Toxic kidney damage is one of the common diseases of the human body. Pathologies arise as a result of toxic substances entering the body from the outside or through their production by the body systems themselves. The disease is called toxic nephropathy (in medical circles - toxic kidney). As a rule, the pathology is manifested by a decrease in the total amount of urine per day, nausea, interruptions in heart function and high blood pressure. If a patient has been diagnosed with such a disease, then treatment is aimed at removing toxic substances and poisons from the body. For this, both drug therapy and hardware methods for purifying the patient’s blood (plasmapheresis and hemodialysis) can be used.
Important: the severe toxic course of the disease poses a particular danger to the patient. In this case, the kidneys may fail completely, and an organ transplant will be needed.
Classification
Toxic nephropathy is divided into two types:
- Specific. This type of toxic kidney damage is associated with acute toxicosis, which occurs during poisoning with various nephrotoxic substances. Liver intoxication causes kidney dysfunction. Specific nephropathy occurs when the body is exposed to toxic substances such as vitriol, arsenic, mercury and lead.
- Non-specific. This type of disease is provoked by hemodynamic disorders of various etiologies caused by severe poisoning of the body. Nonspecific nephropathy develops from insect bites, snake bites, alcohol overdose and consumption of low-quality foods.
The mechanism of development of such a pathology as an infectious-toxic kidney is associated with the impact of waste products of infectious agents on the body.
They have a destructive effect on the functioning of internal organs, including the kidneys. The consequence of this is damage to their structure, disruption of work and the development of a pathological condition.
Nephropathy - what is this pathology?
The human body is a complex and vulnerable mechanism. Any little thing can negatively affect it: hypothermia, stress, infection. Many diseases manifest themselves quickly and clearly, which allows you to begin the fight against the disease in a timely manner.
There is a category of diseases with a hidden course. They make themselves felt too late, when complications and serious health problems can no longer be avoided. This disease is nephropathy, that is, impaired renal function. Since the disease is asymptomatic , it is necessary to answer the question: what is nephropathy and who should be afraid of it?
What is nephropathy?
Renal nephropathy is a pathology in which the glomerular apparatus and renal parenchyma are affected, leading to a decrease in the functions of the organ.
Its ICD 10 code is N08. The kidney tissue is affected, and connective tissue enlarges and proliferates. The disease does not arise as an independent illness, but is a consequence of various serious diseases.
The insidiousness of the disease lies in its asymptomatic course over a long period of time. Patients with serious chronic diseases should be afraid of it. In some cases, it is impossible to determine which disease led to the development of the pathology. Then they talk about unspecified nephropathy .
With nephropathy of complex or mixed origin, the cause of the disease is a number of factors.
Classification of the disease
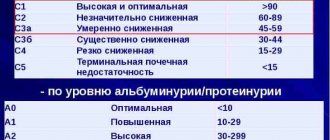
The disease does not manifest itself in any way at the first stage, but pathological processes in the kidneys have already started. There are several stages :
- Asymptomatic. There are no external signs of the disease; tests indicate the onset of the disease. They find an increase in glomerular filtration rate. Microalbumin is normal.
- Initial. The walls of the capillaries thicken, filtration and blood flow in the kidney increase. Microalbumin is also normal.
- Prenephrotic. Microalbumin increases, protein is not detected in the urine, and sometimes blood pressure increases.
- Nephrotic. Protein is constantly present in the urine, cholesterol and ESR are increased, and hemoglobin is decreased. Blood flow and filtration in the glomeruli decreases. The first external symptoms appear: swelling, increased blood pressure.
- Nephrosclerotic. Kidney function declines sharply. The level of creatinine and urea in the blood is increased. There is a high level of protein in the urine. Blood pressure is greatly increased. Almost always, renal failure develops at this stage.
Read all about kidney failure in our article.
Types of nephropathy are divided depending on the factors that influenced the occurrence of the disease:
- Metabolic (dismetabolic). Occurs due to metabolic disorders.
- Toxic and infectious-toxic. Occurs due to the negative effects of toxic substances: lead, chromium, copper sulfate, acetic acid. Or as a result of infectious diseases.
- Gouty. The cause is gout. In this form, the production of uric acid increases and its excretion decreases.
- Membranous. It is a consequence of tuberculosis or tumors. It is characterized by the fact that small vessels in the glomeruli thicken.
- Hypertensive. It is provoked by severe arterial hypertension and is characterized by damage to blood vessels in the kidneys. Leads to kidney failure.
- Analgesic. It occurs as a result of excessive use of analgesics with phenacetin, aspirin, paracetamol, and caffeine. Inflammation begins in the renal tubules and necrosis of the renal papillae. More common in women.
- Paraneoplastic. The cause is neoplasms in the lungs, stomach or thyroid gland. It develops very quickly.
- Ischemic. Occurs as a result of atherosclerosis of the renal vessels. Older people are usually affected. Leads to irreversible changes in the organ.
- Urate and oxalate. It is a consequence of increased secretion of uric acid crystals. One reason is genetic predisposition.
- Myeloma. Characterized by increased protein content in the urine. Progresses to kidney failure.
- Medicinal. Occurs as a result of taking medications. The temperature rises, a rash occurs, and signs of intoxication appear. It is treated by stopping the provoking drugs and prescribing drugs that relieve symptoms.
- Alcoholic. Caused by the effects of alcoholic beverages on the body. Manifested by frequent urination and the presence of blood in the urine. Treatment is aimed at cleansing the body of alcohol.
- Diabetic. The cause is diabetes. The kidney vessels become sclerotic and blood flow is impaired. The disease develops gradually over many years.
- Contrast induced. During an x-ray, a contrast agent is injected into the body. An individual negative reaction of the body may occur and nephropathy may develop. There is a risk of kidney necrosis. Treatment is surgery.
- IGA (IGA) nephropathy, or immune. The cause is infections of the upper respiratory tract and intestines. Immunoglobulin A is administered for treatment.
- Reflux nephropathy. It is formed due to the fact that urine from the bladder is thrown back into the kidneys, the so-called vesicoureteral reflux. The only treatment is surgery.
- Nephropathy of pregnancy. The specific causes of the disease have not yet been determined. Risk factors include alcohol and smoking. Appears in the second half of pregnancy. A woman's blood pressure rises significantly. In some cases, the only solution may be premature delivery.
In adults, triggering factors include diabetes, tumors, and pregnancy. In children, the disease has a primary and secondary nature. Primary nephropathy has hereditary causes. Secondary develops due to substances entering the child’s body that he is not able to remove.
(The picture is clickable, click to enlarge)
In newborns, ischemic nephropathy is a consequence of hypoxia, infection, acute blood loss during childbirth or drug therapy. As a result, the blood supply to the organ is disrupted.
(The picture is clickable, click to enlarge)
Causes and symptoms of the disease
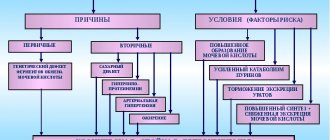
The reasons causing the appearance of such a severe pathology are primary and secondary in nature .
The primary form is caused by a congenital pathology of an organ or the kidney itself:
- abnormal location of the kidneys;
- irregular shape of the organ;
- violation of the kidney structure;
- abnormal development of the glomeruli of the kidney.
Often the root cause is kidney disease: pyelonephritis, glomerulonephritis. Nephropathy is often triggered by pregnancy. Secondary nephropathy is caused by exposure to external factors: diseases, tumors, toxic substances, alcohol, radiation.
This leads to serious disruption of the kidneys and poses a threat to the patient's life.
The insidious disease does not manifest itself in any way at the initial stage. Symptoms appear at the following stages :
- Swelling.
- Weakness.
- Pain in the lumbar region.
- Increased blood pressure.
- Headache.
- Increased fatigue.
- Constant feeling of thirst.
- Smell of ammonia from the mouth.
- Frequent urge to urinate.
- Cloudy and dark urine.
- A urine test reveals protein.
Diagnostic measures
To diagnose pathology, a standard plan :
- General urine analysis. Allows you to identify salt crystals.
- Biochemical urine analysis.
- Specific tests for calcification in urine.
- Ultrasound of the kidneys.
Treatment
Therapy requires hospitalization of the patient. The treatment program for the disease is based on the root cause. surgery is most often to eliminate the pathology of organ development.
In case of secondary nephropathy, therapy is aimed at destroying the factor that provoked it. Then medications are prescribed that eliminate the symptoms of the disease: high blood pressure, swelling.
The diabetic form in the first and second stages does not require therapy.
The task is to maintain blood sugar levels and adhere to the diet.
EHF therapy is used, that is, exposure of the kidneys to laser radiation. At the same time, the condition of the walls of the kidney vessels improves. At the third stage, hemodialysis may be prescribed. In extreme cases, a kidney transplant will be required.
Treatment of toxic, medicinal and alcoholic forms consists of ridding the body of toxic substances. Used: plasmapheresis, hemodialysis, forced diuresis.
For dysmetabolic nephropathy, vitamin therapy, diet, and normalization of lifestyle are indicated.
The gouty form involves treatment of the gout itself. In parallel, diuretics and antihypertensive drugs are prescribed. It is necessary to drink large amounts of fluid.
Nephropathy in pregnant women is treated in a hospital setting. Potassium supplements, diuretics, antihypertensives, and antispasmodics are prescribed. The patient is prescribed strict bed rest. The last resort is early delivery.
The use of traditional medicine is possible as part of complex therapy and after consultation with a doctor.
As monotherapy, traditional medicine is not effective and can lead to serious complications. Various renal herbal preparations, which have a diuretic and antibacterial effect, help well.
In addition to medications, the patient is prescribed a special diet , where the following is allowed:
- Buckwheat and oatmeal porridge.
- Lingonberry juice.
- Low-fat dairy products.
- Vegetables and fruits.
- Lean fish and chicken.
Forbidden:
- Spicy, salty, smoked, fried.
- Sweets and baked goods.
- Red meat.
- Alcohol.
- Canned foods.
Causes and pathogenesis
Kidney damage can occur due to the pathogenic influence of toxic substances and their breakdown products on their tissues, as well as as a result of an autoimmune reaction.
The kidneys continually work to remove waste products from the body, and some of these substances can cause problems with their function.
Experts identify the following factors that can cause the development of a pathology such as toxic kidney nephropathy:
- Taking medications. This is especially true for those medications that are used to provide emergency medical care to a patient.
- Poisonous mushrooms. The entry of such products into the human body is considered extremely dangerous, since they cause acute poisoning, often resulting in death.
- Compounds of heavy metals and nephrotoxic poisons. They have a negative impact on kidney function and cause disease.
- Treatment with antibiotics for a long time. The breakdown products of the active substances of drugs are excreted through the kidneys, and when they accumulate, the functioning of the organ is disrupted.
- Incorrect blood transfusion. Damage to kidney tissue occurs if the patient has been transfused with blood that is incompatible by group or Rh factor.
- Severe damage to the skin, causing blood poisoning and the development of an infectious-toxic kidney due to infection.
In addition, other reasons can cause serious changes in the kidneys, for example, mechanical injuries, radiation and electric shock.
Causes of the disease
The kidneys are a paired organ, similar in shape to a bean, which performs the following functions:
- regulate fluid balance in the body;
- control and maintain blood pressure at the proper level;
- participate in the process of formation of blood cells;
- remove metabolic products from the body.
Each kidney consists of many nephrons - these are special filtration particles. Each of the nephrons consists of a ball of small blood vessels; they are semi-permeable, so metabolic products pass through them, like through a membrane. Well-filtered metabolic products are excreted along with urine.
If toxic substances enter the body, then the entire load falls on the nephrons, which begin to cope poorly with their function. The clinical picture directly depends on what toxic substance has entered the body.
The causes of toxic nephropathy include the following factors:
- poisoning from low-quality alcohol-containing drinks;
- heavy metal poisoning;
- ingestion of various solvents into the body;
- intoxication caused by pesticides;
- overdose of medications, as well as treatment with expired or low-quality medications.
If kidney nutrition is insufficient, ischemia may develop, which is considered a reversible condition . If ischemia is not treated for a long time, necrosis occurs, which is already an irreversible pathology. This condition is characterized by complete dysfunction of the kidneys, due to which toxic substances accumulate in the body, and they are not eliminated naturally.
Toxic nephropathy requires urgent treatment, otherwise life-threatening complications may occur.
Symptoms
The severity of the lesion and the severity of symptoms largely depend on the type of substance that affects the human body. In addition, its quantity matters.
Not the least place is given to the state of the urinary system before the development of toxic nephropathy.
If the patient had chronic kidney pathologies, toxic nephropathy can develop even from small doses of toxic substances.
Manifestations of a toxic kidney resemble the course of glomerulonephritis in acute form. Initially, the patient experiences symptoms such as fever, lethargy, weakness and a feeling of weakness.
Afterwards, the patient may notice swelling of the lower extremities and puffiness of the face. When examining urine, the appearance of protein and red blood cells is noted.
With a pathology such as toxic nephropathy, symptoms may be as follows:
- pain in the lumbar region;
- lowering blood pressure;
- reduction in the volume of urine excreted;
- breathing disorders.
If a toxic kidney is caused by toxic substances entering the body through the gastrointestinal tract, the accompanying symptoms of the disease may be as follows:
- attacks of nausea and vomiting with blood;
- bloating and pain;
- upset stomach;
- increased drowsiness and fainting, other brain disorders.
In each individual case, the signs of toxic kidney damage may vary depending on the nature of the poisoning and its severity. Sometimes disorders of the nervous system, hallucinations and severe psychosis may occur.
Toxic kidney: symptoms and signs
The general symptoms of toxic kidney poisoning with various poisons are divided into several phases, and the signs of pathology will depend specifically on the phase.
The general symptoms of toxic kidney poisoning with various poisons are divided into several phases, and the signs of pathology will depend specifically on the phase.
- Thus, during the initial phase of renal failure, the patient will experience a decrease in the volume of urine excreted. This phase lasts from 1 to 3 days depending on the degree of poisoning.
- During the oligoanuric phase, the patient may develop fluid retention in the body, which will lead to a general overload of the left cardiac ventricle. The patient may also develop wet lung syndrome, which is characterized by wheezing and shortness of breath. During this phase, the patient is likely to develop cerebral and pulmonary edema. There is an intensive accumulation of toxins (products of protein metabolism) in the body. Possible consequences in the form of lethargy and weakness. Possible cardiac arrest. This phase lasts 7-14 days.
- Polyuric phase. If the treatment is prescribed correctly, and the patient’s body provides adequate resistance to the pathology, then the previous phase will turn into polyuric. In this case, the total volume of urine will increase day by day. In extreme cases, the daily volume of urine can reach 35 liters per day. In this case, the urine will have a low specific gravity. You should be careful here, since this phase can lead the patient to dehydration. The phase lasts 15-30 days.
- Then comes a period of recovery, during which the specific gravity of urine and its daily volume are normalized. The recovery phase can last 6-24 months.
Important: the range of deaths from toxic kidney poisoning ranges from 20% to 70%, and completely depends on the causes of poisoning and the complexity of the pathology. If the kidney damage was not critical, then the patient has every chance of a full recovery.
In general, at home, toxic poisoning in the early stages may have the following morphological signs:
- Nagging pain in the lower back;
- Swelling of the legs and face;
- Constant thirst;
- Some yellowness of the skin and its dryness;
- A rash may appear on the inside of the palms;
- Nausea, diarrhea, vomiting;
- Muscle and headache;
- A sharp drop in blood pressure in a patient;
- Decreased urine volume;
- Lethargy, lethargy, hallucinations.
Important: if the patient suspects toxic poisoning (animal/insect bites, inhalation of poisons or tactile contact with them, consumption of toxins), then if the above symptoms appear, you should immediately contact a medical facility. Timely assistance will help protect the patient from acute renal failure.
Complications and consequences
After nephrotic syndrome, the patient develops acute renal failure. In addition, other complications may occur:
- hemolytic anemia;
- bacterial damage to kidney tissue;
- thrombocytopenia.
Impaired kidney function can cause death due to functional uremia, so when the first signs of the disease appear, you should consult a doctor as soon as possible.
The cause of this condition is complete dysfunction of the nephrons and cessation of organ function.
Symptoms of functional uremia are a decrease in the amount of fluid secreted, disturbances in the functioning of the central nervous system and dehydration.
When the kidneys fail, severe poisoning of the body with metabolic products occurs, which becomes the cause of death.
Consequences of toxic nephropathy
Any nephrotoxic effect can cause kidney damage, of which the most severe ones should be distinguished:
- Acute renal failure - manifested by a sharp decrease or complete cessation of urination.
- Chronic renal failure - arising as a result of an acute condition or as a result of moderate poisoning.
Toxic nephropathy is almost always an accidental or unintentional ingestion of toxic or harmful substances into the body. Renal complications in severe diseases and drug-induced nephropathy are much less common.
Diagnostics
If acute kidney damage is suspected, the patient is admitted to a hospital, where general diagnostic tests are performed. The specialist pays attention to the clinical picture of the disease, the patient’s medical history and clarifies the possible nature of the poisoning.
For toxic nephropathy, the following examination methods are used:
- general blood and urine tests;
- Ultrasound of the kidneys;
- biochemical blood test;
- Kidney MRI.
With nephrotic syndrome, an increase in ESR and leukocytes in the blood is most often observed, and anemia is also noted. An increased concentration of protein and nitrogenous compounds is detected in the urine, hemoglobin, red blood cells and casts appear.
First aid
If the patient experiences loss of consciousness and cardiac arrest, it is necessary to perform artificial respiration and chest compressions
- If toxic poisoning is suspected, the patient should be provided with pre-medical care as soon as possible. In this case, it is necessary to stop the entry of toxins into the patient’s body. That is, if poisons enter the body through the air, then you need to provide the patient with fresh air (move him outside, further from the source of infection); if poisons enter the body through the mouth, then you need to rinse the stomach with plain water. A simple water enema is also recommended here. Activated carbon can be given to the patient as a sorbent.
- If the patient experiences loss of consciousness and cardiac arrest, it is necessary to perform artificial respiration and chest compressions. Before carrying out all activities, you should call an ambulance.
Treatment methods
Toxic damage to both kidneys is considered a very dangerous condition that requires urgent treatment. At the first signs of pathology, you should consult a doctor as soon as possible and under no circumstances self-medicate.
The choice of treatment method depends on the severity of the lesion and the individual characteristics of the patient’s body.
Treatment of a toxic kidney is often carried out in the intensive care unit, especially if the patient is diagnosed with kidney failure. With a milder form of the pathology, the patient is placed in the urology department.
First of all, measures are taken to remove toxins from the body, as well as to cleanse the blood. To do this they resort to:
- plasmapheresis;
- hemofiltration;
- hemodialysis;
- hemosorption;
- washing the gastrointestinal tract.
Forced diuresis is carried out using diuretics. To lavage the stomach, Vaseline oil or a large amount of liquid is administered.
Hemodialysis should be carried out within the first few hours after poisoning, and then blood purification through the peritoneum is carried out for two days.
For nephropathy, medications from the group of sorbents, glucocorticosteroids and diuretics may be prescribed.
In addition, the patient is prescribed an alkaline drink, which is supplemented by the administration of glucose with vitamin C, insulin, calcium chloride and vitamins.
Toxic nephropathy is difficult to treat due to poor recovery of renal tissue. Even if all the necessary measures are taken, already in the early stages of the development of pathology, nephron death is possible, which leads to disruption of the organ.
It is for this reason that it is important to begin treatment at an early stage of the development of nephropathy.
Features of therapy
Treatment of nephropathy is carried out in a hospital. If a patient arrives in serious condition, he is kept in intensive care. The first stage of stabilizing the patient’s condition is removing the toxin from the body. If the cause is an autoimmune reaction, then corticosteroids are used to reduce the manifestations of allergies. Doctors carry out the following activities:
- blood purification through special filters;
- administration of antishock drugs;
- gastric lavage (if the toxin came with food);
- connecting the patient to a device that acts as an artificial kidney;
- accelerating diuresis by administering diuretics to the patient.
The patient is given diuretics, alkaline drinks, and sorbents. During your stay in the hospital, you must adhere to bed rest. Foods with a lot of protein should be removed from the diet. If uremia is severe, the patient is transferred to a carbohydrate diet. If the excretory function of the kidneys is not affected, the patient is prescribed plenty of fluids.
Doctors monitor the condition of the skin, as toxic products can come out through it. As a result, patients experience severe itching. To avoid this, it is recommended to shower or rub down at least once a day. During vomiting, patients are given salty foods to reduce sodium chloride loss.
Toxic poisoning in children
When children develop a disease such as infectious-toxic nephropathy, the composition of urine first changes.
A child’s predisposition to the development of this pathology is associated with hereditary kidney diseases or congenital anomalies of the genitourinary system.
The likelihood of nephrotic syndrome increases in situations where such disorders were observed in the mother of the child or worsened during pregnancy.
The risk of kidney disease increases in children who are bottle-fed or who suffer from frequent colds and infectious diseases.
Emergency medicine
Toxic nephropathy is one of the most common pathological syndromes in acute exogenous poisoning.
The exotoxic nature of nephropathy is currently observed in 18-20% of patients with acute renal failure (ARF) treated in modern “kidney centers”. In this case, two main types of exotoxic kidney damage are usually found: specific, reflecting the direct damaging effect of a number of nephrotropic chemicals on the renal epithelium, and nonspecific, constituting the general pathology of the kidney response to “chemical injury”.
Specific kidney damage occurs primarily in acute poisoning with nephrotoxic substances, which, during their “active transport,” cause destruction of the excretory epithelium of the tubules with the development of the general pathomorphological picture of “excretory necronephrosis.” Despite the differences in the intimate mechanism of action of nephrotoxic substances, the overall result is the same: the preferential accumulation of these compounds in the kidneys leads to severe disorders of enzymatic metabolic functions and a decrease in oxygen consumption in them.
When the body is exposed to hemolytic substances in the kidneys, the pathomorphological picture of acute hemoglobinuric nephrosis develops. Pathomorphological data reflect the renal transport of free hemoglobin under conditions of intravascular hemolysis and exotoxic shock.
Free plasma hemoglobin and protein products of tissue destruction absorbed in the area of a chemical burn acquire the character of a foreign protein, causing a corresponding immunological reaction of the body. This reaction is manifested by spasm of the renal vessels, decreased diuresis, increased body temperature and other signs of so-called endogenous toxicosis in shock of toxic etiology.
A large place in the pathogenesis of toxic nephropathy in acute poisoning is occupied by “myorenal syndrome”, which is a peculiar type of the well-known long-term muscle crush syndrome (Crush-syndrome). This syndrome develops as a result of the combined effect on the body of various factors, the most influential of which are acute poisoning with certain toxic substances of narcotic action (carbon monoxide, alcohol and its surrogates, hypnotics, etc.) and prolonged compression of soft tissues, most often the muscles of the extremities. Patients are usually unconscious and lie on a hard surface, usually on their side, sometimes in a half-sitting position, with their limbs tucked in. “Myorenal syndrome” may be preceded by coma, exotoxic shock, disturbances in external respiration, and cooling.
Pathomorphological examination reveals the phenomena of ischemic coagulative muscle necrosis (“rhabdomyolysis”) in areas of local positional compression, where sharp swelling and thickening of muscle tissue develop, which looks like fish meat on the cut. In the kidneys, a picture of acute pigmentary nephrosis is noted, the characteristic feature of which is the presence of myoglobin in the lumen of the nephron and in the epithelium of the convoluted tubules. Myoglobin enters the blood from necrotic areas of the affected muscles.
In the pathogenesis of “myorenal syndrome”, great importance is attached to prolonged spasm of the vessels of the renal cortex and the development of shunted juxtamedullary circulation. It is impossible to exclude a noticeable influence of the phenomena of diffuse intravascular coagulation developing in the kidneys under the influence of thromboplastic factors formed as a result of myolysis, as well as ischemic toxin, which manifests its effect as a tourniquet shock.
In the pathogenesis of toxic kidney damage in acute poisoning with hepatotoxic substances (CC14, fungal toxins, etc.), the nephrotoxic effect of certain amino acids (leucine, tyrosine, etc.), which are normally deaminated by the liver, and in case of massive damage its parenchyma in large quantities will degenerate into kidneys. Pathomorphological data for this pathology are quite similar and present a picture of diffuse cholemic nephrosis. Signs of necronephrosis are usually not observed.
Nonspecific kidney damage of exotoxic etiology can cause toxic nephropathy in cases of acute poisoning with almost any toxic substance with a particularly unfavorable combination of various homeostasis disorders in the body, namely: a sharp decrease in blood pressure with impaired regional blood circulation in the kidneys and liver, disorders of water and electrolyte balance during severe dyspeptic symptoms, prolonged uncompensated acidosis, the presence of chronic kidney diseases (chronic nephritis, nephrosclerosis, etc.).
The clinical characteristics of toxic nephropathy suggest the need for a summary assessment of the main clinical and laboratory indicators of the functional state of the kidneys. The actual clinical symptoms of toxic kidney damage in the toxigenic phase of acute poisoning include a sharp decrease in daily diuresis, pain in the lumbar region associated with increasing interstitial edema of the kidneys, and the appearance of peripheral edema (facial puffiness). The most striking clinical picture of toxic nephropathy is usually found in the somatogenic phase with the development of acute renal failure.
The main attention in the early diagnosis of toxic nephropathy is paid to the “urinary syndrome” with careful measurement of diuresis, taking into account the patient’s infusion therapy and possible extrarenal fluid loss. It is believed that a decrease in diuresis to 500 ml per day (20 ml/h, 0.35 ml/min) indicates the development of oliguria, and up to 100 ml per day (4-5 ml/h, 0.07 ml/min) - anuria.
One of the simplest indicators of the concentrating ability of the kidneys is urine density, which increases significantly with glucosuria and proteinuria. At the same time, 1% glucose increases this indicator by 0.0037, and 1% protein - by 0.0026. The highest figures for urine density (up to 1024-1052) and proteinuria (up to 330%) are observed with toxic nephropathy caused by the action of hemolytic substances, such as vinegar essence, and are a poor prognostic sign. The degree of proteinuria usually corresponds to the degree of hemoglobinuria. A reliable test of the functional state of the kidneys is azotemia, as well as the urea concentration index (the ratio of the concentration of urea in urine to urea in blood). A decrease in this index to 10 or below indicates severe renal dysfunction.
Modern methods of studying the functional state of the kidneys include measuring the osmotic pressure of plasma and urine using the cryoscopic method, studying the relationship between the electrolyte composition of blood plasma and urine, acid-base balance, measuring glomerular filtration and tubular reabsorption using the Rehberg-Tareev test, measuring renal plasma flow using the Smith method, toxicological studies to determine clearance of toxic substances, quantitative calorimetric determination of free hemoglobin in blood plasma and urine, as well as methods of radioisotope diagnosis of renal dysfunction.
Three degrees of severity of toxic nephropathy have been identified. Mild toxic nephropathy, which occurs in approximately 25% of cases of development of renal dysfunction in various poisonings, is manifested by moderate and rapidly passing (1-2 weeks) changes in the composition of urine, a slight decrease in glomerular filtration (76.6 ± 2.7 ml/ min) and renal plasma flow (582.2Hz 13.6 ml/min) with preserved concentration and nitrogen excretory function of the kidneys.
Moderate toxic nephropathy, which occurs in approximately 57% of cases of this pathology, is manifested by more pronounced and persistent changes in the qualitative and morphological composition of urine (up to 2-3 weeks) and is accompanied by a noticeable decrease in glomerular filtration (60.7 ± 2.8 ml/min ), tubular reabsorption (98.2+0.1%) and renal plasma flow (468.7±20.2 ml/min).
Severe toxic nephropathy is characterized by acute renal failure syndrome, which is observed in approximately 10% of cases of this pathology, with pronounced symptoms of oliguria, azotemia, creatininemia, a sharp decrease in glomerular filtration (22.8±4.8 ml/min), inhibition of reabsorption (88, 9±1.8%), a significant decrease in renal plasma flow (131.6±14.4 ml/min).
Acute renal failure in acute poisoning is characterized by a severe clinical course as a result of concomitant damage to the liver (toxic hepatopathy - 82% of cases) and lungs (toxic pneumonia - 36.6% of cases), which causes high mortality, reaching 50%.
It should be taken into account that in case of acute poisoning in the group of severe patients with toxic nephropathy and hepatopathy, renal-liver failure syndrome (RLFS) is usually observed.
As a result of combined damage to the liver and kidneys, the mutually compensating influence of the functions of these organs is excluded. Moreover, the nephrotoxic effect of a number of chemicals that cause toxic hepatopathy and the hepatotoxic effect of chemicals that impair renal function should be recognized. These features make significant changes in the clinical symptoms and dynamics of laboratory data in acute renal failure of exotoxic etiology. In the clinical picture of acute renal failure, it is customary to distinguish 4 main periods:
- 1) the period of initial action of the main etiological factor;
- 2) period of oligoanuria;
- 3) period of diuresis recovery;
- 4) recovery period.
In acute poisoning, the period of initial action of the kidney-damaging factor usually corresponds to the toxicogenic phase of the disease with the clinical symptoms inherent in the action of this toxic substance.
During the period of oligoanuria, which lasts about 2 weeks, a picture of endogenous uremic intoxication develops, which is a consequence of blockade of glomerular filtration with loss of renal cleansing function (renal azotemia) and increased catabolism of proteins in tissues (extrarenal azotemia). However, despite the severe clinical condition of patients, the level of azotemia usually remains moderate (up to 4 g/l), which is explained by a decrease in the formation of urea in the damaged liver. In this period of acute renal failure, disturbances in water-electrolyte metabolism are constantly detected, in which potassium ions leave the cell into the blood, and sodium ions replace them, resulting in the development of hyponatremia and hyperkalemia. This process is explained by the instability of the equilibrium that exists between high intracellular and low intercellular concentrations of potassium, which is maintained due to the expenditure of oxidative energy of cells and poor permeability of cell membranes for K+ ions. In acute poisoning, which is often accompanied by a decrease in redox processes in cells and an increase in the permeability of cell membranes, the loss of intracellular potassium is inevitable. With the phenomena of oligoanuria, which excludes the constant excretion of potassium by the kidneys, hyperkalemia can cause symptoms of potassium intoxication (impaired cardiac activity and neuromuscular conduction) even in the presence of a large deficiency of potassium content in the cells.
The highest degree of hyperkalemia is observed in acute poisoning, causing hemolysis or myolysis with intense release of potassium from damaged cells into the plasma.
During the period of restoration of diuresis or with large losses of potassium through the gastrointestinal tract, hypokalemia occurs, which is usually clinically manifested by nonspecific symptoms of intracellular potassium deficiency - muscle weakness, etc.
The extent of other electrolyte dissociations depends on the level of natural clearance of a given electrolyte. The higher this clearance, the more intense its accumulation during anuria and the more pronounced the deviation of its concentration from the norm.
Despite the fact that in oligoanuria the excretion of all electrolytes is impaired, an increase in plasma concentrations is observed only for some of them. This is due to the development of overhydration of the body in this period of acute renal failure, when the process of water accumulation occurs faster than the process of accumulation of substances with low clearance (sodium, chlorine, calcium), which leads to a decrease in their concentration as a result of dilution. This is confirmed by the fact that in the polyuria phase, when water losses exceed salt losses, the concentration of sodium, chlorine and calcium returns to normal. In addition to the dilution mechanism, one should also take into account the reverse movement of ions from the extracellular space into the cells relative to potassium.
Overhydration of the body in acute renal failure of toxic etiology is caused not only by long anuria, but also by transudation of plasma proteins into the interstitial fluid due to increased capillary permeability, as well as hypoproteinemia due to liver damage. In this case, the osmotic pressure of the plasma quickly drops, edema and swelling of cells occur, which cause severe changes in the brain and lungs with the development of neuropsychiatric disorders and external respiration disorders. The latter are most clearly manifested by the “wet lung” syndrome, which is various stages of increasing interstitial edema of the lung tissue.
These changes in the lungs usually undergo complete reversal when diuresis is restored and overhydration is reduced, but they serve as a favorable basis for the occurrence of pneumonia, the differential diagnosis of which is extremely difficult. A constant companion to acute renal failure of toxic etiology is anemia, which is of an iron deficiency nature and is associated with impaired erythropoiesis. Impaired external respiration and anemia significantly increase tissue hypoxia, which creates unfavorable conditions for the regeneration of the renal epithelium and restoration of renal functions, which are observed no earlier than 30-35 days after the development of severe toxic nephropathy. The restoration of renal function takes a particularly long time in acute poisoning with vinegar essence, when the nitrogen-excreting concentration capacity of the kidneys is completely normalized only by the end of the 6th month after the onset of the disease, and in severe nephropathy caused by ethylene glycol poisoning, such restoration of functions is very rare.
The most common cause of toxic nephropathy is poisoning with vinegar essence, carbon tetrachloride, heavy metal compounds, and alcohol surrogates.
Luzhnikov E. A. Clinical toxicology, 1982
Preventive measures
For preventive purposes, in industries where there is a high risk of poisoning by harmful substances and toxins, people with kidney disease are not allowed to work.
Agricultural work involving the use of pesticides and the production of polymers and rubber are considered especially dangerous.
People whose work involves nephrotoxic substances must undergo a medical examination every year. For safety reasons, it is necessary to comply with hygiene requirements and wear special protective clothing.
Also, to prevent poisoning, you should avoid eating expired products and unknown mushrooms.
When self-medicating, an overdose of drugs is common, which causes the development of toxic nephropathy. It is for this reason that any medication should be taken only after prior consultation with a doctor.