The definition of “diabetic nephropathy” is a collective concept that unites a complex of diseases that result in vascular damage in the kidneys against the background of acute diabetes mellitus.
The term “Kimmelstiel-Wilson syndrome” is often used for this disease, because the concepts of nephropathy and glomerulosclerosis are used as synonymous.
For diabetic nephropathy according to ICD 10, 2 codes are used. Therefore, diabetic nephropathy code according to ICD 10 can have both E.10-14.2 (diabetes mellitus with kidney damage) and N08.3 (glomerular lesions in diabetes). Most often, impaired renal activity is seen in insulin-dependent type 1 - 40-50%, and in type 2 the prevalence of nephropathy is 15-30%.
What is pathology?
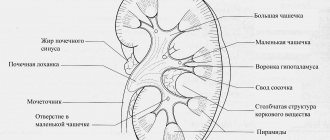
The glomerular apparatus and organ parenchyma are often affected. The main danger of nephropathy is its slow progression. During this period, the disease does not manifest itself at all. At later stages, the signs are more obvious and quite specific. But mainly it depends on the primary pathology that affected the kidneys.
The more advanced the nephropathy, the more the filtration functions of the organ suffer. This leads to an increase in infection with a variety of ailments. A kidney affected by nephropathy can be seen in the photo presentation. The disease develops in people regardless of age and gender.
Note! Many famous scientists have created scientific treatises regarding nephropathy and researched this condition. For example, Bobkov, Shchukin, Shestakov.
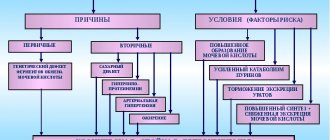
The provoking factors for the appearance are called:
- Pathological conditions of the endocrine system, such as diabetes.
- The influence of nephrotoxins. These include: household and industrial chemicals, poisons, some medications (NSAIDs, analgesics, anticonvulsants). It is worth understanding that contact with such substances and medications does not always produce similar results.
- Metabolic disorders - gout, dysmetabolia.
- Tumors outside the kidneys, in other human organs.
- Exposure to radiation.
- Abnormal development (structure) of the kidneys and urine excretion pathways.
- The period of bearing a child. In this case, the development of such a condition is associated with anemia, glomerulonephritis, pyelonephritis, and gestational hypertension.
Sometimes nephropathy develops in a seemingly absolutely healthy person. This is possible when certain factors influence his body, for example, poisons, strong chemicals. Such exposure can be permanent, but in small doses, or large-scale and one-time. The result is the same – nephropathy.
Diseases contributing to the development of nephropathy
- endocrine diseases (especially diabetes);
- metabolic disorders (metabolic failures);
- tumors located outside the kidneys;
- primary kidney diseases (pyelo- and glomerulonephritis, nephrosis, kidney tumors, anomalies of their structure);
- pathologies during pregnancy.
Damage to the glomeruli and tubules of the kidneys can also occur in a healthy person as a result of external influences of the following nature:
- toxic effects of drugs (antibiotics, painkillers, anti-inflammatory drugs, anticonvulsants);
- alcohol intoxication;
- poisoning by poisons (household or industrial), heavy metals, chemicals;
- exposure to radiation.
Classification
There are many classifications of nephropathy. Basically, the division into types occurs due to the development of the disease, since it is most often secondary. The dysmetabolic form is predominantly found; it has several subtypes, namely:
- Oxalate-calcium. Mostly diagnosed in children.
- Oxalate. It can appear at any age, even immediately after birth. It definitely needs treatment, since the lack of therapy is fraught with the development of urolithiasis.
- Phosphate. Progresses against the background of chronic infections of the genitourinary system.
- Uratnaya. It can be primary and secondary. That is, it can develop against the background of other pathologies of the genitourinary system or independently.
- Exchange.
Other forms: diabetic, gestational, toxic, gouty, myeloma and lga require more detailed consideration.
Diabetic
In this case, simultaneous damage to two kidneys occurs, which naturally leads to disruption of their functionality. The main cause is a primary endocrine disease. It progresses against the background of diabetes mellitus, the manifestation of symptoms occurs smoothly. The clinical picture manifests itself gradually in 5 stages:
- Asymptomatic. There are no symptoms, the pathology is manifested only by the results of tests, which are generally not done because of the detection of kidney pathology.
- Initial structural changes. Blood circulation in the kidneys increases, along with glomerular filtration.
- Prenephrotic. The concentration of microalbumin increases, but there is no pronounced protein concentration in the urine. Blood circulation in the glomeruli is normalized, sometimes an increase in blood pressure is observed, but only slightly. Swelling appears and cholesterol levels rise.
- Nephrotic. There is a constant increase in blood pressure, and protein is found in the urine. Filtration of blood through the organ decreases.
- Uremic. Kidney filtration drops very significantly, as a result urea and creatine accumulate in the blood. Protein levels drop, causing obvious swelling. Blood pressure may increase to critical levels. Almost always, this stage transforms into renal failure. Which, against the background of endocrine pathology, is very dangerous for human life.
Gestational
In pregnant women, this condition is considered a dangerous complication, which can lead to negative consequences for the fetus and develops in varying degrees of severity. At the moment, the causes of the development of nephropathy in pregnant women have not been studied; research is still being conducted. At risk are very young mothers and those who abuse alcohol, smoke, and have other similar bad habits.
This condition develops in the second half of pregnancy, mainly in the third trimester. Among the characteristic features characteristic of this type:
- Significant increase in blood pressure.
- Edema.
- Tests determine protein in urine.
- If the disease is not treated promptly, there is a risk of miscarriage.
Important! Treatment is carried out only in a hospital setting under the close supervision of a doctor.
Today, cases of nephropathy among pregnant women are being discovered more and more often, which is a very dangerous condition.
Three methods of prevention
The most reliable way to prevent the development of nephropathy is acceptable compensation for diabetes mellitus:
- Primary prevention is to prevent microalbuminuria. The main factors for the development of microalbuminuria are: duration of diabetes mellitus from 1 to 5 years, heredity, smoking, retinopathy, hyperlipidemia, as well as the lack of functional renal reserve;
- Secondary prevention involves slowing the progression of the disease in patients who already have either reduced GFR or higher than normal urinary albumin levels. This stage of prevention includes: a low-protein diet, blood pressure control, stabilization of the lipid profile in the blood, glycemic control and normalization of intrarenal hemodynamics;
- tertiary prevention is carried out at the stage of proteinuria. The main goal of the stage is to minimize the risk of progression of acute renal failure, which, in turn, is characterized by: arterial hypertension, insufficient compensation of carbohydrate metabolism, high proteinuria and hyperlipidemia.
Characteristic symptoms of nephropathy
Early nephropathy does not reveal itself in any way, which actually explains the difficulty of diagnosing it at first. Also, the symptoms depend on the disease that provoked this condition, if the pathology is secondary. As it develops, the following manifestations are possible:
- Feeling thirsty.
- General weakness.
- Increased fatigue.
- Headache.
- Pain in the kidneys and their projection sites.
- Periodic pain in the lumbar region. Their character is dull and whining.
- Frequent urination.
In later stages, as it progresses, the following occurrences are possible:
- Swelling throughout the body, they are more pronounced in the lower part of the body. Another characteristic appearance is that swelling appears in the morning and does not increase in the evening.
- Increased pressure.
- Protein in the urine, which is diagnosed during testing.
- It is likely that nephropathy will manifest itself with signs of pyelonephritis if an infectious agent has entered the body.
How is it diagnosed?
To determine nephropathy, the patient's medical history and laboratory tests are used. The main method at the preclinical stage is to determine the level of albumin in urine.
To diagnose diabetic nephropathy according to ICD 10, the following methods can be used:
- determination of GFR using the Rehberg test.
- kidney biopsy.
- Dopplerography of the kidneys and peripheral vessels (ultrasound).
In addition, ophthalmoscopy will help determine the nature and stage of retinopathy, and an electrocardiogram will help identify left ventricular hypertrophy.
Traditional treatment
Treatment is prescribed by a doctor depending on the genesis of the disease. At the stage of preclinical studies, the need for inpatient treatment is determined. Thus, in the clinic it is necessary to carry out therapy for toxic forms, including drug-induced nephropathy. Metabolic forms can be treated on an outpatient basis.
The diabetic form requires special attention; the morphology of its therapy is specific. It is necessary not only to use certain medications to treat nephropathy, but also to control the concentration of sugar in the blood. This is necessary regardless of the flow form, c1a1 or others. In some cases, hemodialysis (infusion of purified blood plasma) will be required; it is important to follow a specific menu.
Important! The cost of treatment in this case is not the most important thing, since the consequences will be much more serious if you refuse or do not carry out therapy in a timely manner.
Nephropathy in pregnant women requires mandatory hospitalization. Groups of drugs used:
- Products with a high protein content.
- Diuretics.
- Antiplatelet agents.
- Antispasmodics.
- Calcium preparations.
- Antihypertensive drugs.
The woman is prescribed bed rest.
Principles of treatment of dysmetabolic form:
- Normalization of lifestyle.
- Diet food.
- Medicines as recommended by a doctor. Sample list: vitamins E, A, B6, dimefosone and other means.
Therapy for gouty form includes:
- Drinking enough liquid, which helps remove excess impurities.
- Diuretics.
- Antihypertensive drugs.
- In case of infection, antibiotics are used.
Arterial hypertension (ICD-10 code: I10)
It is characterized by a persistent increase in blood pressure above the limits of the physiological norm (140/90 mm Hg) in persons not receiving antihypertensive therapy. Isolated systolic hypertension is defined as a persistent increase in systolic pressure above 140 mmHg. Art. at normal diastolic pressure.
Essential arterial hypertension accounts for 92-95% of all cases of chronic high blood pressure and is the result of neurosis of the centers regulating blood pressure, which ultimately leads to increased muscle tone of the arterial wall, narrowing of the lumen of small arteries and arterioles and increased blood pressure.
Secondary mechanisms involved in the increase in blood pressure include renal ischemic and endocrine factors. Currently, there are several types of classification of arterial hypertension. The classification of the Joint National Committee of the European Society on Hypertension (JNC-7-2003) is quite convenient.
Traditional medicine against nephropathy
Folk remedies can be used during the recovery stage or in parallel with drug therapy. Moreover, if the doctor gave the go-ahead. Everything is explained simply - this is a disease that can have serious consequences if treated incorrectly or incompletely.
If approved, herbal infusions can:
- Improve metabolic processes.
- Boost immunity.
- Strengthen your overall health.
Important! Women should not resort to such methods during pregnancy; negative consequences may occur.
Possible treatment options:
- Lingonberries have a positive effect on the urinary system and immunity in general. For treatment, you need to prepare the following remedy: mix berries with sugar in a ratio of 1 to 1 and keep in a cold place for several weeks. After this, make a compote from it, consume it three times a day.
- Herbal collection with the following components: coltsfoot, nettle, St. John's wort, yarrow. In equal proportions of each component. Their dried ones are crushed and mixed thoroughly. Next 2 tbsp. Brew l of the collection in boiling water and let it brew for a couple of hours. Drink 2 times a day. The course of treatment is 25 days.
- The skin of watermelon helps with swelling; you need to boil it and take the decoction orally.
- A decoction of bearberry will help relieve acute symptoms. Infuse 1 tbsp. l plants per 200 ml of boiling water. Drink 1/3 glass after meals.
There are a lot of traditional treatment methods, but any of them should be agreed with your doctor.
Diagnostics
To determine the presence/absence of the disease, it is necessary to conduct specific examinations. The main ones include:
- Blood test to check cholesterol levels;
- Examination of urine for the presence of protein;
- Urinalysis using the Rehberg method (checking kidney function).
Sometimes making a diagnosis is difficult for some reason, so the doctor may prescribe additional tests, for example, x-rays of the vascular system, 24-hour blood pressure monitoring, etc.
To test urine using the Rehberg method, you also need to take blood to compare the creatinine level in urine and blood
Nephropathy in children
Often this condition is diagnosed in children by chance, since the symptoms are not very pronounced. Unlike adults, a child cannot always tell what exactly and where it hurts. In order to exclude such dangerous manifestations, you should pay attention to the transparency of the urine, the presence of sediment and indelible deposits at the bottom of the pot.
Certain appearances may be present from birth. At the same time, it can be suspected based on the medical history of relatives. In addition to characteristic adult signs, a child may exhibit:
- Allergic reactions.
- Reducing pressure.
- VSD syndrome.
- Rapid weight gain.
- Joint pain.
Treatment in children is associated with the following therapeutic effects:
- Diet. It depends on the type of crystalline clusters formed. The main task is not to provoke an increase in their number in the body.
- Normalization of metabolic processes. For this purpose, membrane-impacting medications and antioxidants are used.
- Controlling the amount of water consumed per day. A sufficient amount helps reduce the salt concentration in the urine.
Important! This complex technique helps to have a gentle effect on the child’s body and prevent functional disorders.
Nephrogenic arterial hypertension ICD-10: I12, I13, I15 General.
Nephrogenic arterial hypertension
ICD-10: I12, I13, I15
general information
Nephrogenic (symptomatic) arterial hypertension (AH) is a persistent increase in blood pressure that occurs against the background of congenital, inflammatory or metabolic damage to the kidneys.
Epidemiology
According to various authors, nephrogenic hypertension accounts for 16 to 24% of the number of people suffering from arterial hypertension (Wong J. 2005, Nerset J. 2007). This percentage variation is explained by different approaches to assessing the etiology of hypertension in patients with chronic kidney disease (CKD).
Etiology
Based on the origin of nephrogenic hypertension, there are 5 groups of causes: congenital kidney diseases, inflammatory (immune-dependent and immune-independent) kidney lesions, non-inflammatory kidney diseases (metabolic nephropathy), kidney damage as a result of other diseases and drug-induced interstitial kidney damage.
— Congenital kidney diseases: polycystic kidney disease, changes in the number of kidneys (single kidney, multiple kidneys), renal vascular dysplasia (both extra- and intraorgan).
— Inflammatory kidney damage: acute and chronic pyelonephritis, acute and chronic glomerulonephritis, kidney damage against the background of other immunocompetent pathology (systemic lupus erythematosus, periarteritis nodosa, scleroderma, etc.).
- Non-inflammatory kidney diseases: diabetic nephropathy, gouty nephropathy, renal amyloidosis.
— Kidney damage as a result of other diseases: kidney damage due to circulatory failure, kidney damage due to bronchopulmonary diseases, kidney damage due to multiple myeloma, etc.
— Drug-induced interstitial kidney damage.
Pathogenesis
The main reason for the start of the mechanisms of arterial hypertension formation is ischemia of the juxtaglomerular apparatus (JH apparatus) due to either immunocompetent or non-immune inflammation, or “thickening” of the vascular walls and/or paravascular tissues due to the deposition of metabolic products or perverted synthesis.
In response to ischemia of the JH apparatus, the Tobian mechanism is activated - increased secretion of renin in response to constriction of the renal arterioles, as well as an increase in the activity of the JH apparatus as a result of activation of the macula densa due to the activation of aldosterone synthesis with the formation of a “vicious” circle of persistent JH ischemia. apparatus.
Activation of the renal tissue renin-angiotensin-aldosterone system (RAAS) due to ischemia of the juxtaglomerular complex leads to activation of the ACE-dependent pathway for the formation of angiotensin II and activation of the ACE-independent (chymase) pathway for the formation of angiotensin II due to the prevalence of the latter.
In parallel with the activation of the pressor system for regulating vascular tone, the activity of the depressor system decreases due to a decrease in the synthesis of kinins (primarily bradykinin) as nephrogenic hypertension progresses. In addition, increased degradation of bradykinin occurs due to the high formation of chymases, which are the most powerful kininases.
Unlike essential hypertension, the circulation of adrenaline and norepinephrine in nephrogenic hypertension is normal or reduced, including a decrease in the capacity of adrenaline depots. Significant activation of the sympathoadrenal system is observed only during hypertensive crises. In addition to the main mechanisms mentioned above, other pathogenetic causes also play an important role in the formation of nephrogenic hypertension. Thus, there is a decrease in the concentration of nitric oxide in patients with nephrogenic hypertension, the formation of a nitric oxide depot in the form of nitrosothiols and the activation of lipid peroxidation, free radical oxidation, etc. In addition, the formation of “prostaglandin scissors” has been established - an increase in the content of pressor prostaglandins and a decrease in the content of depressor prostaglandins in patients nephrogenic hypertension.
ICD-10 code
I 12.0 Hypertension with predominant kidney damage and renal failure.
I 12.9 Hypertension with predominant kidney damage without renal failure.
I 13.0 Hypertension with predominant damage to the heart and kidneys with congestive heart failure.
I 13.1 Hypertension with predominant damage to the heart and kidneys with renal failure.
I 13.2 Hypertension with predominant damage to the heart and kidneys with congestive heart and renal failure.
I 13.9 Hypertension with predominant damage to the heart and kidneys, unspecified.
I 15.0 Renovascular hypertension.
I 15.1 Hypertension is secondary to other renal lesions.
Diagnostics
The occurrence of hypertension against the background of kidney disease: primary kidney damage with documented changes in urine tests (proteinuria, leukocyturia, erythrocyturia), blood (anemia, increased levels of creatinine, urea, etc.).
Development and main manifestations: as a rule, a gradual increase in blood pressure (BP), rarely a crisis course, and a high level of BP is rarely felt by patients.
Possible manifestations: swelling; gross hematuria or hemoglobinuria; abdominal syndrome; lower back pain; disturbances in the urinary process; arthralgia.
Laboratory diagnostics
— Clinical blood test (weekly – 1 month, then quarterly, annually);
— biochemical blood test: proteinogram, cholesterol, creatinine, urea levels (2 times/month, then quarterly, annually);
— angiography of renal vessels (once and if necessary);
- 24-hour blood pressure monitoring.
Paraclinical criteria
— Urinalysis - proteinuria, changes in the specific gravity of urine, hypersthenuria with severe proteinuria, hyposthenuria with impaired renal function, cylindruria, possible abacterial/bacterial leukocyturia, possible micro-gross hematuria;
— clinical blood test - increased ESR, possible moderate leukocytosis, possible shifts in the leukocyte formula to the left; biochemical – increase in alpha-2-globulins, hypercholesterolemia, increase in B-lipoproteins, low-density lipoproteins, decrease in high-density lipoproteins, increase in total lipids, hypercoagulation;
Features of nephropathy during pregnancy
Late toxicosis, which is one of the provocateurs for the appearance of protein in the urine, swelling, and increased blood pressure, characterizes nephropathy during pregnancy. Symptoms can be detected with all the signs at once, or be mixed - 1-2 manifestations.
There are a number of factors that contribute to the development of this condition in the later stages of pregnancy, among them:
- Excessive accumulation of breakdown products in the placenta.
- Hormone imbalance associated with the restructuring of a pregnant woman’s body to new living conditions.
- Immunological incompatibility between the fetus and the woman’s body.
Nephropathy in pregnant women, what is it?
In the second half of pregnancy, with nephropathy, a woman experiences swelling, increased blood pressure, and proteinuria. This pathology is very dangerous for pregnancy and there is a high risk of miscarriage.
A pregnant woman should be in a hospital under the watchful supervision of doctors. Adequate treatment for nephropathy is selected for her in order to maintain the pregnancy. Cases of diagnosing nephropathy during pregnancy have recently become more frequent. Young women who smoke and regularly drink alcoholic beverages are at risk.
You can stay at home if the swelling is minor. To reduce swelling and help the kidneys, it is recommended to follow a gentle regimen: rest more (lying down reduces the load on the kidneys), do not lift heavy objects.
Diet for kidney nephropathy is very important: you need to add less salt to your food, limit sweets, pasta, rice, and steam it. It is advisable to reduce fluid intake to 800 ml per day and follow other doctor’s recommendations.
Nutritional Features
Particular attention should be paid to nutrition during and after therapy. The peculiarity is that a lot of protein comes out in the urine during nephritis. And this does not have the best effect on the body, because the kidneys cannot function fully. There is an accumulation of fluid in the body. Basic principles of nutrition:
- Increasing the number of foods containing protein.
- Reducing fatty foods in the diet. Moreover, 40% of fats should be of vegetable origin.
- Normalization of lipid metabolism due to lipotropic substances.
Products and dishes that are recommended to be consumed:
- Dietary bread without salt.
- Vegetable, cereal, fruit soups without meat.
- Only lean meat is allowed. Such as: veal, beef, lean pork. It needs to be steamed or baked.
- Fish is also low-fat. It is baked or steamed.
- Vegetables - potatoes, zucchini, carrots, pumpkin, cauliflower, beets, green peas.
- Any fruits and berries.
- Drinks: compotes, fruit juices, herbal infusions.
Dietary restrictions:
- Salt – its consumption should be reduced, or better yet eliminated altogether.
- Reduce consumption of sweets and other foods containing simple carbohydrates.
- Remove all canned food, spices, spicy dishes, marinades, and smoked foods from the menu.
Causes and pathogenesis
Kidney damage can occur due to the pathogenic influence of the toxic substances themselves, their breakdown products, on their tissues, as well as against the background of the development of an autoimmune reaction.
Most often, the disease is caused by the following substances:
- Heavy metals, their salts;
- Ethylene glycol;
- Oxalic, acetic acid;
- Pesticides, herbicides;
- Arsenic;
- Solvents;
- Copper sulfate;
- Poisons of animals, insects;
- Mushroom toxins;
- Nitrogen-containing compounds;
- Volatile esters;
- Poor quality alcohol.
Toxic nephropathy is often recorded in people employed in hazardous industries, where work involves poisons, chemicals, rubber, and polymers. All substances can enter the body through the respiratory system, through the blood, through the skin (through bites).
Sometimes toxic nephropathy is caused even by certain medications - antibiotics, NSAIDs. Nonspecific kidney damage is possible with myoglobinuria, exotoxic shock, severe disturbances of renal trophism during coma, and compression of organs.
After exposure of the kidneys to toxins and metabolites, swelling of the parenchyma cells is observed, as well as disruption of the renal glomeruli, which causes disruptions in cellular respiration and leads to the precipitation of protein fractions. If the body is exposed to hemotoxic poisons, they simultaneously destroy red blood cells, as a result of which hemoglobin clogs the structural units of the kidneys - nephrons. In some cases, kidney damage occurs against the background of their inhibition by free amino acids. Whatever the pathogenesis, ultimately, oxygen starvation of the kidney tissue occurs, its ischemia, which without treatment leads to necrosis of the tubules and glomeruli.