Inflammation of the bladder (cystitis) is a common disease of the genitourinary system. It is important to know why cystitis is dangerous. Cystitis occurs more often in women than in men, which is due to the characteristics of female anatomy. Out of 10 cases of disease, only 2 occur among the stronger sex. The disease manifests itself at any age. Doctors say that 98% of women had discomfort associated with cystitis.
Complications of cystitis are more painful than the primary symptoms. It happens that cystitis seems to have been cured, but the symptoms remain or quickly return. The transition of the disease to a chronic form will bring significant discomfort with constant lumbar pain, frequent urge to “small”. The infection that causes acute cystitis disrupts the integrity of the bladder and is activated in other organs, serving as a source of new forms of disease: If left untreated, it can become chronic.
Causes of cystitis
Infectious diseases of the bladder are divided into complicated and uncomplicated. Uncomplicated forms of cystitis include inflammation of the bladder in healthy non-pregnant women aged 16-65 years in the absence of other urinary tract diseases. Complicated forms of cystitis also occur in patients with existing urinary tract diseases, for example, pyelonephritis, prostatitis, with severe systemic diseases such as diabetes, heart failure, as well as in men and the elderly. This distinction between the forms of cystitis is necessary for carrying out adequate diagnostic and therapeutic measures.
The main cause of cystitis is infection. As a rule, uncomplicated cystitis is caused by a single microorganism; in chronic inflammation, a mixed flora is determined. The main causative agent is Escherichia coli, in a smaller percentage of cases - saprophytic Staphylococcus, Klebsiella, Enterobacter. Most pathogens are representatives of the normal microflora of the large intestine, rectum and vagina, so cystitis is classified as an autoinfection. Currently, cystitis caused by specific sexually transmitted infections, such as chlamydia, is becoming increasingly common among young people. In people with reduced immunity, fungal cystitis is common, including due to infection with yeast-like fungi of the genus Candida.
, non-infectious cystitis occurs . Hypothermia of the body causes a narrowing of the vessels of the bladder, disruption of the nutrition of its wall, and as a result, a weakening of the protective properties and the development of inflammation. Chemical cystitis is caused by aggressive substances introduced by mistake into the bladder for therapeutic purposes or during an attempt to terminate a pregnancy. Allergic cystitis develops when allergens enter the body. As a rule, certain food products become allergens. Allergic cystitis is characterized by a short course and complete recovery on its own or under the influence of antihistamines. Prolonged stress and neuropsychic overexcitation can cause a functional urination disorder with changes in the mucous membrane of the bladder. Such cystitis is characterized by a persistent course, a tendency to relapse and the absence of bacteria in a urine test.
For the development of cystitis, a combination of at least two factors is necessary: the entry of microorganisms or aggressive substances into the bladder and a decrease in the protective properties of the mucous membrane. Bladder infections can occur in the following ways. The predominant route of infection is the ascending route of infection from the rectum, vagina in women, and urethral region in men. The descending route (with kidney and ureter infections) of infection is less common. Hematogenous and lymphogenous infection is also possible, when microorganisms enter the mucous membrane of the bladder through the blood or lymph flow. In rare cases, a contact route of infection is possible when an organ adjacent to the bladder is affected. In conditions of reduced protective properties of the bladder wall, intensive proliferation of microorganisms occurs. In the process of their life, they secrete certain substances that damage the mucous membrane, and cystitis develops.
Defloration, active sexual activity, pregnancy, childbirth, the postpartum period, and menopausal changes are identified as provoking factors for the disease. Girls of preschool and primary school age are 6 times more likely to suffer from cystitis compared to older age groups. This is due to the immaturity of the ovaries during this period and the lack of female sex hormones in the blood, which play an important role in the formation of protective mechanisms of the vaginal mucosa and paraurethral area. This leads to the colonization of microorganisms and the formation of cystitis as an ascending infection. During defloration (destruction of the hymen), the infection enters the bladder through damaged lymphatic vessels of the hymen. Frequent and rough sexual intercourse contributes to microtrauma of the vaginal mucosa and the penetration of infection into the bloodstream and further into the bladder. But more often, during prolonged sexual intercourse, as a result of massage of the urethra, the infection enters the bladder through the ascending route. During pregnancy, due to the pressure of the growing uterus, stagnation of urine forms, which contributes to the rapid proliferation of microorganisms and predisposes to the development of inflammation. During menopause, in the absence of female sex hormones, which contribute to the formation of local immunity of the mucous membrane of the vagina and bladder, cystitis also often develops.
In men, primary cystitis is extremely rare, usually due to a foreign body in the bladder or after urological procedures. In most cases, cystitis in men is secondary to some disease of the urinary system.
Cystitis and complications during pregnancy
Cystitis causes the greatest danger during pregnancy; complications in the form of pyelonephritis occur more often, occurring in acute and chronic forms.
When carrying a child, several factors complicate treatment are immediately felt:
- hormonal changes in the body, which often provokes an exacerbation of pathological processes;
- fluctuations in immunity, especially in the first trimester;
- compression of the bladder, urinary tract, kidneys by the growing uterus, the occurrence of stagnation of urine, which maintains inflammation.
Treatment of cystitis
If a pregnant woman already has a history of cystitis, an exacerbation is almost inevitable. The main goal of treatment is to prevent complications of cystitis and not harm the woman’s fetus. Taking some types of antibiotics is possible only in the second and third trimesters. Main types of treatment include:
- herbal medicine using medicinal herbs;
- installations - the introduction of drugs directly into the bladder cavity.
Therapy will help you carry your pregnancy to term safely. After childbirth, it is urgent to begin serious treatment.
Pyelonephritis in pregnant women
In case of acute pyelonephritis in pregnant women, intoxication occurs and the following symptoms are observed:
- severe headaches, dizziness;
- pain and heaviness from the inflamed kidney, aggravated by bending over or lying down;
- nausea, vomiting;
- heat;
- severe chills, weakness.
In the chronic form, there may be no symptoms at all, or they will be smoothed out.
Almost every second pregnant woman with cystitis develops acute or chronic pyelonephritis.
The main threat of the disease is the risk of miscarriage. An examination will show whether a miscarriage can occur; therefore, if pyelonephritis is suspected, hospitalization and a detailed examination are necessary.
- Treatment of pyelonephritis in pregnant women is complicated by the need to choose only drugs that are safe for the fetus. These are usually penicillin-based antibiotics.
- Bed rest and a strict diet are recommended for several days to help avoid swelling.
- To eliminate stagnation of urine and restore patency of the urinary tract, “positional therapy” is performed - taking a special position on all fours. This position reduces pressure on the urinary tract.
- It is possible to prescribe physiotherapy - ultrasound treatment, acupuncture.
- In some cases, if normal urine excretion is impossible, a catheter is inserted into the ureter.
If there is no threat of miscarriage and the pregnant woman’s condition is not in danger, it is recommended to move more and walk in the fresh air.
Symptoms of cystitis
Acute cystitis is characterized by a rapid onset of the disease. It is often possible to establish a connection between inflammation and predisposing factors, for example, hypothermia, previous sexual intercourse. Patients complain of frequent urination, a constant desire to urinate, and a strong urge to urinate (urinary incontinence). You often have to make an effort to start urinating. During urination, pain and burning occur in the urethra, and after urination there is pain in the lower abdomen. Urine passes in small portions, the urge to urinate does not stop day or night. In young children, acute urinary retention may occur due to intense pain.
With a significantly pronounced inflammatory process, general poisoning of the body may occur: an increase in body temperature to 38-40 degrees, general weakness, sweating, dry mouth, thirst. As a rule, this indicates the spread of infection with the development of pyelonephritis (an infectious disease of the tissue of the kidneys and renal pelvis).
In the recurrent form of cystitis, exacerbations are replaced by periods of complete absence of inflammation. Moreover, even minimal exposure to provoking factors can again cause the development of the disease.
The chronic form of cystitis is characterized by both mild and severe urination disorders, slight discomfort or sharp pain in the lower abdomen, which are permanent and change slightly during treatment. Such manifestations of cystitis occur due to persistent changes in the wall of the bladder due to frequent previous microbial attacks. In chronic cystitis, microorganisms are not detected in the urine.
If the above complaints occur, you should contact a therapist or nephrologist as soon as possible. Self-medication or loss of time can cause acute cystitis to become chronic and cause complications.
The main sign of the presence of cystitis, in addition to external manifestations, is the detection of leukocytes and bacteria in a general urine test. If bacteria are present, urine culture can be performed to identify the organisms and determine their sensitivity to antibiotics. It is also possible that a small amount of red blood cells may appear in the urine. With hemorrhagic cystitis, the urine becomes the color of “meat slop”, and a large number of red blood cells are detected in it. Ultrasound is informative only in cases of a significantly pronounced process or in a chronic form of the disease. This reveals thickening of the bladder wall, its layering, and swelling.
Echogram for chronic cystitis.
A suspension of desquamated mucosal cells and microbial conglomerates appears in the lumen of the bladder.
Is it possible to avoid the consequences of cystitis?
An extensive list of facts, verified by numerous studies, speaks about whether cystitis is dangerous due to complications. It is possible to avoid their manifestations if you do not self-medicate and undergo comprehensive diagnostics and treatment in a timely manner. You can independently prevent the development of complications if you prevent the process from becoming chronic. Medical recommendations include:
- immediately seek medical help if characteristic signs of cystitis appear (painful voiding, the presence of bloody or purulent impurities in the urine),
- Do not use questionable, externally recommended drugs, herbal medicine, or homeopathy for treatment without the advice of a specialist. Otherwise, self-medication ends in chronic disease,
- do not visit saunas and steam rooms in baths,
- be examined by a gynecologist to rule out possible sexually transmitted infections.
It is important, in case of infectious-inflammatory lesions of the bladder, to focus on professional complex treatment. Acute processes, controlled by a competent specialist, are stopped in a maximum of two weeks.
The consequences of a chronic clinic can last for many years, causing patients both ethical and physical suffering. Complications of the disease require a competent approach - identifying and stopping the root cause of the disease, and treating the consequences that have already appeared.
Complications of cystitis
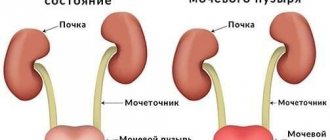
One of the most common complications of cystitis is pyelonephritis. In this case, the infectious process ascends from the bladder through the ureters to the renal pelvis, and from there to the kidney tissue. Of particular importance in this case is the reflux of infected urine into the renal pelvis when pressure in the bladder increases due to inflammation.
Another serious complication is the transition of uncomplicated cystitis to a hemorrhagic form. In this case, inflammation covers not only the mucous membrane, but also other layers of the bladder wall. Bacteria in the course of their life destroy the wall of the bladder, causing bleeding. Hemorrhagic cystitis is characterized by visible changes in the properties of urine: it becomes red due to the admixture of blood, and an unpleasant odor appears. Bleeding from the wall of the bladder can become a serious problem for the patient and even require surgical intervention.
Complicated forms of cystitis and their consequences
In a healthy woman, the urine in the bladder does not contain microorganisms - it is sterile. The inflammatory process starts after pathogens penetrate upward or through the blood and lymph into the lumen of the organ. Acute cystitis is prone to becoming a chronic form of the disease with uncontrolled self-medication and the personal characteristics of the girl’s body.
The likelihood of developing negative consequences is directly proportional to the duration of inflammation in the bladder.
It is customary to distinguish between complications of the disease:
- paracystitis;
- salpingitis and adnexitis;
- renal dysfunction;
- vesicoureteral reflux;
- leukoplakia of the bladder;
- organ empyema;
- pyelonephritis.
Negative consequences of the disease occur when a highly pathogenic infection is introduced. And also with a sharp weakening of the immune system and untimely initiation of treatment.
Paracystitis
It is an inflammatory reaction localized in the fatty tissue located around the bladder. The disease develops more often as a consequence of necrotic and purulent cystitis.
The clinical picture depends on the form of the inflammatory process - infiltrative or purulent. Severe intoxication is characteristic - the body temperature rises to high numbers, 39–40 ° C, the woman shudders, dizziness and cephalalgia are observed.
Inflammation of the peri-vesical tissue, as with cystitis, is characterized by acute unbearable pain above the pubis (below the navel), frequent urination with pain. In girls with an asthenic physique (thin), a swelling above the pubis is palpable.
When a formed abscess is opened into the cavity of the bladder, the general condition of the body improves, but pus and blood impurities are released with urine.
Salpingitis and adnexitis
These gynecological diseases in women can also be consequences of cystitis. Inflammation of the fallopian tubes (salpingitis) rarely occurs independently, but is more often combined with damage to the ovaries on one or both sides. In this case, we are already talking about adnexitis.
The appendages are involved in the pathological process as follows. From an inflamed bladder, infectious agents migrate upward into the female genital tract and affect the reproductive organs.
Clinically, salpingitis and adnexitis are similar and are characterized by the following symptoms:
- the development of the disease often coincides with the end of menstruation;
- the onset is acute, the temperature rises, chills appear;
- characterized by pain that is localized in the lower abdomen and radiates to the rectum and sacrum;
- dysuric disorders, like cystitis, in the form of frequent urination with pain;
- nausea with vomiting, frequent loose stools;
- discomfort during sexual intercourse;
- symptoms of irritation of the pelvic peritoneum, reminiscent of muscle tension in the anterior abdominal wall;
- A distinctive feature is whitish discharge from the genital tract and urethra mixed with pus.
When an inflamed fallopian tube ruptures, exudate enters the abdominal cavity and acute peritonitis occurs - a serious emergency surgical disease requiring emergency surgical intervention.
If treatment for salpingitis or adnexitis is inadequate, there is a risk of modification of the structure of the ovaries, which leads to disruption of menstruation.
Bilateral damage to the fallopian tubes is fraught with the development of their obstruction and, as a consequence, ectopic pregnancy and female infertility.
Renal dysfunction
The chronic form of cystitis can be accompanied by a serious consequence - chronic renal failure.
A long-existing infection in the bladder ascends to the renal pelvis and causes damage to them - pyelonephritis occurs. In addition, under the influence of prolonged cystitis, the normal outflow of urine into the cavity of the bladder is disrupted, which contributes to the throwing of its contents back into the pelvis. Pyelonephritis occurs latently for a long time, nothing bothers the person, and the process gradually progresses.
Having reached an advanced stage, inflammation manifests itself as pain and discomfort in the lumbar region on one or both sides - signs of stretching of the enlarged kidney capsule. Daily diuresis decreases, signs of intoxication gradually appear. This is how chronic renal failure develops.
CRF goes through four stages of development, during which the severity of the symptoms below gradually increases:
- increased nighttime diuresis (nocturia) compared to daytime;
- the release of a large amount of urine, which is replaced by its decrease and complete cessation (anuria);
- swelling on the face (especially in the morning), then descends from top to bottom;
- excruciating thirst, dry mucous membranes and bitter taste in the mouth;
- lack of appetite, nausea with vomiting;
- the skin is pale, flaky, brittle nails are characteristic;
- hand trembling;
- smell of urine from the mouth;
- The heart rhythm is disturbed, blood pressure drops and then rises, and shortness of breath worries.
Harmless cystitis can lead a person to extremely undesirable consequences with subsequent treatment in the hemodialysis department (“artificial kidney”).
Vesicoureteral reflux
The pathology is characterized by the occurrence of reverse flow of urine - from the bladder through the ureter back to the kidney. Vesicoureteral reflux in most cases is a consequence of advanced acute or chronic types of cystitis.
Due to the inflammatory process, the walls of the sphincter (valve) weaken, which normally should not allow urine to flow against its flow. This leads to increased pressure in the ureter, then in the pelvis and renal calyces. This ends with the deformation of these structures. Plus, conditions are provided for bacteria from the bladder to enter the upper parts of the urinary system, and the inflammatory process starts. Normal kidney tissue is replaced by connective tissue, and nephrosclerosis develops, which has negative consequences for the body.
There are no characteristic clinical signs of vesicoureteral reflux. In the initial stages of development, it can usually be hidden. The occurrence of symptoms of pathology is due to prolonged lack of treatment or layered infectious complications. The signs of the relapse stage of the disease are similar to the manifestations of cystitis, pyelonephritis or glomerulonephritis and depend on the age of the person.
In practice, a dangerous consequence of vesicoureteral reflux can be chronic kidney failure and hydronephrosis.
Leukoplakia
The disease is understood as a transformation of the walls of the bladder - a change in the transitional epithelium to atypical for the mucous membranes in this place - multilayered keratinizing squamous cell.
The main cause of leukoplakia is chronic recurrent cystitis.
Urine exhibits an irritating effect on transformed epithelial cells. And this further provokes the inflammatory process and leads to pain, despite adequate antimicrobial therapy. Potassium from urine penetrates through the destroyed layer into the interstitial tissue, which leads to atrophy of nerve endings, blood vessels, and spasm of smooth muscles. The consequences of these processes include urination disorders.
Clinical symptoms of leukoplakia caused by cystitis:
- difficult and frequent urination with pain;
- persistent aching pain in the lower abdomen, under the navel;
- imperative urge to go to the toilet up to urinary incontinence;
- the appearance of hematuria in the final portions of urine.
The consequences of leukoplakia include the development of pyelonephritis and chronic renal failure.
Empyema of the bladder
This is a complication of cystitis, which is a purulent melting of the bladder wall. The consequences are quite dangerous. Organ rupture and exudate leakage into the abdominal cavity with the development of purulent peritonitis, requiring immediate surgical treatment, cannot be ruled out.
Clinically, a complication of cystitis is manifested by severe intoxication of the body (high temperature, weakness, apathy, myalgia). Also characterized by sharp unbearable pain in the abdomen when urinating, the urine is cloudy due to the admixture of pus.
Treatment of cystitis
Treatment of cystitis should be timely and comprehensive. Uncomplicated acute cystitis is treated on an outpatient basis. Depending on the suspected pathogen, antimicrobial therapy is prescribed (ciprofloxacin, ofloxacin, levofloxacin). Anti-inflammatory drugs (diclofenac, nimesulide) are recommended for the treatment of inflammatory syndrome.
From the first hours of the disease, the use of painkillers (solpadeine, suppositories with anesthesin) and antispasmodics (no-spa, papaverine) is necessary to relieve pain and facilitate urination.
To ensure adequate removal of infected urine and prevent stagnation, it is recommended to drink fluid in an amount of at least two liters per day. In addition, it is necessary to abstain from sexual intercourse for 5-7 days. Also, in order to restore the protective properties of the bladder mucosa, the use of immunostimulating drugs is indicated.
Complicated cystitis , as a rule, must be treated in a hospital setting. In this case, the disease that contributes to the occurrence of cystitis is recognized, as well as its adequate treatment. In some cases, for example, with uterine prolapse in women or prostate adenoma in men, surgical treatment is indicated.
For the treatment of chronic cystitis and for preventive purposes, it is permissible to use herbal preparations that have a diuretic effect. Also, some plants (bearberry, horsetail, knotweed, lingonberries and cranberries, celandine) have bacteriostatic, antispasmodic and analgesic properties. Some medicinal herbal preparations have been patented in Russia, for example, canephron, cystone, which have proven themselves well in the complex treatment of cystitis. Exacerbations of chronic cystitis are treated similarly to acute cystitis.
Treatment of acute cystitis with antibiotics
For the treatment of cystitis, medications are prescribed:
- Doxycycline 0.1 mg 2 times a day;
- Levofloxacin 500 mg once a day;
- Erythromycin 500 mg 4 times a day;
- Ofloxacin 300 mg 2 times a day;
- Roxithromycin 150 mg 2 times a day;
- Spiramycin - take 3 mg 3 times a day;
- Monural - take 3 mg 1 time per day;
- Nolitsin - take 1 tablet twice a day, course 3 days;
- Biseptol - take 2 tablets 2 times a day for inflammation, course 3 days.
If for some reason a dose of the drug is missed due to cystitis, it is strictly forbidden to take a double dose of the drug. When the symptoms of the disease have passed, antibiotics are taken until the end of the course of treatment
Prevention of cystitis
To prevent cystitis or its exacerbation in the chronic form of the disease, it is recommended to regularly empty the intestines and bladder and avoid constipation. Lead an active lifestyle, move more, as this helps eliminate congestion in the abdominal organs. In addition, it is necessary to observe the rules of personal hygiene, especially the genitals. It is very important for women to carry out vaginal sanitation in a timely manner. With chronic cystitis, a complete cure is impossible without identifying and treating the primary cause.
This common disease is dangerous due to complications such as pyelonephritis and interstitial cystitis.
Cystitis is one of the most common urological diseases. This disease occurs in women approximately 5-6 times more often than in men. In approximately 10% of cases of those who become ill with the acute form of this disease, it becomes chronic. And in some cases it can lead to serious complications.
Forms of cystitis
Inflammation of the bladder mucosa is called cystitis. Cystitis can develop as a result of infection or due to exposure to some negative factors. On this basis they distinguish:
- Infectious cystitis. It can be specific or non-specific. Specific develops as a consequence of tuberculosis, gonorrhea or Trichomonas infection. Nonspecific occurs as a result of infection of the bladder with E. coli or other intestinal bacteria.
- Non-infectious cystitis can be chemical, thermal, toxic, medicinal, radiation, etc.
Depending on the stage at which this disease is located, there are:
- Acute cystitis. Inflammation of the bladder mucosa occurs suddenly and is pronounced. If not treated correctly, it can become chronic.
- Chronic cystitis. The disease occurs in a less pronounced form and is dangerous because it can serve as a “camouflage” for other chronic diseases and lead to complications.
Cystitis can also develop as a consequence of other diseases and malformations of internal organs.
- Primary cystitis occurs in a healthy person. It can develop as a result of hypothermia, abnormalities of the ureters, and also in pregnant women as a result of “squeezing” of the urinary tract. As a rule, it manifests itself as inflammation, which develops only in the mucous membrane of the bladder.
- Secondary cystitis occurs as a complication of other diseases of the bladder or nearby organs. It can affect not only the mucous membrane of the bladder, but also its other tissues.
Factors contributing to the development of cystitis
There are a number of factors that increase the likelihood of cystitis. This disease can be provoked by:
- bladder injuries
- avitaminosis
- hypothermia
- hormonal problems
- congestion in the veins
Symptoms of cystitis
The manifestations of cystitis vary somewhat depending on the form of the disease. And, nevertheless, the symptoms of both acute and chronic cystitis at the time of exacerbation are common:
- frequent urination, up to several times an hour, which is accompanied by pain
- pain in the lower abdomen that gets worse with urination
- cloudy urine
- general malaise
- temperature rise to subfebrile
In the chronic form of this disease, symptoms may be very vague or practically absent. But the disease must be diagnosed and treated.
How to diagnose cystitis?
If you experience the above symptoms, then there is a high probability that you have “earned” cystitis. In order to accurately establish the diagnosis, you need to do a urine test. It is also necessary to carry out bacteriological culture of the urine fluid to determine which antibiotic to treat the infection causing the disease. Ultrasound, radiography, and cytoscopy are also used to diagnose this disease.
After establishing an accurate diagnosis, the doctor will prescribe adequate treatment, which differs depending on the causes of cystitis and the degree of involvement of the bladder in the inflammatory process. Antibacterial (nitroxoline), anti-inflammatory and diuretic agents (cyston, etc.) can be used. With timely and correct treatment, the likelihood of complications is low. But not fully treated, but only muted cystitis becomes the cause of serious complications.
Complications of cystitis
Complications of cystitis include:
- Interstitial cystitis. With this dangerous type of disease, inflammation affects not only the mucous membrane of the bladder, but also its muscle layer. Which over time leads to shrinkage of this important organ. Eventually, the shriveled bladder can no longer perform its functions and a bladder transplant becomes necessary.
- Hematuria or blood in the urine - this problem can occur as a complication of cystitis. If bleeding is severe, a blood transfusion may be necessary.
- Pyelonephritis. With untreated cystitis, the infection can travel up the ureters and cause inflammation of the kidneys. Pyelonephritis is a serious inflammatory kidney disease that requires urgent treatment and, in severe cases, can be life-threatening.
These complications can be avoided if cystitis is treated promptly and correctly. But it’s even better to prevent cystitis from occurring. To do this, it is worth paying attention to the prevention of this disease.
Inflammation of the bladder (cystitis) is a common disease of the genitourinary system. It is important to know why cystitis is dangerous. Cystitis occurs more often in women than in men, which is due to the characteristics of female anatomy. Out of 10 cases of disease, only 2 occur among the stronger sex. The disease manifests itself at any age. Doctors say that 98% of women had discomfort associated with cystitis.
Complications of cystitis are more painful than the primary symptoms. It happens that cystitis seems to have been cured, but the symptoms remain or quickly return. The transition of the disease to a chronic form will bring significant discomfort with constant lumbar pain, frequent urge to “small”. The infection that causes acute cystitis disrupts the integrity of the bladder and is activated in other organs, serving as a source of new forms of disease: If left untreated, it can become chronic.
Untreated inflammation of the bladder can result in severe pathologies and torment a person for the rest of his life.
What danger does complicated cystitis pose?
For women
Regardless of the form of manifestation of the pathological process, complications of cystitis in women are more acute, with the development of severe pain. An infection that has invaded the bladder organ through the urethral route affects the integrity of the mucous lining of the bladder and is activated in the renal tissues, creating the preconditions for the development of pyelonephritis with the following symptoms:
- stretching the kidney capsules,
- filling them with purulent contents,
- decreased renal excretory functions,
- intoxication symptoms,
- pain in the lumbar area and abdomen.
The neglect of the inflammatory process provokes complete renal failure and the possible development of peritonitis, due to the breakthrough of pus into the peritoneum from a purulent focus in the renal pelvis.
Through the fatty tissue of the pelvic cavity, pathogens can spread into the uterine cavity and the fallopian tubes. Salpingitis develops, causing:
- inflammation and thickening of the tubes,
- development of adhesive cords,
- formation of exudate with pus,
- sticking of pipe cavities.
When the process is neglected, there is a high probability of developing andexitis with the involvement of the ovaries in the inflammatory process - a change in their tissue structure, which leads to instability in the menstrual cycle. An infectious-inflammatory process with bilateral development is dangerous due to the development of tubal obstruction, the possible risk of attachment of the zygote (fertilized egg) outside the uterine cavity, or the development of infertility.
In pregnant women, an enlarged uterus puts pressure on the bladder walls, which interferes with the outflow of urine.
With the latent course of chronic cystitis, there is a risk of activation of the pathogen and spread of infection ascending to the kidneys through the ureters, causing dysfunction in its work. Such disturbances can result in hypoxia or spontaneous miscarriage for the fetus.
For men
In men, the consequences of cystitis can manifest themselves in the form of:
- development of inflammatory reactions in the prostate gland, which in a complicated process threatens male infertility,
- blockage of the urethral canal and exacerbation of the disease,
- a decrease in sperm secretion, which provokes a strong increase in temperature during the disease, and antibiotic therapy prescribed to stop the infectious process.
For children
Frequent cystitis in children is mainly due to untimely or insufficient treatment of their primary form and its latent chronic course. This is manifested by the different nature of morphological changes in the inner mucous membrane of the bladder reservoir. Necrotic tissue damage is also possible.
With a weakened immune system and without timely adequate treatment, the infection spreads to adjacent organs, manifesting itself:
- inflammatory kidney disease (pyelonephritis),
- infectious and inflammatory processes in the urethral canal (urethritis),
- development of vesiculitis in boys (inflammatory damage to the testicles),
- vesico-ureteral reflux, changing the normal flow of urine in the opposite direction (to the kidneys).
The very presence of cystitis in children may indicate the presence of unidentified pathologies in the child’s body - changes in the bladder organ itself, possible neurogenic syndrome, the presence of sand or stones in the bladder, inflammatory processes in the kidneys.
In puberty boys (teenagers) who have experienced the “delights” of sexual intercourse, cystitis can be one of the signs of the presence of sexually transmitted infections, which should be paid special attention to.
What forms of complications after cystitis exist?
- Hemorrhagic form. The defining sign is the presence of blood in the urine, caused by damage to blood vessels in the bladder. There is the presence of both small traces and large blood clots. Characterized by increased temperature, sharp pain in the perineum and lower abdomen. The cause of the disease is viruses, bacteria, fungus. It occurs due to compression of the walls by growing tumors, growths, or a foreign object. The severity of the consequences of cystitis is replacement with connective tissue, muscle and organ dysfunction.
- Interstitial form. The mucous membrane of the organ and the underlying muscle layer are affected. Bacterial exposure leads to the appearance of scars, ulcers in the bladder cavity, and blood in the urine. The bladder copes poorly with its functions, its elasticity and ability to contract decrease, and its volume decreases. The main symptoms are an increasing number of urges, pain during filling. Chronic forms are characterized by sphincter dysfunction and incontinence.
- Gangrenous form. A severe complication in which the entire bladder wall is involved. Complete or partial death of the mucous membrane occurs. An advanced purulent process, necrosis of the muscle membranes provokes the consequences of cystitis in women, such as perforation (rupture) and paracystitis. The main symptoms are hematuria (blood in the urine), urination does not bring relief to the patient, general intoxication of the body, pain in the joints, muscles and headaches.
https://youtube.com/watch?v=6HU-aL4n_Dg
Pathogenesis of cystitis
The infection enters the organ via an ascending route from the urethra, prostate gland, seminal vesicles and testicle. Descending infection is most common with lung diseases such as tuberculosis. Microorganisms spread hematogenously through blood from purulent foci, and lymphogenously - with pathology of the genitourinary organs (endometritis, salpingitis).
The presence of infection alone is not enough for the development of the disease, since the organ has significant resistance. Predisposing factors are necessary for inflammation to occur. For example, decreased immunity, hormonal dysfunction, open and closed operations. Also an important prerequisite for the onset of pathology is stagnation of urine or its backflow into the bladder.
Symptoms of complications after cystitis outside the bladder
- Trigonite. Inflammation affects the area of the vesical triangle (located between the internal opening of the urethra and the orifices of the ureters). Captures the sphincter muscles. Acute trigonitis is caused by an infection affecting the posterior part of the canal or by prostatitis. The chronic form in women occurs with an abnormal position of the uterus and prolapse of the anterior vaginal wall. Diagnosed by cystoscopy. The symptoms are similar to those of acute cystitis, with similar treatment.
- Paracystitis. Occurs when inflammation from the bladder is transmitted to the tissue tissue. The main function of pelvic tissue is to fill the space between the pelvic organs, ensuring their mobility, correct internal position and nutrition. Treatment is possible only through surgery.
- Pyelonephritis is a common consequence of cystitis. The pathogen travels through the ureters to the kidneys, and a purulent infection develops. The main signs are fever, spasm of the anterior abdominal wall, and a decrease in the amount of urine. Symptoms may not appear until the kidney shrinks and develops renal failure. Advanced disease can lead to death due to peritonitis.
What is the threat to women
Inflammation of the bladder is very dangerous, since even an uncomplicated course can provoke the development of salpingitis or complicate its mild manifestation. Salpingitis is an inflammatory process in the fallopian tubes. Its chronic course can lead to thickening of the walls of the pipes and the formation of adhesions.
If this condition is not detected or not treated, then in the early stages of pregnancy the girl may lose the child. Another possible diagnosis is infertility.
A postcoital test is used to determine the patency of the fallopian tubes. It is used to examine the mucus of the cervical canal. This is a kind of test for the compatibility of a married couple.
What other inflammatory processes are there?
- Vesicoureteral reflux is a violation of the direction of urine movement through the ureters from the bladder to the kidneys. The reason is a decrease in the ability of the sphincter to contract due to inflammatory damage, and possible loss of the organ.
- Cystalgia is a complication of cystitis among women and girls aged 20 to 50 years. The patient develops a painful condition, a strong, frequent urge to urinate, but there are no pathological changes in the bladder. The symptoms are sometimes called urethral syndrome. Pregnancy, menopause, and menstrual irregularities contribute to the development of the disease.
- Diffuse ulcerative cystitis and empyema. With insufficient treatment, the infection goes under the mucous membrane, forming bleeding ulcers and ulcers. The structure of the shell weakens, complications may develop. The appearance of scars, loss of tissue elasticity reduces the organ in volume, and other complications develop. The appearance of cysts and polyps is likely. Empyema is a complication of cystitis that occurs when there is a large accumulation of pus and lack of outflow. Requires surgery.
Return to contents
Risk factors
Many female representatives have become accustomed to the fact that they have relapses of cystitis from time to time. They have learned to relieve the symptoms of the disease and treat this problem quite calmly, but this is a serious mistake, since this pathology can provoke the development of serious complications.
The following factors can lead to the development of complications with cystitis:
- complete lack of treatment or its ineffectiveness,
- self-medication or non-compliance with the recommendations of the attending physician,
- unauthorized cessation of antibiotics when symptoms disappear,
- pregnancy,
- anemia,
- weakening of the immune system,
- oncological diseases,
- congenital pathology of the blood system,
- constant fasting,
- metabolic disease,
- hypovitaminosis,
- frequent change of sexual partners,
- chronic diseases of the genitourinary system,
- congenital pathologies of the genitourinary system,
- surgical intervention in the pelvic and abdominal organs,
- failure to comply with intimate hygiene rules.
Cystitis can be caused by one or more of the reasons listed above. Therefore, it is very important to monitor your health and promptly seek qualified medical help.
Why is cystitis dangerous in women and men?
Dangerous consequences from cystitis occur at any age, regardless of gender. The organs adjacent to the bladder (kidneys, uterus and appendages, intestines) are especially affected. An infection that affects an organ through the lymphatic tract spreads to others, causing complications. What can frequent recurrence lead to?
- difficulties of sexual life;
- modification and damage to the membranes of the bladder;
- sphincter dysfunction leading to urinary incontinence;
- inflammation of the uterus and appendages;
- decreased reproductive capacity;
- necrosis of bladder tissue;
- bleeding due to hematuria.
For the most part, the manifestation of acute cystitis is a pathology that develops rapidly, after 10 days it subsides and the symptoms disappear. After a short period of time, severe, exhausting pain begins and the urge to go to the toilet becomes more frequent. A person experiences a feeling of insecurity, becomes irritable, and the nervous balance is generally disturbed. Depression and stress are common side effects of the disease.
Who suffers from cystitis first?
- a person with reduced immunity or chronic diseases;
- people exposed to hypothermia;
- girls starting to be sexually active;
- women during pregnancy;
- postmenopausal women and menopause;
- people leading a sedentary lifestyle;
- people who do not pay enough attention to personal hygiene;
- those who often change sexual partners;
- those who use contraceptives with spermicides.
How to avoid complications of cystitis?
To ensure that side effects from cystitis become a thing of the past, you should carefully adhere to the rules of personal hygiene. Remember, the perineum is wiped in the direction from the pubis to the tailbone, the rule also applies to washing. If possible, you should wash after every bowel movement. It is necessary to change sanitary pads on time, especially during menstruation. It is imperative to treat inflammatory processes in the body. Try not to put off going to the toilet for too long. Avoid hypothermia. Choose clothes that do not compress internal organs and do not impair the movement of lymph and blood. Use underwear made from natural materials. Lead an active lifestyle. Do not overuse baths and saunas. Proper nutrition is an important disease prevention, will help reduce the side effects of the disease and alleviate the condition.
The main rule is that at the first suspicion you should immediately consult a qualified doctor for medical help. At an early stage, the disease, with the right approach, does not require long-term treatment and goes away without consequences. Advanced and complicated cystitis requires immediate medical attention.
There are many remedies for cystitis, but they must be prescribed by a doctor. Do not self-medicate.
What are the reasons for the development of complications
With a properly designed course of therapeutic treatment for an acute form of an infectious-inflammatory process in the bladder, all signs of the disease can be eliminated within one and a half to two weeks. With a protracted clinical picture of the disease, the doctor’s task is to identify the factor that supports the activity of intravesical inflammatory reactions.
Very often, complications after cystitis in women and other patients arise when the disease becomes chronic, which can worsen under the influence of the slightest provocative factors.
Patients have many provocative reasons leading to unpleasant consequences of infectious lesions of urinary bladder tissues. But the main feature of the development of possible pathologies, which are regarded as complications, is the asymptomatic clinical picture of cystitis, which contributes to the chronicization of a sluggish infectious-inflammatory process in the bladder without pronounced signs of the disease. This state can be maintained by:
- incorrectly selected drug therapy,
- disorders of metabolic processes in the body,
- failure of the immune system,
- the course of treatment is not long enough to completely eliminate pathogens,
- non-compliance with recommendations for taking medications,
- frequent exacerbations of the disease,
- non-compliance with intimate hygiene standards and indiscriminate choice of sexual partners,
- chronic infectious diseases in the reproductive and urinary systems.
The result of untimely treatment is infection of organs adjacent to the bladder.
Pyelonephritis
One of the most severe complications of cystitis for the female body is inflammation of the kidneys - pyelonephritis.
Symptoms of the onset of the disease are:
- a sharp increase in body temperature to 38-40 degrees, a febrile state with severe chills and sweating;
- severe, unbearable pain in the kidney area, tension in the abdominal muscles;
- a decrease in urine output with a normal amount of fluid consumed.
Important! If you notice the first symptoms of kidney inflammation, you should immediately consult a doctor. Self-medication and the use of medications without prior consultation can significantly worsen the condition.
Interstitial cystitis
A pathological condition caused by bacterial infection of the deeper layers of bladder tissue is called interstitial cystitis. Inflammatory processes occurring in the muscle layer cause persistent destructive changes, accompanied by chronic pain in the pelvic region.
Acute hemorrhagic cystitis
Due to the fact that tissues damaged as a result of an infectious lesion are systematically exposed to irritating substances contained in urine, scarring occurs and, as a consequence, loss of elasticity of the bladder. Over time, the volume of the bubble decreases, and it loses the ability to perform its functions (accumulate liquid).
The course of interstitial cystitis is accompanied by symptoms characteristic of the acute form of the disease, with the only difference being that the pain, as a rule, is permanent and can intensify during sexual intercourse (especially in women). Symptoms of interstitial cystitis may include:
- constant pain in the pelvic area of unknown origin;
- pressing feeling in the bladder area;
- pain when filling the bladder;
- the appearance of blood in the urine;
- increased frequency of urination;
- soreness of the penis.
Due to the fact that diagnosing interstitial cystitis is, as a rule, extremely difficult due to the lack of a specific localization of pain symptoms, the patient may seek help from doctors of other subspecialties and lose the time necessary for timely treatment.
Inflammatory processes primarily affect the area of the bladder triangle
Prevention
There is prevention of chronic cystitis. It includes a number of measures - these are preventive courses of therapy prescribed by a doctor and timely detection of emerging pathologies in the body.
To prevent exacerbations of the disease, the urologist prescribes herbal diuretics, antibiotic therapy, etc.
It is also necessary to prevent and eliminate purulent processes that accompany urogenital pathologies and hormonal disorders.
We should not forget about maintaining sexual hygiene and intimate care.
Causes
The development is caused by microorganisms that belong to different species groups. Develops under the influence of negative factors:
- Cystitis during pregnancy treatment at home
- Viruses.
- Fungi.
- Allergic reactions.
- Injuries and previous surgeries.
The following factors increase the risk of developing the disease:
- Hypothermia.
- Exhaustion of the body.
- Bad habits. In particular, alcoholic drinks have an irritating effect on the mucous membrane, reducing resistance to pathogenic factors.
- Predisposition to inflammatory processes, which is caused by increased reactivity of the immune system.
The danger is ulcerative and necrotic, leading to perforation of the bladder. This phenomenon causes diffuse urinary peritonitis.
The impact of the aggressive environment of urine on the intestinal walls and other organs of the abdominal cavity causes severe functional and structural disorders.
Provoking factors of complications
The chronic course of the disease occurs not only in the absence of adequate therapy. Relapses of the disease can be caused by:
- failure to comply with personal hygiene rules;
- hormonal imbalances in the body;
- pathologies of the pelvic organs;
- weakened immunity.
It is the chronic form that is dangerous due to the occurrence of many complications. Often the disease takes a chronic course during pregnancy due to hormonal fluctuations and the lack of antibacterial therapy.
Sources used:
- https://cistitstop.ru/vse-o-cistite/posledstviya-cistita-u-zhenshhin.html
- https://artident.ru/zuby/chem-opasen-cistit-u-zhenshchin-oslozhneniya-cistita-u-zhenshchin-posledstviya/
- https://uromir.ru/vospalenie-mochevogo-puzyrya/bolezn/posledstvija-cistita.html
- https://flovit.ru/medicina/drugie-zabolevaniya/chem-opasen-cistit-posledstviya-cistita-u-zhenshhin.html
- https://upraznenia.ru/opasen-tsistit.html
- https://prostatu.guru/lechenie/lechit-tsistit.html
- https://successmed.ru/raznoe/posledstviya-tsistita.html
Acute pyelonephritis
- Pyelonephritis (unilateral or bilateral);
- Paracystitis;
- Vesicoureteral reflux;
- Leukoplakia;
- Empyema of the bladder.
Pyelonephritis
If cystitis is not treated, the pathogenic flora migrates upward from the bladder to the kidneys, causing inflammation of the kidneys - pyelonephritis.
Acute pyelonephritis can be complicated by paranephritis, the formation of a carbuncle or abscess of the kidney, necrosis of the renal papillae, which is an indication for surgical intervention. In chronic bilateral pyelonephritis, the development of renal failure is more common, since both kidneys are inflamed.
Paracystitis
Pathogenic flora penetrates into the paravesical tissue through the blood, in the presence of a distant purulent source in the body, or lymphogenously (through lymph) from the bladder or intestinal tract.
If treatment is not completed completely, paracystitis can become chronic.
A membrane is formed around the zone of chronic inflammation, encystation of the inflammation zone occurs, or compaction and sclerosis of adipose tissue is formed at the site of the chronic process. Treatment in this case is only surgical.
If the ureteral sphincter fails, urine backflows from the bladder into the ureter with further development of the inflammatory process in the kidneys.
This pathology poses a great danger, causing periodic relapses of acute pyelonephritis and cicatricial changes in the kidneys, up to complete atrophy of the kidneys.
This is a chronic disease in which some epithelial cells are replaced by others. Areas appear covered with keratinized epithelium, which is unable to protect the walls of the bladder from the active effects of urine components, which causes a chronic inflammatory process that complicates the activity of the urinary system.
This complication of cystitis occurs when pus accumulates in the bladder, due to purulent inflammation in the wall of the organ and a violation of the outflow of pus from the cavity. Cure is possible only with surgery.
Based on morphological changes in the mucous wall of the bladder, the following are distinguished:
- Interstitial cystitis. With this type of cystitis, inflammation affects not only the epithelium of the bladder, but also the muscle layer. This complication leads to the wrinkling of the bladder, it loses its elasticity and becomes smaller in volume. As a result, stagnation occurs in the organ, which contributes to the formation of kidney stones, the appearance of pyelonephritis, and can lead to bleeding.
- Hemorrhagic cystitis. As a result of an acute process with damage to blood vessels, blood penetrates into the urine. The discharge takes on either a light pinkish or cloudy dirty-brown hue and has a characteristic unpleasant odor. With a prolonged course of the disease and stable blood loss, iron deficiency anemia develops, the main manifestations of which are severe weakness, dizziness, shortness of breath (from a lack of oxygen supply to the body tissues). A blood test shows a low hemoglobin level and a decrease in red blood cells. In rare cases, the urethra or bladder lumen may become blocked by a blood clot. According to statistics, this type of cystitis is most common in elderly men with prostate adenoma. Most often, acute hemorrhagic cystitis occurs after an adenovirus infection, as a result of radiation exposure to the body, and after taking medications from the group of cytostatics.
- Necrotizing cystitis. It occurs as a result of disturbances in trophic processes with the formation of ulcerations that are prone to fusion. Muscle tissue is involved in the process.
Other complications
The consequences of cystitis in women can be expressed in dysfunction of the sphincter, which causes urinary incontinence. This is a common disorder in older women. The opposite development of events is also possible, when acute urinary retention appears as a result of inflammation.
Cystitis itself cannot cause infertility, but its spread to nearby organs, including the uterus and appendages, can lead to infertility.
When the bladder becomes inflamed, the infection can spread to the appendages, causing obstruction of the fallopian tubes and, as a consequence, secondary infertility.
Cystitis and the complications it causes pose a significant health problem, affecting quality of life. Therefore, at the first symptoms of the disease, you should consult a specialist for diagnosis and selection of drug therapy.
Remember, uncomplicated cystitis can be cured within five days, and complications after cystitis can be cured over a long period of time.
There are many factors that can extend pathological processes beyond the “mild” form, but the main cause of complications can be considered the asymptomatic form of the disease characteristic of cystitis. It is characterized by a sluggish course of inflammatory processes in the mucous surface of the bladder, with long-term preservation of the viability of pathogenic microorganisms and the absence of pronounced symptoms that appear in the acute form of the disease.
The main reasons for the subsidence of the acute process and its transition to a chronic form are:
- incorrect selection of medications;
- insufficient duration of treatment;
- violations in the regimen of taking recommended antibacterial drugs or antibiotics;
- repeated illness with acute cystitis within 1-2 months;
- the use of warming procedures without the simultaneous use of antibacterial, antiseptic agents or antibiotics.
Important: You should not take warming procedures (baths, heating pads) at home in case of acute cystitis without simultaneous treatment with antibacterial agents, since increased blood circulation in the area of inflammation contributes to the spread of infection through the bloodstream.
The use of antibacterial drugs is a prerequisite for treatment
All possible complications of cystitis can be divided into:
- causing structural and functional changes in the tissues of the bladder: interstitial cystitis; hemorrhagic; diffuse ulcerative cystitis; leukoplakia of the bladder walls;
- causing diseases of other organs of the genitourinary system: vesicoureteral reflux; pyelonephritis; inflammation of the prostate gland in men; endometriosis in women.
Penetration of pathogenic microflora into the kidney through the ureters (ascending pyelonephritis) is not the most common route of infection. Most often, downward infection occurs from other foci of inflammation, usually carried through the bloodstream.
When an infection enters the kidney tissue, the intermediate tissue (parenchyma) is primarily affected. The structure of the parenchyma is characterized by its inability to repair damage caused by the inflammatory process, so scar tissue forms at the site of the lesion.
Important: Multiple scar formations disrupt the blood supply and contribute to the development of the “shrinked kidney” syndrome, which leads to its complete atrophy.
The first stage of infectious kidney damage is acute pyelonephritis. It can be in the nature of general or focal inflammation with the formation of a focus of infiltration. The consequences of focal inflammation can be a kidney carbuncle (a large focus of suppuration) or apostematous nephritis (multiple small ulcers affecting the external and internal tissues of the kidney).
Healthy kidney and wrinkled kidney
The chronic form of pyelonephritis is a consequence of several stages of the acute form:
- Primary damage to the interstitial tissue;
- Renal tubule damage;
- Damage to the renal glomeruli;
- Atrophy of blood vessels and arterioles.
Characteristic for chronic pyelonephritis, as well as for chronic cystitis, is the absence of severe symptoms. This fact is the reason for the late diagnosis of pyelonephritis and the development of irreversible processes in the kidneys. Some of the symptoms accompanying ascending pyelonephritis are identical to the symptoms of cystitis, some are independent:
- aching pain in the lower back or abdomen;
- high temperature;
- nausea;
- vomit;
- diuretic phenomena.
Regardless of what factors caused the occurrence of cystitis, the further development of the disease in any case will be infectious in nature. Therefore, it is extremely important to take all possible measures to timely suppress the activity of pathogenic microflora with the most effective and safe means. As a rule, combined antibacterial agents are highly effective in treating cystitis.
In a healthy woman, the urine in the bladder does not contain microorganisms - it is sterile. The inflammatory process starts after pathogens penetrate upward or through the blood and lymph into the lumen of the organ. Acute cystitis is prone to becoming a chronic form of the disease with uncontrolled self-medication and the personal characteristics of the girl’s body.
It is customary to distinguish between complications of the disease:
- paracystitis;
- salpingitis and adnexitis;
- renal dysfunction;
- vesicoureteral reflux;
- leukoplakia of the bladder;
- organ empyema;
- pyelonephritis.
Negative consequences of the disease occur when a highly pathogenic infection is introduced. And also with a sharp weakening of the immune system and untimely initiation of treatment.
Paracystitis
It is an inflammatory reaction localized in the fatty tissue located around the bladder. The disease develops more often as a consequence of necrotic and purulent cystitis.
The clinical picture depends on the form of the inflammatory process - infiltrative or purulent. Severe intoxication is characteristic - the body temperature rises to high numbers, 39–40 ° C, the woman shudders, dizziness and cephalalgia are observed.
Inflammation of the peri-vesical tissue, as with cystitis, is characterized by acute unbearable pain above the pubis (below the navel), frequent urination with pain. In girls with an asthenic physique (thin), a swelling above the pubis is palpable.
The dangers of no treatment
Cystitis is a very insidious disease. Even if the symptoms disappear, this does not mean that the infection has passed. She simply lurks in the body and waits in the wings. This disease requires complete cure, otherwise it threatens to become chronic.
Why is cystitis dangerous if left untreated?
- Ureteral reflux may occur - a pathological process in which urine flows back into the ureters and pyelocaliceal apparatus of the kidney.
- Development of hemorrhagic form, regular chronic blood loss.
- Development of sepsis.
- Inflammation of kidney tissue.
- Urethritis is the development of inflammation of the urethra.
- Reduced bladder volume due to the formation of adhesions.
Therefore, it is necessary to visit a doctor as quickly as possible, undergo all the necessary tests and undergo a course of treatment.
Complications of the chronic form
The chronic form can contribute to the development of complications. There are a large number of them, and the impact on women’s health is characterized as sharply negative. Irreversible processes may develop. Main complications:
- pyelonephritis;
- hematuria;
- vesicoureteral reflux;
- interstitial nephritis.
Normally, urine moves in only one direction. This is achieved by a valve that closes when the bladder is full. The chronic process disrupts the structure and function of the valves, as a result of which urine is thrown in the opposite direction and vesicoureteral reflux occurs. This condition contributes to the proliferation of infection and the development of pyelonephritis.
Pyelonephritis is a complication accompanied by fever, decreased urine volume, and increased sweating.
Interstitial cystitis is characterized not only by inflammation of the mucous membrane of the bladder, but also by the transition of this process to the muscle layer. As a result of a long course of the disease, the fibers of the organ can be replaced by scar tissue, which is manifested by a decrease in its elasticity. Symptoms of this complication include frequent urination in small portions, pain at rest and during sexual intercourse.
Hematuria is a consequence of the chronic form and the main symptom of the hemorrhagic course of inflammation. It is dangerous because the layers of the organ are replaced with connective tissue.
- Cystitis from hypothermia: could it be, symptoms and treatment
This causes iron deficiency anemia, which is especially bad for pregnant women.
Cystitis
Inflammatory pathology, which is characterized by damage to the mucous membrane of the bladder.
It occurs much more often in women than in men. This pattern is caused by the fact that the urethra of the female body has a number of anatomical features.
These include:
- Short length of the urethra.
- Funnel-shaped urethra.
- Close location to the vagina and anus.
Such features make infection easier, given that bacteria are the etiological factor. In men, bladder inflammation is relatively rare. More often it is a secondary process that develops against the background of other diseases.
Prevention and treatment
Prevention consists of eliminating all the dangerous factors listed above. You should lead a healthy lifestyle, eat right, observe personal hygiene rules, wear comfortable clothes and underwear. If your work involves constantly sitting at a computer, you should walk for 5 minutes every hour and a half. Get checked periodically for infections (especially genital infections). Strengthen your immune system.
If you still experience symptoms of cystitis, treatment should begin immediately. However, it is not the manifestations that need to be treated, but the disease itself, the causes of the disease. Most often, antibacterial drugs and uroseptics are used to combat the disease, and a course of physiotherapy is prescribed. But initially the etiological factor and its sensitivity of the flora to antibiotics should be established. Otherwise, treatment may lead to the development or exacerbation of another disease. To treat a mild form of the disease, sometimes it is enough to use herbal preparations and biological supplements. You should also eat right, maintain a proper routine, and strengthen your immune system.
Exacerbations of cystitis are observed with hypothermia. It is at this time that the body’s resistance decreases, which leads to the active proliferation of infections. It penetrates the bladder and leads to inflammatory processes. Cystitis can develop due to damage to the urethra as a result of sexual intercourse or frequent sexual activity. Sometimes the disease manifests itself in girls during the menstrual cycle.
And it is important to remember that at the first signs of the disease you should immediately consult a doctor. After consultation with a specialist and diagnosis, treatment for the disease is prescribed.
Cystitis is a disease of the honeymoon, and also of short skirts!
In medical terms, “cystitis” is an inflammation of the bladder. What does this tell us? But, in fact, nothing concrete and understandable, but its symptoms will tell you a lot. However, more on that later. Cystitis occurs more often in women, due to our anatomical nature, our urethra is short compared to men's, and therefore it is easier for infection to reach the bladder.
Cystitis is divided into two types:
- Acute
- which develops rapidly, pain during urination increases, and over time becomes constant. The sooner treatment is started (under the guidance of a doctor), the greater the chance that the attack will not recur; - Chronic
is an advanced form of cystitis, in which, due to a number of factors, regular repetitions of attacks of cystitis occur. Self-medication and the hope that “it will go away on its own” lead to the chronic form.
An attack of cystitis is difficult to confuse with anything else; its intensity is so noticeable that the attack will not go unnoticed.
So, the symptoms of acute cystitis
speakers:
- Pain when urinating;
- Sharp or dull pain in the suprapubic region;
- Frequent urination and the urge to urinate (every 10-20 minutes) with little urine output;
- Discharge of a small amount of blood at the end of urination;
- Cloudy urine color, sometimes pungent odor;
- Rarely: chills, fever, fever, nausea and vomiting.
For chronic cystitis
characteristic:
- Less severe pain when urinating;
- The same symptoms as with acute cystitis, but the picture may be blurred (some symptoms are present, others are absent);
- Well, the most “important” symptom is recurrence of attacks 2 or more times a year.
Treatment
For successful treatment, it is necessary to accurately identify the causative agent of the disease; diagnosis is very important.
To do this, it is necessary to conduct the following research:
- general analysis of urine and blood;
- urine test for bacterial culture;
- cytoscopy;
- The amount of antibodies to each microorganism is determined in the blood.
It is extremely important for patients to follow all recommendations during treatment and complete the full course. Under no circumstances should you reduce the duration of medication or skip therapy.
Modern drugs are much more effective than those that were previously available and reduce treatment time.
Treatment must be completed, tests must be taken again, and only after they show that the infection has disappeared can we talk about complete victory over the disease.
However, it is necessary to avoid factors that provoke the occurrence of the disease and diligently adhere to preventive measures.