Ischemic kidney disease: characteristics and symptoms
Renal ischemia is considered one of the most dangerous diseases, as it very often occurs without any symptoms. A large number of doctors are confident that it is still possible to determine the presence or development of kidney disease using certain signs. The problem of the disease lies in the disruption of the blood supply to the organs of the system. The term was first used in 1988, but to this day the group of diseases is still being studied. Modern medicine has only been able to establish the reason why people suffer from the disease. Most often it affects people aged 60+. In this article we will look at all the nuances of ischemia and its treatment.
General information
Ischemic renal disease or ischemic nephropathy was first diagnosed not so long ago, but the group of diseases that are united by this term has not been subject to deep study for a long time. Today it has been established that the pathology is caused by ischemia of the kidney, when an insufficient amount of blood enters it. The reason for this phenomenon is problems with blood vessels. The pathology is more typical for older people, since they are characterized by atherosclerosis, but the disease can develop in any category of patients, including newborns. Every year the disease is diagnosed more often, which is explained by longer life expectancy, especially in developed countries.
General characteristics of kidney disease
Renal ischemia is divided into three types, depending on the speed of disease processes in the patient’s body, including:
- Sluggish form. Characterized by chronic renal failure;
- Form with rapidly progressive kidney failure;
- The most dangerous form is associated with an acute form of deficiency.
The last of the above is observed during exacerbations of sudden occlusion. In this case, the patency in the vessels of the system is impaired, which occurs due to the presence of their stenosis. Risk factors that may arise should be highlighted:
- Thrombosis formation may occur;
- Some patients experience embolization of cholesterol crystals;
- The vessel may also be injured.
The following signs may indicate occlusion:
- The patient may have pain in the abdomen, kidney area and lower back;
- Blood pressure rises sharply;
- The level of body temperature rises;
- There is a dramatic change in blood parameters.
One of the main reasons for the development of insufficiency in humans is a side effect after a course of treatment, for example, against stenosis of the arteries of an organ. This can happen if, with weak kidneys, the patient uses a large amount of antibiotic and anti-inflammatory medications.
Attention! The sluggish form is also called torpid. It is the most common of all existing ones, and even in many situations it is never diagnosed because the symptoms are quite mild.
Myocardial diseases: causes and symptoms of ischemia
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Myocardial ischemia is a pathological condition when the movement of blood to the heart muscle is hampered due to partial or complete blockage of the coronary artery by atherosclerotic plaques, blood clots, or due to severe spasm.
Changes in blood vessels during ischemia
Impaired blood flow is accompanied by a decrease in the volume of oxygen delivered to the heart muscle cells (cardiomyocytes), which they are sorely lacking.
This leads to damage to part of the myocardium. The heart stops actively pumping blood and delivering it to vital organs and the brain. Vascular ischemia also leads to severe disturbances in heart contractions - arrhythmia, increased heart rate or, conversely, a dangerous slowdown in rhythm. A significant narrowing or complete occlusion of the coronary artery leads to myocardial infarction.
Causes of the disease
There are two groups of basic causes of low blood supply and oxygen deficiency.
Pathological changes in the walls of blood vessels, which include:
- Atherosclerosis, which gradually develops with the formation of cholesterol plaques on the vascular walls, which causes a significant restriction of blood flow to the heart muscle cells.
- Spasm of the coronary (heart) arteries is a sharp contraction of the muscles of the vessel wall, during which it narrows, partially or completely blocking the oxygen supply to the heart. Spastic conditions are more common in patients with high cholesterol, systemic lupus erythematosus and hypertension.
- Formation of blood clots. In areas where atherosclerotic plaques are deposited, a thrombus often forms, blocking the lumen of the vessel.
Changes occurring outside the vessels:
- Severe illnesses associated with a sharp drop in blood pressure, which is observed with serious infectious diseases and internal bleeding.
- Tachycardia, atrial fibrillation, hypertrophy (increase in volume) of the heart muscle.
Risk factors
There are certain factors that increase the likelihood of developing ischemia.
Nicotine intoxication leads to damage to the walls of the coronary vessels, causing thrombus formation and slowing down the speed of blood movement.
Diabetes mellitus is accompanied by severe vascular damage. An increased concentration of cholesterol in the blood, deposited on the walls, leads to a narrowing of the arteries, and deposits of triglyceride fats contribute to the development of atherosclerosis.
Regularly high blood pressure gradually weakens the tone of the arteries. A high percentage of body fat increases the likelihood of atherosclerosis and vascular ischemia.
Hereditary factors are important, in which the susceptibility to myocardial ischemia increases.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
General symptoms
Often, myocardial ischemia does not give obvious manifestations and pain (“silent” form) and is determined only on an ECG. There is also a transient form, which quickly develops due to spasm of the cardiac artery as a reaction to physical stress, cold, and strong emotional stress.
There are general symptoms that indicate a malfunction of the heart; in fact, they are signs of angina pectoris:
- painful sensation in the heart area;
- periodic attacks of pressure, burning and compression behind the sternum or pain on the left side, stopping after taking Nitroglycerin (lasting for 15–60 minutes);
- irradiation to the scapula, lower jaw, shoulder and arm;
- signs of heart failure - arrhythmia, profuse sweating, shortness of breath.
Symptoms appear separately and complexly, in different combinations.
Possible complications
Without adequate timely treatment, myocardial ischemia leads to severe complications.
This could be a myocardial infarction. The ineffectiveness of Nitroglycerin, arrhythmia, and elevated temperature indicate the development of this formidable complication.
Possible heart rhythm disturbance. When there is a lack of oxygen, the contraction of the heart muscle occurs with pauses (arrhythmia), abnormally quickly (tachycardia), and slowdown (bradycardia). With the so-called atrial fibrillation, which causes multiple formation of blood clots, the threat to life increases many times over.
Heart failure often develops. Loss of blood supply damages heart tissue. Weakness of the myocardium causes heart failure—the inability of the heart to pump blood and provide oxygen to cells.
Diagnostic examination methods
First of all, a careful examination is carried out, the anamnesis is studied, and the features of heredity are clarified.
For more accurate diagnosis, the following types of studies are used:
- An electrocardiogram that helps to see and analyze the activity, condition and functional abilities of the myocardium.
- A specialized blood test for the amount of cardiac enzymes, which enter the blood much more slowly when the heart muscle is damaged.
- Coronary angiography with the introduction of a contrast agent. When examining angiograms (images), the patency of the coronary vessels and possible narrowing are studied.
- An echocardiogram, the study of which makes it possible to detect the damaged area and identify a weakening of the pumping function of the heart.
- CT scan of the heart - the study determines the manifestations of atherosclerosis of the heart arteries.
- Bicycle ergometry - a stress test with a load on an exercise bike and simultaneous ECG often reveals that myocardial ischemia occurs in a “silent” painless form.
- Holter monitoring, in which a small device records heart rhythm indicators throughout the day.
All diagnostic methods are aimed at a complete study of the heart condition, making an accurate diagnosis and developing the correct treatment regimen.
Tactics and treatment regimen
Therapeutic tactics for myocardial disease include measures to activate blood flow and uninterrupted supply of oxygen to the heart muscle.
Drug treatment
To improve the condition of the heart muscle, effective medications are used, but only with the permission of a doctor.
Products containing acetylsalicylic acid (aspirin): Cardiomagnyl, ThromboASS - reduce blood thickness, preventing the formation of thrombotic clots.
Nitroglycerin, which dilates the coronary vessels, activates blood flow to and outflow from the heart, reducing the need for oxygen.
Beta blockers: Concor, Carvedilol, Labetalol, Nebilet (third generation) - relieve spasms, slow down the heartbeat in case of tachycardia, reduce blood pressure, facilitate the movement of blood to the heart.
Medicines for lowering cholesterol include statins, fibrates, bile acid sequestrants, and niacin.
Calcium channel blockers: Lerkamen, Zanidip, Kalchek, Normodipin, Norvax, Tenox, Felodip - reduce spasm, reduce the load on the heart.
ACE inhibitors: Fosinopril, Enalapril, Captopril - relax the walls of blood vessels, reduce blood pressure.
Surgical methods to stabilize blood flow
In order to activate the blood supply to the myocardium during narrowing of the coronary vessels during angina pectoris or after a heart attack, more intensive treatment is used.
To unblock blocked or spasmed arteries, they resort to surgery. Angioplasty and stenting are done to preserve the normal lumen of the vessel. To do this, a small mesh coil called a stent is inserted into the artery. This operation improves blood flow to the heart and eliminates the most severe manifestations of ischemia.
Coronary artery bypass grafting is a complex operation. It is performed on an open heart and is performed only when several arteries are completely blocked. A graft is created from a healthy vessel, which allows blood to flow through it, bypassing the blocked coronary arteries.
Results
Impaired blood supply to the heart requires immediate medical attention. If you experience a feeling of heaviness in the chest, pain accompanied by arrhythmia, palpitations, shortness of breath, swelling of the lower extremities, the first action is to call a medical team without waiting for the condition to worsen.
Factors in the development of the disease
Although ischemic kidney disease is not expressed in clear symptoms, there are some phenomena that develop the disease. We will now try to find out the factors that form the disease. Bilateral atherosclerosis causes disturbances in blood volume and movement. As a result, significantly less blood flows to the kidney organs.
Important! If only one half is affected, and then only half, then ischemia forms on a healthy organ and reduces the functioning of the entire system.
The disease can form as a result of a violation of the integrity of the aorta in the abdominal cavity or the kidneys. The biggest risk is that if all the vessels become clogged, blood may stop flowing into the body altogether. Due to the stoppage of kidney function, a person’s rate of elimination of toxins and other elements will sharply decrease. It is worth noting that in the acute form of deficiency, a person can die, which is why it is so important to stop the development of the disease.
Consequences and complications
If you do not adhere to treatment, the result of ischemic nephropathy will be the transition to chronic renal failure. This is the most common and expected complication.
The consequences can also manifest themselves in the form of an infarction in the renal tissue. This process represents the death of a tissue area due to oxygen starvation and impaired trophism. One of the known complications is high blood pressure, which is very difficult to reduce.
Main signs of ischemia
Among the main signs that may indicate the presence of kidney disease are:
- Many experience a terminal stage, which occurs in people without organ damage, for example, with scanty urinary syndromes, minimal or obvious proteinuria.
- Most often, ischemia is diagnosed in the elderly population over 60.
- If there is damage to the system by atherosclosis;
- With regular spikes in blood pressure.
Attention! In modern medicine, it has been recorded that coronary disease is present in many people, however, due to poorly expressed symptoms, most cases cannot be diagnosed. In older citizens, it is precisely this that causes organ dysfunction.
Toxic nephropathy symptoms
In case of possible poisoning, the kidney area most often falls into the risk group with the further development of toxic nephropathy. To avoid complications, for example, further development of renal failure, it is necessary to consult a specialist in a timely manner. A high-quality course of treatment will relieve negative consequences.
Toxic nephropathy is damage to the kidney parenchyma and glomerular apparatus.
This manifestation is typical for poisoning with internal or external toxic products or metabolites. In medical terminology, there are two types of disease: specific and nonspecific nephropathy. The first type is associated with poisoning by external toxins, which adversely affects not only the kidneys, but also the functional functioning of the liver. The nonspecific type of disease is caused by hemodynamic disorders.
7 causes of the disease
They release a large number of harmful elements that can harm the body, in particular the kidneys. In addition to some of the harmful substances that a person acquires during his life, some of them can arise independently as a result of injuries or certain diseases.
- Among the factors that provoke the development of toxic nephropathy are taking medications. This is especially true for those drugs that are used to provide emergency medical care and others.
- Medical experts consider microbial organisms to be sources of poisoning. Due to their entry into the blood, microorganisms contribute to a septic condition. The infection process can also occur during a normal transfusion. The development of the disease is provoked by group incompatibility, or the Rh factor of the blood.
- Poisonous mushrooms are especially dangerous; they provoke severe poisoning of the body.
- Chemical substances and salts of heavy metals negatively affect the functional functioning of the kidneys. This category also includes substances of a radioactive nature.
- Among the possible causes of toxic nephropathy are the use of antibiotics or antimicrobial drugs over a long period of time. With prolonged use, they can cause damage to health.
- Poisoning with low quality alcohol or organic poisons. The latter includes acetic acid, or carbon tetrachloride.
- Harmful substances can occur after severe injuries or burns. Tissues begin the process of destruction, as a result of which decay products enter the human blood.
All these reasons are the main provocateurs in the occurrence of toxic nephropathy. Normal kidney function is significantly impaired.
In the future, this leads to complications that become a serious threat to life.
Symptoms
The level of damage depends largely on the type of harmful substance, or its method of entry. The condition of the urinary system plays a significant role. Even with a small amount of toxic substance ingested, the clinical picture becomes more complicated if a person suffers from chronic diseases in this area.
The main symptoms of toxic nephropathy are:
- manifestations, discomfort from shortness of breath;
- pain in the side, in the lumbar region;
- a sharp decrease in blood pressure;
- decrease in the volume of urine excreted.
In cases of exposure to toxic or poisonous particles, symptoms may manifest themselves as follows:
- attacks of vomiting and nausea, possible blood;
- bloating and pain in the abdominal area;
- stomach upset;
- drowsiness, fainting, and overall deterioration of brain activity.
It is believed that toxic nephropathy causes great harm to human health. This is true. If ignored, the disease provokes the development of acute renal failure.
Diagnostics
First of all, a qualified specialist addresses the symptoms, then determines the cause of the disease. In this case, the following necessary procedures are prescribed:
- ultrasound examination of the kidneys;
- blood and urine tests, as well as biochemical blood tests.
These procedures are necessary in order to determine the condition and performance of the kidneys and prescribe an effective course of treatment.
Often, a specialist will prescribe a series of procedures, such as MRI or CT, to confirm the diagnosis.
Treatment method for toxic nephropathy
In order to recover quickly, it is necessary to remove harmful substances. The procedure takes place as quickly as possible. Experts identify the following effective methods.
- Rinsing will be necessary in cases of poisoning with mushrooms or medications.
- Using an antidote. This is a drug that helps remove poison from the body in case of poisoning with industrial or other chemicals.
- Hemosorbium is a method that is based on blood purification using activated carbon.
- There is hemodialysis. This procedure is prescribed in severe cases.
For treatment, diuretics are used, which reduce pulmonary edema (Lasix, Mannitol), as well as polyonic solutions, which normalize the pH level in the blood (sodium bicarbonate is used for these purposes).
Pathogenesis
Depending on the etiology, the pathogenesis of the disease occurs. Due to poisoning, for example, ethylene glycol, swelling of the nephrons occurs.
If the poisoning process occurs due to hemolytic poisons, then the nephrons become clogged. In this case, red blood cells are destroyed.
Taken together, all of the above factors provoke membrane ischemia in the nephrons. Continuous ischemia threatens with irreversible consequences in the form of necrobiotic changes in tangles and tubules.
Toxic poisoning in children
It is worth noting that toxic nephropathy also occurs in children. In this case, you should pay attention to the composition of the urine.
Also, toxic nephropathy manifests itself against the background of a predisposition due to hereditary pathologies. If the mother of the baby in the family was ill during or before pregnancy, the child’s disease may also worsen.
Provocateurs of the disease in childhood can be artificial feeding, or frequent infectious and cold diseases.
Preventive measures
Separately, it is worth noting that no one has canceled first aid. It is necessary to stop the flow of toxic substances into the patient’s body. If poisoning occurs due to vapors, then it is necessary to provide fresh air to the person and immediately remove him from the room. If chemicals get into the stomach, then you need to rinse it urgently. Enemas are also used, and activated charcoal is used.
If a person has no heartbeat or is unconscious, then it is necessary to perform indirect cardiac massage and artificial respiration.
Along with these actions, you must call for medical help.
In preventive measures in industries where there is a high risk of poisoning by harmful substances, people with susceptibility to tumors or kidney damage are not allowed. Most often, such industries include heavy agricultural work and the production of rubber or polymers.
If you work in an industry where there is a high risk of kidney damage, then you need to undergo regular tests (at least once a year). Compliance with hygiene standards and special protective clothing will also have a beneficial effect on your health. If you are observing the initial stage of kidney damage, then it is advisable not to hesitate and change your place of work.
Consequences
If you suspect this disease, you should immediately contact a qualified specialist. Inaction provokes further kidney damage:
- acute renal failure, which is accompanied by a gradual decrease or complete cessation of urine output;
- chronic renal failure, which occurs after severe poisoning.
Any penetration of toxic, harmful substances into the body are possible causes of the development of the disease. In order to avoid complications, it is worth taking the necessary measures as soon as possible.
Thanks to advances in modern medicine, the disease is treatable. It is worth remembering that if you consult a specialist correctly and quickly, there is a great chance of recovery as soon as possible.
Symptoms of coronary artery disease
As mentioned a little above, the disease does not have pronounced symptoms, however, it can manifest itself in a number of other characteristics. For example, in the acute form of insufficiency, the patency of blood vessels in the system is destabilized, which manifests itself in some symptoms. Additional risk zones may form:
- Vessels may be injured, even to the point of rupture;
- Some develop thrombosis, which can lead to death;
- Cholesterol crystals also clog the blood vessels.
Plus, the disease can be diagnosed based on the symptoms of blockage of blood vessels, including:
- Pain in the lumbar and abdominal region;
- In most cases, blood pressure levels increase;
- There is an increase in normal temperature;
- Changes are also diagnosed in the analysis
Kidney failure develops rapidly and is caused by blockage of the renal artery. When the disease is present, other health problems are often observed. In general, the symptoms resemble the course of the disease vasculitis. Thus, during ischemia, disturbances are also observed in other systems. For example:
- In the kidneys, the level of creatinine in the blood and blood pressure increases;
- Problems with the skin are very often observed, for example, nodular forms of erythema, cyanosis, necrosis appear on the toes;
- The nervous system is also affected, in some situations paralysis occurs;
- The patient often suffers from pain in the abdomen, feels nauseous, and vomits.
Chronic abdominal ischemia
This disease develops when the blood supply to the digestive organs is disrupted. Chronic abdominal ischemia is also called “abdominal toad.” The disease is very rare compared to the ischemia described above. The cause is the same atherosclerosis. Impaired blood supply leads to changes in the motor and secretory activity of the organ. The consequence of the disease can be an infarction of the intestinal wall.
Symptoms of the disease in the compensatory stage are expressed by pain after a heavy meal in the left iliac or epigastric region, aggravated by physical or nervous stress.
During the period of subcompensation, constipation or diarrhea, bloating and belching occur. The patient loses weight.
During the decompensation stage, diarrhea intensifies, the body becomes dehydrated, and exhaustion develops.
Features of diagnosis and therapeutic treatment
Modern medicine uses a huge variety of different techniques to help diagnose the presence of a disease such as renal ischemia. Doctors conduct a detailed analysis of kidney function, the actual state of the organ’s muscle tissue, and vascular performance. They are also able to measure blood flow and its level of saturation of all cells of the renal system. The most popular diagnostic procedures include the following:
- The presence of the disease can be detected using a radioisotope renograph;
- When performing duplex ultrasonography;
- Using spiral computed angiography;
- Nuclear magnetic resonance can also be considered an effective diagnostic method.
Attention! Most diagnostic results show an accurate and reliable result. Its probability is 85-100 percent.
It is worth noting that this disease makes itself felt already in the later stages, when renal failure forms. During this period, the body is oversaturated with toxins, which impairs the functionality of the organ. For this very reason, the course of therapy starts with blood cleansing procedures. Treatment cannot get rid of the problem itself, so it can only eliminate unpleasant symptoms. In order to improve the functional functioning of the kidneys, it is necessary to get rid of the problem of blood supply to the system.
In the early stages of the disease, when changes occur in the tissues of the kidneys, it is possible to get rid of arterial stenosis through surgery. Plus, in modern pharmacology there are drugs that slow down renal failure. But, do not forget that the consequences of the disease can be very serious, so it is better to treat ischemia immediately.
Diagnostics
There is no generally accepted algorithm and sequence of actions for diagnosing ischemia. Based on complaints and possible causes that may lead to ischemia, the doctor may prescribe the following types of examinations:
- General blood analysis.
- Blood chemistry.
- General urine analysis.
- Zimnitsky's test.
- Ultrasound examination of the urinary system.
- Duplex study of renal vessels.
- Angiographic examination of blood vessels.
- Magnetic resonance angiographic study.
- Scintigraphy.
- Positron computed tomography.
During these examinations, the condition of the vessels, features of blood flow, as well as changes in the parenchymal component of the kidneys and their functional ability are clarified.
Renal ischemia: causes, symptoms and methods of treatment
Kabardino-Balkarian State University named after. HM. Berbekova, Faculty of Medicine (KBSU)
Level of education – Specialist
State educational institution "Institute for Advanced Medical Studies" of the Ministry of Health and Social Development of Chuvashia
Among other types of ischemic damage to internal organs, renal ischemia occupies one of the leading positions in terms of incidence, which is facilitated by various external and internal factors: congenital kidney pathologies, acquired and chronic diseases of the body. The symptoms of the pathology are quite characteristic, which makes it possible to identify it in a timely manner and prevent the possibility of worsening the disease.
Treatment tactics
Patients with suspected renal infarction require emergency hospitalization. Patients (especially those with hematuria) are prescribed strict bed rest.
In a hospital setting, narcotic analgesics are prescribed to relieve pain. Disorders of the blood coagulation system are corrected by taking direct anticoagulants. In the absence of hematuria, thrombolytics are prescribed, and if hematuria is present, hemostatic agents are prescribed.
In case of renal infarction, bed rest is indicated
In the early stages, it is possible to restore blood flow by surgically removing the thrombus or embolus. Angioplasty may be required in the future. In the presence of profuse hematuria, arterial hypertension, which do not respond or respond poorly to conservative therapy, as well as in case of total organ infarction, nephrectomy is resorted to.
After a kidney tissue infarction, in some cases long-term (often lifelong) use of antiplatelet agents is indicated.
The goal of treatment for renal infarction may vary depending on the stage and course of the pathological process. First, the patient’s condition is restored and blood flow in the organs of the urinary system is normalized.
This reduces the risk of developing complications of ischemia.
After this, bleeding and manifestations of general intoxication of the body are eliminated. They also try to preserve the functionality of the part of the kidney that is not affected by the infarction.
To do this, prescribe medications with the opposite effect (hemostatics, anticoagulants).
The list of medications for conservative treatment includes:
- painkillers. Prescribed if the pain is intense. Sometimes you have to take potent narcotic analgesics;
- thrombolytic drugs. They are used if it is necessary to eliminate a blood clot in the lumen of a vessel and normalize blood flow. If blood is detected in the urine, then these drugs are prohibited for use;
- hemostatic drugs. Indicated in cases of severe hematuria and renal bleeding;
- anticoagulants. Prescribed to prevent blood clots. These medications cannot be taken without a coagulogram;
- antiplatelet drugs. In acute cases of the disease, they are rarely prescribed. Prevents relapses and complications.
A surgical operation is performed to restore the patency of the main arteries to normalize renal blood flow.
If necrotic changes are detected during late diagnosis, nephrectomy may be performed. It is important that the second kidney is healthy.
Ancillary procedures include hemodialysis, diuretics and antihypertensive drugs.
First medical aid for a heart attack is to improve the blood supply to the heart, prevent thrombosis, and maintain the vital functions of the body. Further treatment aims to quickly scar the necrosis and achieve the most complete rehabilitation.
The success of rehabilitation largely depends on how responsibly the patient takes the prescribed treatment and recommendations for lifestyle changes. In order to prevent relapse (repeated heart attack develops in more than a third of cases), it is necessary to give up bad habits, follow a diet, ensure adequate physical activity, adjust body weight, control blood pressure and cholesterol levels in the blood, and also avoid overwork and psycho-emotional stress - then is to eliminate all factors contributing to the development of myocardial infarction.
General description and pathogenesis
Ischemic kidney disease is expressed in a deterioration in the blood circulation process, which leads to a significant decrease in the amount of blood entering the organ, resulting in impaired nutrition of the kidney. A lack of incoming oxygen and nutrients can cause a deterioration in the condition of the kidney tissue, which, when the pathological process starts, can provoke necrosis. Hypoplasia of the arteries and tissues of the kidney, hereditary predisposition to renal failure, mechanical effects on the organ - all this can cause pathology of the kidney with a deterioration in its blood supply and transition to ischemia.
Even minor damage to the only blood vessel in the kidney can lead to manifestations of ischemic damage, which causes further development of the pathology. The pathogenesis consists of an intensification of the bilateral atherosclerotic process, which leads to a significant narrowing of the lumen of the vessel. Leading to a gradual weakening of the speed of blood movement through the veins and arteries, atherosclerosis and excess cholesterol in the blood can lead to serious disturbances in the functioning of the kidneys, which can provoke insufficiency of their work - this condition is considered dangerous both for the health and for the life of the patient.
The speed of transition of the disease from the initial stage to a more advanced and then advanced stage occurs very quickly, which should be taken into account when diagnosing it. The treatment method for the initial stage of the disease is quite simple and highly effective, therefore the start of treatment should be as quickly as possible from the moment the kidney pathology is identified.
Cerebral ischemia
Cerebral ischemia develops due to insufficiency of cerebral circulation, which provokes oxygen starvation of the organ. The acute course of cerebral ischemia has an incoming nature of an ischemic attack, the chronic form develops over a long period of time and causes serious disturbances in the brain.
The main causes of cerebral ischemia include arterial hypertension and atherosclerosis. There are additional risk factors for the development of the disease, such as venous pathologies, vascular compression, cardiovascular diseases, vascular pathologies and hereditary angiopathy, diabetes mellitus, systemic vasculitis, blood diseases and cerebral amyloidosis.
With cerebral ischemia, the symptoms of the initial stage are expressed by memory deterioration, disruption of the nervous system, and increased fatigue. The patient may experience increased nervous excitement and mood swings, and sleep disturbances.
As cerebral ischemia develops, it causes the patient dizziness, nausea, vomiting, impaired speech and vision, and fainting.
In the absence of the necessary treatment, the disease goes through three stages of development, ending with changes in memory, speech, thinking and often leads to dementia or stroke.
Chronic cerebral ischemia ranks first among cerebrovascular disorders.
Causes
Renal ischemia occurs, as mentioned above, due to a significant deterioration in the quality of blood circulation, which entails a decrease in the required intensity of supply of oxygen and nutrients to the kidney tissue. Heredity, predisposition to renal vascular damage and general vascular contamination, expressed in the development of atherosclerosis, are the most common reasons for the occurrence of renal ischemia.
There are also a number of provoking factors that, if repeated for a long time, can provoke disturbances in the blood supply to the kidney tissue. These include:
- systemic vasculitis, which impairs blood circulation in the kidney tissues;
- thromboembolism;
- hypoplasia of the arteries of the kidneys or aorta;
- fibromuscular dysplasia of blood vessels in kidney tissue.
Causes
The etiology of renal ischemia is congenital or acquired.
Among the main factors that provoke the disease during life are:
- atherosclerosis (accumulation of cholesterol plaques on the walls of blood vessels);
- thromboembolism - blockage of the lumen of the vein;
- mechanical damage to the kidneys or adjacent tissues;
- frequent vasculitis (inflammation);
- cholesterol embolism in the arteries of the kidneys.
Among the causes of the acquired form in adults are also the consequences after warm ischemia. Warm renal ischemia is a manipulation that is a standard procedure for laparoscopic surgery.
Kidney nephropathy in newborns is characterized by damage to the tubules and glomeruli due to poor blood supply. The disease occurs due to fetal hypoxia during intrauterine pneumonia or sepsis. Ischemic nephropathy is found in infants and with hypovolemia - large blood losses during childbirth. A pregnant woman's use of strong antibiotics also has a negative impact.
Stages of the disease
There are three main stages of development of the pathology in question, each of which has its own characteristic symptoms and requires a certain type of therapeutic intervention:
- The chronic form, which has a minimal number of obvious signs of the course and worsening of the disease. In the chronic form of renal ischemia, the disease develops sluggishly, and its detection is difficult due to the difficulty of identifying symptoms.
- An acute form in which the symptoms are very obvious and allow you to quickly diagnose the current pathology. Delaying the onset of therapeutic effects is fraught with the development of complications, therefore, at the acute stage, the diagnosis should be clarified as quickly as possible and treatment should begin, tailored to the individual characteristics of the patient’s body.
- A rapidly progressive form, which is characterized by the appearance of dark bruises and bruises on the skin, a feeling of nausea, vomiting, and the initial stage of necrosis of the fingers of the lower and upper extremities. When analyzing blood, a change in its composition is noted, and blood pressure may jump sharply.
The listed stages of the disease have their own characteristic features of the course and require a rapid therapeutic response, which avoids aggravation of the pathological process in the kidney tissues.
Identification of the disease most often occurs in old age, when the function of the adrenal cortex is weakened and organic damage accumulates. However, at present, the initial stages are increasingly observed in younger people, so regular preventive examinations should be carried out to identify any abnormalities in the kidney tissue.
Hydrocalycosis of the kidney
Have you been trying to cure your KIDNEYS for many years?
Head of the Institute of Nephrology: “You will be amazed at how easy it is to heal your kidneys just by taking it every day...
Read more "
Hydrocalycosis of the kidneys is now rightfully considered a common problem related to nephrology. After all, pathologies of this paired organ are common today, and this happens in people of different ages and social status. But what is kidney hydrocalycosis, how to treat the disease? This pathology is a violation of the release of urine from the fluid-filtering organ, which causes expansion of the base of the pelvis and also leads to increased pressure on the renal tissue. This condition not only causes disruption of the functioning of the urinary system, but also brings discomfort to the patient. Therefore, it is important to treat the disease as soon as symptoms are detected, which is carried out by taking medications, as well as following traditional recipes.
Hydrocalycosis of the kidney is a serious pathology that impairs the functioning of all organs related to the urinary system. Doctors say that today disease of only one kidney, located on the right or left, is common. However, a bilateral type of disease can also be diagnosed in a person - most often it appears at a time when the patient did not treat the pathology that had just arisen, and over time it turned into an advanced form.
Currently, the disease appears as a result of:
- hydrocalycosis of the left kidney appears as a result of a long absence of outflow of urine that passes through the organ;
- hydrocalycosis of the right kidney is also associated with the fact that urine is retained, as well as with the expansion of the pelvis or calyx of the organ.
It is somewhat more difficult to notice bilateral hydrocalycosis, since many compare its appearance with a cold in the back or other problems with the lower back.
According to modern statistics, today about 60% of all patients with hydrocalycosis are faced with the development of right-sided disease, 30% with left-sided pathology, and only 10% suffer from bilateral kidney damage. Diagnosing the disease is not difficult, because after taking tests and performing an ultrasound (ultrasound), the doctor will detect stagnation of urine, which will allow him to prescribe the correct treatment.
Kidney hydrocalycosis is especially dangerous in children, so it is important to pay attention to all the causes of this disease and try to eliminate them from life.
These reasons include:
- urolithiasis;
- narrowing of the ureter that occurs at a pathological level;
- nephroptosis;
- urolithiasis;
- renal failure;
- advanced prostatitis;
- tuberculosis that does not develop in the respiratory system;
- injuries localized to the lower back;
- polyps or neoplasms on the intestines;
- malignant lesions of the kidneys or urinary organs and tract.
The development of hydrocalycosis of the kidneys most often appears as a result of a long absence of treatment for these diseases, so a person should not avoid therapy, as well as carry out treatment on their own, because this can cause unpleasant diseases and complications, which include the appearance of hydrocalycosis of both kidneys. It is worth noting that if the patient ignores treatment for this disease, he will soon need surgery.
Often, hydrocalycosis of both organs appears in a healthy pregnant woman, which is associated with the peculiarities of the course of pregnancy (low position of the baby), as well as the peculiarities of growth of the uterus in one direction. However, in such a situation, the disease does not require treatment - the doctor only needs to regularly monitor the patient’s health. After childbirth, the disease usually goes away on its own.
Doctors say that the course of hydrocalycosis of the kidneys, which is treated as signs of the disease are detected, is usually associated with a deterioration in urinary patency. Impaired outflow of urine leads to involuntary expansion and increase in the diameter of the pelvis, which ultimately puts pressure on the nephrons and tissues of the organ. Because of this, they are also involved in the inflammatory process, bringing a person many unpleasant symptoms.
Clinical picture of the disease
With the diagnosis of hydrocalycosis of the kidney, what it is has now become clear. But how can we determine the course of the disease in an adult or child? To do this, you should monitor the body and not “miss” the development of symptoms of pathology. Most often, it is difficult not to detect its occurrence, since it significantly changes the functioning of the body and brings discomfort to the patient. However, sometimes the disease may not reveal itself through symptoms for a long time - in this case, it is possible to identify the course of hydrocalycosis only after special tests are carried out.
If the size of the affected organ changes significantly upward, a person will notice the development of the following signs:
- a sharp increase in temperature up to 40 degrees;
- severe deterioration in general condition;
- occasional chills;
- nausea leading to vomiting;
- deterioration or complete loss of appetite;
- changes in the smell, color and amount of urine;
- frequent release of a small portion of urine, which goes away with pain;
- pain in the lumbar region where the ureters are blocked;
- presence of blood in urine.
The severity and duration of these symptoms directly depend on the causes of the disease, so they should be identified by the doctor first.
Complications of hydrocalycosis and its diagnosis
When confirming the diagnosis, the doctor diagnoses hydrocalycosis of the kidneys, which means a serious disease, the absence of treatment of which leads to the rapid development of unpleasant and often dangerous complications.
These include:
- hydronephrosis - rapid and aggressive expansion of the pelvicalyceal system (pyelocalyceal system), as well as the course of tissue destruction;
- urosepsis - the development of acute inflammation in the urinary organs caused by the development of infection in them;
- renal failure, occurring in both normal and advanced forms.
It is for this reason that this diagnosis should not be ignored, since a completely affected kidney requires immediate removal.
Diagnosis of the disease does not contain any dangerous or complex procedures - all diagnostic methods are quite easy and fast.
The doctor will prescribe the following comprehensive examination to the patient:
- Laboratory tests. These include urine and blood tests to assess the type of disease and the possible cause of its development.
- Ultrasound. Using computer graphics, doctors will be able to determine whether the patient has congestion in the kidney and dilation of the pelvis or calyx. In addition, with the help of this study it is possible to accurately understand the cause of the disease, as well as assess the degree of inflammation of the organ.
If these diagnostic methods cannot show the complete picture of the disease, the doctor will prescribe the patient radiation diagnostic methods, namely:
- MSCT (multispiral computed tomography);
- angiography.
At the same time, the patient should not ignore the diagnostic procedures of the attending physician, since only with their help will it be possible to accurately diagnose and prescribe the correct treatment. You especially shouldn’t skip procedures when it comes to your child’s health.
The doctor, based on the person’s current condition, prescribes one or another procedure. When discharging them, he must interview the patient, find out the symptoms and the possible cause of the development of the pathology. In addition, he should ask whether the patient has other diseases of the urinary system.
Treatment of hydrocalycosis of the kidneys
If a person has been diagnosed with hydrocalycosis of the kidneys, treatment should be carried out not only for unpleasant symptoms, but also to eliminate the underlying cause that caused the disease.
Therapy for this pathology today is carried out in two ways: conservative and surgical.
The folk way to cleanse the kidneys! Our grandmothers were treated using this recipe...
Cleaning your kidneys is easy! You need to add it during meals...
In the first case, the patient will be prescribed the following groups of medications:
- antispasmodics (these include Spazmalgon, No-shpa, Papaverine, Riabal);
- painkillers (Ibuprofen, Movalis);
- diuretics (these include both medicines and folk recipes);
- antibacterial compounds necessary for prevention (Palin, Nitroxoline);
- uroseptics created on a natural basis (Canephron, Urolesan, Hofitol).
The dosage and type of drug are prescribed only by the doctor, taking into account, in addition to the test results, the patient’s age and weight.
The second important stage of the treatment method is to exclude and prevent the consequences of the disease.
These include:
- treatment and prevention of urinary diseases (cystitis, pyelonephritis, etc.);
- improving the nutrition of the kidneys and normalizing blood circulation in them (this is done with the help of drugs Pentoxifylline or Trental);
- hemodialysis when signs of failure develop;
- following a special diet prescribed by a doctor.
To normalize the functioning of a damaged paired organ, the patient may be prescribed:
- nephrectomy - complete removal of the diseased organ;
- nephrotomy - dissection of the kidney cavity for its drainage;
- nephrostomy - normalization of urine flow in the lumbar system, carried out using an opening in the lower back.
Any method of surgical treatment described above is prescribed only by a doctor after a complete examination of the patient and diagnostic measures.
Symptoms
The most characteristic manifestations of an ischemic condition of the kidneys, in which pathologies of the adrenal cortex are detected, can be considered the following:
- a feeling of squeezing in the kidney area, especially when making sudden movements;
- nausea;
- crawling and tingling sensation on the skin, especially in the lower and upper extremities;
- bruising of the skin;
- sudden jumps in blood pressure.
Restriction of the adrenal cortex, which is most often observed upon reaching the age of 55-65 years, is often accompanied by changes in the condition of the kidney tissue. Therefore, monitoring your own health allows you to timely identify both pathologies of the adrenal cortex and negative changes in the functioning of the kidneys and the condition of their tissues.
Ischemic nephropathy of newborns
Newborn children often experience problems with their kidneys, which sometimes develop into kidney failure or inflammation of the urinary ducts. Almost every case of renal ischemia leads to dysfunction of the organ. In infant nephropathy, the renal glomeruli and tubules are damaged, which is caused by impaired blood microcirculation in the kidney area. In infants, the disease may progress in 3 stages:
- 1 - there are practically no symptoms, a blood test does not show critical creatinine levels, weight loss, dehydration or minor manifestations of problems with the cardiovascular system are possible;
- 2 - the concentration of creatinine increases, moderate swelling or slight swelling of the skin appears, minor hemorrhages occur on the mucous membranes and skin, etc.;
- 3 - severe swelling occurs, fluid accumulates in the cavity, painful lumps form under the skin, necrosis of the skin, etc.
Diagnosis and treatment methods
Detection of the ischemic state of the kidneys and disturbances in the functioning of the adrenal cortex can be carried out using both a number of laboratory diagnostic methods and instrumental research techniques.
Laboratory options for studying the functioning of the kidneys and the degree of damage to their tissues include:
- blood tests - biochemical and general tests;
- urine test (plus urine test according to Zimnitsky);
- lipid profile;
- ratio of red blood cells to blood plasma.
Instrumental methods for identifying ischemic conditions are the following:
- ultrasound examination of the chest and kidney area;
- electrocardiogram;
- echocardioscopy;
- Doppler study of the kidneys.
The listed tests are prescribed after passing through a surgeon, nephrologist, therapist, and also an ophthalmologist. A comprehensive examination allows you to obtain the most complete picture of the current disease and create a treatment plan that will be especially effective.
Treatment and prevention
Since this kidney pathology is most often detected in the late stages of the disease due to the almost complete absence of symptoms in the early stages of the process in the kidney tissues, treatment consists of eliminating the consequences of renal failure.
Drug treatment brings a pronounced positive result when using drugs prescribed by a nephrologist at an early stage of the disease. The most commonly used medications when diagnosing any stage of the ischemic process in the kidneys include drugs that normalize kidney function, eliminate congestion in them and stimulate blood circulation in the kidney tissues.
If surgical intervention is necessary, a roundabout route of blood supply to the kidney is created, and if there is stenosis of a vessel in the kidney tissue, surgery to remove a stent is used.
As a preventive measure for such a pathology as ischemic kidney damage, one should mention the exclusion of such provoking factors as an excess of salty, smoked, spicy foods in the diet, giving up bad habits such as smoking and excessive consumption of alcoholic beverages, and taking measures to lose extra pounds. Regular examination by doctors and careful attention to one’s own health can prevent the worsening of any kidney pathology and prevent the disease from progressing to a more advanced stage.
Ischemia: causes, forms, manifestations and course in various organs, treatment, prognosis
Ischemia is a special pathological process that is characterized by insufficient supply of arterial blood to organs and tissues. It is not an independent disease, but accompanies a variety of pathologies as its root cause and the main pathophysiological mechanism of development.
Ischemia is the basis of cerebrovascular pathology, when the brain experiences a lack of nutrition, and coronary heart disease is a whole group of diseases that arise solely due to a lack of arterial blood supply to the heart.
The cause of ischemic lesions is, first of all, a vascular factor, and it is not so important whether the vessel is clogged from the inside or compressed from the outside, and in some cases irreversible changes occur in the vascular walls themselves, leading to a lack of blood flow. The picture that is observed in organs during ischemia is largely stereotypical and is associated primarily with hypoxia.
The concepts of hypoxia and ischemia should not be confused. Hypoxia is a broader phenomenon that reflects a lack of oxygen due to external or internal causes, while the vessels may be passable and quite capable of delivering the required volume of blood. With ischemia, there is often a local problem that leads not only to hypoxia, but also to a variety of other metabolic disorders. In addition, hypoxia is considered reversible, while ischemia is potentially dangerous due to the development of a heart attack with the death of a tissue area.
Different organs respond to ischemia differently. This is due to the characteristics of the blood supply and functional activity of the tissue. For example, bones and cartilage are able to withstand a lack of arterial blood for quite a long time without changing or causing symptoms of pathology, while the brain, heart and kidneys are extremely vulnerable and are the very first to feel the ischemic effects.
The severity of ischemia and its consequences depend on the rate of progression of the disorder, the type of tissue, the degree of obstruction of the vessel, the general condition of the body, but in all cases suspicious of ischemic processes anywhere in the body, a thorough examination of the patient is necessary, and often a serious treatment.
Types of ischemia and the changes it provokes
Ischemia can be acute or chronic. Its duration determines the nature of the structural restructuring of the tissue, and the depth of the changes will depend on the sensitivity of the tissue to the lack of oxygen and the degree of insufficient blood supply to the organ.
The duration and speed of development of the pathological process are important prognostic factors for anemia. The faster the overlap occurs, the deeper the damage will be in the tissue, since collateral (bypass) blood flow pathways do not have time to turn on in a short time. A long-term ischemic process leads to irreversible sclerotic and dystrophic changes, in contrast to short-term ischemia, which can stop at the subcellular level.
The changes that develop in tissue under ischemic conditions are caused by insufficient oxygen supply. This can be intracellular damage during short-term and superficial ischemia or deep destructive processes resulting in organ infarction.
Acute ischemia causes dystrophy and necrosis, which are preceded by changes at the ultrastructural level - destruction of cell components, slowing down the activity of enzymes and biochemical reactions. This type of anemia is considered a pre-infarction condition, followed by the heart attack itself.
If ischemia is prolonged, atrophy begins in the tissue, and constant hypoxia activates connective tissue cells, fibroblasts, which begin to actively form collagen. The consequence of prolonged ischemia is sclerosis.
Among the causes of ischemia of various organs are:
- Thrombosis and embolism;
- Atherosclerosis;
- Arrhythmias;
- Arterial hypotension and shock;
- Compression from the outside by a tumor, foreign body, ligature;
- Congenital anomalies of arterial development;
- Focal vasospasm.
There are several types of ischemia:
- Angiospastic;
- Obstructive;
- Compression;
- Redistributive.
Angiospastic ischemia is associated with spasm of arterial vessels, which can be caused by pain, the effects of medications, cold, emotional experiences or injuries, infections, fever and many other reasons. This ischemia is transient and, as a rule, short-term, but under pathological conditions the spasm can be quite long-lasting and even cause a complete stop of blood flow.
Angiospastic vascular ischemia most often appears when large arteries narrow - coronary arteries in the heart, one vessel from paired organs with irritation of the opposite artery (kidney, for example). A serious threat is posed by brain tumors, strokes, and toxic damage to nervous tissue, which can lead to increased activity of the vasomotor center and subcortical structures with the development of widespread vasospasm and ischemia in the tissues.
The obstructive type of ischemia is a consequence of blocking the lumen of the vessel from the inside. The cause of obstruction may be a thrombus, an embolus, sclerosis of the arterial wall or its inflammation, or an atherosclerotic plaque. Obstruction by thrombotic masses is often accompanied by vascular spasm, and spasm can provoke subsequent thrombosis or embolism.
Compression anemia develops due to compression of an arterial vessel by a neoplasm, ligature, exudate, or a tourniquet. Compression of the artery can also be caused by a foreign body acquired during trauma or a gunshot wound.
The redistributive type of anemia occurs after anemia. For example, fluid has accumulated in the abdominal cavity. After the contents are removed, the vessels of the abdominal cavity expand sharply and are filled with arterial blood, while other organs will experience a lack of it due to uneven distribution. This type of ischemia is associated with cases of fainting after removal of ascitic fluid, which are caused by a temporary lack of arterial blood supply to the brain.
A relatively harmless type of ischemia is considered to be angiospastic, which can be eliminated with treatment or will go away on its own, and one of the most dangerous is obstructive, when the entire vessel is completely blocked in a short time, and necrosis develops in the tissue.
The outcome of ischemia and its significance for the body are determined by the organ in which the disorder occurred. More severe consequences are typical for anemia of vital organs - heart, brain, kidneys. Ischemia of the spleen, respiratory organs, and liver is more easily tolerated, which, in turn, is more severe than anemia of bones, cartilage or muscles. The more active the biochemical processes in tissues are, the more sensitive it is to the lack of arterial blood flow.
The degree of ischemic-dystrophic changes is also influenced by the development of the organ’s own vascular network. For example, the brain or heart are not sufficiently supplied with collateral blood flow pathways, so ischemia in them quickly turns into necrosis. The lungs and liver essentially have two sources of blood supply and abundant vascular collaterals, so ischemia in them is less pronounced.
Another factor on which the course of ischemia depends is the initial functional state of the tissue: the higher the level of metabolism, the greater the need for oxygen, and with its deficiency, degeneration is stronger and necrosis is more likely.
Manifestations of ischemia in various organs
Ischemia is characterized by a number of signs:
- Pallor of the tissue due to lack of arterial blood;
- Local decrease in temperature (for example, the skin becomes cool with severe vasospasm);
- Paresthesia - numbness, sensation of “pins and needles”;
- Pain - associated with the accumulation in the ischemic zone of under-oxidized metabolic products, lactate, free radicals that irritate nerve endings;
- Reduction in the size of the organ, its compaction in the chronic course of the pathology.
Symptoms of ischemia depend on its duration, rate of development and functional characteristics of the affected organ. As a rule, the pain syndrome associated with hypoxia and the accumulation of acidic metabolic products comes first. In some cases, the function of the organ is disrupted, which affects the general condition of the body.
Myocardial ischemia
The most serious changes are caused by anemia of vital organs. The lack of arterial blood supply to the heart muscle underlies coronary heart disease, the morbidity and mortality rate of which is close to those from cancer pathology.
Ischemia in the heart most often develops due to an atherosclerotic process in its arteries, that is, it is obstructive in nature. Vasospasm and thrombosis due to plaque rupture significantly aggravate the degree of blood flow disturbance.
Chronic ischemia in the heart provokes growth in its muscle layer of connective tissue under the influence of constant hypoxia - diffuse atherosclerotic cardiosclerosis is formed. At the same time, atrophic changes in cardiomyocytes increase, the heart becomes flabby, its contractility decreases, and heart failure develops.
Symptoms of cardiac ischemia, which has a chronic and long-term course, are pain in the heart, spreading to the area of the left arm and shoulder blade, various cardiac arrhythmias, weakness, shortness of breath, decreased performance and resistance to physical activity are common. One of the most common forms of chronic coronary heart disease is angina, which is often accompanied by various arrhythmias.
As ischemic-dystrophic and sclerotic changes in the heart deepen, signs of its dysfunction appear and intensify - shortness of breath worries not only during exercise, but also at rest, diffuse cyanosis of the skin develops, fluid accumulates in the body cavities, and the liver enlarges.
Acute myocardial ischemia due to obstruction of the coronary arteries by a plaque or thrombus can very quickly turn into necrosis - a heart attack will develop. A patient with this disease experiences severe burning pain in the chest, anxiety, fear of death, increased shortness of breath, and possible rhythm disturbances up to severe blockades and ventricular fibrillation.
The consequences of cardiac ischemia are considered to be diffuse and focal cardiosclerosis. The first is the outcome of chronic ischemia, the second remains after a heart attack. Subsequently, heart failure occurs.
Cerebral ischemia
Ischemic changes in the brain underlie cerebrovascular pathology, which, along with ischemic heart disease, leads in the number of severe complications and deaths. The cause of cerebral ischemia is usually atherosclerotic changes and arterial hypertension.
In atherosclerosis, fat deposits create a mechanical obstruction to blood flow, resulting in obstructive ischemia. If the plaque ruptures, and this often happens in the extracranial segments of the brachiocephalic arterial trunks, the fat embolus will cause blockage of the cerebral arteries, and ischemia will develop in the brain tissue, which will quickly turn into a focus of necrosis (stroke).
Arterial hypertension promotes persistent and irreversible changes in the vascular walls, which become saturated with plasma proteins and grow with connective tissue, which leads to stenosis and reduced delivery of arterial blood to the brain.
Cerebral ischemia can be chronic, and then they talk about discirculatory encephalopathy, or acute in the form of a stroke (cerebral infarction). Chronic ischemia is accompanied by symptoms such as:
- Decreased memory, forgetfulness, which older people are prone to;
- Decreased intellectual abilities, difficulty concentrating;
- Changes in behavior and psyche - irritability, emotional lability, tendency to depression;
- Sleep disorders - insomnia, daytime sleepiness.
The most important symptom of cerebral ischemia is considered to be headaches associated with metabolic disorders due to lack of oxygen. Dizziness and noise in the ears or head are also possible.
Acute cerebral ischemia is a severe complication of atherosclerosis and hypertension, in which complete obstruction of the arterial vascular bed occurs. As a result of such ischemia, a heart attack (stroke) develops, which is manifested by a variety of neurological symptoms - paralysis and paresis, impaired sensitivity, speech, and the functioning of many internal organs; in severe cases, coma occurs, cerebral edema increases and the patient dies.
Ischemia of the kidneys and intestines
The kidneys are another organ that reacts very sharply to any manifestations of a lack of arterial nutrition. Ischemia in the kidneys can develop due to vascular damage by atherosclerosis, congenital developmental anomalies in the form of local narrowing, thrombosis, and compression by a tumor. An important unfavorable factor is the high probability of spasm of the renal arteries when the vessels of the opposite side are damaged. In other words, with ischemia in one kidney, almost inevitably the same changes will develop in the second due to a reflex spasm of its vessels.
Chronic ischemia in the renal parenchyma causes pronounced dystrophic and sclerotic changes, one of the main symptoms of which is secondary hypertension, which is difficult to correct with antihypertensive drugs. Patients will complain of headaches, flashing spots before the eyes, visual disturbances, nausea, dizziness, episodes of arrhythmia, increasing against the background of hypertensive crises.
Acute ischemia resulting in renal infarction is observed with thromboembolism of its vessels. Symptoms include hypertension and pain in the lumbar region. Total ischemia of the cortical layer of both kidneys occurs with severe hemocoagulation disorders - disseminated intravascular coagulation syndrome, severe hypotension, shock. In these conditions, the kidneys stop producing urine, and the symptoms of acute organ failure increase.
Chronic intestinal ischemia appears with atherosclerosis of the mesenteric arteries, when blood flow is partially preserved, but insufficient. Patients' complaints include abdominal pain, indigestion, and general weakness.
Acute intestinal ischemia due to thrombosis of the arteries supplying it can very quickly lead to necrosis (infarction) of the intestine, which is characterized by the highest mortality. Abdominal pain and signs of intestinal obstruction occur, body temperature rises, and peritonitis develops, requiring emergency surgical care.
Signs of ischemia can be found in other organs, and its symptoms can be expressed to varying degrees:
- Thus, anemia in the retina of the eyes is accompanied by a decrease in vision, but its complete loss is also possible with retinal infarctions.
- With ischemia of the lower and upper extremities, pain is inevitable, the skin turns pale, sensitivity disorders occur, and in severe cases, gangrene occurs.
- Angiospasm in the vessels of the skin is accompanied by pallor and coldness of the body, and severe ischemia can lead to focal necrosis. Long-term anemia of the skin and soft tissues leads to trophic changes - peeling, thinning of the skin, hair loss, cyanosis, deeper changes lead to the formation of trophic ulcers.
Ischemic kidney disease (renal ischemia, ischemic nephropathy, vascular nephropathy)
Causes of the disease
Ischemic nephropathy is a group of diseases based on renal ischemia, which developed as a result of primary damage to renal vessels of various diameters with disruption of their patency and severe diffuse depletion of renal blood flow, leading to a decrease in filtration function and progressive nephrosclerosis.
The term “ischemic nephropathy” appeared in 1988, but for a long time this group of kidney diseases remained insufficiently studied. To date, the cause of ischemic kidney disease has been identified. This is atherosclerosis, which leads to stenosis and obstruction of the patency of large vessels supplying the kidney with blood. The majority of patients with renal ischemia are people over 60 years of age. Scientists associate the increase in the number of diagnosed ischemic nephropathy in developed countries with an increase in life expectancy.
Bilateral atherosclerotic process, which reduces the amount of blood flowing to the kidneys, or 50% damage to the only functioning renal artery leads to the development of renal ischemia and impairment of their functions. Ischemic nephropathy can be caused by damage to the abdominal aorta, renal arteries of both large and small caliber. The main danger is that the vessels may be completely blocked, which will stop the blood supply to the kidney and stop the process of removing waste products from the body. This will result in acute kidney failure, a life-threatening condition.
The need for timely diagnosis
There are no standard procedures for diagnosing coronary kidney disease. The doctor may suspect renal ischemia if certain diseases are already present or based on certain clinical symptoms, for example:
- in patients with coronary heart disease and aortic and peripheral vascular diseases.
- if there is a sudden deterioration in kidney function after the use of antihypertensive (arterio-controlling) drugs known as ACE inhibitors.
- for shortness of breath or difficulty breathing caused by pulmonary edema;
- for hypertension;
- with progressive azotemia in an elderly patient;
- If sounds or murmurs caused by turbulent blood flow inside the arteries are heard when listening with a stethoscope, they can be found in the neck (in the carotid artery), abdomen and groin (in the femoral artery).
- when the patient experiences pain in the legs when walking caused by circulatory problems:
To confirm the diagnosis, the doctor may order magnetic resonance angiography.
If ischemic nephropathy is suspected, instrumental testing is required for an accurate diagnosis:
- double Doppler sonography;
- radioisotope renography;
- magnetic resonance angiography;
- spiral computed tomography.
Acute renal failure.
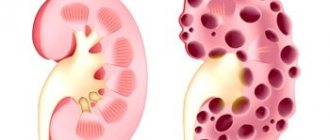
Acute renal failure is morphologically characterized by cyclic changes depending on the stage of the process: initial (shock), oligoanuric or stage of diuresis restoration. Macroscopically, the kidneys in all stages look the same: enlarged, swollen, pronounced swelling, a tense fibrous capsule is easily removed. The pale gray cortex is wide and sharply separated from the dark red medulla, multiple hemorrhages in the intermedial zone and pelvis. During histological examination in the kidneys, changes depend on the stage of the disease.
In the shock stage, there is a sharp venous congestion of the intermedial zone and pyramids and ischemia of the cortical layer (collapsed glomerular capillaries). Lymphostasis is combined with interstitial edema. Hyaline-droplet, fatty or hydropic degeneration of the tubular epithelium is noted, with uneven expansion of the lumen.
In the oligoanuric stage, focal necrotic changes develop in the tubules, accompanied by destruction of the basement membrane of the distal tubules (tubulorhexis). The cylinders clog the nephron at different levels, and stagnation of the glomerular ultrafiltrate develops in the glomerular capsule. The swelling of the interstitium increases and leukocyte infiltration and hemorrhages occur. Venous thrombosis develops against the background of sharply increasing venous stagnation.
Acute renal failure in the stage of diuresis restoration is characterized by plethora of most glomeruli and a significant decrease in edema and infiltration of kidney tissue. Zones of necrosis of the tubular epithelium alternate with areas of epithelial regeneration. In the presence of a preserved basement membrane, complete restoration of the epithelium of necrotic tubules occurs. Sclerosis develops in areas of damage to the basement membrane.
Acute renal failure is complicated by the development of total necrosis of the renal cortex associated with prolonged renal ischemia and severe circulatory disorders.
Acute renal failure
Acute renal failure (ARF), a predominantly reversible, rapid disruption of the homeostatic function of the kidneys, most often of ischemic or toxic origin, manifested by rapidly increasing azotemia and severe water and electrolyte disturbances.
Depending on the mechanism of development, three types of acute renal failure are distinguished:
1. prerenal (hemodynamic), caused by acute impairment of renal circulation;
2. renal (parenchymal), caused by damage to the renal parenchyma;
3. postrenal (obstructive), developing as a result of acute disruption of the outflow of urine from the kidneys.
This division of acute renal failure is of important practical importance, since therapeutic measures for different types of acute renal failure differ. In urological practice, we often encounter cases of acute renal failure that arise as a result of an acute violation of the outflow of urine from the upper urinary tract into the bladder, the so-called excretory obstructive (surgical) or postrenal anuria.
The causes of prerenal acute renal failure are decreased cardiac output, acute vascular insufficiency, hypovolemia and a sharp decrease in circulating blood volume. This leads to a long-term and sometimes short-term decrease in blood pressure to 80–70 mm Hg. Art. and lower, which is accompanied by a violation of general hemodynamics and circulation. Due to depletion of renal circulation, redistribution (shunting) of renal blood flow occurs, leading to ischemia of the renal cortex and a decrease in glomerular filtration rate. As renal ischemia worsens, prerenal acute renal failure can develop into renal acute renal failure due to ischemic necrosis of the epithelium of the renal convoluted tubules.
Risk factors for the development of hypovolemia and a decrease in circulating blood volume are:
1. traumatic shock;
2. crushing and muscle necrosis (cruch syndrome);
4. burns and frostbite;
5. surgical trauma (shock);