PYELOGRAPHY
(Greek, pyelos trough, vat + grapho write, depict) - x-ray examination of the kidney after filling the collecting system with a contrast agent.
Rice.
1. Retrograde right-sided pyelogram is normal: 1 - calyces, 2 - pelvis, 3 - ureter. Depending on the route of administration of the contrast agent, retrograde (or ascending) and antegrade P. are distinguished. In the case of contrasting only the ureter, they speak of retrograde ureterography. In retrograde P., the contrast agent is injected into the pelvis or ureter; in antegrade P., the contrast agent is injected directly into the pyelocaliceal system by percutaneous puncture or through a pyelonephrostomy. Retrograde P. was proposed in 1906 by F. Voelcker and A. Lichtenberg. In some cases, instead of a liquid contrast agent, gas is injected into the pyelocaliceal system, for example, oxygen or carbon dioxide (pneumopyelography), and double contrast is also used, based on the simultaneous use of liquid contrast agents and gas. Thus, according to the method proposed in 1954 by R. Klami, a mixture of a liquid contrast agent with a 3% solution of hydrogen peroxide is administered, which, when it comes into contact with purulent exudate in the urinary tract, decomposes into water and oxygen. Using a series of sequential images (serial P.), you can obtain approximate information about the motor function of the urinary tract if excretory urography is contraindicated (see). P. gives an idea of the anatomo-morphol. features of the collecting system of the kidneys, and with simultaneous contrasting of the kidneys and ureter (retrograde pyeloureterography) - about the upper urinary tract as a whole. With P.'s help, the shape, size, position of the pelvis and calyces, their number, relative position (Fig. 1), the presence or absence of patol, changes are determined. In this case, even minor destructive processes in the renal papillae and calyces can be detected.
Target
- Identify the cause of upper urinary tract obstruction - stricture, stone, blood clot, tumor.
- Confirm the diagnosis of hydronephrosis based on the results of excretory urography or ultrasound and facilitate the establishment of nephrostomy drainage.
- To assess the functional state of the upper urinary tract after surgical interventions on the ureter and urinary diversion operations.
- Assess the reserve capacity of the kidney before the upcoming surgical intervention.
Preparation
- The patient is explained that antegrade pyelography is an X-ray examination of the kidney.
- The patient should refrain from eating and drinking for 6-8 hours before the test.
- The patient should be warned that before and after the study he may be prescribed antibacterial therapy.
- The patient is informed who will perform the study and where.
- It should be explained to the patient that before puncture of the renal collecting system, he will be given sedatives and local anesthesia, that the urine pumped out during puncture will be examined, and in order to drain the upper urinary tract, a nephrostomy tube may be left in the kidney.
- During the administration of local anesthetic and contrast agent, the patient may experience minor discomfort. In addition, during the administration of a contrast agent, a transient burning sensation or flushing of blood to the face may be observed.
- The patient is warned that during the examination (while taking pictures) he will hear loud clicking sounds.
- It is necessary to find out whether the patient is allergic to radiocontrast agents, iodine and foods rich in iodine (for example, shellfish). All cases of an allergic reaction must be recorded in the medical history. You should also find out whether the patient has diseases accompanied by increased bleeding.
- It is necessary to ensure that the patient or his relatives give written consent to the study.
- Before the procedure, the patient is sedated and all blood tests (including kidney function assessment) have been completed.
What is this?
Pyelography is a type of x-ray examination, the purpose of which is to determine the condition of the renal tubules and pelvis . The essence of the study is that the patient is injected with a radiopaque substance, which gradually fills the renal structures. This happens quite quickly, after which one or more x-rays of the lumbar region and pelvis are taken.
The need for a contrast agent is due to the fact that the kidneys, like most soft tissues, are quite poorly visible on an x-ray. And their individual structures are indistinguishable without contrast, since they have approximately the same X-ray density.
The picture will show:
- Anomalies in the structure of the renal tubules, pelvis and ureters.
- Breaks of the specified structures.
- Stones and foreign bodies.
- Narrowings, kinks, adhesions in the urinary tract.
Procedure and aftercare
- The patient is placed on the X-ray table on his stomach. The skin in the area of the intended puncture is treated with an antiseptic solution. Local anesthesia is performed.
- To determine anatomical landmarks, previously taken x-rays or filmed ultrasound results of the kidney are studied. (This only matters if the kidney is in its usual place. Otherwise, the angle of the needle is corrected during the percutaneous puncture.)
- Under the control of fluoroscopy or ultrasonography, the puncture needle is passed below the XII rib at the level of the transverse process of the II lumbar vertebra. The discharge of urine through the needle confirms its location in the expanded pyelocaliceal system (in adult patients the needle has to be inserted an average of 7-8 cm in depth).
- To prevent the needle from moving during the examination, a flexible tube is connected to it. To measure intrapelvic pressure, the tube is connected to a manometer. If necessary, a urine sample is taken.
- To prevent overstretching of the collecting system, a volume of urine is evacuated from it equal to the amount of contrast agent that is planned to be administered.
- The contrast agent is administered under fluoroscopic control. Pictures are taken in posteroanterior, semilateral and anteroposterior projections. To determine the location and degree of ureteral obstruction, fluoroscopic monitoring of the progress of the contrast agent is performed.
- When intrapelvic pressure increases, dilation of the upper urinary tract, as well as intrarenal reflux, when drainage of the collecting system is necessary, a nephrostomy tube is installed in the kidney. If there is no need for drainage, the catheter is removed and a sterile bandage is applied to the puncture site.
- Monitor vital signs for 24 hours (every 15 minutes for the first hour, every 30 minutes for the second hour, then every 2 hours).
- The condition of the bandage is checked at the same frequency; this is necessary for timely diagnosis of bleeding, hematoma or urinary leakage. If there is bleeding, apply a pressure bandage. When a hematoma forms at the puncture site, warm compresses are prescribed. If, within 8 hours after the examination, urine continues to leak from the puncture canal or spontaneous urination is absent, you must notify the doctor.
- Fluid intake and diuresis are monitored for 24 hours. Each urine sample is examined for gross hematuria. If hematuria does not stop after the third urination, notify the doctor.
- Particular attention should be paid to the appearance of signs of urinary sepsis or reflux of the contrast agent into the systemic circulation (chills, fever, rapid pulse, rapid breathing, arterial hypotension).
Warning.
Be alert for signs of possible damage to other organs, such as abdominal or flank pain, pneumothorax, indicated by sudden onset of chest pain when breathing, shortness of breath, decreased vocal tremors on the affected side, and tachycardia.
- When installing a nephrostomy tube, it is necessary to monitor its patency and the adequacy of drainage of the upper urinary tract. Use 5~7 milliliters of sterile saline to flush the tube.
- After the study, antibacterial drugs and painkillers are prescribed.
- In patients with hydronephrosis, the amount of fluid drunk and diuresis are taken into account, the dynamics of edema, arterial hypertension, pain in the lumbar region, acid-base balance and blood glucose levels are monitored.
Kinds
There are several types of urinary tract examinations, which differ in the way the contrast agent is administered. retrograde pyelography was the first to be used , and it is also the simplest method of performing the procedure.
In this case, the patient is administered the substance through the bladder. Most often it is performed together with cystoscopy, since both procedures are very painful, especially for men.
The advantages of retrograde injection of contrast in a clear image, the disadvantage is a high risk of damage to the mucous membrane of the urinary tract, the risk of overstretching the renal pelvis.
Intravenous pyelography (excretory urography) is performed less painfully for the patient. Contrast is injected into a vein, after which it waits until it fills the kidney structures and several pictures are taken.
- Retrograde pyelography. Retrograde urography Indications and Contraindications
The advantage of the method is a very detailed image of the renal tubules, the ability to observe the output of the contrast agent over time and indirectly assess the filtration rate.
Disadvantages - risk of systemic side effects due to intravenous administration of contrast, higher radiation dose than with other methods.
Antegrade pyelography is performed when it is not possible to perform the procedure retrograde. The essence of the method is that a catheter or thick needle is inserted into the renal pelvis, through which the contrast goes directly into the urinary tract. The procedure is very risky, since it is performed in conditions of impaired outflow of urine from the kidneys.
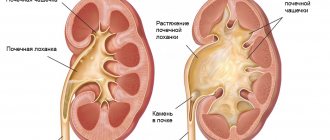
Deviation from the norm
Dilatation of the upper urinary tract indicates the presence of obstruction in the underlying sections. Antegrade pyelography allows you to determine the severity of dilatation, the level of obstruction and the presence of intrarenal reflux. With hydronephrosis, a narrowing of the ureteropelvic segment and an expansion of the pyelocaliceal system are noted. The method also allows one to obtain a clear image of the upper urinary tract after recent surgery (for example, visualization of a ureteral stent or prestenotic dilatation). Intrapelvic pressure exceeding 20 cm of water. Art., indicates obstruction. The results of bacterial or cytological examination of a urine sample obtained during antegrade pyelography can confirm the diagnosis of pyelonephritis or tumor.
Factors influencing the result of the study
- The presence of gas and feces in the intestines or residual contrast with barium after an X-ray examination of the gastrointestinal tract (poor image quality).
- Obesity (poor image quality).
BH Titova
"Antegrade pyelography" and others
> X-ray (pyelography) of the kidneys, types of pyelography
This information cannot be used for self-medication! Consultation with a specialist is required!
What is pyelography and how is it performed?
Pyelography is an X-ray examination of the kidneys with preliminary filling of the urinary tract with a contrast agent. Using pyelography, the size, shape, location of the calyces and pelvis of the kidneys, the structure and function of the ureters are assessed.
Most often, retrograde (ascending) pyelography is performed. In this case, the contrast agent is injected through the ureter using a catheterization cystoscope. Antegrade (descending) pyelography is usually used in cases where, due to obstruction of the ureter, it is impossible to administer contrast through it, or when the patient has contraindications to cystoscopy. In the descending version of the study, contrast is injected directly into the renal collecting system by puncture or by installing a drainage.
The contrast can be a liquid, a gas (pneumopyelography), or both at the same time (double contrast).
Indications for pyelography
Pyelography is prescribed to confirm the diagnosis of hydronephrosis, pyelonephritis, urolithiasis or cancer. The images visualize tumors, stones, blood clots and other obstacles to the passage of urine. The study helps surgeons plan the course of the upcoming operation.
Who sends you for the study, and where can you get it?
Nephrologists, urologists, oncologists, and surgeons refer for pyelography. It is advisable to undergo it in a treatment or diagnostic medical center equipped with an X-ray machine and specializing in the diagnosis and treatment of pathologies of the urinary organs.
Contraindications for pyelography
The study is contraindicated in case of hypersensitivity to contrast and during pregnancy. The retrograde technique is not used in cases of impaired patency of the ureters, insufficient bladder capacity, hematuria (presence of blood in the urine), and the antegrade method is not used in cases of blood clotting disorders.
Preparation for pyelography
Method of performing pyelography
When performing retrograde pyelography, the patient lies on a special table with his legs bent at the knee and hip joints, the position of which is fixed with special stirrups. After preliminary anesthesia, the doctor inserts a cystoscope into the bladder, and through it to the level of the renal pelvis - a special catheter. Under X-ray guidance, a contrast agent is slowly injected through the catheter. When the required filling of the collecting system is achieved, radiographs are taken in the anteroposterior projection, and in some cases additionally in semilateral and lateral projections.
When performing antegrade pyelography, the patient lies on a special table with his back up. After preliminary local anesthesia, the doctor inserts a needle into the collecting system (below the level of the 12th rib) to a depth of approximately 7–8 cm and connects a flexible tube to it. Under fluoroscopic control, a contrast agent is injected through it. Then radiographs are taken in posteroanterior, anteroposterior and semilateral projections.
Interpretation of pyelography results
Normally, the passage of the contrast agent through the catheters occurs without difficulty, the calyces and pelvis of the kidneys fill quickly, have smooth, clear contours and normal sizes. Kidney mobility (assessed during inhalation and exhalation) should not be more than 2 cm.
Incomplete filling of the upper urinary tract with contrast, its dilation, and delayed emptying after catheter removal indicate the presence of a tumor, stone, or other obstruction. Impaired kidney mobility may indicate pyelonephritis, paranephritis, tumor or kidney abscess. With hydronephrosis, the renal collecting system dilates.
The results of the study (images and the radiologist’s report) should be shown to the doctor who referred for pyelography.
Imaging techniques are often used to evaluate patients with nephrological and urological pathologies.
Plain radiography without contrast
An X-ray of the abdominal cavity without the use of radiocontrast agents is practically useless in the diagnosis of nephrological and urological diseases. Such radiography is insensitive, capable of detecting only 50-60% of kidney stones (calcium oxalate stones and rarely staghorn stones), and the detection of calcifications resembling stones is also nonspecific.
X-ray using contrast
Images obtained after administration of water-soluble contrast agents allow visualization of the kidneys and collecting system. Currently, non-ionic isosmolar drugs (iohexol, iopamidol) are widely used; they have fewer side effects than the older hyperosmolar drugs, but still pose a risk of acute kidney injury (radiographic nephropathy).
In urography, the image is taken after intravenous, percutaneous antegrade or retrograde, or cystoscopic retrograde administration of a radiocontrast agent. The main contraindications for all patients are allergies to iodine and risk factors for radiocontrast nephropathy.
IVU (IV urography or pyelography)
. IVU has been widely replaced by the rapid introduction of multislice CT and MRI with and without contrast agents. During IVU, abdominal compression and increased intra-abdominal pressure can improve visualization of the renal pelvis and the proximal ureters (when it is created), and the distal ureters (after it is removed). Additional radiographs at 12 and 24 hours after contrast administration may be indicated to identify postrenal obstruction or hydronephrosis.
Percutaneous antegrade urography
. When performing percutaneous antegrade urography, a radiopaque contrast agent is administered through the existing nephrostomy drainage or, less commonly, after percutaneous puncture of the pelvis under X-ray control. In some cases, ureterostomy or puncture of the intestinal reservoir may be used.
Antegrade urography is used in the following circumstances:
- When retrograde urography cannot be performed (for example, due to obstruction by a tumor at the level of the bladder).
- When should large kidney stones be visualized for which percutaneous assistance is required?
- When the presence of transitional cell carcinoma of the upper urinary tract is suspected.
- When patients cannot tolerate general anesthesia or the required degree of sedation for retrograde urography.
Complications associated with puncture and installation of drainage in the genitourinary tract and include bleeding, sepsis, damage to adjacent organs, microhematuria, pain and urinary extravasation.
Retrograde urography
. Retrograde urography uses cystoscopy and ureteral catheterization to inject radiopaque contrast directly into the ureters and renal collecting systems. Sedation or general anesthesia is required. The technique is used when CT or MRI are necessary (for example, to accurately localize and determine the nature of the obstruction), but their implementation is ineffective.
It can also be used to study in detail the anatomy of the collecting system, ureters (for example, in the diagnosis of ureterovaginal fistulas) and the bladder. However, overdistension and reverse flow of fluid can distort the contours of the cups and hide detailed features of their anatomy. The risk of infection is higher than with other types of urography. Acute swelling of the ureteral mucosa and the formation of iatrogenic strictures are rare complications.
Cystourethrography
. In cistrourethrography, a radiopaque contrast agent is injected directly into the urethra and bladder. This technique provides more detailed information than other imaging studies for diagnosis.
Victory cystourethrography is performed during urination and is used to diagnose posterior urethral valves. No special preparation of the patient is required. A relative contraindication is extended urethral strictures.
Angiography
. Traditional angiography using vascular catheters has been widely replaced by non-invasive vascular imaging techniques (eg, magnetic resonance angiography, CT angiography, ultrasound, radionuclide scanning). Remaining indications include measurement of renin levels in the blood of the renal veins, and, among patients with renal artery stenosis, angioplasty and stenting. Arteriography is rarely used for the diagnosis and treatment of renal bleeding and before organ-sparing kidney surgery. Digital subtraction angiography is no longer used given the availability of rapid serial multidimensional or helical CT.
Ultrasonography
Doppler ultrasound is commonly used to visualize the renal arteries, kidneys, bladder, etc. The test is safe, but does not provide information about renal function, and renal images are difficult to obtain in obese patients. Also, there is no way to improve the discrimination between tissue types, and image quality depends on the examiner. Ultrasound examination can determine the volume of urine after urination (residual urine volume). Doppler ultrasound in patients with testicular pain helps distinguish torsion from other causes by assessing testicular blood flow.
CT scan
CT scans can provide a complete picture of the urinary tract and surrounding structures. In most cases, conventional or spiral tomographs are used with or without the introduction of intravenous radiocontrast agents. The use of contrast agents in any technique is similar to the IVU procedure, but can provide additional information. Native multislice CT is the method of choice for imaging urinary stones. It is also best to avoid the use of radiocontrast agents for CT scanning of kidney injuries and other pathology, which may include acute bleeding (it may appear bright white and may be confused with contrast agent) and urinary extravasation. CT angiography is a less invasive alternative to traditional angiography.
Magnetic resonance imaging
MRI is safer than CT for patients at risk of radiopaque nephropathy and does not expose patients to ionizing radiation. Applications include all of the following:
- Differential diagnosis of kidney cysts complicated by hemorrhage and infection.
- Determination of the degree of tumor invasion into the bladder wall.
- High-quality visualization of the pelvic and genital organs using a pelvic or endorectal coil.
Magnetic resonance angiography, used to improve visualization of blood vessels, has almost completely replaced traditional angiography in the diagnosis of renal artery stenosis and renal vein thrombosis in patients with normal renal function. However, nephrogenic systemic fibrosis remains a dangerous side effect of gadolinium-based contrast agents. MRI does not visualize intrarenal calcifications well because... the latter contain few free protons. MRI with intravenously injected lymphotropic superparamagnetic nanoparticles (for example, monocrystalline iron oxide) can detect lymphatic metastases in prostate cancer, but is not available everywhere.
Radionuclide scanning
Cortical radiopharmaceuticals that have affinity for proximal tubular epithelial cells (for example, technetium-99m-dimercaptosuccinic acid [99m Ts-DMSA) are used to visualize the renal parenchyma. Excreted markers that are rapidly filtered and excreted into urine (eg, iodine-125-iothalmate, technetium-99m-diethylenetriamine pentaacetic acid (DTPA), technetium-99m-mercaptoacetyl-triglycerol-3 (MATG)) are used to estimate GFR and integral renal function. blood flow. Radioisotope scanning can be used to assess renal function when the use of intravenous radiocontrast agents is not advisable. Radioisotope scanning also provides more information than IVU or cross-sectional scanning on the following:
- Emboli in the segmental branches of the renal arteries.
- Scarring of the renal parenchyma due to vesicoureteral reflux.
- Functional significance of renal artery stenosis.
- Kidney function in a living donor before transplantation.
Technetium-99m-pertechnetate can be used to visualize testicular blood flow and to differentiate torsion from epididymitis in patients with acute testicular pain, although Doppler ultrasound is more often used because it is faster. No special preparation is required for a radionuclide scan, but patients should be asked about any known allergies to the radiopharmaceutical.
Intravenous Pyelogram - Topic Guide
What is an intravenous pyelogram (IVP)?
Intravenous pyelography refers to a series of x-rays taken from the kidneys, their collection or drainage system (ureters) and bladder. The ureters are small tubular structures that connect the kidneys to the bladder.
- An intravenous pyelogram (IVP) may be performed to identify problems in the kidneys, ureters, and bladder. IVP is most often performed to detect suspected obstruction of urine flow through the collection system. The most common cause of blockage is a kidney stone. The IVP test also provides information about kidney function.
- In the IVP test, dye is injected through a catheter inserted into a person's vein, usually in the arm or forearm. X-rays are then taken to follow a path of dye through the system.
What are the risks of an intravenous pyelogram?
Dyes (also called radiocontrast media) come in two types: ionic and non-ionic. Both types of dye contain iodine, but differ in two key ways: the rate of adverse reactions and cost.
Although the overall rate of adverse reactions is relatively low with both, a higher incidence of adverse reactions is observed with the less expensive ionic dye than with the nonionic dye.
- Minor reactions, which are infrequent and short-lived, include flushing, nausea, vomiting and itching.
- A small percentage of people experience a serious reaction to the dye, such as difficulty breathing, speaking, or swallowing; swelling of the lips and tongue; low blood pressure; or loss of consciousness. People who have had a serious reaction after receiving the dye once should not undergo it again.
- Pregnant women should not have IVP due to the risk of radiation exposure to the unborn child.
- People with known kidney disease or damage should not have IVP because the dye may worsen kidney function.
- Older adults and people with diabetes, high blood pressure, heart disease, or evidence of dehydration are at risk of developing kidney failure after dye injection. To avoid this complication, kidney function should be tested with a blood test for creatinine, and the results should be known before IVP is performed.
- Those with diabetes who take metformin (Glucophage) will need to
Urological manipulations
Some manipulations are used only for diagnosis, and some for treatment.
Bladder catheterization
Bladder catheterization is used for the following purposes:
- Obtaining a urine sample for testing.
- Measurement of residual urine volume.
- Resolving urinary retention or incontinence.
- Delivery of radiopaque contrast agents or medications directly to the bladder.
- Bladder rinsing.
Catheterization can be performed through the urethra or suprapubic access.
Catheters
. Catheters vary in gauge (thickness), tail configuration, number of strokes, balloon size, material type, and length.
Gauge is described in French (F) units, also known as Charrière (Ch) units. Each unit represents 0.33 mm, so the 14Ch catheter has a diameter of 4.6 mm. Sizes range from 14 to 24 Ch for adults and from 8 to 12 Ch for children. Smaller catheters are usually sufficient to allow urine flow in the absence of preexisting disease and are suitable for use in urethral strictures.
Most catheter tips have a straight configuration (eg, the whistle tip of a Robinson catheter) and are used for single-use catheterizations. Foley catheters have a straight tip and an inflatable balloon that is used to hold itself in the bladder. Other self-retaining catheters may have a flared mushroom cap tip (Pezzer catheter) or a four-winged mushroom cap tip (Malecote catheter); they are used for suprapubic catheterization or nephrostomy. Curved catheters, which may have self-retaining balloons, have a curved tip to facilitate passage through strictures and obstructive sites (eg, prostatic urethra).
All catheters used for long-term urine drainage have passages. Many catheters have ports for balloon inflation, irrigation, or both (eg, 3-way Foley catheter).
Balloons on self-retaining catheters come in a variety of volumes, from 2.5 to 5 ml in balloons intended for use in children and from 10 to 30 ml in balloons used in adults. Large balloons and catheters are commonly used to treat bleeding.
Stylets are flexible metal guides inserted into the lumen of the catheter to stiffen it and facilitate passage through strictures and obstructive areas.
The material of the catheter depends on the purpose of its use. Plastic, latex, or polyvinyl chloride catheters are intended for single use. Latex-silicone, hydrogel, or polymer (to reduce bacterial contamination) catheters are intended for continuous use.
Urethral catheterization
. A urethral catheter can be inserted by any doctor and sometimes by the patient himself. No patient preparation is required; therefore, unless the urethral route of catheterization is contraindicated, the bladder is catheterized through the urethra. Relative contraindications include the following:
- Urethral strictures.
- Current UTIs.
- Reconstructive urethral surgery or bladder surgery.
- Urethral injuries.
After thoroughly cleaning the external opening of the urethra with an antibacterial solution under conditions of strict sterility, the catheter is lubricated with sterile gel and carefully passed through the urethra into the bladder. To help reduce discomfort, lidocaine gel may be injected into the male urethra before the catheter is inserted.
Complications of bladder catheterization include all of the following:
- Trauma to the urethra or bladder with bleeding or microhematuria (common).
- Urinary tract infection
- Creation of false moves.
- Scarring and stricture formation.
- Bladder perforation. Suprapubic catheterization.
Suprapubic catheterization for percutaneous cystostomy is performed by a urologist or other experienced physician. No preliminary preparation of the patient is required. Common indications include the need for long-term bladder drainage and the inability to pass a catheter through the urethra or contraindications to the use of a catheter if catheterization is necessary.
Contraindications include the following:
- Inability to determine the position of the bladder clinically or ultrasound.
- Empty bladder.
- Suspicion of adhesions.
After local anesthesia of the abdominal wall in the suprapubic region, a spinal needle is passed into the bladder; If possible, use ultrasound guidance. The catheter is then placed through a special trocar or along a string passed through a puncture needle. A history of surgery in the lower abdominal cavity is a contraindication to blind needle placement. Complications include urinary tract infection, intestinal damage, and bleeding.
Cystoscopy
Cystoscopy involves inserting a rigid or fiber optic instrument into the bladder.
Indications include the following:
- Help in diagnosing urological pathology.
- Treatment of urethral strictures.
- Access to the bladder for radiological visualization of the ureters or placement of JJ stents.
The main contraindication is active UTI.
Cystoscopy is usually performed on an outpatient basis using local anesthesia or, if necessary, sedation or general anesthesia. Complications include urinary tract infection, bleeding, and trauma to the urethra and bladder.
Biopsy
Carrying out a biopsy requires the presence of a qualified specialist (nephrologist, urologist or interventional radiologist).
Kidney biopsy
. Indications for diagnostic biopsy include idiopathic nephritic or nephrotic syndrome or acute renal impairment. A biopsy is sometimes used to evaluate response to treatment. Relative contraindications include bleeding diathesis and uncompensated arterial hypertension. Moderate preoperative sedation with benzodiazepines may be required. Complications are rare but may include renal bleeding, which requires blood transfusion, radiological or surgical intervention.
Bladder biopsy
. Bladder biopsy is indicated to diagnose specific pathology and in some cases to assess response to treatment. Contraindications include hemorrhagic diathesis and acute tuberculous cystitis. Preoperative antibiotic therapy is only necessary if there is an active UTI. The biopsy instrument is inserted into the bladder through a cystoscope; rigid or flexible instruments can be used. The biopsy site is coagulated to prevent bleeding. A drainage catheter is left in place to facilitate healing and drainage of clots.
Prostate biopsy
. A prostate biopsy is usually performed to diagnose prostate cancer. Contraindications include bleeding diathesis, acute prostatitis and UTI. Patient preparation includes stopping aspirin a week before the biopsy, taking a preoperative antibiotic (usually a fluoroquinolone), and a cleansing enema. In the lateral position, the position of the prostate is determined by palpation, or, more preferably, with an ultrasound probe. The tissues overlying the prostate (perineum or rectum) are anesthetized, then a spring-driven biopsy needle is inserted into the prostate tissue and usually 12 columns of tissue are obtained.
Complications include the following:
- Urosepsis.
- Bleeding.
- Urinary retention.
- Hematuria.
- Hemospermia (often up to 3-6 months after biopsy).
Bougienage of the urethra
Urethral dilation is performed to treat the following conditions:
- Urethral stricture.
- Urethral syndrome (with urge urinary incontinence).
- Meatostenosis.
Contraindications include untreated infection, bleeding diathesis, extended strictures, and severe urethral scarring.
In the case of a stricture, a thin thread-like guidewire is passed, then bougies of successively increasing diameter are attached to the distal end of the thread-like guidewire and passed behind it until the urine stream is adequate. Usually the procedure is performed in several sessions. Facebook
Standard intravenous pyelography
Standard intravenous pyelography is a relatively valuable examination method for lesions of the renal vessels, allowing one to determine the size and anatomical structure of the kidneys, as well as identify intra- or extra-renal formations. However, if a diagnosis of kidney or renal vascular disease is established, in almost 40% of patients the pyelogram may not be changed. Patients with glomerulonephritis are recommended to undergo a kidney biopsy.
Indications for renal angiography are signs of renal vascular damage identified during CVD, increased plasma renin activity, severe hypertension in the anamnestic data on umbilical artery catheterization. In approximately 55% of cases in patients with pathology of the renal vessels, a murmur can be heard during auscultation of the abdominal cavity , but it is detected in almost 40% of children in whom there are no changes on the angiogram. During arteriography, the level of renin in the renal vein should be determined.
Plasma renin activity is studied against the background of standardized sodium intake. The most reliable data are obtained when blood is taken with the patient lying on his back and standing at intervals of 2-4 hours. Contraceptives or antihypertensive drugs reduce the reliability of the results. Aldosterone testing should also be standardized to urinary sodium levels. In most patients with pathology of the adrenal cortex or pheochromocytoma, data from the anamnesis and physical examination indicate the need to determine the urinary excretion of catecholamines, 17oxysteroids and 17ketosteropds. When diagnosing pheochromocytoma, its location should be clarified. To do this, blood is taken sequentially along the inferior vena cava. This should be done with caution against the background of alpha-adrenergic blockade.
The diagnosis of essential hypertension can be assumed based on the patient’s age, race, blood pressure, obesity and scanty symptoms of the disease. A history may indicate a family history of hypertension or coronary artery disease, as well as excess salt intake.
The course and prognosis depend on the nature of the underlying disease. Previously disappointing mortality data, especially in patients with renal hypertension, have now become somewhat more reassuring due to the widespread introduction of dialysis, kidney transplantation and active drug treatment. When the ratio of renin activity in the blood flowing from each kidney is more than 1.5 in a patient with renovascular hypertension, it is a sign of a favorable outcome of the operation. Newborns with this pathology respond successfully to drug treatment; In most of them, medications can be discontinued several months after starting treatment. Early diagnosis and surgical treatment for coarctation of the aorta has reduced the level of late complications and mortality in this disease. Although 90% of untreated children with malignant hypertension die within 1 year of diagnosis, intensive drug treatment can help prolong their lives. Likewise, the rapid progression of hypertension can be slowed by active treatment.
In 30% of untreated adolescents, essential hypertension develops into adult hypertension. Treatment of adults with moderate to severe hypertension can significantly reduce morbidity and mortality. The risk of complications is directly proportional to the average blood pressure level. Concerns expressed regarding the adverse effects of antihypertensive drugs on child development are gradually dissipating based on data from the results of observations of children for 2-10 years.
Treatment. The method of choice in the treatment of many types of secondary hypertension, for example, with unilateral kidney damage, renovascular pathology, coarctation, secreting and non-secreting tumors, is surgery.
In case of essential hypertension, reducing salt intake and the patient’s body weight may be sufficient to normalize blood pressure, so treatment should always begin with these measures. The effectiveness of other non-drug treatments, such as moderate exercise, meditation, and biofeedback, has not been well studied. However, in patients with high motivation, such measures can lead to a moderate decrease in blood pressure. With the familial nature of hypertension and elevated fasting serum lipid levels, the patient's daily intake of cholesterol should not exceed 300 mg, saturated fatty acids up to 10%, and is almost never accompanied by signs of methemoglobin intoxication. Minoxidil is a powerful antihypertensive drug used in patients with no effect from intensive polytherapy.
Captopril inhibits the conversion of angiotensin I to angiotensin II, causing immediate vasodilation and a prolonged decrease in aldosterone secretion, despite extremely high activity . It is used not only for chronic hypertension, but also for the development of acute hypertensive encephalopathy and rapidly progressing hypertension. In combination with powerful new vasodilators, captopril or similar drugs eliminate the need for bilateral nephrectomy for severe, intractable hypertension.
Emergency conditions in these patients include the development of hypertensive encephalopathy, intracranial hemorrhage, dissecting aneurysm, acute congestive cardiovascular failure and/or myocardial infarction, crises with pheochromocytoma, pressor crises during catheterization, abdominal crises after coarctectomy, and eclampsia. Treatment in these cases is carried out in an intensive care unit, where there are conditions for quickly organizing treatment measures and reducing their safety, as well as for selecting the dose of administered drugs with constant monitoring of vital parameters.