Polyneuritis - damage to the structure of multiple nerve fibers can develop at any age. In rare cases, the disease occurs and develops as an independent illness, but most often it is a secondary complication of toxic poisoning, trauma, diabetes, and alcohol addiction. The first possible signs of polyneuritis are considered to be the appearance of a feeling of numbness and “running” goosebumps in the extremities, recorded over several weeks; later, a decrease in physiological muscle tone and insufficiency of tendon reflexes are noted.
Types and features of polyneuritis
The disease is characterized by predominant pathological damage to the distal, that is, distant parts of the nervous system of the extremities, this is manifested by a decrease in sensitivity and strength in the hands and feet, while in the higher located parts these signs characteristic of the disease appear already in advanced cases.
Treatment of the disease depends on the influence of the primary cause, so during diagnosis it is necessary to identify this provoking factor.
Polyneuritis, first of all, covers the nerve sections of the limbs, therefore the symptoms of the disease are associated precisely with this area of the human body. Polyneuritis of the extremities usually begins with a feeling of decreased temperature in the feet and hands, and later a loss of sensitivity occurs.
The pathological reactions that occur in the nerves are characterized by the presence of dystrophic changes; their inflammation is not typical in this disease.
The course of polyneuritis and its prognosis depend on the cause of the disease, so the attending physician must determine the etiology of the disease before treatment.
Alcoholic polyneuritis
It is characterized by the simultaneous appearance of severe sensory and motor disorders. For this type of disease, the characteristic defining symptom is the presence of mental disorders, the most obvious of which is pathological memorization - the patient does not remember the events that occurred and may distort events and facts.
The patient fills in the gaps in memory with fiction, which sometimes has an obviously fantastic plot. To this is added polyneuritis of the lower extremities. The legs or arms become bluish, lose sensitivity and mobility.
Polyneuritis of the kidneys
Develops with severe glomerulonephritis and pyelonephritis. The disease is associated with impaired glomerular filtration. Swelling appears in the lower extremities, weakening of the arms and legs.
Acute polyneuritis
Usually develops during or after illnesses with a viral nature of origin. After eliminating the main cause, low-grade fever, “aches” in the limbs, and severe, burning pain along the nerves appear. All symptoms increase in a matter of hours or days.
Diabetic polyneuritis
Develops in patients with diabetes mellitus. In some cases, disturbances in the limbs that are noticeable to the patient are recorded earlier than the symptoms of the underlying disease.
With successful treatment of the underlying disease, the symptoms of polyneuritis can persist for a long time, manifested by difficulties in walking, the inability to perform precise manipulations with the fingers, muscle atrophy and paresis.
As already mentioned, the cause of polyneuritis can be various diseases. Thus, VSD against the background of cervical osteochondrosis can lead to the manifestation of symptoms of polyneuritis. You can read about this in this article.
Symptoms and manifestations of hydrocephalus or dropsy of the brain are quite extensive and varied. Read more about the disease.
Chronic polyneuritis
Gradually develops with constant exposure to the disease-provoking factor. Severe weakness and atrophy in the muscles located in the lower and upper extremities slowly increases, then signs of changes in the functions of the brain and spinal cord appear, speech disorders and inflammation of the meninges may be recorded.
Toxic polyneuritis
Develops under the influence of alcohol, salts of heavy metals. Depending on the amount of toxin entering the body, it can be acute or subacute.
Acute poisoning is accompanied by obvious symptoms of intoxication - vomiting, pain in the digestive tract, diarrhea.
Then the noticeable signs that define polyneuritis and the deterioration of the general condition are added.
Vegetative polyneuritis
Occurs in cases of intoxication, thyrotoxicosis, and negative professional working conditions. This form of the disease is characterized by the spread of burning pain throughout the body, deterioration of tissue trophism, expressed by changes in temperature, excessive or insufficient sweating.
Infectious polyneuritis
It is caused by an infectious agent and is considered a long-term consequence of the disease. It begins with fever, lesions in the extremities are usually recorded in two at once and develop along an ascending path, that is, from the feet to the higher nerve fibers.
Alimentary polyneuritis
It is caused by a lack of vitamin B in food or its improper absorption by the body. In addition to signs of pathological damage in the peripheral nerves of the extremities, serious disturbances in cardiac activity are recorded.
Types
Polyneuritis of the lower extremities
- infectious type. Appears due to catarrh of the upper respiratory tract. A type such as infectious polyneuritis involves an increase in temperature, as well as inflammation of cells;
- diphtheria type. Appears when treatment is started incorrectly or untimely. The soft palate is paralyzed, the nasal tone in the voice increases. Eating as a result of vagus nerve disease is usually difficult;
- lead type. It often appears due to the consumption of sour berry jam, which was preserved in clay dishes. The disease affects the radial nerves. The patient complains of abdominal pain, as well as lead plaque in the gum area;
- arsenic type. There are two types: household and professional. Signs of the disease are stomach pain, vomiting and paralysis of the lower extremities;
- diabetic type. Suggests nerve damage to the face, arms, or legs;
- professional type. Occurs in people whose professional activities involve tools that emit vibration or work that involves strong muscle tension. Symptoms include pain in the hand, pale fingertips and sweating.
Differences between polyneuritis and neuritis
The main difference between polyneuritis and neuritis is the generalization of the entire pathological process. With neuritis, one nerve may suffer, which is manifested by the presence of pain at its location.
With polyneuritis, nerve damage is usually defined as symmetrical and affects several groups at once, which only aggravates the severity of the disease and the patient’s well-being, gait and performance are impaired.
The cause of local neuritis can be tumors, injuries or arthritis, while polyneuritis has an infectious and toxic etiology of origin.
Alcoholic polyneuropathy
Ethanol disrupts the integrity of neuron processes and their membranes, which is manifested by sweating of the hands, swelling of the hands and feet.
The disease progresses slowly and - which is typical - when you give up alcohol, the functions of the nerve fibers are resumed.
Alcoholic neuropathy is often associated with brain damage. If it turns into dementia, normalization of the activity of nerve cells when giving up alcohol is impossible.
The disease is treated with vitamin therapy, drugs that improve tissue respiration, and hepatoprotectors.
Reversibility distinguishes alcoholic polyneuropathy from all other types of disease, but not everyone is able to cope with the addiction.
One of the complications of diabetes is diabetic neuropathy of the lower extremities, which can lead to gangrene if treatment is not started in time.
The massage technique for neuritis of the facial nerve is described here.
An occupational disease for drillers and people who work on vibrating equipment is vibration disease. Symptoms, types and diagnosis are described in the article.
Causes of polyneuritis
The reasons leading to the development of polyneuritis are conventionally divided into several groups:
- Infections - sore throat, diphtheria, influenza, various types of typhoid infection, severe dysentery.
- Exogenous intoxication factors - poisoning with alcohol substitutes, lead, chlorophos, arsenic.
- Endogenous intoxications developing with diabetes mellitus, thyroid pathologies, nephritis.
- Avitaminosis is a lack of B vitamins.
- Professional working conditions – constant work in the cold, vibration of tools.
- Chronic metabolic disorders.
In addition, the development of polyneuritis can be facilitated by the presence of a disease such as encephalopathy. They are inextricably linked and are characterized by loss of sensitivity and motor functions of the extremities, both upper and lower.
The signs of polyneuropathy of alcoholic origin are similar to the manifestations of polyneuritis. It is very important, when you first notice symptoms, to immediately seek qualified help.
The prognosis for the treatment of alcoholic encephalopathy in the later stages is most often unfavorable. You will find out why from the article.
How to cure a nervous tic of the eye in various ways is described in detail here https://gidmed.com/bolezni-nevrologii/nevralgija/nervnyj-tik-glaza-prichiny-vozniknoveniya-i-lechenie.html.
Prevention measures
Polyneuritis can develop in any person; the main measures to prevent it include the following:
- Elimination of the influence of toxic substances.
- Prevention of viral infections.
- Compliance with safety precautions when working with poisons.
- In special working conditions - compliance with all recommendations for performing work.
A balanced and rational diet and treatment of chronic diseases are important in preventing illness.
Polyneuritis is a serious and dangerous disease associated with damage to the peripheral nervous system. The pathology is multiple and extensive. Polyneuritis is accompanied by multiple paresis, decreased functionality and sensitivity of the limbs. With the acute nature of the disease, polyneuritis can become complicated. Inflammatory processes that have spread to the central nervous system significantly worsen the patient’s well-being.
Symptoms of the disease
Patients note the following symptoms:
- Periodic goosebumps, burning sensation and numbness.
- On examination, the skin of the extremities is pale, sometimes with a marbled pattern, colder to the touch than the rest of the body and moist due to excessive sweating.
- Weakness in the muscles begins to manifest itself as discomfort when performing usual work - patients cannot fasten buttons, it is difficult to hold small objects in their hands.
- On the feet, the muscles involved in dorsiflexion weaken, this leads to the fact that the leg seems to hang down and when walking a person is forced to raise the limb high.
- Sensitivity is impaired - many patients do not feel touch, changes in external temperature, or pricks with sharp objects. At the same time, burning and severe pain are expressed.
- Changes in deep-seated muscles lead to movement disorders, unsteady gait, and trembling of the hands.
- Over time, the skin on the extremities becomes thinner, becomes swollen and acquires a dark purple hue, and the structure of the nails changes.
In unfavorable cases, the fibers of the vagus nerve may be involved in the pathological process, which is manifested by a functional disorder of breathing and cardiovascular activity.
Severe pneumonia with severe shortness of breath and tachycardia is recorded. Without appropriate treatment, this condition can be fatal.
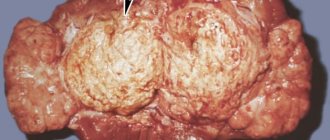
The photo shows damage to the lower extremities with polyneuritis:
Preventive measures
To reduce the likelihood of developing kidney polyneuritis, doctors recommend:
- completely give up bad habits (tobacco, alcohol), follow the principles of a healthy lifestyle;
- eat well and properly, avoid eating too salty, pickled, smoked and too fatty foods;
- avoid hypothermia, protect the lower back (at low temperatures, wear high-waisted trousers, a jacket below the knees, a special woolen belt, etc.);
- promptly diagnose and treat kidney infections and urinary tract infections;
- strengthen the immune system;
- observe safety precautions at work.
Have you had your kidneys checked lately?
Since renal polyneuritis is most often a consequence of pyelonephritis or glomerulonephritis, it is important to be attentive to your health and undergo regular preventive examinations. Timely diagnosis and treatment of acute kidney infections in most cases leads to complete recovery of the patient without the disease progressing to the chronic stage. This significantly reduces the risk of developing polyneuritis and other serious complications.
Diagnostics
Making a diagnosis is usually not difficult. The doctor examines and interviews the patient.
Among additional research methods, the following are important:
- Determination of the presence of toxic substances in biological fluids - urine, blood.
- Examination of internal organs and endocrine system.
- Exclusion of oncological pathologies.
- Electromyography is a study aimed at studying the electrical impulses of muscle fibers. This examination is recommended to be performed during the treatment period as a control over the improvement of the disease.
Treatment
All forms and types of polyneuritis begin to be treated according to the same scheme:
- In the acute period, bed rest and rest are prescribed.
- It is necessary to eliminate the influence of intoxication; in case of acute poisoning detected by laboratory diagnostics, antidotes are administered, that is, drugs aimed at neutralizing toxins.
- For infectious polyneuritis, 4% Urotropin or 1% Tripaflavin is administered for several days. For the diphtheria form, the administration of anti-diphtheria serum is indicated; for the influenza form, interferons and gamma globulins are indicated.
- Detection of vitamin deficiencies requires a course of vitamin complexes, especially from group B.
- To reduce swelling on nerve fibers, Magnesium sulfate, Glucose, and diuretics are prescribed.
- Improve microcirculation and metabolism by using Aminalon, Nootropil, Trental, and potassium supplements.
- Analgesic therapy is selected based on the severity of the pain symptom and the presence of concomitant diseases.
After the acute period, physiotherapy, massage, mud therapy, therapeutic exercises, and reflexology are indicated. To prevent the development of contractures in cases of severe atrophy and weakness in the limbs, splints are put on them.
The recovery period lasts several months, during which time sanatorium-resort treatment, constant massage and gymnastics, and a specially formulated diet have a good effect.
The diet should be especially rich in B vitamins - pork, buckwheat and oatmeal, eggs, dairy products, liver, kidneys, brewer's yeast.
It is recommended to constantly drink freshly prepared vegetable and fruit juices, especially carrots. During the recovery period, radon and hydrogen sulfide communal baths are used.
Unconventional methods of treatment
Traditional methods of treatment can be considered only after the acute signs of the disease have been eliminated. The patient is recommended to drink herbal decoctions that improve metabolic processes in the body and use compresses.
- Crushed stems and leaves of garden raspberries in the amount of a tablespoon are poured into a glass of boiling water and left for a little less than an hour. Take three tablespoons before meals.
- A spoonful of Ivan tea herb is poured with half a liter of boiling water, placed in a thermos and left for 8 hours. Drink the infusion throughout the day.
- Nettle and birch leaves improve metabolic processes. They can be brewed separately or together at the rate of one spoon of the mixture per half liter of boiling water. The prepared decoction is drunk a day before.
To prepare compresses or baths, take plants such as wormwood, birch and eucalyptus branches, and pine shoots. To prepare a bath, 100 grams of the plant and a liter of boiling water are enough, the resulting infusion is poured into water.
Folk remedies
“Grandma’s” recipes can be used as an independent preventive measure and as an addition to therapy prescribed by a doctor. For urological diseases, brew lingonberries, cranberries, chamomile, raspberries, fireweed, and make warm compresses from red clay and vinegar or from a decoction of elderberry and chamomile flowers. Lotions made from poppy pods have an analgesic effect.
Traditional medicine offers the following recipes:
- half a tablespoon of dried birch leaves and the same amount of dried nettle leaves, pour 0.5 liters of boiling water, leave for 1 hour, drink everything on the same day;
- 1 tbsp. Pour 0.5 liters of hot water over fireweed tea and leave overnight. Drink 1/3 of the decoction per day in 3 servings;
- 1 tbsp. Infuse dried raspberry stems and leaves in a glass of boiling water for 40 minutes. Take 3 tablespoons before meals;
- Brew 100 g of a mixture of pine stems and wormwood, birch and eucalyptus leaves with 1 liter of boiling water. Pour the resulting infusion into a bath, which should be taken at night for 15 minutes.
Folk remedies must be approved by a doctor. Otherwise, the situation may get worse. For example, consuming a decoction of rose hips, lingonberry or cranberry juice is fraught with the deposition of salt crystals.
Alcoholic encephalopathy is damage to brain cells caused by long-term alcohol addiction. The disease causes serious consequences that can greatly aggravate the health condition.
As a result of excessive alcohol consumption, another dangerous disease develops - alcoholic polyneuropathy. Read about the symptoms and treatment of this disease here.
You can read how diabetic polyneuropathy is treated in this material.
Consequences and prognosis
Timely treatment of polyneuritis usually results in a favorable outcome; it must be taken into account that the restoration of nerve fibers takes months.
Therefore, during the recovery period, it is necessary to fully comply with all the doctor’s recommendations, undergo physical therapy and pay attention to nutrition.
It is also necessary to exclude contact with substances that cause intoxication - repeated exposure to them leads to relapses, the treatment of which will be difficult and long.
If parts of the vagus nerve are involved in the process and if help is not provided in time for this condition, the outcome of the disease can be fatal.
Frequent and prolonged headaches in the temple area should not go unnoticed. Any pain must be correctly diagnosed and treated in order to avoid serious consequences in the future.
Everything about the symptoms and treatment of occipital neuralgia is described in detail in the article.
Pathological anatomy
Rice.
1. Microscopic specimen of the vagus nerve in polyneuritis: arrows indicate accumulations of macrophages in foci of segmental demyelination; hematoxylin-eosin staining; x 100. Fig. 2. Microslide of the optic nerve for polyneuritis: infiltrate in the focus of demyelination, containing lymphocytes (1) and macrophages (2); hematoxylin-eosin staining; X 400. Fig. 3. Microscopic specimen of nerve fibers of the anterior root of the spinal nerve in acute polyradiculoneuritis: 1 - clear and band-like swelling, 2 - lysis of the nerve fiber, 3 - proliferation of lemmocytes; silver impregnation; X 1500. In pathomorphology. P. is divided into parenchymal and interstitial. Among parenchymal P., there are forms with predominant changes in myelin and lemmocytes (periaxonal P.) and forms with a predominance of axon damage (axonal P.). Interstitial P. are characterized by changes in the membranes and vessels of peripheral nerves. Forms involving the roots and spinal ganglia are called polyradiculoneuritis. Depending on the etiology of the pathomorphology process, the picture has a number of differences. In acute primary P. of infectious-allergic origin, clinically occurring as Landry's ascending paralysis (see Landry ascending paralysis) or Guillain-Barre-Strol syndrome, a predominant lesion of the myelin sheaths is observed. In the early stages of these diseases, there is an accumulation of mononuclear cells near the myelin sheaths, which undergo decay. At the same time, lemmocytes proliferate, and their number increases 8-14 times. The myelin sheaths swell, acquire a honeycomb-like structure, myelin balls form and, in some places, myelin dissolves. In foci of demyelination, especially those located perivenously, focal necrosis is formed (Fig. 1) with an accumulation of macrophages containing fat. Inflammatory perivenous and pericapillary infiltrates consist of lymphoid cells, polymorphic mononuclear cells, and macrophages (Fig. 2). The axon increases in size, its ribbon-like swelling occurs, clear-shaped swellings are formed along the axon, lysis of fibers and proliferation of lemmocytes occur (Fig. 3). The death of nerve fibers leads to the development of Wallerian degeneration (see Wallerian degeneration). Due to the destruction of myelin, the endoneural spaces are brought closer together, and the perineural spaces are expanded and infiltrated with lymphoid elements. The inflammatory and demyelinating process in primary P. is reversible. Remyelination occurs in the 2-3rd week. from the onset of the disease, as a rule, is accompanied by regeneration of nerve fibers. In rare cases, axons die and collagen fibrils and amorphous endoneurium substance form in their place.
Rice. 4. Microscopic specimen of a nerve fiber in porphyrin polyneuritis: 1 — decay of nerve fibers, 2 — endoneurium fibers, 3 — macrophages, 4 — bundles of slightly changed nerve fibers; Van Gieson staining; X 460.
With hypovitaminosis, diabetic, toxic, porphyrin, alcoholic P., predominantly axonal damage is observed, which is accompanied by axonal degeneration, proliferation of lemmocytes, swelling of motor motor terminal plaques. In nerve fibers, various stages of axonal death can be traced, up to their complete disappearance. In place of the dead nerve fibers, randomly located endoneurium fibers and macrophages remain (Fig. 4). Simultaneously with axon degeneration, regeneration processes can be traced, when new small fibers are formed in place of dead fibers. In the later stages of regeneration in myelinated nerve fibers, individual axons reach normal size, most of them remain atrophic. Axonal neuropathy is accompanied by myelin degeneration, most often in the form of segmental demyelination. This mixed pathology is explained by the involvement of lemmocytes in the process and disruption of the myelin formation process. In ultrastructural studies, disruption of metabolic processes in axons is manifested by thinning of axoplasmic organelles, vacuolization and reduction of axon diameter, and accumulation of glycogen in lemmocytes.
Interstitial P. are observed in common infections: viral hepatitis, leprosy, herpes zoster (see Herpes), etc., as well as in arteritis, rheumatoid arthritis, ischemia, amyloidosis and other diseases. Patol. the process is characterized by an increase in endoneurial collagen with the formation of inflammatory changes in the interstitial tissue of peripheral nerves. Moderate proliferation of lemmocytes is noted.
Morphol. differentiation of various forms of P. presents significant difficulties and must be supplemented by electron microscopic studies of material taken by biopsy of cutaneous nerves (eg, sural nerve), with determination of the nature of changes in the axon, lemmocytes and myelin sheaths. It is important to determine the caliber and density of fibers, their length between the nodes of Ranvier, as well as the morphometric assessment of nerve fibers deprived of myelin.