Urolithiasis - urolithiasis - can be considered one of the most common pathologies in people. If we consider the population of the entire planet, this chronic disease is diagnosed in 1-3% of the population. At the same time, the localization of stones is different; in children and members of the older generation they form in the bladder, in young people and people of the middle age group - in the ureters or kidneys.
Urolithiasis (ICD 10) is also called nephrolithiasis and is a metabolic disorder caused by various reasons. Often this pathology is hereditary in nature, but the main symptom of the condition is the formation of stones in sections of the urinary system.
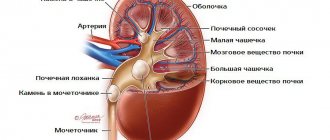
According to statistics, stones form three times more often in men than in women, but if we consider coral-shaped formations, in 70% they are found in the fairer sex. For the most part, the appearance of stones occurs in one of the paired organs, although in some cases (and this is from 9 to 17%), urolithiasis of the kidneys is bilateral. According to ICD 10, it is classified as a separate group of diseases. Kidney stones can be single or multiple, their number can reach about 5000 formations. The sizes can also be different, reaching from 1 mm to 10 cm or more. Their weight can be up to one kilogram.
According to the international classification of diseases - ICD 10 - the code of the pathology in question occupies positions No. 20-23:
- ICD code No. 20 indicates the formation of stones in the ureter or kidney;
- ICD 10 code No. 21 indicates the formation of stones in the lower sections of the urinary tract;
- if we consider the codes, No. 22 indicates that there are stones in the urinary tract that form as a result of diseases that are classified in other categories;
- Urolithiasis, code No. 23, is unspecified renal colic.
Reasons for the formation of stones
As for the reasons that cause the formation of urolithiasis, modern medicine has not yet reached a consensus. However, for the most part, the basis for the formation of urinary stones is metabolic disorders, which include an increase or decrease in the concentration of uric acid in the blood or urine, an increase in the level of phosphate, calcium salts and oxalates, and changes in the acidity of urine. Influencing factors that contribute to malfunctions and the appearance of urolithiasis include kidney pathologies, heredity, diseases of other internal organs, improperly structured nutrition, lack of fluid in the body, exposure to an unfavorable climate, and physical inactivity. Some of these factors should be considered in more detail:
- Heredity. Urolithiasis in humans can be transmitted genetically, which is greatly facilitated by a predisposition to increased levels of calcium in the circulatory system.
- Diseases of the kidneys and other organs. The risk of developing kidney stones increases if pathologies developing in the human body negatively affect the filtration abilities of the organ or lead to disruption of the metabolism of oxalates, cystine or urates. The list of such diseases may include pyelonephritis, kidney deformation, gout, inflammatory processes, and infections occurring in the intestines.
- Nutrition. Often the causes of urolithiasis in people are indulgence in their own food preferences and abuse of overly salty or sour foods, which negatively affect the functionality of the kidneys.
- Dehydration. If there is not enough fluid in the body of adults or children, it is not possible to remove a sufficient amount of harmful compounds, which results in the formation of kidney stones.
- Climatic conditions. The causes of urolithiasis may also include insufficiently favorable environmental conditions. For example, constant heat helps to reduce fluid content in the body, resulting in kidney damage.
- Physical inactivity. If it is present, metabolism deteriorates.
The list of reasons for the formation of urolithiasis includes increased sweating, because the more abundant and more often fluid is released through a person’s pores, the more actively the salts are concentrated, from which the stone is then formed.
Proven fact. A certain risk comes from both a lack of ultraviolet radiation and the water consumed, especially if the liquid has increased hardness and contains various salts.
Who is the operation indicated for?
Surgeons resort to removing the entire kidney only in emergency situations, when the patient’s condition does not require delay; in all other cases, they always try to preserve it as much as possible (that is, if possible, only the affected tissue is excised).
Radical nephrectomy is always a complex and lengthy procedure that requires the doctor to be highly trained, special skills and good knowledge of anatomy and surgery.
The main indications for complete kidney removal are as follows:
- Severe damage to the kidney tissue, violating its structural integrity, in which it is not possible to restore functional abilities, and there is also massive bleeding from the destroyed vessels.
- Multiple large stones in different structures of the organ with frequent relapses of renal colic.
- Tumor growth of large sizes, when it is not possible to completely remove it from the kidney tissue (more than 6-8 cm).
- Tumor growth into the lumen of large blood vessels (renal and inferior vena cava), into the surrounding adipose tissue, regional lymph nodes, or involvement of adrenal tissue in the pathological process.
- Diagnostically proven single metastases in the tissues of only one kidney, while the second kidney functions normally.
- Severe polycystic disease (most often acquired), which threatens the development of renal failure (ineffectiveness of adequate drug therapy).
- Severe anomalies in the development of the kidneys, when the organ is completely deprived of its functions, and at the same time there are violations that threaten the life and health of the patient.
- Purulent melting of kidney tissue, lack of effect from antibacterial therapy (threat of septic condition).
- Hydronephrosis with an increase in the size of the organ by more than 20% of its original volume, when conservative treatment does not restore the outflow of urine.
In case of polycystic degeneration of one of the kidneys, it is removed; a necessary condition is to preserve the functioning of the other
Partial nephrectomy is performed in the following categories of patients:
- The presence of a tumor or pathological focus of another origin, the size of which does not exceed 7 cm. It should not extend beyond the kidney and be located in anatomical areas convenient for surgical access (upper or lower pole). In this case, the process does not involve regional vessels and lymph nodes.
- In diseases of both kidneys, when the patient has signs of renal failure, and removing one of them will sharply worsen the patient’s well-being.
The most gentle treatment option is partial nephrectomy, in which a larger volume of the organ remains unchanged.
There is also a category of patients for whom even complete removal of an organ will improve their condition only temporarily and will not lead to a complete recovery. We are talking about patients with multiple metastases in the kidney tissues and other structures of the body. In this case, they resort to palliative nephrectomy, that is, the “non-functioning” kidney is removed. But at the same time, all metastatic foci remain in the patient’s body.
What do stones look like and how do they manifest themselves?
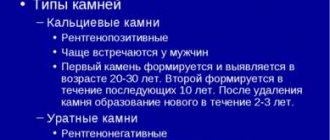
We talked about what urolithiasis is and why it appears in humans. Now let's look at what stones can form during urolithiasis and the symptomatic manifestation of the pathology. Concretions vary in chemical properties, dimensions, color shades and shape. The features of such formations are as follows:
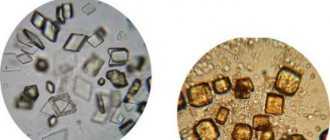
- Phosphate stones are based on calcium salts, a small amount of urates and oxalates. Their color is grayish or off-white. Characteristic features include rapid growth and gradual transformation into coral stones - the treatment of such a pathology is significantly difficult.
- The basis of oxalate formations is a dicarboxylic acid salt. The color of such stones is brown or brown, they are equipped with spikes, the structure is dense and heterogeneous. Oxalates can transform into coral formations and are diagnosed in the kidneys especially often.
- With urolithiasis, urate stones can form in men, although women are not immune from their occurrence. The peculiarity of such stones is their loose structure, smooth surface and beige tint.
- Xanthine stones have a brownish-red color, a round shape, and a very dense structure. The main problem is to cure such uric acid stone, since conservative methods cannot cope with it.
- Cystine formations are distinguished by their softness and homogeneity of structure, and are white with a pronounced yellow tint. Such stones often form in young people.
- Struvite formations are distinguished by their white color, soft and loose structure. Despite the fact that they increase in size quite quickly, therapy is not complicated.
Rehabilitation period
The patient's condition after surgery always requires a certain rehabilitation and postoperative recovery, the timing of which directly depends on the underlying disease, surgical approach, the severity of the patient's condition and concomitant pathology.
During the first 24 hours, all patients are recommended to remain strictly in bed to prevent complications, in particular, dehiscence of postoperative sutures.
During this period, patients wear compression stockings, do breathing exercises and smoothly move their limbs (this is necessary to prevent the formation of blood clots in the lumen of the blood vessels).
Eating light food is allowed only on the second day after the patient has undergone surgery. In this case, food should be according to the rules of a special diet, which excludes the intake of fatty and fried foods, spicy and spicy foods. Food is prepared only by steaming or boiling. The diet is expanded only when the patient has a full-fledged stool, without the use of enemas or laxatives.
In order not to burden the only healthy kidney, the volume of fluid taken should not exceed 2 liters per day.
On the second day after surgery, all patients are seated in bed (with the exception of severely ill patients). Sutures are usually removed on days 10-12, after which the patient is prepared for discharge. Those patients who underwent laparoscopic surgery are sent home after 5-6 days.
For 10 days, treatment with antibacterial drugs and painkillers is prescribed as needed (if the patient suffers from severe pain at the surgical site).
It must be remembered that complete recovery of the body occurs within a period of 12 to 18 months.
If there are any complications or disturbances in the activity of the remaining kidney, the patient is referred to a special commission (ITU), where the issue of establishing a disability group is decided.
The higher the patient’s immune status and the fewer concomitant diseases, the faster the rehabilitation process occurs.
The period after surgery requires the patient to comply with a number of requirements, thanks to which the risk of possible complications is minimized and the recovery process is accelerated. Such events include:
- daily walks, which can be combined with light exercise;
- adherence to the principles of proper nutrition and optimal drinking regimen;
- dose the level of physical activity;
- regular visits to the attending physician and timely completion of the necessary tests;
- taking necessary medications.
Principles of treatment of the disease in question
After the victim contacts and the diagnosis is confirmed, treatment of urolithiasis can be either conservative or surgical. The urologist determines exactly how to treat in a particular case, based on a number of factors:
- Age category of the victim.
- His general state of health.
- Localization of the stone and its dimensions.
- The stage of renal failure reached by the disease.
- Clinical course of the pathology.
- The presence of various changes - both anatomical and physiological.
Typically, effective treatment for urolithiasis requires surgery. This method may not be used in the presence of stones formed under the influence of uric acid, since there is a possibility of dissolving them. For this purpose, citrate mixtures are used for several months.
Even if it was possible to get rid of this formation surgically or the stone passed away on its own, no one is immune from relapse of the disease. Accordingly, not only medical examinations and treatment are required, but also preventive measures, the purpose of which is to prevent exacerbations. It will be necessary to maintain water balance, apply diet therapy, and use herbs when treating urolithiasis. You may need to take pharmaceuticals, undergo physical therapy, physiotherapy and balneology, or a trip to a sanatorium.
Surgical intervention is indicated in cases where the formation of large stones is observed, in the formation of renal failure, if other methods are contraindicated or unavailable.
Help in the presence of coral nephrolithiasis is provided by paying attention to the degree of dysfunction of the organ. If functionality is maintained at 80%, conservative therapy is prescribed. When indicators deteriorate by 20-50%, extracorporeal lithotripsy is performed. If kidney function continues to decline, surgery will be required to remove the stones.
Main surgical approaches and types of interventions
Removal of an organ or resection of its part occurs in two available ways:
- open (laparotomy) nephrectomy;
- closed (laparoscopic) nephrectomy.
Each of these approaches has its own advantages and disadvantages, and the preference in choosing each of them depends on the underlying disease, the severity of the patient’s condition and the extent of the process.
If we are talking about emergency surgical intervention, then patients are unconditionally referred to open surgery, thanks to which the doctor can assess the extent of the problem as much as possible and conduct a complete inspection of the lesion.
Before the kidney is removed, the renal “leg” is ligated - the place where large arteries and veins enter the organ, as well as the ureter
Diagnostic methods
To determine the causes of symptoms, the doctor examines the patient and takes a medical history.
It is important for specialists to know about the lifestyle, nutrition, type of activity, features of the manifestation of symptoms, previous surgical interventions, injuries and other aspects of the patient’s life.
To establish the characteristics of the disease and identify an accurate diagnosis, the following diagnostic methods are prescribed:
- Ultrasonography . Allows you to visualize formations, determine its location and size.
- CT and MRI . They are the most informative diagnostic methods, allowing one to assess the degree of development of the disease.
- Laboratory research . To determine the presence of inflammation in the body, biochemical and general blood tests, urine and stool tests are prescribed. A microflora culture is prescribed.
- Biochemical examination of the kidneys , which allows you to see the overall picture of the patient.
- Pneumopyelography , which can be used to identify radiolucent stones.
Based on the results obtained, the doctor determines the number and location of kidney stones, the general condition of the body and prescribes a course of therapy.
Characteristic symptoms and signs: how long does the attack last?
The leading symptom of renal colic is acute, cramping pain in the lower back, radiating to the groin and external genitalia. The attack occurs suddenly, its appearance is not associated with physical stress or other conditions. Unbearable pain does not disappear in any position and lasts from 2 to 15 hours .
The attack may also be accompanied by:
- nausea;
- vomiting;
- increased temperature;
- tachycardia;
- increased blood pressure;
- frequent urge to urinate.
Often the patient has blood in the urine , a decrease in the volume of urine or no urine at all.
In children, renal colic manifests itself as acute abdominal pain combined with nausea, vomiting, and indigestion. For this reason, difficulties arise with diagnosis. A characteristic symptom is dysuria. In pregnant women, colic is mistakenly mistaken for the onset of labor.
You can find out more about dysuria in our article.
Characteristics of code 25.4
With long-term non-healing ulcers on the gastric mucosa, a chronic form of the disease develops. According to ICD 10 gastric ulcer, this code means a complication of profuse (heavy) bleeding in the chronic stage or with an unspecified genesis. Hemorrhage in such cases is severe and does not subside. Urgent surgical care is required.
N20—N23 Urolithiasis
N20 Kidney and ureteral stones
- N20.0
Kidney stones - N20.1
Ureteral stones - N20.2
Kidney stones with ureteral stones - N20.9
Urinary stones, unspecified
N21 Stones of the lower urinary tract
- N21.0
Bladder stones - N21.1
Stones in the urethra - N21.8
Other stones in the lower urinary tract - N21.9
Stones in the lower urinary tract, unspecified
N22* Urinary tract stones in diseases classified elsewhere
- N22.0*
Urinary stones in schistosomiasis [bilharzia] B65.- - N22.8*
Urinary tract stones in other diseases classified elsewhere
N23 Renal colic, unspecified
Add a comment Cancel reply
List of classes
- Class I. A00-B99. Some infectious and parasitic diseases
Excluded: autoimmune disease (systemic) NOS (M35.9)
disease caused by the human immunodeficiency virus HIV (B20 - B24) congenital anomalies (malformations), deformations and chromosomal disorders (Q00 - Q99) neoplasms (C00 - D48) complications of pregnancy, childbirth and the postpartum period (O00 - O99) certain conditions arising in the perinatal period (P00 - P96) symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere (R00 - R99) trauma, poisoning and some other consequences of external causes (S00 - T98) endocrine diseases, nutritional disorders and metabolic disorders (E00 - E90).
Note. All neoplasms (both functionally active and inactive) are included in class II. The corresponding codes in this class (for example, E05.8, E07.0, E16-E31, E34.-) can, if necessary, be used as additional codes to identify functionally active neoplasms and ectopic endocrine tissue, as well as hyperfunction and hypofunction of the endocrine glands, associated with neoplasms and other disorders classified elsewhere.
Description 25.3
Acute (when epithelial damage is diagnosed for the first time) stage of the disease without complications such as bleeding and perforation. Most often localized on the anterior wall and lesser curvature. It begins acutely with severe pain and dyspeptic disorders. The lesions are oval or round in shape up to 2 cm with clear hyperemic edges.
Code 25.5 according to ICD 10
This category is characterized by symptoms similar to other acute diseases of the abdominal cavity (pancreatitis, cholecystitis). In an unspecified or chronic course of the disease, the perforated hole is exposed, and peritonitis develops (inflammation of the abdominal cavity with a general severe condition of the body). All the conditions necessary for the formation of a limited abscess (abscess, purulent inflammation of the abdominal cavity, enclosed in a pyogenic capsule) occur.
Results
Renal colic is a disease that is difficult to miss in the practice of any doctor, since the patient presents active complaints and his condition worsens.
In addition, if the power is not provided in a timely manner, serious consequences for the body can occur. The most dangerous among them are the development of intoxication of the body, as well as hydronephrosis. The latter condition is characterized by the development of irreversible consequences.
You should not self-medicate; traditional methods should only be used with the advice of a specialist.
If you follow a few rules of proper nutrition, move more, and get rid of bad habits, then the likelihood of getting sick is very low.
Organization of medical care
Indications for hospitalization:
- Unconfirmed diagnosis (especially after 60 years for differential diagnosis with an aneurysm);
- Intractable or frequently recurrent pain attack;
- Signs of a urinary infection;
- Stone larger than 7 mm;
- Single or transplanted kidney;
- Anuria, oliguria;
- Inability to quickly outpatient examination and observation;
- Repeated visits with renal colic due to the same cause;
- Pregnancy;
- Bilateral nephrolithiasis
Indications for discharge of a patient from the hospital with renal colic:
- The pain syndrome is permanently relieved
- The size of the stone allows conservative lithokinetic therapy
- Drainage has been completed and staged treatment is planned.
- The causes of obstruction have been eliminated.
Outpatient consultation with a urologist within 7-14 days.
When a patient is discharged with a stone whose spontaneous passage is unlikely, hospitalization for surgical treatment is planned within 4 weeks.
Urolithiasis (N20-N23)
Included: calculous pyelonephritis.
Excludes: with hydronephrosis (N13.2)
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Description of code 25.6
The slow development of symptoms in a chronic course, the duration of the course with periods of exacerbation and attenuation of symptoms often leads to complications with bleeding and perforation at the same time. This group is classified according to the predominant symptoms or morphological characteristics.
Clinical picture of a perforated ulcer complicated by atypical bleeding:
- there may be no pronounced pain syndrome or tension in the abdominal muscles;
- there are no symptoms of peritoneal inflammation.
A rare case of a combination of bleeding with perforation according to international classification code 25.6—a perforated ulcer of the anterior wall and hemorrhage on the posterior side of the stomach (kissing ulcers)—finding the location of the perforated and wound ulcers in this case is difficult.
Description according to code 25.1
The acute phase of a peptic ulcer with perforation (perforation) is a penetrating (through) hole at the site of ulceration. Occurs in silent (asymptomatic) infections.
There are two forms:
- covered (by other organs, without constant pouring of contents into the abdominal cavity);
- naked (the contents of the stomach constantly exit into the cavity between the organs).
Characteristics of code 25.7
A chronic gastric ulcer without perforation and hemorrhage of this code according to ICD 10 develops when it is impossible to heal an acute ulcer. Symptoms develop slowly, sometimes without pain. For a long period, only symptoms common to diseases of the digestive system are present: nausea, heartburn, heaviness after eating. Gradually, the symptoms increase, at the same time complications develop and the disease passes into another code.
Description by code 25.0
A complication of the acute stage of the disease occurs as a result of arrosion (violation of the integrity of the walls during necrotic and ulcerative processes) of the vessel, with disturbances in the outflow of venous blood.
Clinic complications:
- dizziness;
- pale skin;
- weakness;
- collapse (sudden cardiovascular failure with loss of consciousness and death);
- melena (black, shapeless stool with an unpleasant odor, a mixture of blood with the contents of the intestines and stomach);
- single or repeated vomiting, including masses of the type of coffee grounds;
- hypotension (low blood pressure);
- acute pain (may be absent).
Decoding 25.2
Acute stage of gastric ulcer, complicated by both bleeding and perforation of ulcers.
Symptoms:
- health is at a consistently good level;
- weakness;
- confusion;
- dizziness;
- bloody vomiting;
- melena;
- hypotension (low blood pressure) or hypertension (high blood pressure);
- acute increasing pain.