The folk way to cleanse the kidneys! Our grandmothers were treated using this recipe...
Cleaning your kidneys is easy! You need to add it during meals...
Have you been trying to cure your KIDNEYS for many years?
Head of the Institute of Nephrology: “You will be amazed at how easy it is to heal your kidneys just by taking it every day...
Read more "
Chronic kidney disease (CKD) is a disease that represents a decrease in the functional capacity of the kidneys or a violation of their integrity within 3 months. The prevalence of the disease among the population exceeds 10%, reaching 20% in a certain category of people (for example, patients with diabetes). There was no uniform classification of chronic renal failure (CKD). Doctors used the Ratner or Tareev classification. However, there is an urgent need to introduce a common system for diagnosing the disease so that every doctor can understand what his colleague is talking about.
Modern classification of CKD
American nephrology experts have proposed a universal way to classify the disease, which is based on 2 criteria. These are, first of all, the glomerular filtration rate and signs of kidney damage.
The combination of these two criteria defines 5 stages of ESRD development:
- normal GFR (glomerular filtration rate);
- slight decrease in eGFR;
- decrease within the normal range;
- pronounced decrease;
- severe decline;
- renal failure.
The last 3 stages are identical to the term “chronic kidney disease”, resulting in a disruption of the functional functioning of the organ.
Causes of disease development and syndromes
Chronic kidney disease can develop or progress under the influence of a number of factors, including:
- diabetes;
- excess weight;
- arterial hypertension;
- elevated lipid levels;
- urinary tract infections;
- smoking;
- autoimmune diseases;
- elderly age;
- kidney damage from toxins.
However, this is not the entire list of reasons that contribute to the development of CKD.
Chronic kidney disease can develop due to hereditary diseases or organ loss.
Due to the progress of CKD, the following syndromes are observed: increased blood pressure, changes in the acid-base balance in the body, decreased hemoglobin levels, azotemia, decreased concentrations of certain trace elements in the blood.
Diagnosis and treatment
Previously, it was assumed that kidney failure began after a patient was diagnosed with chronic kidney disease. However, at this stage of development of nephrology, the diagnosis of CKD means the inevitability of disease progression. This should concern the attending physician, otherwise the risk of complete loss of kidney function is very high.
Based on this, the patient must follow all the doctor’s clinical recommendations, otherwise the progression of the disease can cause irreparable dysfunction of organs. In case of illness, nephroprotective and specific treatment is prescribed.
Specific treatment is aimed at treating chronic kidney disease. If we are talking about glomerulonephritis, then steroids or BIARL should be used. If the urinary tract is affected by infection, antibiotics must be used. An important part of treatment is antihypertensive therapy.
Nephroprotective treatment is prescribed for renal failure and is aimed at slowing the progression of the disease. If renal failure progresses, special therapy is prescribed. It consists of taking vitamin D, erythropoietin, following a diet, and correcting secondary hyperparathyroidism. If chronic kidney disease is at the last stage, hemodialysis or a kidney transplant should be performed immediately.
Search by ICD-10 code
International Statistical Classification of Diseases and Related Health Problems, 10th Revision. With changes and additions published by the World Health Organization in 1996-2016. The latest changes to ICD-10 (as of 2020) were made by WHO in 2020.
The term “chronic kidney disease” (CKD) is a new concept, previously known as chronic kidney failure.
It is not a separate disease, but a syndrome, that is, a complex of disorders that are observed in the patient for three months.
According to statistics, the disease occurs in approximately 10% of people, and both women and men are susceptible to it.
Grades and stages of CKD when diagnosed: 1 2 3 4 5
Many people do not even realize that their kidneys are sick, that they have CKD of 1 2 or 3 4 and 5 degrees or stages. Chronic kidney disease is unknown, since measures for its prevention and detection in Russia are simply not developed. In different countries of the world, in the process of so-called screening studies of tens of thousands of people for the presence of CKD, based on indicators of urine and kidney function tests, it was found that approximately every tenth person examined has one or another kidney damage: some have milder, others things are much worse, that is, more serious, which ultimately may require treatment to replace kidney function - dialysis, or even an undesirable procedure - a kidney transplant.
According to large population registries, the prevalence of chronic kidney disease or CKD is indeed at least 10%, reaching 20% or more in certain categories of people, including older people and patients with type 2 diabetes mellitus. By comparison, chronic heart failure occurs in only one percent of the population, asthma in five percent of adults, diabetes in seven or ten percent, and widespread hypertension in 20-25 percent.
Causes
There are many factors that cause kidney dysfunction; the most likely causes include:
- arterial hypertension . Persistently elevated blood pressure and the disorders that accompany hypertension cause chronic failure;
- diabetes . The development of diabetes mellitus provokes diabetic kidney damage, which leads to chronic disease;
- age-related changes in the body. Most people develop CKD after age 75, but if there are no associated diseases, the syndrome does not lead to serious consequences.
In addition, CKD can provoke conditions that are associated with dysfunction of the kidneys and urinary system (renal artery stenosis, urinary outflow disorders, polycystic disease, infectious diseases), poisoning accompanied by kidney damage, autoimmune diseases, obesity.
Hypertension and kidney function are directly related - in people diagnosed with CKD, it ultimately causes problems with blood pressure.
Theoretical information
At the very beginning, renal tissue dysfunction practically does not manifest itself, this is due to the fact that the remaining tissue functions in an enhanced mode. This phenomenon can be characterized as an adaptation of the kidneys, for example, with the loss of 23 all kidney tissue, GFR (glomerular filtration rate) decreases by only 50% when compared with normal. The decrease in kidney performance is compensated by their ability to regulate electrolyte and water homeostasis. Changes occur in a clear sequence, but there are also parallel processes that can create many problems for the patient.
As the GFR content in plasma decreases, the concentration of urine and creatine elements increases; this process depends on the degree of glomerular filtration. At first, changes are minimal. The content of creatine and urine are not the most important signs of uremia (autointoxication, acute or chronic, resulting from renal failure, which is caused by the retention of nitrogenous metabolites in the body), they are just markers for a large number of other substances, and it is they that lead to symptoms.
Kidney problems are characterized by water and sodium overload, which can cause heart failure, especially in those patients who have a small cardiac reserve.
Thanks to adaptation, the levels of substances are at an acceptable level, the nephrons are responsible for this, secretion occurs in them, this occurs until the progression of renal failure begins. Patients experience problems with the metabolism of calcium, vitamin D, phosphates, parathyroid hormone, and we must not forget about the likely development of renal-type osteodystrophy. As a result of these changes, the body experiences significant problems, and the continued absence of the problem only aggravates the situation.
Symptoms
At the first and second stages of the disease, it does not manifest itself in any way, which greatly complicates the diagnosis.
As the disease progresses, other signs appear, including:
- rapid and unexplained weight loss, loss of appetite, anemia;
- decreased performance, weakness;
- pale skin, dryness and irritation;
- the appearance of edema (extremities, face);
- frequent urge to urinate, decreased amount of urine;
- dry tongue, ulceration of mucous membranes.
Most of these symptoms are perceived by patients as signs of other ailments or ordinary fatigue, but if they continue for several months, they should consult a doctor as soon as possible.
CKD: signs
It is often very difficult to predict a chronic disease, especially at the beginning. In addition, the main manifestations, for example, stage 4 of CKD, can be hidden with herbal treatment. At the same time, such self-medication does not restore the normal functioning of the organ, but only masks the main manifestations of the disease, preventing it from being detected in time. So it turns out that a lover of self-medication, having hidden his disease from himself and doctors, is faced with the need to know at what stage of CKD hemodialysis is performed - after all, nothing else will simply help at the late stage of development of the disease.
To avoid such an outcome, you should be as attentive as possible to your body and, if you have any doubtful signs, immediately go to the doctor and get tested to identify the cause.
The first symptom that should alert a person is a change in the volume of discharge. The amount of urine may become less than usual, which is associated with poor functioning of the organ. In some cases, the opposite happens: urine is produced in volumes exceeding the norm, which is accompanied by constant thirst.
The composition and color of urine also changes under the influence of pathology: blood and sediment appear. Quite often, with CKD, the pressure in the kidneys increases, renin is released, due to which the pressure in general increases. The person feels weak and loses his appetite. This is explained by toxicosis caused by insufficient blood purification by the kidneys. At the same time, swelling of the extremities is disturbing, and inflammatory processes occur in the kidneys.
Classification
The pathological process develops gradually, sometimes over several years. passing through several stages.
With a pathology such as chronic kidney disease, the stages are as follows:
- initial. The patient’s tests at this stage may not show serious changes, but dysfunction is already present. As a rule, there are also no complaints - there may be a slight decrease in performance and an increased urge to urinate (usually at night);
- compensated _ The patient often gets tired, feels drowsy and generally unwell, begins to drink more fluids and go to the toilet more often. Most test parameters may also be within normal limits, but dysfunction progresses;
- intermittent. Signs of the disease increase and become pronounced. The patient's appetite worsens, the skin becomes pale and dry, and sometimes blood pressure rises. In a blood test at this stage, the level of urea and creatinine increases;
- terminal. The person becomes lethargic, feels constant drowsiness, and the skin becomes yellow and flabby. The water and electrolyte balance in the body is disrupted, the functioning of organs and systems is disrupted, which can lead to early death.
Chronic kidney disease according to ICD-10 is classified as N18.
Chronic kidney disease
The kidneys are a kind of laboratory of the human body. During the day they pump a lot of blood, cleanse it of toxins and other harmful waste products. Disturbances in the functioning of this organ often lead to the development of complex and sometimes irreversible processes that not only reduce the quality of life, but can also cause the death of the patient. Clinical signs of diseases affecting the kidneys may have pronounced or hidden symptoms, but if their functionality is impaired for more than 3 months, a nephrologist can make a diagnosis of “chronic kidney disease,” which can manifest itself against the background of other sluggish pathologies of the urinary system.
In urology, chronic kidney disease is often called chronic renal failure, which is a serious disease in which there is disruption of the functioning of almost all organs and systems. What is CKD, how does it develop, what are the symptoms, types of disease, how to treat and what prognosis awaits the patient? You can get answers to these questions by reading this article.
What is CKD?
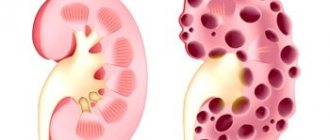
Chronic kidney disease (CKD) is a pathology that combines several conditions in which damage or decreased function of the glomerular filtration rate (GFR) occurs in the kidney tissues. During the development of this disease, the nephrons of the kidneys die or are replaced by connective tissue. Such pathological processes lead to irreversible disturbances in the functioning of the kidneys, which are unable to perform their functions of purifying the blood and removing excess water and absorbing electrolytes.
Chronic kidney diseases often develop against the background of a disorder of water, electrolyte, nitrogen or acid-base balance, which lasts for several months. The diagnosis of CKD is most often made by a doctor after the results of differential diagnosis, the results of which make it possible to determine the underlying disease that caused the development of pathologies of the urinary system.
Those at risk for developing the disease are those with a history of pathologies of the cardiovascular system, diabetes mellitus, neurological diseases or pancreatic diseases. According to statistics, this disease is diagnosed in 10% of the population of different age categories, including children.
When diagnosing CKD, the GFR indicator is considered important, which allows one to determine the number of dead nephrons. When the readings are less than 60 ml per minute, and there are significant disturbances in the functioning of the urinary system, we can talk about the death of half of the nephrons in the renal tissues, which is already considered a fairly serious pathology with irreversible consequences.
Causes
Chronic kidney disease most often develops in the presence of systemic or nephrological diseases, which may have indolent symptoms or manifest themselves with severe symptoms:
- chronic glomerulonephritis;
- chronic pyelonephritis;
- urolithiasis with impaired urine outflow from the renal pelvis;
- hydronephrosis;
- anatomical structure of the urinary system;
- malignant kidney lesions;
- systemic connective tissue diseases;
- arterial hypertension;
- acute renal failure;
- diabetes;
- hepatitis;
- gout;
- heredity;
- severe intoxication of the body;
- chronic alcoholism;
- polycystic ovary syndrome;
- long-term use of potent drugs;
In addition to the main causes, predisposing factors can act as a trigger for the development of this condition, including smoking, old age, regular nervous strain, and autoimmune disorders.
Chronic kidney disease in children most often manifests itself as a result of a family history, when one of the parents suffers from severe pathologies or as a result of congenital defects. The folk way to cleanse the kidneys! Our grandmothers were treated using this recipe...Cleaning your kidneys is easy! You need to add it during meals...
Classifications and stages of the disease
The modern classification of CKD identifies 5 stages of the disease, each of which has its own characteristics, types according to stages of severity, and indicators of the level of glomerular filtration rate (GFR). Until recently, the stages of CKD consisted only of GFR indicators, but at the moment, when making a diagnosis, special attention is paid to other indicators.
If we consider the stages according to GFR, they can be divided into the following indicators of norm and deviation, but initially it should be noted that in a healthy person 80-120 ml min is considered normal.
Filtration rates at various stages:
- CKD stage 1. Accompanied by a slightly increased GFR from normal, on average 90 ml/min.
- CKD stage 2. Indicators decreased slightly, about 80-60 ml/min.
- 3rd stage. GFR in CKD c3a is moderately reduced and amounts to 60-30 ml/min.
- 4th stage. The GFR level is up to 30-15 ml/min.
- CKD stage 5. The most severe is terminal, in which GFR is less than ml/min.
In addition to GFR indicators, the classification of chronic kidney disease consists of the same stages of the disease, each of which has characteristic symptoms.
Stage 1 of the disease
The glomerular filtration rate is slightly increased, but there may be no symptoms or only minor symptoms. At this stage, tubulointerstitial syndrome, disorders of the urinary system, nephrogenic hypertension and other minor symptoms may be present. With timely diagnosis, it can be cured or kept under control, but if there is no therapy, the clinical picture will be more pronounced, and the disease itself will actively progress.
Stage 2 CKD
Clinical signs of stage 2, more pronounced than in the 1st phase of the disease. This syndrome most often affects older people. Stage 2 CKD is accompanied by such symptoms as:
- decreased daytime diuresis;
- increased thirst;
- chronic weakness;
- pale skin;
- swelling of the upper and lower extremities;
- heart rhythm disturbance;
- increased blood pressure;
- change in urine parameters in the analysis.
Stage 3 CKD
Compensated or CKD stage 3. accompanied by damage to the mucous membranes and disorders of other organs and systems. Daily diuresis can reach a volume of 2.5 liters, problems with the functioning of the cardiovascular system appear, renal blood flow is disrupted, which can provoke acidosis or anemia in CKD. In addition to the main symptoms, the clinical picture of stage 3 CKD is constantly increasing, the patient develops:
- heart rhythm disturbance;
- blood pressure surges;
- dry mouth;
- insomnia;
- dry mouth.
Stage 4
At this stage, the disease is severe and can lead to death. The patient has all the symptoms of chronic renal failure, and azotemia, oliguria or anuria are also present. In stage 4 CKD, the amount of urea and creatinine in the blood increases significantly, which should normally be excreted in the urine. Characteristic symptoms at this stage are:
- increased weakness;
- nausea;
- lack of appetite;
- dry mouth;
- decreased diuresis or its complete absence;
- swelling of the body;
- damage to the heart muscle;
- skin itching.
Stage 5
The last and most severe stage of the disease, in which a large amount of protein metabolism products and toxins accumulate in the patient’s blood, which significantly affects the functioning of all organs and systems. CKD stage 5 also called terminal, characterized by persistent symptoms of renal and cardiovascular failure, the functioning of the bronchopulmonary system is disrupted. The patient feels:
- constant fatigue;
- nausea, urge to vomit;
- complete lack of appetite;
- decreased daily diuresis;
- pronounced swelling;
- severe skin itching;
- ammonia odor from the mouth;
- convulsions, even paralysis;
- severe anemia;
- dyspnea;
- uremia.
At this stage, there is a high risk of developing internal bleeding; the patient requires constant medical supervision.
Regardless of the stages of chronic kidney disease, treatment should begin as early as possible. Timely diagnosis of the underlying disease that has led to impaired renal function will help significantly reduce the risk of complications that can be life-threatening.
Complications
If chronic kidney disease is not treated in time, the consequences can be irreversible and very disastrous. With constant disruption of organ function, the entire body suffers, so complications can have severe and irreversible consequences.
- fluid retention in the body.
- anemia;
- pathologies of the cardiovascular system;
- damage to the skeletal system;
- severe intoxication of the body;
- death.
Chronic kidney damage can combine a whole group of diseases that affect the organs of the urinary system, so before starting treatment, it is important to identify and eliminate the main etiological factor. Depending on the stage of chronic kidney disease, the stages can provoke certain disturbances in the functioning of internal organs, so the earlier the disease is diagnosed, the greater the chances of a successful recovery.
Diagnostics
In order to make a correct diagnosis of kidney dysfunction, you need to undergo a series of laboratory and instrumental tests, which will be prescribed by a nephrologist or urologist after taking an anamnesis and studying the patient’s medical history.
- Urine and blood analysis.
- Ultrasound of the kidneys and abdominal organs.
- Kidney CT.
- Contrast urography.
- Analysis of GFR indicators (determination of creatinine clearance).
The research results will help the doctor create a complete picture of the disease, make the correct diagnosis, and prescribe appropriate treatment. If necessary, the doctor may prescribe other research methods, including the use of the MDRD formula, which allows you to determine the exact cause of the disease and determine the indicators of CKD with GFR. The correct formulation of the diagnosis is the first step on the path to recovery. The main thing is to recognize the disease in time and take all necessary measures to treat it.
Treatment methods
Treatment of CKD always consists of a set of therapeutic measures that allow influencing the cause, symptoms, and reducing the risks of complications. Therapy directly depends on the stage of the disease, the cause, the age of the patient and the characteristics of his body. Complex treatment may include taking medications and following a diet. If the disease is diagnosed in the last stages, then the patient needs constant hemodialysis, which will cleanse the blood of toxins and prolong the patient’s life. Curing CKD in the later stages is difficult and almost impossible, and the only way to improve a person’s life is an organ transplant.
Conservative therapy gives good results only in the initial stages of the disease. Patients are prescribed a number of medications, dietary nutrition, and adherence to work and rest schedules. With the right treatment, you can slow down the progression of the disease, improve the functioning of the kidneys and other organs and systems.
Drug therapy
Drug therapy will reduce the symptoms of uremia, reduce the content of nitrogen metabolic products in the blood, accelerate their elimination, and also eliminate the root cause. Therapy may include taking the following groups of drugs:
- Angiotensin-converting enzyme inhibitors.
- Angiotensin receptor blockers.
- Vitamin D preparations.
- Statins.
- Anabolic steroid.
In addition to the main medications, the doctor prescribes other medications, the mechanism of action of which will be aimed at eliminating the symptoms of the disease. The choice of drug and therapeutic course should always remain with the attending physician.
Replacement therapy
If chronic kidney disease has reached stage 5, the only treatment option will be replacement therapy, which consists of blood purification using an “artificial kidney.”
- Hemodialysis.
- Peritoneal dialysis.
- Kidney transplant.
A kidney transplant operation has high risks and high costs, and is also often complicated by finding a donor. People with advanced CKD sometimes undergo hemodialysis for decades, performed once or more times a week. Without hemodialysis, a person dies within a few months or weeks.
Nutrition for CKD
An integral part of treatment and prevention is considered to be a diet for chronic renal failure, which must be followed at all stages of the disease. Patients with impaired renal function are prescribed table No. 7a, b, p, which includes limiting protein foods. Patients are recommended to switch to plant protein and adhere to a vegetarian diet. The diet consists of limiting the following foods:
- cottage cheese;
- fatty meats;
- fish;
- legumes;
- any alcohol;
- butter.
It is important to reduce your salt intake. The patient is recommended to take no more than a third of a teaspoon per day. It is strictly forbidden to consume spicy, fried, fatty foods, as well as strong coffee and alcohol. Eating prohibited foods puts a significant strain on the kidneys. Patients are recommended to do “fasting days” or follow a mono-diet 2 times a week, which will consist of eating one product during the day.
When the patient is on dialysis, the diet, on the contrary, should consist of eating protein foods. It is recommended to consume at least 1 g of protein per 1 kg of body weight per day, and amino acids should also be included in the diet. The energy value of food should be 30–35 kcal per 1 kg of weight per day. An approximate menu will be prescribed by the attending physician individually for each patient.
Chronic kidney disease, treatment should always be prescribed by a doctor. This will increase the chances of a successful forecast.
Forecast
With proper and timely treatment of kidney disease, the patient has every chance of a full recovery, but when CKD reaches the 4th or 5th stage of the disease, full recovery can only be achieved with the help of a kidney transplant.
Prevention
To reduce the risk of developing chronic kidney disease, it is necessary to promptly and correctly treat all concomitant diseases of the urinary system and internal organs. The following preventive measures will help reduce the risk of developing pathologies affecting the kidneys:
- quitting smoking and alcohol;
- proper and healthy nutrition;
- weight control;
- proper treatment of all concomitant diseases;
- absence of stress and nervous tension;
- regularly boosting immunity.
Kidney diseases are quite difficult to treat, but with timely diagnosis and proper therapy, it is much easier to reduce the risk of their complications. It is important to understand that preventing a disease is much easier than treating it, therefore, at the first sign of it, you should not hesitate to visit a doctor and in no case should you self-medicate.
Diagnostics
The diagnosis of CKD is made on the basis of a set of studies, which include urine tests (general, biochemical, Zimnitsky test) and blood tests, kidney ultrasound and CT, and isotope scintigraphy.
The presence of the disease may be indicated by protein in the urine (proteinuria), an increase in the size of the kidneys, cysts and tumors in the tissues, and dysfunction.
One of the most informative studies to identify CKD and its stage is to determine the glomerular filtration rate (GFR). A significant decrease in this indicator can indicate CKD, and the lower the rate, the more severely the kidneys are affected. According to the GFR level, chronic kidney disease has 5 stages.
A decrease in GFR to 15-29 units or lower indicates the last stages of the disease, which poses a direct threat to human life.
What is chronic kidney disease?
Until recently, our doctors operated only with the concept of chronic renal failure. But recently they began to use the definition - chronic kidney disease. The category of these diseases includes various renal pathologies that last for three months or more and are accompanied by pathological or pathological disorders in renal activity. This diagnosis can only be made to a certain category of the population - adults, pregnant women and adolescents over 16 years of age. Children are not given this diagnosis.
Criteria for the disease according to the international classification
In world practice, this classification has been used since 2002.
In world practice, this classification has been used since 2002, and in our country, CKD, which is the abbreviated name for chronic kidney disease, began to appear in patient diagnoses since 2006. According to the international classification, this disease has clear criteria:
- Any kidney disease that continues for three or more months. In this case, the disease should manifest itself as functional and structural disturbances in the functioning of the organ. If GFR does not decrease, then one of two manifestations of the disease is present:
- pathomorphological changes;
- signs of kidney disease - abnormalities in blood, urine and other tests.
- There is a decrease in glomerular filtration rate (GFR). This diagnosis is made if the GFR is less than 60 ml per minute for three months or more, but there are no symptoms of kidney damage.
In other words, if during a medical examination (laboratory tests of urine, blood, biopsy) signs of renal pathology are detected, and if the disease lasts more than 3 months, then a diagnosis of CKD is made. If, apart from a decrease in EF of less than 60 ml/min during the specified period, there are no more signs of the disease, then the diagnosis of CKD is made automatically.
Important: based on the above, it can be argued that all chronic kidney diseases fall into the category of CKD.
At first glance, it seems strange that in addition to chronic renal failure, there is another medical term for a similar condition. However, this term is needed because chronic kidney disease has certain stages, which is why it is important to indicate the stage of CKD when making a diagnosis. Based on the stage of CKD, you can determine the prognosis - find out the volume of damaged kidney tissue, the time period during which the organ can function without the use of an artificial kidney apparatus. This will also help develop a single universal approach to the treatment of different types of kidney diseases.
Classification by GFR
Chronic kidney disease is divided into several stages according to the glomerular filtration rate
Chronic kidney disease is divided into several stages based on the rate of glomerular filtration. There are 5 stages, of which the first and second are the most common. The fifth stage of this disease is a rather rare occurrence.
Chronic kidney disease – stages according to GFR:
- Kidney diseases with increased or normal filtration rate. GFR greater than 90 ml per minute. The incidence of the disease is 3.3%.
- Slight decrease in SF (60-89 ml per minute). Occurs in 3% of the population.
- Moderate reduction in filtration rate (30-59). Frequency – 4.3% of the population.
- Marked decrease in filtration rate (15-29). Occurs in 0.2% of the population.
- Renal failure (GFR below 15). Frequency – 0.1% of the population.
It is worth knowing: if we sum up the prevalence of this disease among the population, then the share of all stages accounts for 10.9%. It is this proportion of people who suffer from CKD.
From this we can conclude that every tenth inhabitant of our planet has kidney diseases. Moreover, many of them do not even suspect the existence of such a problem. Often the diagnosis is made in an advanced stage of the disease, when it is impossible to restore the functions of the organ even with the use of the most highly effective therapeutic techniques. Treatment is prescribed depending on the stage of CKD. At the same time, you should not ignore treatment, since the disease can lead to dire consequences.
Features of treatment
The classification of kidney diseases by stages was not invented by chance; knowledge of the stage allows you to choose the right treatment tactics
The classification of kidney diseases by stages was not invented by chance. Knowing the stage allows you to choose the right treatment tactics. Thus, clinical recommendations for CKD depend on the stage. As the disease progresses, the likelihood of death increases. That is why renal replacement therapy is used in the treatment of the most extreme form of development.
Treatment of chronic kidney disease:
- Stage 1 – diagnosis and reduction of risks of chronic disease;
- Stage 2 – identification and treatment of other concomitant diseases, reducing the rate of progression of the disease, reducing the risk of CKD;
- Stage 3 – assessment of the progress of the disease and treatment of all kinds of complications;
- Stage 4 – the patient is being prepared for the use of an artificial kidney device;
- Stage 5 – in case of presence of uremia, renal replacement therapy (hemodialysis) is carried out.
In addition to the listed stages, the classification of CKD distinguishes a previous stage, which manifests itself in the form of an increased risk of kidney pathology. At this stage, the disease manifests itself only in the form of an increased risk of various renal pathologies, therefore, early diagnosis, reduction of the influence or complete elimination of dangerous factors of increased risk of organ pathologies are provided as therapeutic and preventive measures.
Why is kidney failure dangerous?
In addition to the risk of the disease progressing to the terminal stage, which carries with it the risk of death, CKD can cause a number of serious complications:
- disorders of the cardiovascular system (myocarditis, pericarditis, congestive heart failure);
- anemia, blood clotting disorder;
- gastrointestinal diseases, including duodenal and gastric ulcers, gastritis;
- osteoporosis, arthritis, bone deformities.
Disease: what are we talking about?
CKD is a chronic disorder of the kidneys, which over time leads to the development of insufficient functioning of this organ. Often the disease occurs without symptoms in the first stages, and the patient consults a doctor already at stage 4. Treatment of CKD at this stage is quite challenging.
There are quite a few cases from medical practice in which CKD was discovered at a stage when the only tangible effect could be provided by either organ transplantation or hemodialysis. This is the so-called terminal stage.
Treatment
Treatment of CKD includes treatment of the primary disease that causes the syndrome, as well as maintaining normal kidney function and protecting it. In Russia, there are National Recommendations regarding chronic kidney disease created by experts from the Scientific Society of Nephrologists of the Russian Federation.
Chronic kidney disease treatment involves the following:
- reducing the load on healthy kidney tissue;
- correction of electrolyte imbalance and metabolic processes;
- cleansing the blood of toxins and breakdown products (dialysis, hemodialysis);
- replacement therapy, organ transplantation.
If the disease is detected at a compensated stage, the patient is prescribed surgical treatment, which restores the normal outflow of urine and returns the disease to the latent (initial) stage.
At the third (intermittent) stage of CKD, surgical intervention is not performed, since it is associated with a high risk for the patient. Most often, in this case, palliative treatment methods are used, which alleviate the patient’s condition, and detoxification of the body is also carried out. Surgery is possible only if kidney function is restored.
Approximately 4 times a year, all patients with CKD are recommended to receive infusion treatment in a hospital setting: administration of glucose, diuretics, anabolic steroids, and vitamins.
For stage 5 chronic kidney disease, hemodialysis is performed every few days, and for people with severe concomitant pathologies and heparin intolerance, peritoneal dialysis is performed.
The most radical method of treating CKD is organ transplantation, which is performed in specialized centers. This is a complex operation that requires tissue compatibility between the donor and recipient, as well as the absence of contraindications to the intervention.
Literature[edit | edit code]
- Sigitova, O. N.
Chronic kidney disease: terminology, methods for assessing progression and principles of nephroprotection // Medical practice: [site]. - 2009. - October 18. - Sigitova, O. N.
Chronic kidney disease and chronic renal failure: modern approaches to terminology, classification and diagnosis // Bulletin of modern clinical medicine: journal. - 2008. - No. 1. - P. 87. - UDC 616.61-036.12-07.001.33(G). - Chronic kidney disease: Recommendations for diagnosis and treatment: [arch. October 20, 2016] / Ed. prof. F. I. Belyalova. — Irkutsk: Irkutsk State Medical Academy of Postgraduate Education, 2020. — 30 p. — (inaccessible link). — BBK 54.1. — UDC 616.61-008.6(G).
- Pilotovich, V. S.
Chronic kidney disease: methods of renal replacement therapy / V. S. Pilotovich, O. V. Kalachik. - M.: Medical literature, 2009. - 288 p. - (Medical literature). — 2000 copies. — ISBN 978-5-89677-125-8. - Balkarov, I. M.
Nephrology: textbook. benefits for postgraduate students. education / I. M. Balkarov, V. V. Borisov, N. B. Gordovskaya ... []. - M.: GEOTAR-Media, 2007. - Chronic kidney disease. - pp. 599-612. — (Library of continuing education for doctors). — 5000 copies. — ISBN 978-5-9704-0482-9. - Shilov, E. N.
Chronic kidney disease / E. N. Shilov, V. V. Fomin, M. Yu Shvetsov // Therapeutic archive: journal. - 2007. - T. 79, No. 6. - P. 75–78. — ELIBRARY ID: 9584814. — UDC 616.61-036.12-08(G). - Shvetsov, M. Yu.
Everyone should know this! : What are kidneys for and how do they work? How to check your kidney condition? What causes kidney disease? How to keep your kidneys healthy? // Kidneys and health: journal. - 2011. - T. 15, No. 1. - P. 3–32. — Popular scientific supplement to the journal “Nephrology”. — ISSN 1561-6274. - doi:10.24884/1561-6274-2011-15-0-3-32.
Prevention
- balance your diet, avoid fatty, smoked and spicy foods, reduce your consumption of animal protein and salt;
- treat infectious diseases in a timely manner, especially diseases of the genitourinary system;
- reduce physical activity, avoid psycho-emotional stress if possible;
- do not self-medicate and do not take drugs that have a toxic effect on the kidneys.
Once a year (after 40 years - once every six months), take a general urine test and undergo a preventive ultrasound, which will help identify changes and kidney dysfunction in the early stages.
Infection and CKD
In recent years, kidney inflammation has occurred with much greater frequency than several decades ago. Of the other bacterial diseases common to all ages, kidney inflammation is diagnosed especially often.
It is known that in a healthy state a person has sterile urine and the urinary tract is free of germs. If the source of the disease enters the urinary canals, the bladder, an inflammatory process may begin. The disease is usually accompanied by pain and increased frequency of urination, and a burning sensation occurs when the bladder is emptied of fluid. When analyzing, it is noted that the urine is cloudy, often pinkish, which is explained by the presence of red blood cells.
The progress of the disease is accompanied by fever, abdominal and back pain, as well as vomiting and nausea. Re-infection can occur without fever. At the same time, it is known that in childhood, temperature is often the only indicator of the presence of infection. Repeated inflammation is associated with a high probability of developing renal failure. Often, secondary infection indicates progression of CKD.