Project news
2012-02-26
—
Updating the design and functionality of the site
We are pleased to present you the result of a lot of work, the updated ROS-MED.INFO.
The site has changed not only externally, but also new databases and additional functions have been added to existing sections:
⇒ The drug reference book now contains all possible data about the drug you are interested in:
— brief description by ATX code
- detailed description of the active substance,
- synonyms and analogues of the drug
— information about the presence of the drug in rejected and falsified batches of drugs
— information about the stages of drug production
— checking for the presence of the drug in the Vital and Essential Drugs (VED) register and displaying its price
— checking the availability of this drug in pharmacies in the region in which the user is currently located and displaying its price
— checking for the presence of the drug in the standards of medical care and patient management protocols
⇒ Changes in the pharmacy certificate:
— an interactive map has been added on which the visitor can clearly see all pharmacies with prices for the drug of interest and their contact information
— updated display of drug forms when searching for them
— added the ability to instantly switch to comparing prices for synonyms and analogues of any drug in the selected region
— full integration with the drug reference book, which will allow users to receive maximum information about the drug of interest directly from the pharmacy certificate
⇒ Changes in the Russian healthcare facilities section:
— the ability to compare prices for services in different health care facilities has been removed
— added the ability to add and administer your own healthcare facility in our Russian healthcare facility database, edit information and contact details, add employees and specialties of the institution
Acute renal failure
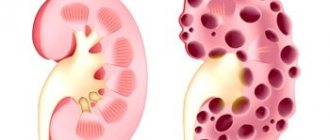
The kidneys are the main “filters” of the human body, the nephrons of which continuously pass blood through their membranes, removing excess fluid and toxins with urine, sending the necessary substances back into the bloodstream.
Kidneys are organs without which human life is impossible. Therefore, in a situation where, under the influence of provoking factors, they cease to fulfill their functional task, doctors provide emergency medical care to the person, diagnosing him with acute renal failure. The somatic pathology code according to ICD-10 is N17.
Today, statistical information makes it clear that the number of people facing this pathology is growing every year.
Etiology
The causes of acute renal failure are as follows:
- Pathologies of the cardiovascular system that disrupt the blood supply to all organs, including the kidneys:
- arrhythmia;
- atherosclerosis;
- heart failure.
- Dehydration against the background of the following ailments, which causes changes in blood parameters, or more precisely, an increase in its prothrombin index, and, as a consequence, difficulty in the functioning of the glomeruli:
- dyspeptic syndrome;
- extensive burns;
- blood loss.
- Anaphylactic shock, which is accompanied by a sharp decrease in blood pressure, which negatively affects kidney function.
- Acute inflammatory phenomena in the kidneys, which lead to damage to organ tissue:
- pyelonephritis.
- A physical obstruction to the outflow of urine during urolithiasis, which first leads to hydronephrosis, and then, due to pressure on the kidney tissue, to damage to the kidney tissue.
- Taking nephrotoxic drugs, which include a contrast composition for X-rays, causes poisoning of the body, which the kidneys cannot cope with.
Class XIV. N00-N99 Diseases of the genitourinary system
- selected conditions occurring in the perinatal period (P00-P96)
- some infectious and parasitic diseases (A00-B99)
- complications of pregnancy, childbirth and the puerperium (O00-O99)
- congenital anomalies, deformities and chromosomal disorders (Q00-Q99)
- diseases of the endocrine system, nutritional disorders and metabolic disorders (E00-E90)
- injuries, poisoning and some other consequences of external causes (S00-T98)
- neoplasms (C00-D48)
- symptoms, signs and abnormalities identified by clinical and laboratory tests, not classified elsewhere (R00-R99)
Class blocks
- N00-N08 Glomerular diseases
- N10-N16 Tubulointerstitial kidney diseases
- N17-N19 Renal failure
- N20-N23 Urolithiasis
- N25-N29 Other diseases of the kidney and ureter
- N30-N39 Other diseases of the urinary system
- N40-N51 Diseases of the male genital organs
- N60-N64 Breast diseases
- N70-N77 Inflammatory diseases of the female pelvic organs
- N80-N98 Non-inflammatory diseases of the female genital organs
- N99-N99 Other genitourinary system disorders
The following categories are marked with an asterisk:
- N08* Glomerular lesions in diseases classified elsewhere
- N16* Tubulointerstitial lesions of the kidneys in diseases classified elsewhere
- N22* Urinary tract stones in diseases classified elsewhere
- N29* Other lesions of the kidney and ureter in diseases classified elsewhere
- N33* Lesions of the bladder in diseases classified elsewhere
- N37* Lesions of the ureter in diseases classified elsewhere
- N51* Lesions of the male genital organs in diseases classified under other headings
- N74* Inflammatory lesions of the pelvic organs in women with diseases classified elsewhere
- N77* Ulceration and inflammation of the vulva and vagina in diseases classified elsewhere
Classification of surge arresters
The process of acute kidney failure is divided into three types:
- Prerenal acute renal failure - the cause of the disease is not directly related to the kidneys. The most popular example of a prerenal type of acute renal failure can be called disturbances in the functioning of the heart, which is why the pathology is often called hemodynamic. Less commonly, it occurs due to dehydration.
- Renal acute renal failure - the root cause of the pathology can be found precisely in the kidneys themselves, and therefore the second name of the category is parenchymal. Renal functional failure in most cases results from acute glomerulonephritis.
- Postrenal acute renal failure (obstructive) is a form that occurs when the urine excretion pathways are blocked by stones and subsequent disruption of urine outflow.
Classification of acute renal failure
Calculous pyelonephritis. Code N20.9
Develops against the background of kidney stones. If you identify the presence of stones in time and begin treatment, you can avoid chronicity of the disease.
Stones may not make themselves felt for years, making their diagnosis difficult. The appearance of severe pain in the lumbar region means only one thing - it’s time to contact a qualified specialist. It is sad that most patients are reluctant to consult a doctor at the first symptoms of the disease.
From the above it follows that this disease is a real chameleon among other pathologies. Insidious in its love to take the guise of other diseases, it can end sadly. Listen to your body. Do not drown out pain and other symptoms with self-medication. Seek help promptly.
Pathogenesis
ARF develops over four periods, which always follow in the specified order:
- initial stage;
- oliguric stage;
- polyuric stage;
- recovery.
The duration of the first stage can last from several hours to several days, depending on what is the root cause of the disease.
Oliguria is a term that briefly refers to a decrease in urine volume. Normally, a person should excrete approximately the amount of fluid that he consumed, minus the portion “spent” by the body on sweating and breathing. With oliguria, the volume of urine becomes less than half a liter, without a direct connection with the amount of fluid drunk, which entails an increase in fluid and breakdown products in the body tissues.
Complete disappearance of diuresis occurs only in extremely severe cases. And statistically it rarely happens.
The duration of the first stage depends on how quickly adequate treatment was started.
Polyuria, on the contrary, means an increase in diuresis, in other words, the amount of urine can reach five liters, although 2 liters of urine per day is already a reason to diagnose polyuric syndrome. This stage lasts about 10 days, and its main danger is the body’s loss of the substances it needs along with urine, as well as dehydration.
After completion of the polyuric stage, the person, if the situation develops favorably, recovers. However, it is important to know that this period may last for one year, during which deviations in the interpretation of analyzes will be identified.
Stages of acute renal failure
Differential diagnosis
| Sign | surge arrester | chronic renal failure |
| Subsequence Stages | Oliguria - polyuria | Polyuria - oliguria |
| Start | Acute | Gradual |
| Arterial pressure | + | + |
| Retarded physical development, osteopathy | — | -/+ |
| Kidney ultrasound | Enlarged more often | Reduced, increased Echogenicity |
| Dopplerography of renal vessels | Decreased blood flow | Decreased blood flow in combined with an increase resistance index Vessels |
Treatment abroad
Get treatment in Korea, Israel, Germany, USA
Get advice on medical tourism
Clinical picture
The initial stage of acute renal failure does not have specific symptoms by which the disease can be unmistakably recognized; the main complaints during this period are:
- loss of strength;
- headache.
The symptomatic picture is complemented by signs of the pathology that caused acute renal failure:
- With oliguric syndrome against the background of acute renal failure, the symptoms become specific, easily recognizable and fit into the overall picture of the pathology:
- decreased diuresis;
- dark, foamy urine;
- dyspepsia;
- lethargy;
- wheezing in the chest due to fluid in the lungs;
- susceptibility to infections due to reduced immunity.
- The polyuric (diuretic) stage is characterized by an increase in the amount of urine excreted, so all the patient’s complaints stem from this fact, and the fact that the body loses a large amount of potassium and sodium with urine:
- disturbances in the functioning of the heart are recorded;
- hypotension.
- The recovery period, which takes from 6 months to one year, is characterized by fatigue, changes in the results of laboratory tests of urine (specific gravity, red blood cells, protein), blood (total protein, hemoglobin, ESR, urea).
Hospitalization
Indications for hospitalization
1. Clinical: increased fatigue, nausea, vomiting, loss of appetite, weight loss, shortness of breath, itching, cramps, arterial hypertension, swelling and deterioration of the skin.
2. Exacerbation of the underlying disease or sudden decrease in kidney function.
3. Initiation of treatment with erythropoietin, parenteral administration of iron, vitamin D, paracalcitol, and hypolipidemic drugs.
Necessary examination before planned hospitalization: minimal examination upon referral to the hospital - clinical manifestations and laboratory tests confirming chronic renal failure (CBC, TAM, blood creatinine, glomerular filtration rate).
Diagnostics
Diagnosis of acute renal failure is carried out using:
- questioning and examining the patient, compiling his anamnesis;
- clinical blood test showing low hemoglobin;
- biochemical blood test, which detects increased creatinine, potassium, urea;
- diuresis monitoring, that is, control over how much liquid (including soups, fruits) a person consumes in 24 hours and how much is excreted;
- ultrasound method, in acute renal failure more often shows the physiological size of the kidneys; a decrease in size indicators is a bad sign, indicating tissue damage, which may be irreversible;
- nephrobiopsy - taking a piece of an organ using a long needle for microscopic examination; It is performed infrequently due to the high degree of trauma.
Treatment
Treatment of acute renal failure occurs in the intensive care unit of the hospital, less often in the nephrology department of the hospital.
All medical procedures performed by doctors and medical staff can be divided into two stages:
- Identification of the root cause of a pathological condition is carried out using diagnostic methods, studying symptoms, and specific complaints of the patient.
- Eliminating the cause of acute renal failure is the most important stage of treatment, because without treating the root cause of the disease, any treatment measures will be ineffective:
- when the negative effect of nephrotoxins on the kidneys is detected, extracorporeal hemocorrection is used;
- If an autoimmune factor is detected, glucocorticosteroids (Prednisolone, Metipred, Prenizole) and plasmapheresis are prescribed.
- in case of urolithiasis, drug litholysis or surgery is performed to remove stones;
- For infection, antibiotics are prescribed.
At each stage, the doctor adjusts the prescription based on the symptomatic picture at the moment.
During oliguria, it is necessary to prescribe diuretics, a strict diet with a minimum amount of protein and potassium, and, if necessary, hemodialysis.
Hemodialysis, a procedure for cleansing the blood of waste products and removing excess fluid from the body, has an ambiguous attitude among nephrologists. Some doctors argue that prophylactic hemodialysis for acute renal failure is necessary in order to reduce the risk of complications. Other experts warn of a trend towards complete loss of kidney function since the start of artificial blood purification.
During the period of polyuria, it is important to replenish the patient’s missing blood volume, restore the electrolyte balance in the body, continue diet No. 4, and take care of any infection, especially when taking hormonal medications.
General principles of treatment of acute renal failure
Prognosis and complications
Acute renal failure with proper treatment has a favorable prognosis: after suffering the disease, only 2% of patients require lifelong hemodialysis.
Complications from acute kidney failure are associated with, that is, with the process of poisoning the body with its own decay products. As a result, the latter are not excreted by the kidneys during oliguria or when the rate of blood filtration by glomeruli is low.
Pathology leads to:
- disruption of cardiovascular activity;
- anemia;
- increased risk of infections;
- neurological disorders;
- dyspeptic disorders;
- uremic coma.
It is important to note that with acute nephrological failure, unlike chronic failure, complications rarely occur.
Disease Prevention
To avoid the development of inflammation in the kidney tissues, a number of preventive measures should be followed. Experts recommend:
- avoid hypothermia;
- Healthy food;
- strengthen immunity;
- promptly treat infectious diseases.
The chronic form is dangerous because it may not manifest itself for a long time. The disease is diagnosed through the diagnosis of other pathologies. If symptoms occur, you should consult a doctor, since the acute form always develops into a chronic form, which is difficult to treat.
Prevention
Prevention of acute renal failure is as follows:
- Avoid taking nephrotoxic medications.
- Treat chronic diseases of the urinary and vascular system in a timely manner.
- Monitor blood pressure readings, and if signs of chronic hypertension are detected, immediately consult a specialist.
In the video about the causes, symptoms and treatment of acute renal failure:
The course of acute renal failure can be divided into initial, oligoanuric, diuretic and the phase of complete recovery. The initial phase can last from several hours to several days. During this period, the severity of the patient’s condition is determined by the cause that caused the development of the pathological mechanism of acute renal failure. It is at this time that all the previously described pathological changes develop, and the entire subsequent course of the disease is their consequence. A common clinical symptom of this phase is circulatory collapse, which is often so short-lived that it goes unnoticed. The oligoanuric phase develops in the first 3 days after an episode of blood loss or exposure to a toxic agent. It is believed that the later acute renal failure develops, the worse its prognosis. The duration of oligoanuria ranges from 5 to 10 days. If this phase lasts more than 4 weeks. , we can conclude that there is bilateral cortical necrosis, although there are known cases of recovery of renal function after 11 months. Oliguria. During this period, daily diuresis is no more than 500 ml. Urine is dark in color and contains a large amount of protein. Its osmolarity does not exceed plasma osmolarity, and the sodium content is reduced to 50 mmol/l. The content of urea nitrogen and serum creatinine increases sharply. Electrolyte imbalances begin to appear: hypernatremia, hyperkalemia, phosphatemia. Metabolic acidosis occurs. During this period, the patient notes anorexia, nausea and vomiting, accompanied by diarrhea, which after some time gives way to constipation. Patients are drowsy, lethargic, and often fall into a coma. Overhydration causes pulmonary edema, which is manifested by shortness of breath, moist rales, and Kussmaul breathing often occurs. Hyperkalemia causes severe heart rhythm disturbances. Pericarditis often occurs against the background of uremia. Another manifestation of an increase in serum urea is uremic gastroenterocolitis, which results in gastrointestinal bleeding that occurs in 10% of patients with acute renal failure. During this period, there is a pronounced inhibition of phagocytic activity, as a result of which patients become susceptible to infection. Pneumonia, mumps, stomatitis, pancreatitis occur, the urinary tract and postoperative wounds become infected. Sepsis may develop. The diuretic phase lasts 9-11 days. The amount of urine excreted gradually begins to increase and after 4-5 days reaches 2-4 liters per day or more. Many patients experience a loss of large amounts of potassium in the urine - hyperkalemia is replaced by hypokalemia, which can lead to hypotension and even paresis of skeletal muscles and cardiac arrhythmias. Urine has low density, it has low creatinine and urea content, but after 1 week. During the diuretic phase, with a favorable course of the disease, hyperazotemia disappears and electrolyte balance is restored. During the full recovery phase, kidney function is further restored. The duration of this period reaches 6-12 months, after which kidney function is fully restored.
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan) Version: Archive - Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2010 (Order No. 239)
Acute renal failure, unspecified (N17.9)
Symptoms
The symptoms of chronic renal failure are largely determined by the course of the underlying disease, however, regardless of the nosology that caused the development of glomerulosclerosis, chronic renal failure is characterized by changes in organs and systems caused by the effects of toxic metabolic products. At the moment, along with uremic toxins, more than 200 substances are known, the accumulation of which causes the progression of chronic renal failure. The appearance does not suffer until the stage when glomerular filtration is significantly reduced. Due to anemia, pallor appears, due to water and electrolyte disturbances, dry skin. As the process progresses, yellowness of the skin and mucous membranes appears and their elasticity decreases. Spontaneous bleeding and bruising may occur. Scratching occurs due to itchy skin. Characterized by so-called renal edema with puffiness of the face, up to the common type of anasarca. The muscles also lose tone and become flabby, which causes fatigue to increase and the ability of patients to work decreases. Nervous system lesions. This is manifested by apathy, night sleep disorders and daytime sleepiness. Decreased memory and learning ability. As chronic renal failure increases, severe inhibition and disturbances in the ability to remember and think appear. Disturbances in the peripheral part of the nervous system affect the limbs with chilliness, tingling sensations, and crawling sensations. Later, movement disorders in the arms and legs develop. Urinary function. She first suffers from polyuria (increased urine volume) with a predominance of nighttime urination. Further, chronic renal failure develops along the path of a decrease in urine volume and the development of edematous syndrome until the complete absence of excretion. Water-salt balance. Salt imbalance is manifested by increased thirst and dry mouth. Weakness, darkening of the eyes when standing up suddenly (due to sodium loss). Excess potassium is responsible for muscle paralysis. Breathing disorders. Decrease in heartbeats, arrhythmias, intracardiac blockades up to cardiac arrest. Against the background of increased production of parathyroid hormone by the parathyroid glands, high levels of phosphorus and low levels of calcium appear in the blood. This leads to softening of the bones, spontaneous fractures, and itchy skin. Nitrogen balance disturbances. They cause an increase in blood creatinine, uric acid and urea, as a result: When GFR is less than 40 ml per minute, enterocolitis develops (damage to the small and large intestines with pain, bloating, frequent loose stools). Ammonia odor from the mouth. Secondary articular lesions such as gout. The cardiovascular system. Firstly, it reacts by increasing blood pressure. Secondly, damage to the heart (muscles - myocarditis, pericarditis - pericarditis). Dull pain in the heart, heart rhythm disturbances, shortness of breath, swelling in the legs, and enlarged liver appear. If the course of myocarditis is unfavorable, the patient may die due to acute heart failure. Pericarditis can occur with the accumulation of fluid in the pericardial sac or the loss of uric acid crystals in it, which, in addition to pain and expansion of the borders of the heart, when listening to the chest, gives a characteristic (“funeral”) pericardial friction noise. Hematopoiesis. Against the background of a deficiency in the production of erythropoietin by the kidneys, hematopoiesis slows down. The result is anemia, which manifests itself very early in weakness, lethargy, and decreased performance. Pulmonary complications. Characteristic of late stages of chronic renal failure. This is uremic lung - interstitial edema and bacterial inflammation of the lung against the background of a decrease in immune defense. Digestive system. She reacts with decreased appetite, nausea, vomiting, inflammation of the oral mucosa and salivary glands. With uremia, erosive and ulcerative defects of the stomach and intestines appear, fraught with bleeding (black feces appear). Acute hepatitis is a frequent accompaniment of uremia. A sore throat. Nipple discharge. Lethargy. Hyperkalemia. Hypercalcemia. Hyperprolactinemia. Hypoglycemia. Hyponatremia. Thirst. Weight fluctuations. Lymphocytopenia. Muscle aches. Metallic taste in the mouth. Colostrum-like discharge from the nipples. Malaise. Neutrophilia. Belching. Lack of appetite. Diarrhea (diarrhea). Constant thirst. Sweating. Taste of acetone in the mouth. Taste in the mouth. Absent-mindedness. Vomit. Intense thirst. Weakness. Cramps. Dry mouth. Tonic convulsions. Nausea. Nausea on an empty stomach. Tremor. Increase in ESR.
general information
Short description
Acute renal failure
(AKI) is a nonspecific syndrome that develops as a result of acute transient or irreversible loss of homeostatic functions of the kidneys caused by hypoxia of the renal tissue with subsequent primary damage to the tubules and edema of the interstitial tissue. The syndrome is manifested by increasing azotemia, electrolyte imbalance, decompensated metabolic acidosis and impaired ability to excrete water. The severity of the clinical picture of acute renal failure is determined by the relationship between the degrees of involvement of tubules, interstitial tissue and glomeruli in the pathological process.
Protocol
"Acute renal failure"
ICD-10:
N17 Acute renal failure
N17.0 Acute renal failure with tubular necrosis
N17.1 Acute renal failure with acute cortical necrosis
N17.2 Acute renal failure with medullary necrosis
N17.8 Other acute renal failure
N17.9 Acute renal failure, unspecified
Causes
The main causes of chronic renal failure are: 1. Diseases accompanied by predominant damage to the glomeruli: acute and chronic glomerulonephritis, diabetic nephrosclerosis, amyloidosis, lupus nephritis, gout, long-term septic endocarditis, myeloma, malaria. 2. Diseases characterized by primary damage to the tubular apparatus: most urological diseases accompanied by impaired urine outflow, congenital and acquired tubulopathies (renal diabetes insipidus, Albright's tubular acidosis, Fanconi syndrome, poisoning with medicinal and toxic substances). 3. Secondary lesions of the renal parenchyma due to vascular diseases: renal artery stenosis, essential hypertension, malignant hypertension. 4. Hereditary malformations of the kidneys and ureters: polycystic disease, kidney cysts, renal hypoplasia, neuromuscular dysplasia of the ureters.
Attention!
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Directory” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.