Causes of the disease
Megaureter is one of the most common and severe ureteral anomalies.
There is currently no consensus on the origin of megaureter. It is believed that the most likely cause of megaureter is the presence of an obstruction to the outflow of urine in the lower parts of the ureter, as well as insufficient development of the neuromuscular apparatus of the ureter (neuromuscular dysplasia). As a result, its expansion occurs. The wall of the ureter becomes sharply thinner. Most often, megaureter in the early stages is detected in children from 3 to 15 years old, mainly at the age of 6-10 years. Girls suffer from this defect 1.5 times more often. The megaureter is localized on the right 2 times more often than on the left. Bilateral lesions are much more common.
Symptoms and course of the disease
Occasionally there are complaints of pain in the abdomen or in the lumbar region on the affected side. But most often, in the absence of pathology of the bladder and urethra, megaureter does not manifest itself clinically until the development of pyelonephritis. The latter has a characteristic clinical and laboratory picture, well known to pediatricians. In the acute phase of the disease, high temperature and symptoms of intoxication are noted. The number of leukocytes in the urine increases and protein appears. An increased level of leukocytes and an increased ESR are also detected in the blood. As a rule, pediatricians refer children with acute pyelonephritis to hospital treatment, after which a urological examination is usually carried out.
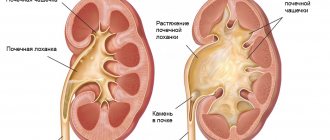
In pediatric practice, ureterohydronephrosis (Megaureter) is one of the diseases leading to impaired renal function, and, in a bilateral process, up to renal failure. When the ureter expands, its transport function suffers and it becomes impossible to quickly move urine into the bladder and remove microbial flora that penetrates the urinary tract, causing chronic inflammation of the kidneys (pyelonephritis). Another dangerous consequence of urine stagnation in the ureter is an increase in pressure in the renal pelvis and calyces, which causes impaired renal circulation. The outcome of chronic inflammation and impaired renal circulation is scarring of the renal tissue (parenchyma) with loss of function (secondary renal shrinkage, nephrosclerosis).
Reasons for development
Uretherohydronephrosis in a newborn can occur for the following reasons:
- underdevelopment of the lumen of the ureter in the fetus;
- the location of the ureters is twisted;
- the vessels tighten the ureter and create obstruction;
- muscle spasm, which could occur during childbirth or due to spinal cord injury;
- tumors of the pelvic organs.
Cystic kidney formations can cause this pathology.
- stones in the ureters;
- organs affected by cysts, such as kidneys;
- mechanical injury to the ureter resulting in the formation of edema that prevents the outflow of urine;
- obstruction occurs if a blood clot enters the duct;
- When the spinal cord is injured, the impulses of the excretory system are disrupted;
- chronic diseases;
- deformation of the kidneys and ureters;
- purulent formations in the kidneys.
Risk factors that influence the development of the disease:
- urolithiasis disease;
- scarring of connective tissue in the lymph nodes;
- uncontrolled use of painkillers;
- anemia;
- diabetes;
- a course of radiation exposure, during which kidney cells begin to die;
- oncology.
There are 2 fundamentally different causes of ureterohydronephrosis: congenital and acquired. The first manifests itself in children at an early age, which requires immediate action. These include:
- developmental anomalies of the ureter (valves);
- deviations in the development of the kidney itself (stricture of the calyces and pelvis);
- pathological location of the ureter (for example, behind the inferior vena cava);
- strictures and obstruction of the urinary tract in various areas;
- spasm of the ureteral sphincter (due to hypertonicity of the nervous system in children);
- abnormal bending of the ureter in its suprapubic part.
Acquired causes of ureterohydronephrosis include:
- Urolithiasis (especially when the size of the stones is more than 0.5 cm or their coral shape).
- Ureteral injuries.
- Tumors whose growth compresses the ureter (cervical, prostate or rectal cancer).
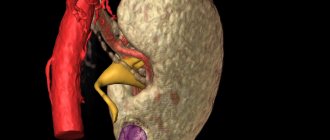
- Aneurysm of the abdominal aorta and iliac vessels.
- Spinal cord injuries and, as a result, disruption of the nervous regulation of the urinary system.
- Blood clots.
- Chronic inflammation of the ureter, calyces and pelvis.
- Kidney cyst.
- Abscess or carbuncle of the kidney on both the right and left.
Ureterohydronephrosis is an expansion of the ureter, renal pelvis and calyces with a gradual decrease in kidney function and atrophy of its parenchyma. As a result, the patient has a violation of the patency of the ureter in the pelvic region.
People at risk for developing ureterohydronephrosis include:
- childhood, when ureterohydronephrosis is a consequence of a violation of the outflow of urine through the urethra due to
- the presence of a congenital valve in the urethra;
- the presence of persistent spasm of the urethral sphincter, in particular in neurological disorders;
- urolithiasis - due to blockage of the ureter by a stone, intrarenal pressure increases, and the physiological outflow of urine does not seem as natural as it should be;
- sickle cell anemia – there are disturbances in renal blood flow;
- diabetes mellitus – there is also a violation of blood flow in the kidneys;
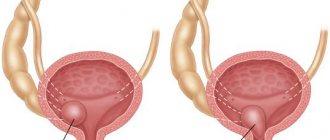
- adenoma or malignant hypertrophy of the prostate - pathology is formed against the background of increased pressure in the urethra in the central part of the organ;
- analgesics – leads to renal failure
- anticholinergic drugs - impairs renal blood flow;
The classification of ureterohydronephrosis is based on its origin:
- primary or congenital ureterohydronephrosis - for example, with narrowing of the ureteral opening, ureterocele, etc.;
- secondary or acquired – due to previously developed diseases of the genitourinary system (urolithiasis, trauma, etc.).
Ureterohydronephrosis also differs by localization:
- unilateral;
- bilateral.
According to the degree of ureteral obstruction, the following types of ureterohydronephrosis are distinguished:
- refluxing - due to vesicoureteral reflux, there is an equal expansion of the ureter along the entire length;
- obstructive - expansion of the ureter in the upper section and, accordingly, a violation of the outflow of urine, provoked by a pronounced narrowing of the ureter in the lower section;
- combined – in the presence of simultaneous narrowing of the ureter and vesicoureteral reflux.
There are five stages in the development of ureterohydronephrosis:
- decreased tone and expansion of the pelvic ureter;
- decreased tone of the ureter and its ability to contract, impaired excretory function of the kidney;
- decreased tone of the renal bowls and calyces, impaired secretory-excretory function of the kidneys;
- decreased tone and motor-evacuation function of the upper urinary tract, increased intralumenal pressure and severe impairment of renal function;
- atrophy of the renal parenchyma.
The most eloquent is the clinical picture of acute ureterohydronephrosis. at the same time, the symptoms of the disease may at first glance resemble symptoms of hydronephrosis. So, the manifestations of the acute form of ureterohydronephrosis include:
- renal colic,
- pronounced changes in urine analysis,
- dysuric disorders,
- chronic urinary tract infections,
- hematuria,
- enlargement of the abdomen in the lower third.
Diagnostics
Diagnosis of the disease is possible using laboratory and hardware examination methods:
Laboratory tests include mandatory blood and urine tests. They show the condition of not only the kidneys, but also the entire body as a whole. These studies cannot be considered fundamental indicators, but they are very important for monitoring the dynamics of the disease. A blood test for ureterohydronephrosis may have the following abnormalities:- signs of azotemia;
- increased calcium and sodium levels.
urea level exceeds normal;
The presence of protein, red blood cells, and white blood cells is detected in urine. If the pathology is provoked by temporary factors, for example, pregnancy, incomplete development of internal organs in children while in the womb, then the results of clinical studies may be within normal limits.
The leader in prescription is ultrasound examination. Its big advantage is the complete absence of radiation exposure.
The method is approved for use in pregnant women and children. Ultrasound can be informative for determining the parameters and location of the kidneys and ureters. You can also see what causes the difficulty in the outflow of urine through the ureter. With the simultaneous use of a Doppler sensor, you can find out at what speed and force the blood flows in the affected kidney.
A study using X-rays is called excretory urography. During this procedure, it is necessary to inject a contrast agent into the cubital vein.
Over the next half hour, a series of images are taken that will help visually assess the condition of the pyelocaliceal system and bladder, the process of formation and excretion of urine, as well as how sufficient the renal blood flow is. If the urinary tract is dilated, then the images will show a slow excretory function of the kidneys and atrophy of the renal parenchyma.
Diagnostics using MRI is an excellent method for identifying pathologies in neighboring tissues, allows you to measure their density, exclude the presence of tumors and the causes of their appearance. Using chromocystoscopy, you can visualize the ureters, bladder, and uterus. Aortography examines the blood flow in the kidneys, as well as how much the parenchyma of the affected kidney is changed.
Treatment of the disease
The disease can be bilateral.
Ureterohydronephrosis is classified according to the location of pathological changes. In total, there are 2 types - one-sided and two-sided. According to statistics, unilateral pathology is more often detected, only 5% are bilateral. And also ureterohydronephrosis is distinguished by the degree of dysfunction:
- reflexive - complete obstruction along the entire length;
- obstructive - expansion in the upper part of the ureter;
- combined - simultaneous narrowing of the ureter and reflux.
By origin:
- congenital;
- acquired.
Most often, the disease must be treated surgically.
Ureterohydronephrosis is treated in two ways: conservative and surgical. The first is applicable only in the early stages of development; the problem is that it is difficult to identify the disease, because symptoms appear at later stages. According to statistics, the most commonly used treatment method is surgery.
Prevention
The main measures to prevent reflexive ureterohydronephrosis in a child are timely emptying of the bladder. This is especially true for schoolchildren and students. Prolonged abstinence from urination leads to reflux. Certain precautions must be taken to prevent ureterohydronephrosis.
When studying the medical history of ureterohydronephrosis, attention is drawn to the early onset of the disease and relatively rapid progression. Therefore, when the first signs of kidney disease appear, you should immediately consult a doctor. Timely treatment will help preserve health and life.
Source: moi-pochki.ru
How to treat ureterohydronephrosis?
Treatment of ureterohydronephrosis is determined individually after an in-person consultation with a physician and specialized diagnostics. There are cases where ureterohydronephrosis resolved on its own, but this is rather an exception. The choice of treatment method or observation regimen depends on the severity of the pathology, the patient’s age, the presence of pyelonephritis and the degree of renal dysfunction.
Based on the medical history and taking into account the causes of the disease, the functioning of the genitourinary system as a whole is normalized. Most often, it will not be possible to achieve a stable result with conservative therapy alone, therefore surgical intervention becomes the method of choice for ureterohydronephrosis:
- removal of the obstacle - ureterolysis, ureterolithotomy, removal of ureterocele, etc. are carried out;
- resection of the ureter with end-to-end, end-to-side anastomosis;
- the use of direct or indirect ureterocystoneostomy.
With the development of medical progress, a minimally invasive endoscopic method of treating ureterohydronephrosis is gaining popularity. It is most appropriate for obstructive ureterohydronephrosis. The narrowed section of the ureter is widened, the so-called bougienage, followed by the installation of a stent. With progressive obstructive ureterohydronephrosis, this method is significantly inferior in effectiveness to surgical treatment, since obstacles to the outflow of urine remain.
In case of atrophy of the renal parenchyma, nephroureterectomy is advisable.
Conservative therapy in most cases of ureterohydronephrosis does not have a comprehensive effect, therefore pharmaceutical drugs are used to a greater extent in the pre- and postoperative period. You should talk to your doctor about specific names and dosages. The latter must be aware of the origin of the disease and its history, and have the patient’s test results in hand.
Diagnostic measures
A general urine test is performed to assess the inflammatory process. An increased number of white blood cells in the urine indicates an infection. Microhematuria implies exclusion of a tumor. A general blood test may show leukocytosis and accelerated ESR.
An increase in serum urea and creatinine is a consequence of 2-sided hydronephrosis and hydroureter.
Hyperkalemia, which often accompanies kidney failure, is life-threatening.
Instrumental diagnostics
Early detection of renal hydronephrosis and urinary tract obstruction prevents serious complications associated with loss of renal function. To confirm acute or chronic urinary retention, bladder catheterization is performed. An increased amount of residual urine can be diagnosed by ultrasound.
X-ray diagnostic methods are used to exclude obstruction at the level of the ureters and above, which is confirmed by dilatation of the renal collecting system. To clarify the extent of the pathological process, if a tumor or retroperitoneal fibrosis is suspected, magnetic resonance imaging is performed.
Indications for CT/MRI are as follows:
• ambiguity of ultrasound results; • poor visualization; • inability to determine the cause of urinary tract obstruction.
The combination of MRI, CT to detect radiopaque stones, ultrasound and excretory urography is sufficient for diagnostic purposes in more than 90% of cases. To assess the functional capacity of each kidney, radioisotope scintigraphy is used.
According to indications, additional instrumental diagnostic methods are possible: voiding cystourethrography is performed to identify malformations of the lower urinary tract.
Magnetic resonance urography in children is increasingly used in the diagnosis of congenital uropathy (obstruction of the ureteropelvic segment).
The disadvantages of the method include the need for general anesthesia or heavy sedation in children. In addition, gadolinium contrast agent may be used if renal function is preserved.
Antegrade or retrograde pyelography is used to insert stent drainage to normalize adequate urine flow.
Stages and symptoms
There are unilateral and bilateral ureterohydronephrosis, there are several degrees of severity (depending on how intact the patency of the ureter is) and the main stages in the development of the disease (from decreased tone and minor stretching to large-scale atrophy of parenchymal tissue.
Accordingly, the clinical picture in different patients may differ significantly. Pathognomonic (exclusively inherent) symptoms of ureterohydronephrosis, distinguishing it from other renal pathologies (for example, hydronephrosis with a preserved ureter) have not been described to date. However, the most typical manifestations of ureterohydronephrosis most often include the following:
- renal colic (paroxysmal, sharp, sometimes unbearable pain in the kidney area);
- specific “bloating” in the lower abdomen;
- urination disorders (frequency, lack of feeling of emptying the bladder, false and repeated urges, etc.);
- presence of blood in the urine;
- predisposition or actual presence of infections of the genitourinary system, their easy chronicity and persistent (persistent) nature due to congestion favorable for the pathogenic pathogen.
Ureterohydronephrosis is diagnosed (and differentiated from other diseases with a similar clinical picture) mainly by radiography - urology-specific contrast modifications of the X-ray examination are prescribed. In some cases, diagnostic and/or drainage catheterization, ultrasound and other diagnostic studies may be indicated. Laboratory tests of urine and blood are required.
About our clinic Chistye Prudy metro station Medintercom page!
| Stage | Symptoms |
| 1 | Decreased muscle tone |
| The lumen is expanding | |
| 2 | The ureter is unable to contract |
| Urine flow worsens | |
| Kidneys suffer | |
| 3 | The tone of the cups and pelvis decreases |
| 4 | The efficiency of the upper excretory tract decreases |
| The pressure in the renal vessels increases, which adversely affects their function | |
| 5 | The renal parenchyma (the lining of the kidneys) atrophies |
| Kidney failure develops |
At the onset of the disease, a person may have slight swelling of the face.
- Painful sensations - pain occurs suddenly, it does not go away for several hours. At night, the pain worsens; when changing position, relief does not occur.
- Tissue swelling - due to the fact that the excretory system suffers, the swelling of the skin increases. At first, swelling of the face is barely noticeable, then it spreads to all limbs.
- Increased blood pressure.
- Specks of blood in the urine indicate disorders of the excretory system.
- Fever, headache, fatigue.
Hydronephrosis of the kidneys in newborns
For early detection of the pathological process, antenatal ultrasound examination is performed; hydronephrosis in the fetus can be detected by the end of the first trimester of pregnancy.
Most cases of antenatal hydronephrosis in the fetus are not clinically significant, and the newborn child does not need instrumental examinations.
Physical examination
With severe hydronephrosis, the kidney can be palpated as an enlarged, painful formation. With 2-sided hydronephrosis, swelling in the lower extremities may occur. An enlarged bladder, located above the pubis, is characteristic of obstruction of the lower urinary tract.
In newborns, physical examination helps detect abnormalities that suggest disruption of the normal functioning of the urinary system associated with antenatal hydronephrosis. Pay attention to the following aspects:
• Palpation of an enlarged kidney. • Palpation of a full bladder in an infant boy, especially after emptying, which may indicate posterior urethral valves. • For some malformations, undescended testicles are diagnosed in the scrotum.
Treatment of other diseases starting with the letter - y
Ureterohydronephrosis can be primary only in the case of a congenital diagnosis. However, in most cases, including in children, this disease develops against the background of other kidney dysfunctions and pathologies of the genitourinary system:
- urolithiasis disease;
- vesicoureteral reflux;
- sickle cell anemia;
- diabetes;
- ureterocele;
- BPH;
- malignant prostatic hypertrophy.
In its development and course, ureterohydronephrosis certainly goes through the stage of hydronephrosis, and ultimately risks ending with atrophy of the renal parenchyma.
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.
Ureterohydronephrosis is diagnosed when part of the urinary system (kidney and ureter) ceases to function due to physical obstruction of the ureter.
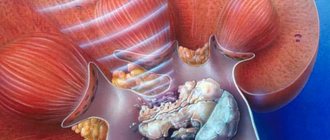
In this case, the muscle fibers of the ureter stretch as its lumen is filled with accumulated urine; it may become slightly longer and more tortuous. The body of the kidney (pelvis and calyx) also gradually fills with urine, taking on the appearance of a large muscular sac with many filled chambers.
This leads to the fact that the most functional part of the organ, the membrane of the kidney (parenchyma), stretches and becomes much thinner, which is why the cells (nephrons) are no longer able to perform their functions.
This leads to acute renal failure, a condition that requires emergency medical attention from a surgeon.
In severe and rapidly progressing disease, the volume of the kidney can reach several liters. In such a situation, any injury to the kidney or ureter can result in organ rupture
During pregnancy, ureterohydronephrosis can be diagnosed in both mother and child.
In women, this pathology most often occurs due to the growing uterus, which puts pressure on nearby organs, including the ureters, blocking their lumen. After childbirth, kidney function is completely restored.
Such a diagnosis can be made to a baby starting from 14-16 weeks of intrauterine development, when the physiological position and size of the organs can be assessed. The pathology is more common in boys and is localized on the left.
In 95% of cases, ureterohydronephrosis is unilateral, and only when the pathology is caused by systemic disorders (for example, with spinal cord injuries, there is a lack of nervous regulation of the ureteral muscles) is bilateral localization observed. In other cases, damage to the right or left ureter occurs with equal frequency.
Depending on the time of onset of the pathology, congenital and acquired ureterohydronephrosis are distinguished.
The congenital form is most often found in boys and is diagnosed during fetal development. The acquired form can occur in any person, in the presence of predisposing factors, despite his age, gender or social status.
Classification according to the presence of additional conditions involves division into:
- aseptic type of disease (when there is no additional infection of the affected areas);
- infectious (when urinary retention is also accompanied by an inflammatory process caused by a bacterial, fungal or other type of pathogenic microflora).
In some cases, the pathology may be accompanied by pyelonephritis
Ureterohydronephrosis has certain stages of development:
- 1st degree. The condition is characterized by incomplete urinary retention and a slight disruption of the physiological state of the kidney and ureter. The pelvis and calyx suffer slightly, but functional disorders in the filtering and excretory capacity of the kidney are not detected;
- 2nd degree. The ureter and kidney significantly increase in volume, the overall activity of the kidney is disrupted (by about 20-40%);
- 3rd degree. The kidney space is completely filled with urine, the ureter is swollen, and its peristalsis is impaired. The parenchyma completely ceases to function, necrotization of tissue areas is observed, and acute renal failure occurs.
- The transition from one stage to another can occur very quickly (within several days), or take a long time (with chronic processes causing ureteral obstruction).
- Depending on when exactly ureterohydronephrosis occurred, the factors that caused it will vary.
- So, if a pathology is diagnosed in a child during the period of intrauterine maturation or in the first months of life, then most likely it was preceded by:
- physiologically incorrect location of the ureter or central blood vessels of the kidney, which causes compression of any part of the ureter;
- muscle spasm of the ureteral sphincter due to immaturity of the nervous system or spinal cord injury during childbirth. In most cases, the condition resolves on its own;
- pathologies of the formation of the ureter (for example, its kinking or the presence of a non-return valve);
- tumors of the urinary system or neighboring organs.
Children with this diagnosis should be observed by a nephrologist and urologist
Enlarged renal pelvis in a newborn
- blocking of the ureter with a kidney stone;
- tumors or cysts of the kidney, ureter, rectum, uterus and other organs. The neoplasm in this case physically compresses the lumen of the ureter;
- ureteral injury. In this case, the outflow of urine can be complicated by swelling and hematoma that occurs after the blow, or by cellular changes due to injury (when muscle tissue and mucous membrane are replaced by many fibers of connective tissue);
- blockage by a blood clot. This can occur in the presence of glomerulonephritis, as well as other kidney or blood diseases;
- violation of the nervous regulation of the urinary system. Most often this is a consequence of spinal cord injury;
- chronic inflammatory processes. In this case, one type of cell is replaced by another in some parts of the urinary system (for example, the elastic tissue of the smooth muscles of the walls of the ureter can be replaced by connective or fibrous tissue, forming compactions, thickenings and cysts).
In addition to the reasons that directly affect the physical patency of the ureter, there are also general conditions that predispose to the appearance of ureterohydronephrosis, for example, diabetes mellitus, pregnancy, polycystic ovary syndrome, etc.
Ureterohydronephrosis is a disease without specific symptoms.
Most of the manifestations that accompany this pathology are also inherent in many other diseases of the urinary system.
But as the process of ureterohydronephrosis develops and worsens, a person may experience:
- pain in the lower third of the back on one side (right or left). The pain is most often aching and constant, but it can also be paroxysmal with intensification, up to renal colic. Localization can also be different - from the lower back to the anterior abdominal wall, groin or inner thigh;
- swelling of tissues. At the beginning of the disease, this manifests itself only in the mornings as a slight puffiness of the face. But subsequently, the more serious the damage to the kidney, the more pronounced the swelling becomes. They are observed on all parts of the body and do not decrease during the day;
- arterial hypertension. The condition may be permanent or transient. This symptom appears at later stages and requires medical attention;
- increase in abdominal volume. This manifestation is more noticeable and typical for children (due to physiological characteristics). Often there is a noticeable enlargement of not only the abdomen, but also the diseased kidney (it is determined by palpation as a relatively large formation);
- blood in urine. This is a sign of serious kidney problems.
Against the background of a decrease in renal function, the general condition also worsens - symptoms of intoxication appear (nausea, vomiting, fever, loss of strength, dizziness, etc.).
Indirect manifestations of the clinical picture of chronic ureterohydronephrosis include additional diseases of the urinary system that often arise against its background (cystitis, pyelonephritis, urethritis, etc.).
Diagnostics
To accurately confirm the diagnosis of ureterohydronephrosis and identify the causes of its occurrence, hardware diagnostic methods (ultrasound, X-ray examination methods, MRI) are mainly used. Laboratory tests of urine and blood are carried out to determine general indicators of the condition of the body and kidney function in particular.
Ultrasound is considered the most preferred and popular instrumental research method.
When performing an ultrasound, there is no radiation exposure and it can be used an unlimited number of times even in very young children, as well as in pregnant women. This type of study reveals the physiological location and parameters of the ureters and kidneys.
The process also identifies the location and possible cause of the obstruction in the outflow of urine through the ureter. The parallel use of a Doppler sensor allows you to measure the speed and strength of renal blood flow, which is very important for assessing the functioning of the organ.
A more accurate and informative method is urography and computed tomography using contrast. After contrast is injected into the bloodstream (via the ulnar or femoral vein), a series of images are taken. This approach allows you to visualize the process of formation and excretion of urine, measure time parameters, and assess the sufficiency of renal blood flow.
The MRI method is used to assess damage to adjacent tissues, identify concomitant pathologies and neoplasms, measure tissue density, and identify the causes of pathology.
General and biochemical tests of urine and blood, although not fundamental, are absolutely necessary to monitor the condition over time
- Thus, in the blood with ureterohydronephrosis, an increased content of urea and nitrogen, as well as sodium and calcium, is found.
- A urine test contains red blood cells, white blood cells, and sometimes protein.
- If the pathological condition is caused by temporary reasons (pregnancy, underdevelopment of organs during intrauterine development in newborns in the first months of life) and is partial, then clinical tests may be within normal limits.
Treatment
Classification of the disease
If the disease progresses quickly and is severe, the kidney can reach very large sizes and contain several liters of urine in its tissues. In this condition, even a slight injury to the organ can lead to its rupture.
In almost all cases of the disease, it is characterized by one-sided localization. Ureterohydronephrosis on the right occurs as often as on the left. Only in 5% of all cases is bilateral ureterohydronephrosis recorded. A bilateral pathological process can occur as a result of spinal cord injury.
Depending on when the first signs of the disease appeared, there are two types of ureterohydronephrosis: congenital and acquired. The congenital disease is more common in boys, and its diagnosis occurs in the womb. As a result of compression of this vessel, the pressure in the urinary tract increases. The development of an acquired type of disease can occur in any person, regardless of the patient’s age category, gender and social status.
There is also a division into the aseptic form of the disease and an infectious disease:
- with the aseptic type of ureterohydronephrosis, there is no bacterial flora that could lead to an additional infectious inflammatory process of the renal parenchyma;
- the infectious form of the disease develops as a result of complications of urinary retention by an inflammatory process provoked by the presence of bacteria, fungi and other pathogens. Sometimes a complication develops in the form of pyelonephritis.
The transformation of one stage into another can occur in a short period of time, up to several days, but a long protracted process is also possible.
Stages of development of ureterohydronephrosis:
- First degree. The physiological state of the kidney and ureter is slightly impaired, urinary retention does not occur completely. The filtering and excretory functions of the organ are preserved.
- Second degree. There is a progression of enlargement of the kidney and ureter in volume. The functioning of the organ is impaired by approximately 30%.
- Third degree. The affected organ is completely filled with urine, the ureter swells, and its peristalsis does not occur properly. The work of the parenchyma is stopped, tissue necrosis is observed, and acute renal failure increases.
Concomitant pathologies
Degree of development of pathology:
- First degree. The changes are insignificant; partial urine retention is observed. The main functions of natural filters are preserved.
- Second degree. Ureterohydronephrosis develops rapidly, and organs increase in size. The excretory function is partially impaired.
- Third degree. Irreversible processes have started, the cavity is filled with urine, the ureter is increased in size. The kidneys stop functioning and tissue necrosis begins. Acute renal failure develops.
Diabetes mellitus often develops simultaneously with this disease.
- sickle cell anemia;
- vesicoureteral reflux;
- stones in the kidneys;
- prostate cancer;
- diabetes.
Forecasts
The prognosis for ureterehydronephrosis depends entirely on its type and the stage at which the disease is detected. If you recognize a cyst or narrowing of the ureter at the very beginning and carry out full conservative therapy, the outcome is the most favorable. The most important thing then is to regularly do urine tests and ultrasounds so as not to miss a possible relapse.
But if ureterehydronephrosis is not treated, it can lead to the most dangerous complications: acute renal failure and impaired liver function.
Therefore, at the slightest sign indicating possible ureterehydronephrosis in you or your child, immediately contact a urologist or nephrologist and undergo all tests.
And in the presence of chronic diseases that can provoke narrowing or obstruction of the ureter (kidney stones, diabetes mellitus, etc.), you need to remember basic preventive measures. That is, follow a low-salt diet, avoid hypothermia, and treat inflammation and swelling in a timely manner.
Treatment of ureterohydronephrosis with traditional methods
The use of folk remedies in the treatment of ureterohydronephrosis is unacceptable, since such remedies do not have a pronounced effect. At the same time, in the postoperative period, the patient can discuss with his doctor folk remedies that help maintain and improve bladder and kidney function. These include herbal decoctions:
- burdock,
- daisies,
- birch buds and young leaves,
- oat grains,
- juniper fruits,
- hop cones.
Sanatorium-resort treatment of hydroureter
As a rule, hydroureter manifests itself in combination with various pathologies of the kidneys and other organs of the urinary system. Sanatorium-resort therapy reduces the risk of the occurrence and development of complications, stops the progression of the disease, and helps to achieve stable remission of the disease.
The spa therapy program includes:
- Therapeutic exercise.
- Physiotherapy.
- Aromatherapy.
- Intestinal irrigation.
- Treatment with microenemas.
- Reception of mineral waters.
Repeated courses of sanatorium-resort therapy have a high positive effect.
Sanatorium treatment is carried out according to a special treatment program for 21 days