Factors provoking pathology
Prerenal acute renal failure occurs when the patient has serious problems with the cardiovascular system. Doctors can detect anemia, cardiogenic shock, and diagnose heart failure.
This condition is often observed in those who have had low blood pressure for a long time, with the upper level being below eighty millimeters of mercury.
Prerenal acute renal failure can be triggered by reasons such as a general decrease in blood volume, which occurs with severe vomiting, diarrhea, and blood loss.
Myocardial infarction can also cause acute renal failure. In anaphylactic shock, a sharp decrease in vascular tone is observed.
Acute renal failure of the renal form is provoked due to serious intoxication of the body caused by the consumption of mushrooms and the ingestion of heavy metal salts.
This problem is also typical for those who are addicted to the process of self-medication, as a result of which they take an excessively unjustifiably large number of medications. Most often, such drugs include antibiotics, drugs aimed at treating a malignant tumor, as well as sulfonamides.
Acute renal failure can be caused by improper diagnostic testing, when the body receives a deliberately high dose of a contrast agent. This can happen if the patient himself concealed the fact of undergoing such an x-ray. In other cases, this can only act as a medical error.
If the patient has recently undergone a blood transfusion, as a result of which he was given incompatible blood, a situation arises accompanied by a sharp increase in hemoglobin. It also provokes acute renal failure.
The cause of renal failure may be prolonged tissue compression.
Pyelonephritis and glomerulonephritis are also common culprits, as a result of which the patient is diagnosed with acute renal failure.
The causes of postrenal acute renal failure are obstruction of the urinary tract with concomitant pathology such as urolithiasis. Tumors and urethritis are also provocateurs of postrenal renal failure.
Treatment
Indications for hospitalization in a specialized department:
- AKI requiring intensive care with rapid deterioration of renal function
- The need for hemodialysis
- For uncontrolled hypertension and multiple organ failure, hospitalization in the ARC is indicated.
Prerenal acute renal failure
Normalization of general blood circulation. Treatment of prerenal acute renal failure and renal acute renal failure are fundamentally different from each other in the amount of infusion therapy. In case of circulatory failure, intensive restoration of fluid volume in the vessels is often necessary; in case of renal acute renal failure, intensive infusion is contraindicated, as it can lead to edema of the lungs and brain. Reduce hypovolemia and dehydration.
Postrenal acute renal failure
Normalization of urine outflow through the urinary tract (bladder catheterization, surgery on the urinary tract, epicystostomy).
Parenchymal acute renal failure
Restriction of fluid, sodium, potassium, phosphates.
- anuric stage
: agents that increase blood flow and energy exchange in the kidneys: dopamine 3-4 mcg/kg/min - no-shpa, papaverine
- aminophylline 5 mcg/kg/day
- glucose 20% with insulin
- furosemide
:
- infusion therapy - zero water balance. In the polyuric stage, the infusion can reach 5-6 l/day.
:
Indications for emergency hemodialysis
- Hyperkalemia (potassium g above 7mmol/l) due to the threat of cardiac arrest
- Hypervolemia threatening pulmonary or cerebral edema.
Clinical manifestations
Symptoms of acute renal failure differ at different stages of the disease. Urologists distinguish four such stages.
The initial stage is characterized only by those symptoms that provoked acute kidney failure. Symptoms characteristic of acute renal failure are still absent at the first stage.
The oligoanuric (second) stage is accompanied by signs characteristic of the pathogenesis of acute renal failure, manifested as a significant decrease in the daily volume of urinary fluid. At this stage, metabolic breakdown products are already beginning to concentrate in the patient’s blood; nitrogen compounds are concentrated to a greater extent.
Due to the fact that the kidney organ experiences a serious functional failure, acid-base and water-electrolyte imbalance is provoked in the body. Metabolic acidosis occurs due to acidification of the blood.
A little later, characteristic pathological signs appear in the form of frequent attacks of nausea, followed by vomiting, loss of appetite, swelling, headache, and drowsiness. There is a risk of coma.
In the third stage of acute renal failure, the pathogenesis demonstrates a clear increase in the volume of urine excreted, reaching two liters per day. This fact may please the patient somewhat, since it indicates that the functioning of the glomeruli of the kidneys has been restored, only the tubular epithelium has been affected.
Doctors consider decreased urine density, the content of protein and red blood cells as characteristic manifestations indicating acute renal failure. During this period, the quantitative indicators of potassium content are gradually normalized, nitrogenous compounds are successfully removed, and the blood is purified.
The fourth stage is accompanied by a healing process; during this period, the water-electrolyte and acid-base balance is normalized. Also, the daily secretion of urinary fluid is completely restored to natural norms.
The recovery process, unfortunately, is accompanied by a sufficient duration, it can even reach one year. With improper treatment, non-compliance with medical prescriptions, as well as in particularly severe cases, chronic renal failure occurs against the background of an acute form.
Acute renal failure. Types, etiology, pathogenesis
One of the most severe consequences of various kidney lesions is renal failure (RF) - the inability of the kidneys to cleanse the blood of metabolic products and maintain a constant composition of the blood plasma. According to the mechanism of occurrence and course of PN, it can be acute (ACN) or chronic (CRF).
Types, etiology and pathogenesis of acute renal failure is a sudden impairment of kidney function due to the action of exogenous or endogenous damaging factors on them.
Etiological factors of acute renal failure are divided into 4 types:
1) prerenal,
2) renal,
3) postrenal and
4) arenal.
Prerenal causes of acute renal failure:
a) sudden drop in blood pressure (bleeding, trauma, shock, collapse),
b) loss of large quantities of water and electrolytes due to uncontrollable vomiting, diarrhea, and overdose of diuretics. All this leads to a decrease in blood volume, a drop in renal plasma flow, a decrease in glomerular filtration, and the development of the first, initial stage of acute renal failure - oligoanuric. Thus, the main thing in the pathogenesis of initial acute renal failure is impaired blood circulation in the kidneys and ischemic damage to the renal tissue - hypoxia and even necrosis of tissue elements.
ARF of renal origin develops as a consequence of direct damage to the kidney parenchyma due to poisoning with specific nephrotoxic substances, especially salts: mercury, uranium, chromium, poisoning with phosphorus, acetic acid, mushrooms, drugs - sulfonamides, antibiotics, quinine substances in case of overdose or as a result of increased individual sensitivity to drugs. The mechanism of their action is that they have a direct toxic effect on the epithelial cells of the kidney tubules, causing
1) necrobiotic changes in the protoplasm of tubular epithelial cells with subsequent rupture of their basement membrane,
2) tubulorrhexis.
Anuria during these measurements in the kidneys is due to the fact that the glomerular filtrate is completely
1) reabsorbed back in the tubules or
2) goes into the interstitial tissue of the kidney, and then leaves the renal parenchyma through the interlymphotic and venous vessels, enters the blood and causes intoxication of the body.
The cause of renal acute renal failure may be severe toxic-allergic processes.
ARF of postrenal origin is a consequence of occlusion (blockage) of the upper urinary tract with stones due to urolithiasis and tumors of various origins.
The arenal form of acute renal failure develops in the case of traumatic crushing of both kidneys or removal of kidneys for health reasons.
The pathogenesis of acute renal failure is acute blockade of kidney function, first of all, leading to disturbances in extracellular hemostasis. The accumulation of various substances in the extracellular space creates an increased load inside the cells, where catabolic processes begin to predominate.
During acute renal failure there are 4 main stages:
1) initial,
2) oliguric,
3) polyuric,
4) recovery or recovery stage.
The initial stage of acute renal failure usually coincides with the period of exposure to the etiological factor (shock, collapse, sepsis, poisoning). Already on the first day, diuresis decreases and oliguria develops, fluid retention occurs and hyperazotemia appears up to 1.5-2 g/l.
In the oligoanuric stage (the main stage of the disease), the most severe changes in homeostasis occur and the entire pathogenetic chain unfolds: hyperhydration (water retention in tissues); hyperkalemia (due to the release of large amounts of potassium from the cells, which, under conditions of acidosis, can cause cardiac arrest - this is the most common cause of death in acute renal failure in the oligoanuria stage. An increase in phosphates in the blood leads to hypocalcemia and tendencies
to cramps from lack of calcium. Acute kidney blockade is partially compensated in the first phase by other organs - especially the gastrointestinal tract, which secretes up to 3-4 grams per day. dry urea. Urea is partially released through the skin - sweat glands. Often, at the height of uremic intoxication, frost—urea crystals—can be seen on the wings of the nose. However, compensatory possibilities are very limited. Therefore, an extremely serious condition usually develops quite quickly and, in the absence of proper treatment (especially connection to an artificial kidney), there is a high mortality rate. In addition, hyperazotemia develops (disintegration of tissue proteins; hyponatremia as a result of blood dilution, i.e., blood hyperhydration. Erythropoiesis is very quickly disrupted - anemia (Hb up to 50-60 g/l). If the acute stage passes, then polyuria occurs and after After several months, renal function is restored.
The polyuric stage occurs in 2 stages. The first stage is the early diuretic phase, the second is the polyuria phase. Diuresis increases gradually over 4-5 days, the amount of urine increases from 400-500 ml to 2-4 liters. Initially, urine has a low specific gravity and low urea and creatine content. The decrease in the concentrating ability of the kidneys persists for 2-3 weeks and then recovers. Anemia lasts longer. The polyuric stage is characterized by:
1) hypohydration (release of water);
2) hypokalemia,
3) hyponatremia,
4) hypocalcemia.
The recovery or recovery stage continues for several months, depending on the severity and duration of acute renal failure.
Diagnostics
In acute renal failure, treatment should be based on diagnostic results, which in this case implies an analysis of clinical manifestations and the results of laboratory and instrumental studies.
Urologists also strive to identify the causes that provoked the pathology, since the treatment process involves direct impact on the source of the problem in order to not only eliminate the disease, but also prevent relapse in the future.
A general blood test reveals anemia; in some cases, lymphopenia and leukocytosis can be detected.
A general analysis of the urinary fluid is also performed. Eosinophils in the urine indicate that the patient is developing acute nephritis. If pigment casts are detected, the fact of acute necrosis of the renal tubules is established. Red blood cells, leukocytes, hyaline and granular casts can also be detected in the urine.
Urologists also refer the patient for a biological examination of urine, during which it is possible to confirm the fact of acute inflammatory processes. Along with this, a biochemical blood test is performed, making it possible to establish accurate indicators of urea and creatinine levels. Thanks to this laboratory test, metabolic acidosis can be detected.
Urologists also direct the patient to undergo instrumental diagnostics. Initially, the cardiovascular system and heart performance are checked, so the patient is recommended to have an ECG, which allows to identify heart rhythm disturbances.
A chest x-ray is required because doctors need to know the condition of the lungs. Pulmonary edema or fluid accumulation in the pleural areas may be diagnosed.
Angiography is a type of instrumental diagnostic that allows you to evaluate the vascular system.
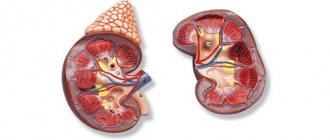
Ultrasound diagnostics allows doctors to determine the size of the kidneys, identify the presence of stones, as well as possible tumor formations.
To assess the performance of the kidneys in renal forms of acute renal failure, radioisotope scanning, computed tomography and MRI are performed. In exceptional cases, a kidney biopsy is performed.
Differential diagnosis
A diagnosis of AKI may be indicated by a sudden increase in serum creatinine or blood urea nitrogen. Reduced diuresis is also an important factor. The presence of chronic kidney disease should be determined.
In acute renal failure, laboratory and radiological diagnostic methods are much more effective than medical history and physical examination.
Disease history
The possibility of developing acute renal failure should be considered in all children in critical condition. Reduced diuresis, hematuria, dysuria, nausea, and vomiting may accompany acute renal failure. Prenatal history and birth can help identify the causes of acute renal failure in newborns, such as oligomeganephronia in children who had a small gestational age at birth (premature), etc.
Physical examination
- Impaired water excretion (diuresis less than 10-12 ml/kg/day or 0.5 ml/kg/hour)
- Increasing azotemia (urea nitrogen more than 7 mmol/l, creatinine more than 0.1 mmol/l, residual nitrogen more than 30 mmol/l)
- Electrolyte imbalance (increase in potassium more than 6 mmol/l, decrease in calcium less than 2 mmol/l and sodium)
- Decompensated metabolic acidosis (BE more than 10 mmol/l)
The difference between prerenal insufficiency and renal insufficiency:
| surge arrester | Urine density | Na concentration in urine | urea (urine)/urea (plasma) | creatinine (urine)/creatinine (plasma) | osmolarity (urine)/osmolarity (plasma) | test with mannitol (diuresis) |
| Prerenal | >1015 | <30 | >20/1 | >30/1 | >1,8 | >40 ml/hour |
| Renal | <1015 | >30 | <10/1 | <10/1 | <1,2 | <40 ml/hour |
Mannitol test - 100 ml 20% Manitol intravenously per hour. No diuresis - furosemide 200 mg per hour. No diuresis - renal failure.
Notes
- Milovanov Yu. S., Nikolaev A. Yu.
Acute renal failure // Russian Medical Journal. - 1998. - No. 19. - Shabalin V.V. Grinshtein Yu.I. Baykova O.A. Modern criteria for acute renal failure. The meaning of rifle classification Siberian Medical Review Issue No. 2 / volume 62 / 2010
- Fortenberry JD, Paden ML, Goldstein SL. Acute kidney injury in children: an update on diagnosis and treatment. Pediatr Clin North Am. 2013;60(3)
- Carol D. Berkowitz.
Berkowitz's Pediatrics: A Primary Care Approach. — 5th Edition. - American Academy of Pediatrics, 2014. - ISBN 9781581108460.