrenal glands themselves; determination of aldosterone in the blood: how much it is reduced; hidden forms of hypocortisolism are revealed by a stimulation test with ACTH: cortisol is determined initially, as well as half an hour and an hour after the administration of synthetic ACTH. If the cortisol level has increased by less than 550 nmol/l, it means there is adrenal insufficiency. Normally, cortisol levels increase 4-6 times. The test is carried out at a certain time - at 8:00, when there is a natural peak in the activity of the hormones being studied.
The diagnosis has been established. Now we need to determine how much electrolyte, protein, carbohydrate and lipid metabolism have been affected, and how much immune defense has been reduced. To do this, a general blood test is taken; sodium, potassium, calcium, protein and its fractions, and glucose are determined in venous blood; a lipid profile is performed. An electrocardiogram is required - this way you can judge how much the heart responded to changes in the electrolyte composition of the blood.
Treatment
The main task of doctors when diagnosing adrenal hemorrhage is to restore water and electrolyte balance , prevent dehydration and shock. This is possible thanks to the introduction of adrenal hormones - replacement therapy with minerals and glucosteroids is carried out.
The hormonal drugs Hydrocortisone or Prednisolone are administered intravenously. The child should be under regular medical supervision, since the first drug can cause the development of psychosis in the child.
In case of hemorrhage of infectious origin, it is necessary to eliminate it in a short time. For this purpose, antibiotic injections are prescribed. Dehydration can be prevented by administering saline solution, the side effect of which can be the development of edema. This is why the child needs constant monitoring during treatment.
If there is a risk of developing hemorrhage in the adrenal glands, Vikasol .
SITUATIONAL TASKS II CATEGORY OF COMPLEXITY
At autopsy: diffuse pneumosclerosis, chronic pulmonary emphysema, chronic pneumonia with a predominant lesion of the lower lobe of the left lung. Left-sided hydrothorax (350 ml), portal cirrhosis. Ascites (2800.0). “Pulmonary” heart: hypertrophy of the right ventricle of the heart (0.9 cm) and expansion of its cavity. Thromboembolism of the branches of the pulmonary artery. Polycystic kidney disease. Atherosclerosis of the aorta. Atherosclerotic nephrosclerosis.
At autopsy: The liver is dense, with a fine-grained surface. In the left lobe, the tumor is whitish-gray in color (histologically - cholangiocellular adenocarcinoma). Varicose veins of the esophagus. Splenomegaly (580.0), ascites (2500 ml). Cachexia. Atherosclerosis of the aorta and coronary arteries of the heart. Pulmonary edema.
A 53-year-old patient was taken to the neurological department unconscious and in serious condition. Blood pressure = 140/80 mm Hg. A lumbar puncture yielded blood-stained fluid. A day later, the patient died due to a decrease in cardiac activity.
At autopsy: moderate tension of the dura mater of the brain. The convolutions of the brain are flattened, the furrows are somewhat smoothed. The brain tissue on the section is full-blooded and swollen. In the area of the subcortical nodes of the left hemisphere, the tumor measures 3.0 x 3.0 cm, soft, without clear boundaries. There are hemorrhages around her and in her tissue, with blood escaping into the lateral ventricles of the brain. The vessels of the base of the brain and the coronary arteries of the heart have thickened walls and narrowed lumens. Their intima contains yellowish plaques. The myocardium is brownish, with small whitish layers of connective tissue. The thickness of the wall of the left ventricle of the heart is 1.2 cm. The liver, spleen, and kidneys are cyanotic. The lungs are swollen.
The patient (71 years old) has been suffering from hypertension for 20 years, five in the last three years.
Source
Forecast
Hemorrhage into the adrenal glands is fatal in most cases. This is largely due to the fact that in the first stages the disease is difficult to diagnose. At the same time, during hemorrhage, the synthesis of hormones stops, water-salt and carbohydrate metabolism is disrupted, and irreversible changes begin in the entire body.
This causes severe dehydration, neuropsychic and immune changes, gastric disorders, and then adrenal dysfunction.
At the same time, with timely treatment, there is a chance of a favorable outcome of the disease . However, even if the life of the newborn is preserved, complications such as chronic adrenal insufficiency and developmental disorders may occur.
Hemorrhages in the adrenal glands
Bilateral hemorrhage into the adrenal glands is the cause of acute adrenal insufficiency. In medical practice, this pathological condition is called Waterhouse-Friderichsen syndrome. Hemorrhage, or hemorrhagic infarction of the adrenal glands, often occurs against the background of a progressive infectious disease in the stage of decompensation.
Acute disruption of the blood supply to the adrenal glands leads to a complete or partial cessation of the formation of gluco- and mineralocorticoid hormones, which regulate water-salt, carbohydrate, immune metabolism and, in general, the homeostasis of the whole organism. Severe dehydration, collapse, neuropsychic and gastrointestinal disorders occur. If assistance is not provided at this stage, acute adrenal insufficiency develops into a coma, which ends in death.
The adrenal glands synthesize a large number of hormones that regulate important parameters of human life.
Causes of hemorrhages in the adrenal glands
In adults, the development of the syndrome is due to the following reasons:
- severe fulminant sepsis;
- extensive burns;
- thrombosis of adrenal vessels;
- systemic connective tissue diseases;
- pathology of pregnancy.
The listed diseases and pathological conditions, if left untreated and with a progressive course, ultimately lead to the formation of disseminated intravascular coagulation syndrome. In the vessels and capillaries of vital organs, the process of thrombus formation begins, blocking blood flow.
Intensive consumption of coagulation factors for the formation of blood clots quickly leads to their deficiency. At the next stage, the blood loses its ability to clot, and some of the formed elements and plasma leave the vascular wall.
This forms a hemorrhagic infarction in the adrenal tissue, which can subsequently become necrotic.
The most common cause of adrenal infarction in both adults and children is generalized meningococcal infection.
Table. Characteristics of the causes and mechanisms of development of hemorrhage in the adrenal glands
| Causes | Pathogenesis of development | Examples of diseases |
| Sepsis | Bacterial toxins, when released into the bloodstream, damage the vascular wall and activate blood clotting factors. | Meningococcal, streptococcal, staphylococcal infections, diphtheria, destructive purulent pneumonia, osteomyelitis, peritonitis and other diseases complicated by the generalization of the infectious process. |
| Burns | Shock from deep burns is accompanied by loss of plasma, decreased blood pressure and thickening of the blood. Toxins from necrotic tissues, entering the bloodstream, trigger the formation of blood clots. | Deep or widespread superficial thermal or chemical burns. |
| Systemic connective tissue diseases | The autoimmune process leads to the formation of circulating immune complexes, which are fixed on the vessel wall and can disrupt blood clotting processes. | Systemic lupus erythematosus, vasculitis, periarteritis nodosa |
| Pathology of pregnancy | In severe forms of gestosis, widespread vascular spasm and immune inflammation of the cells of the vessel wall occur. The result is activation of tissue thromboplastin (clotting factor). | Preeclampsia, eclampsia, amniotic fluid embolism, total placental abruption. |
Any septic or progressive autoimmune disease, any type of shock if medical care is not provided can lead to the formation of intravascular coagulation syndrome, the manifestation of which will be various bleeding and hemorrhages, including in the adrenal glands.
In newborns, adrenal gland damage is most often associated with trauma received during childbirth. This can occur during a prolonged period of expulsion of the fetus, clamping of the umbilical cord loops, or the application of obstetric forceps. Incorrect provision of obstetric care at birth (especially with breech presentation) can also cause hemorrhages in the adrenal glands in newborns.
Meningococcal infection is the most common cause of adrenal hemorrhage
General principles of treatment
With the development of acute adrenal insufficiency, the complex of treatment measures includes:
- hormone replacement therapy with gluco- and mineralocorticoid drugs;
- fluid therapy to combat dehydration and shock;
- restoration of electrolyte imbalance;
- treatment of concomitant disease (infection, autoimmune disease, etc.).
Treatment of newborns is also based on the use of hormone replacement therapy.
The prognosis for hemorrhages in the adrenal glands is serious, but with adequate and timely treatment, impaired functions can be compensated and possible negative consequences can be minimized.
Source: https://sksochi.ru/bolezni/krovoizliyaniya-nadpochechniki-detey-vzroslyh