Diabetic nephropathy (or chronic kidney disease) is a set of kidney pathologies associated with diabetes mellitus. Often the symptoms caused by this particular disease become the first signs of diabetes noticeable to a person.
The course of diabetes, often hidden at the beginning, eventually leads to vascular disorders throughout the body: the kidneys are the first to suffer. In addition to nephropathy, diabetes also causes complications in the form of retinopathy (on the eyes), neuropathies (on the nervous system), arthropathy (on the joints), and general angiopathy (on the blood circulation in general). Nephropathy is the general name for various kidney injuries: from stenosis (narrowing) of the renal arteries to pyelonephritis (kidney infection) and nephronecrosis (kidney death).
Description
Diabetic nephropathy.
Specific pathological changes in the renal vessels that occur in both types of diabetes mellitus and lead to glomerulosclerosis, decreased renal filtration function and the development of chronic renal failure (CRF). Diabetic nephropathy is clinically manifested by microalbuminuria and proteinuria, arterial hypertension, nephrotic syndrome, signs of uremia and chronic renal failure. The diagnosis of diabetic nephropathy is based on determining the level of albumin in the urine, the clearance of endogenous creatinine, the protein and lipid spectrum of the blood, ultrasound data of the kidneys, and ultrasound examination of the renal vessels. In the treatment of diabetic nephropathy, diet, correction of carbohydrate, protein, and fat metabolism, taking ACE and ARB inhibitors, detoxification therapy, and, if necessary, hemodialysis and kidney transplantation are indicated.
Hemodialysis and peritoneal dialysis
Extracorporeal methods are prescribed by a council of specialists. It is used at the last stage for the purpose of detoxification, removing excess potassium, nitrogen and urea from the blood. The criterion for these procedures is a creatinine level of over 500 µmol/l.
Before hemodialysis, a special intravenous catheter is installed, which is connected to a special device that takes blood, and then purifies it and immediately returns it to the patient’s vascular bed. This procedure should be performed several times a week and only in a clinical setting, as it is associated with the risk of infectious complications and hypotension.
A feature of peritoneal dialysis is that the peritoneum performs the filter function, so the catheter is installed in the abdominal cavity. Then liquid is injected inside, which then flows out on its own through the tubes. Through this, excess toxic substances are removed.
Hemodialysis
To prevent the development of CKD, improve the prognosis and maintain a fairly high level of quality of life, it is necessary to regularly undergo a comprehensive examination, monitor glucose levels daily and take maintenance drug therapy prescribed by the attending physician.
Interesting:
- Indications for a urine test for UIA, reasons for increased albumin levels, preparation for the examination, interpretation of the results and the norm for diabetes mellitus
- Indications for tests for diabetes mellitus, their information content and potential complications of the disease
- Treatment and prevention of ketoacidosis in type 2 diabetes mellitus
- Symptoms of glycemic coma, how to recognize and treat the disease
- Dizziness in diabetes mellitus: causes and treatment
- Treatment methods for impotence in diabetes mellitus, causes of the disorder, diagnosis, potential complications, prognosis and prevention
- Causes of rash in severe diabetes mellitus, symptoms, principles of treatment, diagnosis and complications
Additional facts
Diabetic nephropathy is a late complication of diabetes mellitus types 1 and 2 and one of the main causes of death in patients with this disease. Damage to large and small blood vessels that develops in diabetes (diabetic macroangiopathy and microangiopathy) contributes to damage to all organs and systems, primarily the kidneys, eyes, and nervous system. Diabetic nephropathy occurs in 10-20% of patients with diabetes; Somewhat more often, nephropathy complicates the course of the insulin-dependent type of disease. Diabetic nephropathy is detected more often in male patients and in persons with type 1 diabetes mellitus that developed during puberty. The peak development of diabetic nephropathy (stage of chronic renal failure) is observed with a duration of diabetes of 15-20 years.
ICD-10 code, causes of occurrence in children and adults
The definition of “diabetic nephropathy” is a collective concept that unites a complex of diseases that result in damage to blood vessels in the kidneys against the background of acute diabetes mellitus.
The term “Kimmelstiel-Wilson syndrome” is often used for this disease, because the concepts of nephropathy and glomerulosclerosis are used as synonymous.
For diabetic nephropathy according to ICD 10, 2 codes are used. Therefore, diabetic nephropathy code according to ICD 10 can have both E.10-14.2 (diabetes mellitus with kidney damage) and N08.3 (glomerular lesions in diabetes). Most often, impaired renal activity is seen in insulin-dependent type 1 - 40-50%, and in type 2 the prevalence of nephropathy is 15-30%.
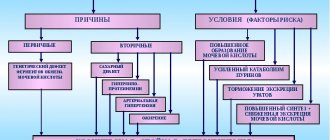
Reasons for development
Doctors have three main theories regarding the causes of nephropathy:
- exchange . The essence of the theory is that the main destructive role is attributed to an elevated level of glucose in the blood, which is why vascular blood flow is disrupted and fats are deposited in the vessels, which leads to nephropathy;
- genetic _ That is, a hereditary predisposition to the disease. The meaning of the theory is that it is genetic mechanisms that cause diseases such as diabetes and diabetic nephropathy in children;
- hemodynamic . The theory is that in diabetes there is a disturbance in hemodynamics, that is, blood circulation in the kidneys, which causes an increase in the level of albumin in the urine - proteins that destroy blood vessels, the damage in which becomes scarred (sclerosis).
In addition, the reasons for the development of nephropathy according to ICD 10 often include:
- smoking;
- high blood sugar levels;
- increased blood pressure;
- poor triglycerides and cholesterol levels;
- anemia.
Often, the following diseases are identified in the nephropathy group:
- diabetic glomerulosclerosis;
- atherosclerosis of the renal artery;
- necrosis of the renal canals;
- fatty deposits in the renal canals;
- pyelonephritis.
Symptoms
Causes
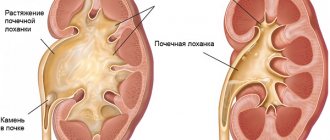
Diabetic nephropathy is caused by pathological changes in the renal vessels and glomeruli of capillary loops (glomeruli), which perform a filtration function. Despite various theories of the pathogenesis of diabetic nephropathy considered in endocrinology, the main factor and trigger for its development is hyperglycemia. Diabetic nephropathy occurs due to long-term insufficient compensation for carbohydrate metabolism disorders. According to the metabolic theory of diabetic nephropathy, constant hyperglycemia gradually leads to changes in biochemical processes: non-enzymatic glycosylation of protein molecules of the renal glomeruli and a decrease in their functional activity; disruption of water-electrolyte homeostasis, fatty acid metabolism, reduction of oxygen transport; activation of the polyol pathway for glucose utilization and toxic effects on kidney tissue, increasing the permeability of renal vessels. The hemodynamic theory in the development of diabetic nephropathy assigns the main role to arterial hypertension and disturbances of intrarenal blood flow: an imbalance in the tone of the afferent and efferent arterioles and an increase in blood pressure inside the glomeruli. Long-term hypertension leads to structural changes in the glomeruli: first to hyperfiltration with accelerated formation of primary urine and the release of proteins, then to the replacement of glomerular tissue with connective tissue (glomerulosclerosis) with complete occlusion of the glomeruli, a decrease in their filtration capacity and the development of chronic renal failure. The genetic theory is based on the presence in a patient with diabetic nephropathy of genetically determined predisposing factors that manifest themselves in metabolic and hemodynamic disorders. All three developmental mechanisms are involved and closely interact with each other in the pathogenesis of diabetic nephropathy. Risk factors for diabetic nephropathy are arterial hypertension, prolonged uncontrolled hyperglycemia, urinary tract infections, lipid metabolism disorders and excess weight, male gender, smoking, and the use of nephrotoxic drugs.
Symptoms
Diabetic nephropathy is a slowly progressive disease, its clinical picture depends on the stage of pathological changes. In the development of diabetic nephropathy, the stages of microalbuminuria, proteinuria and end-stage chronic renal failure are distinguished. For a long time, diabetic nephropathy is asymptomatic, without any external manifestations. At the initial stage of diabetic nephropathy, there is an increase in the size of the glomeruli of the kidneys (hyperfunctional hypertrophy), increased renal blood flow and an increase in the glomerular filtration rate (GFR). Several years after the onset of diabetes mellitus, initial structural changes in the glomerular apparatus of the kidneys are observed. A high volume of glomerular filtration remains, urinary albumin excretion does not exceed normal levels (Incipient diabetic nephropathy develops more than 5 years from the onset of pathology and is manifested by constant microalbuminuria (30-300 mg/day or 20-200 mg/ml in the morning portion urine). Periodic increases in blood pressure may be observed, especially during physical activity. Deterioration in the well-being of patients with diabetic nephropathy is observed only in the later stages of the disease. Clinically pronounced diabetic nephropathy develops after 15-20 years with type 1 diabetes mellitus and is characterized by persistent proteinuria (protein levels in urine - 300 mg/day), indicating the irreversibility of the damage. Renal blood flow and GFR decrease, arterial hypertension becomes constant and difficult to correct. Nephrotic syndrome develops, manifested by hypoalbuminemia, hypercholesterolemia, peripheral and cavitary edema. Levels of creatinine and blood urea are normal or slightly increased. At the terminal stage of diabetic nephropathy, there is a sharp decrease in the filtration and concentration functions of the kidneys: massive proteinuria, low GFR, a significant increase in the level of urea and creatinine in the blood, the development of anemia, severe edema. At this stage, hyperglycemia, glycosuria, urinary excretion of endogenous insulin, as well as the need for exogenous insulin can significantly decrease. Nephrotic syndrome progresses, blood pressure reaches high values, dyspeptic syndrome, uremia and chronic renal failure develop with signs of self-poisoning of the body with metabolic products and damage to various organs and systems. Metallic taste in the mouth.
Signs and symptoms of diabetic nephropathy
The first warning signs are:
Before they die, nephrons become “leaky.” They begin to leak proteins into the urine that should not be there, namely, a large amount of albumin. When the content of this protein in urine varies from 20 to 300 mg/l, we speak of microalbuminuria.
This pathology can be cured. But its more severe stage - proteinuria - is considered irreversible and indicates that renal failure has developed. In the first months, diabetic nephropathy together with microalbuminuria almost does not manifest itself.
The initial symptoms of this pathology are very similar to a simple runny nose or chronic fatigue:
- legs swell;
- elevated blood pressure persists;
- weakness;
- frequent urge to go to the toilet (often at night);
- anemia.
Few patients can associate such symptoms with poor kidney function. And if a diabetic rarely undergoes blood and urine tests, then the pathology is detected too late.
Later, signs of intoxication appear more clearly:
- thinness appears;
- skin itching and rashes;
- swelling of the eyes;
- muscle cramps;
- disturbance of consciousness.
Diagnostics
Early diagnosis of diabetic nephropathy is a critical challenge. In order to establish a diagnosis of diabetic nephropathy, a biochemical and general blood test, a biochemical and general urine test, a Reberg test, a Zimnitsky test, and an ultrasound scan of the renal vessels are performed. The main markers of the early stages of diabetic nephropathy are microalbuminuria and glomerular filtration rate. During annual screening of patients with diabetes, the daily excretion of albumin in urine or the albumin/creatinine ratio in the morning portion is examined. The transition of diabetic nephropathy to the stage of proteinuria is determined by the presence of protein in a general urine test or urinary albumin excretion above 300 mg/day. There is an increase in blood pressure and signs of nephrotic syndrome. The late stage of diabetic nephropathy is not difficult to diagnose: in addition to massive proteinuria and a decrease in GFR (less than 30 - 15 ml/min), an increase in the levels of creatinine and urea in the blood (azotemia), anemia, acidosis, hypocalcemia, hyperphosphatemia, hyperlipidemia, facial edema is added. and the whole body. It is important to carry out a differential diagnosis of diabetic nephropathy with other kidney diseases: chronic pyelonephritis, tuberculosis, acute and chronic glomerulonephritis. For this purpose, bacteriological examination of urine for microflora, ultrasound of the kidneys, and excretory urography can be performed. In some cases (with early developed and rapidly increasing proteinuria, sudden development of nephrotic syndrome, persistent hematuria), a fine-needle aspiration biopsy of the kidney is performed to clarify the diagnosis.
Treatment
The main goal of treatment of diabetic nephropathy is to prevent and delay as much as possible further progression of the disease to chronic renal failure, and reduce the risk of developing cardiovascular complications (coronary artery disease, myocardial infarction, stroke). What is common in the treatment of different stages of diabetic nephropathy is strict control of blood sugar, blood pressure, compensation for disorders of mineral, carbohydrate, protein and lipid metabolism. The first choice drugs in the treatment of diabetic nephropathy are angiotensin-converting enzyme (ACE) inhibitors: enalapril, ramipril, trandolapril and angiotensin receptor antagonists (ARA): irbesartan, valsartan, losartan, which normalize systemic and intraglomerular hypertension and slow the progression of the disease. The drugs are prescribed even with normal blood pressure in doses that do not lead to the development of hypotension. Starting from the stage of microalbuminuria, a low-protein, salt-free diet is indicated: limiting the consumption of animal protein, potassium, phosphorus and salt. To reduce the risk of developing cardiovascular diseases, it is necessary to correct dyslipidemia through a low-fat diet and taking medications that normalize the blood lipid spectrum (L-arginine, folic acid, statins). At the terminal stage of diabetic nephropathy, detoxification therapy, correction of diabetes treatment, taking sorbents, anti-azotemic agents, normalization of hemoglobin levels, and prevention of osteodystrophy are required. If there is a sharp deterioration in kidney function, the question is raised whether the patient should undergo hemodialysis, continuous peritoneal dialysis, or surgical treatment by transplanting a donor kidney.
Treatment of nephropathy in diabetes mellitus
Depending on the degree of disease progression, treatment for diabetic nephropathy will vary. If we talk about the initial stages, it is enough to take preventive measures to avoid the development of irreversible changes in the kidneys. Such events include:
- decreased blood sugar levels;
- maintaining normal blood pressure;
- control and compensation of metabolic disorders in the body (carbohydrate, lipid, protein, mineral);
- maintaining a salt-free diet.
Thus, ARA-ACE inhibitors are most often prescribed to stabilize kidney function and blood pressure. Among them are such drugs as Enalapril, Fosinopril, Lisinopril, Trandolapril, Ramipril (ACE); "Valsaran", "Irbesartan", "Losartan" (ARA).
When diabetic nephropathy has reached the terminal stage, all possible treatment is reduced to radical therapy, dialysis (cleaning the blood of toxins using a special device) or kidney transplantation is indicated.
Diet should be as balanced as possible, regardless of the stage of the disease. So, starting from the stage of microalbuminuria, it is recommended to limit the consumption of protein foods (animal protein):
- Meat and offal;
- Fish (including caviar) and seafood;
- Eggs;
- Dairy products.
In addition, in order to correct high blood pressure at this stage, it is also necessary to follow a salt-free diet, that is, eliminating salt in any form from the diet. This rule also applies to such products as:
- pickled cucumbers and tomatoes;
- sauerkraut;
- salted and pickled mushrooms;
- canned fish and meat;
- carbonated and mineral drinks.
In the event of the development of hyperkalemia at the stage of chronic renal failure, it is also strongly recommended to limit potassium intake by replacing foods rich in potassium with foods that contain several times less potassium.
List of allowed foods low in potassium:
- cucumbers;
- Bell pepper;
- White cabbage;
- bulb onions;
- watermelon;
- melon;
- asparagus;
- cherry plum;
- cowberry;
- pears;
- pumpkin;
- strawberry;
- blueberry;
- cowberry;
- blueberry;
- cranberry;
- rose hip.
Foods with an average potassium content that can be consumed in moderation: cauliflower, eggplant, zucchini, green onions and leeks, green peas, lettuce, turnips, radishes, beets, carrots, tomatoes, persimmons, cherries, plums, apples, grapefruits, oranges, gooseberries, raspberries, blackberries, red currants.
List of foods high in potassium that are prohibited for hyperkalemia: Brussels sprouts and red cabbage, potatoes, yellow peas, nuts, radishes, spinach, rhubarb, sorrel, dried apricots, prunes, raisins, peaches, apricots, bananas, pineapples, dogwoods, mulberries, dates, black currant.
One of the leading roles in the regulation of phosphorus-calcium metabolism is assigned to the kidneys. As a result of disruption of their work and progression of chronic renal failure, conditions such as hyperphosphatemia and hypocalcemia may develop.
List of foods rich in calcium:
- dried apricots;
- sunflower seeds;
- dried fruits (mainly apples);
- oranges;
- raisin;
- figs;
- almond;
- peanut;
- sesame;
- cabbage;
- salad;
- onion;
- celery;
- olives;
- beans;
- rye and wheat bread.
Dietary nutrition in the treatment of diabetic nephropathy, especially in the case of proteinuria and chronic renal failure, has its positive results and is a fairly effective method in combating the development of irreversible processes in the renal structures.
But we should not forget that the clinical picture of the disease is very diverse. It is also important to take into account the individual characteristics of each patient’s body and, along with the use of a low-protein diet, control blood pressure levels and maintain carbohydrate metabolic processes.
Folk remedies
As an auxiliary therapy and only after consultation with your doctor, you can also turn to traditional medicine methods. Thus, medications can complement drug treatment or kidney recovery after therapy.
To restore impaired renal function, infusions and decoctions of various medicinal herbs are used, such as chamomile, cranberries, lingonberries, strawberries, rose hips, plantain, and rowan fruits.
Here are a few folk recipes that can help in the fight against diabetic nephropathy, especially in the initial stages of the disease:
- Pour pumpkin stalks with water in a ratio of one to five, boil, strain, and then drink a quarter glass before meals 3 times a day.
- Pour half a liter of boiling water over 10-15 bay leaves, leave for two hours, then take half a glass 3 times a day before meals.
- Pour 50 grams of dry bean leaves with a liter of boiling water, leave for 3 hours, drink half a glass once a day for a month.
- Pour two tablespoons of birch buds into a glass of water and bring to a boil, leave for half an hour, then consume two tablespoons warm before meals for two weeks.
In the later stages of the disease, when irreversible changes have occurred in the kidneys, dialysis or a complete kidney transplant is indicated. Using the dialysis procedure, the blood is purified by hardware instead of the kidneys. There are two types of this procedure:
- hemodialysis;
- peritoneal dialysis.
In hemodialysis, catheterization occurs directly into the artery. This method can only be carried out in a hospital setting due to possible unpleasant consequences (blood poisoning, sharp decrease in blood pressure).
In peritoneal dialysis, the catheter is inserted into the abdominal cavity rather than into an artery. This procedure must be carried out every day, and can be done at home, but the risk of infection at the tube entry points still exists.
After the organ transplant and for the period of its further functioning, the patient’s condition improves significantly, chronic renal failure and other life-threatening manifestations of the disease go away.
The main cause of kidney damage in people with diabetes is uncontrolled high blood sugar levels. Mandatory monitoring of this indicator with the help of insulin and other glucose-lowering drugs, as well as proper nutrition, help prevent or slow down the progression of the disease diabetic nephropathy.
Diet is of great importance in this regard, and it provides for fractional meals, at least five meals a day in small portions, an emphasis on vegetables, especially for people with excess body weight, and the rejection of sugar in favor of its substitutes. A varied diet with approximately the same amount of proteins, carbohydrates and fats is important.
It is reliably known that diabetic nephropathy develops mainly in patients who do not pay due attention to controlling sugar levels. Intensive therapy can reverse the process of glomerular hypertrophy and delay the development of microalbuminuria, preventing kidney damage.
Regular monitoring of blood pressure levels helps protect diabetics from complications such as kidney and heart diseases. Data show that for every 10 mmHg increase in blood pressure.
Intensive control of blood pressure slows down the development of the disease diabetic nephropathy, the stage of microalbuminuria can be prevented, and the level of proteinuria is reduced. In this case, antihypertensive drugs are mainly used.
Recent research has shown that the main cause of kidney tissue damage in diabetes is immune dysregulation, which causes the immune system to fight against its own cells. Immunotherapy is intended to correct dysregulation and control symptoms of diabetic nephropathy.
Prevention
Microalbuminuria, with timely and adequate treatment, is the only reversible stage of diabetic nephropathy. At the stage of proteinuria, it is possible to prevent the progression of the disease to chronic renal failure, while reaching the terminal stage of diabetic nephropathy leads to a condition incompatible with life. Currently, diabetic nephropathy and the resulting chronic renal failure are the leading indications for replacement therapy - hemodialysis or kidney transplantation. CRF due to diabetic nephropathy accounts for 15% of all deaths among patients with type 1 diabetes under 50 years of age.