What is hypoplasia of the frontal sinus
There is congenital hypoplasia, acquired or secondary.
A doctor can diagnose a unilateral form of pathology. For example, there is hypoplasia of the frontal sinus on the right. What this is is already clear from the name. Of course, this is not the only scenario. Hypoplasia of the left frontal sinus also occurs with the same frequency. The doctor will tell you what it is if he discovers such an anomaly.
There is also bilateral hypoplasia and multilocular (trabecular).
Functions of the frontal sinus or frontal sinus:
- reducing the mass of the skull, making it lighter;
- protection of the brain from injury, a kind of shock absorption;
- acoustic function, formation of a characteristic voice timbre;
- individuality of facial features;
- moisturizing the mucous membranes of the nasal cavity.
Agenesis or atresia of the frontal sinuses can also be acquired. Such hypoplasia is essentially secondary sclerosis. This occurs as a result of past infections - frontal sinusitis, pansinusitis, or injuries to the facial area. Their consequences are regression of cavity development and bone compaction.
As a result of recent clinical studies, it has become clear that hypoplasia of the frontal sinus is not the cause and does not at all affect the occurrence of inflammation of the mucous membranes of the paranasal sinuses or sinuses, which is called sinusitis.
This is frontal sinusitis, sinusitis, ethmoiditis or inflammation of the mucous membranes of all sinuses at once (pansinusitis). Such diseases are complications of colds and infectious pathologies of the upper respiratory tract, that is, the throat and nasopharynx, and require special examination and treatment by an otolaryngologist.
Sinusitis can be acute: catarrhal, purulent, polymeric, as well as chronic. These diseases require special treatment with antibiotics, antivirals and possibly antifungals. This inflammatory process threatens with such serious complications as meningitis, arachnoiditis and encephalitis (this is inflammation of the hard arachnoid membrane of the brain and the substance of the brain).
The frontal paranasal sinuses are second in size after the maxillary sinuses. In another way they are also called frontal. They are concentrated in the thickness of the frontal bone in the area just above the bridge of the nose. We are talking about a paired anatomical formation, which is divided into two parts by a special partition.
In Welcome to the question: What is frontal sinus aplasia? The best answer given by the author Andrey is the Frontal sinuses (lat. sinus frontales) - paranasal sinuses located in the frontal bone posterior to its superciliary ridges. The lower walls of the frontal sinuses are the upper walls of the orbits, the posterior walls separate the sinuses from the frontal lobes of the brain.
The inside of the sinuses is lined with mucous membrane. At birth, the frontal sinuses are absent, develop by 7-8 years and reach their maximum size after puberty. More often they are asymmetrical, the bony septum between them is deviated to one side or another from the midline. There are additional partitions.
2 - frontal sinus;
3 - ethmoid bone;
4 - sphenoid sinus.
Aplasia or hypoplasia of the frontal sinus is not a rare phenomenon that does not pose any negative consequences for a person.
Basilar artery
Merging together, the two PAs form a single vessel at the base of the brain, supplying blood to the entire central nervous system. It carries oxygen and important nutritional compounds to the occipital lobes, cerebellum and brainstem - the most important structures of the brain. The basilar artery divides into several more vessels.
Like a tree, they send out many branches to significant elements of the central nervous system. The posterior cerebral arteries supply the temporal and occipital lobes. The superior and anterior cerebellar vestibular organs, respectively. Additional paramedian and annular vessels provide nutrients to the deep tracts and nuclei. The pons Varolievs supplies blood to the artery of the same name.
In 15% of people, the basilar vessel has another branch - the internal auditory and labyrinthine.
Pathogenesis of frontal sinus hypoplasia
The formation of frontal sinuses is a genetically programmed process. Every child is born without them, that is, a newborn baby does not have them at all. The frontal sinuses normally begin to develop at about 7-8 years of age and by the age of 25 this process ends. Their cavity in an eight-year-old child is a maximum of 0.7 cm3, and in adults it reaches 7 milliliters.
Functions of the frontal sinus or frontal sinus:
- reducing the mass of the skull, making it lighter;
- protection of the brain from injury, a kind of shock absorption;
- acoustic function, formation of a characteristic voice timbre;
- individuality of facial features;
- moisturizing the mucous membranes of the nasal cavity.
Agenesis or atresia of the frontal sinuses can also be acquired. Such hypoplasia is essentially secondary sclerosis. This occurs as a result of past infections - frontal sinusitis, pansinusitis, or injuries to the facial area. Their consequences are regression of cavity development and bone compaction.
Why is hypoplasia of the cerebral arteries dangerous?
The classification of this disease indicates three main forms of hypoplasia:
Normally, these highways supply most of the brain. Their damage is a serious blow to the nervous system and health in general. Disturbances in the structure of the vascular wall do not allow the brain to receive the necessary substances in sufficient quantities. Oxygen and nutritional compounds do not reach their destination. The brain is starving. A defect in the vascular wall carries the risk of an aneurysm or stroke.
Therefore, this pathological condition is considered extremely dangerous to human life. Due to the seriousness of the consequences, hypoplasia of the cerebral arteries is given special attention in neurosurgical and neurological practice. The extreme condition in vascular development is aplasia. This is a defect in which the brachiocephalic arteries (BCA) are absent at birth.
Classification of sinuses by type of structure
There are also several types of paranasal sinuses according to their type:
- Pneumatic type;
- Sclerotic type.
The frequency of occurrence of frontal sinuses can be affected by the type of sinus - in the presence of a sclerotic type, more favorable conditions are created for the development of the pathological process in it.
This type of sinus is characterized by:
- significant reduction in size;
- the presence of thick bone structures;
- small, limited cavity.
This cavity, when pathogenic microflora enters it, serves as a fairly good reservoir, which ensures the proliferation of microorganisms, and due to its structural features, there is a violation of the evacuation and removal of foreign particles along with mucus.
An interesting fact is that in men, in the vast majority of cases, the severity of the brow ridges depends on the degree of development and size of the frontal sinus.
There are several types of developmental disorders of the frontal sinuses:
- complete lack of development - aplasia;
- its underdevelopment - hypoplasia;
- absence of a septum between the sinuses;
- secondary sclerosis – reduction in the size of the sinus.
What causes pathology?
It should be noted that aplasia is a congenital disease that occurs as a result of exposure directly to the fetus or indirectly through the maternal body of physical, chemical and biological factors. They, by acting on the gametes of parents or their ancestors, are capable of causing chromosomal pathologies with the absence of some organ or tissue.
By the way, the nondevelopment of one organ in the embryo practically never happens in isolation and, as a rule, leads to the death of another organ associated with it. For example, in the absence of a ureteric bud, aplasia of the secondary kidney occurs, etc.
And the deadline after which the described defects in the embryo can no longer develop is the first month of intrauterine life.
Bone marrow
Aplasia of the brain or aplasia of hematopoiesis is a syndrome characterized by an insufficient amount of bone marrow, which leads to suppression of the function of blood formation in the body. The patient has a deficiency of red blood cells, platelets and leukocytes. Severe disease often leads to death.
The main causes of this aplasia include radiation and chemotherapy. Naturally, the presence of autoimmune diseases can lead to abnormalities
It is also important what the environmental situation is in the patient’s place of residence, since harmful working conditions may influence health. For example, constant contact with pesticides and other harmful chemicals that can suppress the immune system
Some medications can also cause suppression of hematopoietic function (those that help with rheumatoid arthritis and some groups of antibiotics). Connective tissue diseases and, in some cases, pregnancy can cause aplasia. Last but not least are infectious diseases, hepatitis viruses and influenza. Mutations are also possible during fetal development.
Bone marrow aplasia can cause anemic coma or dysfunction of certain organs. The patient may be constantly bothered by fungal and infectious diseases, since the immune system with such a disease is greatly weakened.
Treatment mainly consists of two techniques:
- The use of anabolic steroids that stimulate protein formation.
- Blood transfusion with washed red blood cells. This is an extreme measure and is used when the patient’s life is at risk.
Who is at risk
The following conditions are considered to be provoking factors of pathology:
- heredity;
- transmission of influenza, rubella and other infectious diseases by the mother in the first trimester of pregnancy;
- long-term use of contraceptives before pregnancy;
- the presence of diseases of the endocrine system;
- alcohol abuse;
- transmission of sexually transmitted diseases.
The above factors must be taken into account by the attending physician during pregnancy.
Bad habits of the mother often become a provoking factor for fetal malformations
Physiological features
There are unfilled spaces in the facial bones of every person's skull. These are the sinuses of the nose, which in medicine are called paranasal or paranasal.
Air passes through them, so they are connected to the nose. Depending on the location of the sinuses, they form groups:
- the maxillary cavities are paired and are located in the upper jaw; there is a frontal cavity in the frontal bone; in the main bone of the skull there is a wedge-shaped cavity; The ethmoid cavity is formed from parts of the ethmoid bone.
The paranasal sinuses perform the following functions:
- breathing, because they are the ones who moisturize, warm and purify the inhaled air before it enters the lungs. This makes it clear why impaired nasal breathing generally worsens the well-being of the entire body; protection, since they are the ones who hold back coarse particles. So, when such particles get on the mucous membrane, it becomes irritated and the person sneezes, thereby clearing the nasal passages; sense of smell, special epithelial tissue helps detect odors; The paranasal sinuses take part in the formation of the timbre of the voice.
The frontal sinus is divided into 2 parts, and its sections are pneumatized in different ways. The same thing happens with the sphenoid sinus, which also has 2 parts and their pneumatization is different.
The paranasal sinuses are examined externally by a doctor, when the nasal and oral cavity and their swelling are visible. Upon palpation, you can notice pain in the patient. However, a deep examination can only be carried out using rhinoscopy.
A more complex diagnostic technique is probing, which is carried out either through the frontal or through the sphenoid cavity.
The frontal sinus or frontal sinus is a cavity in the bone located behind the brow ridge, shaped like an irregular pyramid with smoothed corners. Its sides are: the outer wall of the frontal bone in front, the upper wall of the orbit below, the back wall is the inner side of the frontal bone, bordering the frontal lobe of the brain, the inner wall is, in fact, the intersinus septum. The norm is that they are asymmetrical, that is, the partition is always slanted to the side.
A developmental anomaly is considered to be slit-like communications between the sinuses and surrounding tissues. They are called dehiscences. For example:
- Communication of the ethmoidal labyrinth with all sinuses.
- Holes in the lateral wall of the sinus. They bring its mucosa into contact with the meningeal membrane and the optic nerve, cavernous sinus and internal carotid artery.
- Reducing the thickness of the wall of the sphenoid sinus. This anomaly promotes contact with the abducens and trochlear, oculomotor and trigeminal nerves.
The paranasal sinuses are represented by cavities internally covered with epithelial tissue. Most of them are located in the bones of the facial skull or within the anterior cranial fossa.
Another important function is to humidify and warm the air while it is in the sinuses. Also, the sinuses themselves perform a resonator function for the voice - they provide its tonality, sonority and individual coloring
Thus, they are quite important structures of the human body.
The frontal sinuses are located directly in the thickness of the frontal bone posterior to the superciliary arches. They communicate with the nasal cavity through the middle meatus via the frontonasal canal.
A characteristic feature of the frontal sinus is that at birth this sinus is absent - it develops only by the 7-8th year of life, reaching its maximum development by puberty - for boys - 13-14, for girls - 12-13 years.
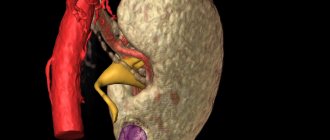
Structure of the vertebral artery
These vessels are important participants in providing nutrition to the brain. They are especially active in supplying its posterior sections with the necessary substances - the cerebellum and occipital lobes, partially the temporal lobes, the hypothalamus, and also the trunk. These arteries provide the brain with about 30% of all incoming blood.
The left ventricle of the heart gives rise to the aorta, the most voluminous and largest artery of the human body. The brachiocephalic trunk, which is the progenitor of the subclavian vessel, departs from it. And it, in turn, has two large branches - the right and left PA. The diameter of such a vessel reaches approximately 2–4 mm.
The cervical vertebrae form a narrow canal that serves as a container for the PA and conducts it to the brain. The vertebral artery runs next to the vein of the same name. These vessels enter the canal at the level of the 6th cervical vertebra and exit at the 1st. The foramen magnum is the conductor of the vessel to the cranial cavity. Approaching the base of the brain, the right and left PAs merge into one common main one - the basilar one.
This vessel also branches into two - the posterior cerebral vessels. The basilar and vertebral arteries form a single system - the vertebrobasilar. It has short branches that penetrate into the brain cavity, as well as long ones that go around it. The cerebellum is fed by the vessels of the same name - the lower anterior, posterior and superior.
The influence of aplasia on the occurrence of sinusitis
In cases of incomplete recovery or with advanced frontal sinusitis, the disease can take a chronic form. This is dangerous due to frequent relapses of the disease and other serious consequences in the form of meningitis or inflammation of the brain.
There is congenital hypoplasia, acquired or secondary.
A doctor can diagnose a unilateral form of pathology. For example, there is hypoplasia of the frontal sinus on the right. What this is is already clear from the name. Of course, this is not the only scenario. Hypoplasia of the left frontal sinus also occurs with the same frequency. The doctor will tell you what it is if he discovers such an anomaly.
The formation of frontal sinuses is a genetically programmed process. Every child is born without them, that is, a newborn baby does not have them at all. The frontal sinuses normally begin to develop at about 7-8 years of age and by the age of 25 this process ends. Their cavity in an eight-year-old child is a maximum of 0.7 cm3, and in adults it reaches 7 milliliters.
Functions of the frontal sinus or frontal sinus:
- reducing the mass of the skull, making it lighter;
- protection of the brain from injury, a kind of shock absorption;
- acoustic function, formation of a characteristic voice timbre;
- individuality of facial features;
- moisturizing the mucous membranes of the nasal cavity.
Agenesis or atresia of the frontal sinuses can also be acquired. Such hypoplasia is essentially secondary sclerosis. This occurs as a result of past infections - frontal sinusitis, pansinusitis, or injuries to the facial area. Their consequences are regression of cavity development and bone compaction.
This is frontal sinusitis, sinusitis, ethmoiditis or inflammation of the mucous membranes of all sinuses at once (pansinusitis). Such diseases are complications of colds and infectious pathologies of the upper respiratory tract, that is, the throat and nasopharynx, and require special examination and treatment by an otolaryngologist.
Sinusitis can be acute: catarrhal, purulent, polymeric, as well as chronic. These diseases require special treatment with antibiotics, antivirals and possibly antifungals. This inflammatory process threatens with such serious complications as meningitis, arachnoiditis and encephalitis (this is inflammation of the hard arachnoid membrane of the brain and the substance of the brain).
Science does not stand still, new methods of treating diseases are being created, drugs are being produced that can quickly and easily cure and correct defects. But all prescriptions are made exclusively by the doctor, based on the results of the examination. There is no point in doing something on your own, since in this case it can lead to undesirable consequences. Therapy is carried out only under the supervision of the attending physician and according to his recommendations.
Birth defects and anomalies can be directly related to hereditary pathology, when the normal process of formation of other cranial parts is disrupted. For example, abnormal development of the maxillary sinuses (maxillary sinuses) is detected in 13 percent of children diagnosed with sinusitis. Most often, anomalies of the paranasal sinuses manifest themselves as follows:
- A person’s sinuses may be partially narrowed or completely absent as a result of excess pressure on them from the facial or nasal walls. In this case, underdevelopment will vary widely, starting with a slight depression of the canine fossa, and ending with complete fusion of the nasal wall and the facial wall. In the latter case, the sinus simply disappears in the lower section.
- Doctors often diagnose unilateral anomalies. In this case, facial asymmetry is clearly visible. When attempting to puncture (puncture) an underdeveloped sinus, the doctor’s needle passes into the soft tissue of the cheek.
- Anomalies and defects of the frontal sinuses will differ from each other in both their size and volume. In some clinical cases, doctors diagnose agenesis of the frontal sinuses with a volume of up to 500 milliliters. There are four main types of delay in the development of sinuses. We are talking about a violation of pneumatization or its complete absence, unilateral or bilateral aplasia of the frontal sinus, trabecular agenesis and secondary sclerosis (regressive type anomaly).
- It is worth noting that aplasia is most often diagnosed in men. In addition, with unilateral disorders, the most reliable diagnosis is poor development of the opposite sinus.
Aplasia of the right kidney
But this condition is usually combined with aplasia of tissue located deeper, for example, in cases with non-closure of embryonic clefts (so-called dysarphia). In medicine, cases of aplasia of individual parts of the body are recorded, often this happens to human limbs. If a newborn has no skull bones, then brain aplasia (also called anencephaly) is often observed along with them.
Some types of aplasia (absence of the cerebral hemispheres, heart muscle, both kidneys, etc.) are incompatible with life. APLASIA - (from a negative prefix and Greek plasis formation) a malformation, congenital absence of any part of the body or organ. Aplasia - * aplasia * aplasia congenital absence or underdevelopment of cells. parts of the body, organ.
The causes of aplasia are external teratogenic factors (physical, chemical, biological) affecting the embryo directly or indirectly through the mother’s body. Aplasia can be observed in any human organ (brain, spinal cord, heart, lungs, genitourinary organs, etc.).
Aplasia of the skin can be combined with aplasia of deeper tissue, for example, with various forms of dysraphism (non-closure of embryonic fissures). Focal aplasia of the muscular layer of the gastrointestinal tract is of practical importance. Focal aplasia of the diaphragm leads to a false diaphragmatic hernia (see Diaphragm). Aplasia of the nerve cells of the Auerbach plexus can cause Hirschsprung's disease (see Megacolon).
Only a few dozen cases of splenic aplasia, which is usually combined with other severe congenital malformations, have been described in the world literature. Aplasia of the distal parts of the limbs should be distinguished from intrauterine amputation, most often caused by amniotic threads (see Amniotic threads, constrictions, adhesions).
Aplasia can be observed not only in the permanent tissues of the fetus, but also in the afterbirth (placenta, umbilical cord). Some types of aplasia (anencephaly, amyelia, acardius and bilateral renal aplasia) are incompatible with life. In the case of kidney aplasia, its function is performed by the second paired organ, which hypertrophies due to additional compensatory work.
Also, agenesis or aplasia can provoke kidney stones, arterial hypertension or pyelonephritis. With this anomaly, compensatory hypertrophy of the contralateral kidney is almost always observed. Bilateral renal aplasia is incompatible with life. Bilateral anomaly (complete absence of kidneys) - bilateral agenesis or arena. Aplasia of the right kidney is practically indistinguishable from agenesis, but the kidney is a rudimentary fibrous tissue without renal glomeruli, ureter and pelvis.
Agenesis of the right kidney can appear from the first days of birth if the left kidney is not capable of compensatory function. If the left kidney takes over the function of the missing right kidney, then agenesis of the right kidney practically does not manifest itself symptomatically and is discovered randomly. Ocular hypertelorism is not a specific symptom that indicates renal agenesis, but it often accompanies it in the same way as an enlarged abdomen and deformed lower limbs.
This anomaly is almost identical to agenesis of the right kidney, except that normally the left kidney should be slightly more advanced than the right. Agenesis of the left kidney is a more complicated case, since its function should be performed by the right kidney, which is more mobile and less functional by nature.
As a rule, underdevelopment of one of the kidneys is considered a relatively favorable anomaly compared to agenesis. Aplasia of the right kidney has a favorable prognosis; usually people with one kidney live a full, high-quality life. Aplasia of the left kidney, as well as aplasia of the right kidney, is quite rare, not more than 5-7% of all patients with anomalies of the urinary system. Aplasia is often combined with underdevelopment of nearby organs, for example, with an anomaly of the bladder.
Online consultations with doctors
| Consultation with a neurosurgeon |
| Consultation with a specialist in the field of stem cell treatment |
| Consultation with a reproductive specialist (diagnosis and treatment of infertility) |
| Pediatrician consultation |
| Consultation with a vascular surgeon |
| Family doctor consultation |
| Doctor consultation-ultrasound |
| Consultation with a urologist |
| Psychiatrist consultation |
| Consultation with a psychologist |
| Dentist consultation |
| Consultation with a plastic surgeon |
| Consultation with a cosmetologist |
| Genetic consultation |
| Consultation with an oncologist-mammologist |
Medical news
Football fans are in mortal danger, 01/31/2020
“Smart glove” returns grip strength to victims of injuries and strokes, 01/28/2020
An easy way to improve health has been named, 01/20/2020
Top 5 massage salons in Kyiv according to Purchase, 01/15/2020
Health news
The head of WHO declared a pandemic COVID-19, 03/12/2020
Coronavirus has already attacked more than 100 countries, almost 120,000 people have been infected, 03/11/2020
Coronavirus has attacked 79 countries, the number of victims is approaching 3,200 people, 03/04/2020
The new coronavirus has attacked 48 countries of the world, the number of victims is growing, 02/27/2020
Hypoplasia of the right vertebral artery
The cause of the defective structure of the second branch of the VA is often intrauterine anomalies. Their appearance can be triggered by the following factors affecting a pregnant woman:
- Injuries and bruises; Irradiation; Prolonged exposure to the sun; Alcohol and nicotine; Viral infection with influenza or rubella.
Signs of the disease usually overtake a person in adulthood. Intensity increases:
- Headache; High blood pressure – hypertension; Drowsiness; Emotional weakness with frequent mood swings, lethargy; Vestibular disturbances; Reduced sensitivity.
Other diseases from the group Diseases of the ear and mastoid process:
| Brain abscess |
| Cerebellar abscess |
| Adhesive otitis media |
| Adhesive otitis media |
| Ludwig's tonsillitis |
| Sore throat with measles |
| Sore throat with scarlet fever |
| Sore throat of the lingual tonsil |
| Nasal abnormalities |
| Atresia of the nasal cavity |
| Meniere's disease |
| Inflammatory diseases of the middle ear |
| Congenital preauricular fistula (parotid fistula) |
| Congenital anomalies of the pharynx |
| Hematoma and abscess of the nasal septum |
| Hypervitaminosis K |
| Hypertrophy of pharyngeal lymphoid tissue |
| Laryngeal sore throat |
| Diphtheria of the pharynx |
| Diphtheria of the nasal cavity |
| Zygomaticitis |
| Malignant tumors of the outer ear |
| Malignant tumors of the middle ear |
| Ulceration of the nasal septum |
| Foreign bodies in the nose |
| Foreign bodies of the ear |
| Deviated nasal septum |
| Paranasal sinus cysts |
| Labyrinthitis |
| Latent otitis media in children |
| Mastoiditis |
| Mastoiditis |
| Myringitis |
| Mucocele |
| Otitis externa |
| Otitis externa |
| Neuroma of the vestibulocochlear nerve |
| Sensorineural hearing loss |
| Nose bleed |
| Burns and frostbite of the nose |
| Tumors of the nose and paranasal sinuses |
| Orbital complications of diseases of the nose and paranasal sinuses |
| Osteomyelitis of the maxilla |
| Acute sinusitis |
| Acute purulent otitis media |
| Acute primary tonsillitis |
| Acute rhinitis |
| Acute sinusitis |
| Acute otitis media in children |
| Acute serous otitis media |
| Acute sphenoiditis |
| Acute pharyngitis |
| Acute frontal sinusitis |
| Acute ethmoiditis |
| Otoanthritis |
| Otogenic brain abscess |
| Otogenic meningitis |
| Otogenic sepsis |
| Otomycosis |
| Otosclerosis |
| Facial nerve paresis |
| Perichondritis of the external ear |
| Perforation of the eardrum |
| Petrosit |
| Damage to the nasal cavity due to influenza |
| Damage to the nasal cavity due to whooping cough |
| Damage to the nasal cavity due to measles |
| Damage to the nasal cavity in cerebrospinal meningitis |
| Ear malformations |
| Occupational ear diseases |
| Retronasal tonsillitis (acute adenoiditis) |
| Recurrent otitis media in children |
| Allergic rhinitis |
| Atrophic rhinitis |
| Vasomotor rhinitis |
| Simple chronic catarrhal rhinitis |
| Chronic hypertrophic rhinitis |
| Rhinogenic arachnoiditis |
| Rhinogenic meningitis |
| Rhinosinusogenic intracranial complications |
| Erysipelas of the nose |
| Sulfur plug |
| Sulfur plug |
| Goldenar syndrome |
| Konigsmarck syndrome |
| Treacher Collins syndrome (Franceschetti) |
| Synechiae of the nose |
| Chronic sinusitis |
| Scarlet fever in the nasal cavity |
| Subdural (intrathecal) abscess |
| Subdural abscess |
| Tympanosclerosis |
| Tympanosclerosis |
| Inner ear injuries |
| Throat injuries |
| External ear injuries |
| Injuries of the paranasal sinuses |
| Middle ear injuries |
| Ear injuries |
| Cavernous sinus thrombosis |
| Ear tuberculosis |
| Tubootitis (eustachitis) |
| Furuncle of the nasal vestibule |
| Cholesteatoma of the external ear |
| Chronic inflammatory diseases of the nasal cavity |
| Chronic suppurative otitis media |
| Chronic suppurative otitis media |
| Eczema of the outer ear |
| Eczema of the nasal vestibule |
| Exudative otitis media |
| Extradural abscess |
| Extradural abscess |
| Ulcerative-membranous sore throat of Simanovsky-Plaut-Vincent |
Pathological development of bone tissue
As in the cases described above, isolated bone aplasia is extremely rare. Thus, with such a pathology of the fibula, the patient’s limb is shortened, an equinovarus deformity of the foot develops (its anterior edge is raised and the outer edge is lowered), the tibia is bent, and the gastrocnemius and peroneal muscles are absent.
In medicine, cases of aplasia of individual parts of the body are recorded, often this happens to human limbs. This may be the absence of one or more fingers, or the entire hand or foot. It is not uncommon to have a missing forearm, lower leg, shoulder, or thigh in the presence of a foot or hand.
Diseases of the maxillary sinuses
The private name for inflammation of the maxillary sinuses is sinusitis. The term that summarizes the damage to the paranasal cavities is sinusitis. It is usually used until a definitive diagnosis is made. This formulation indicates the localization of the inflammatory process - the paranasal sinuses or, in other words, the sinuses.
Depending on the concentration of the disease, several types of sinusitis are distinguished:
right-sided, when only the right maxillary sinus is affected; left-sided, if the inflammation occurs in the left paranasal cavity; bilateral. This implies infection of both areas.
Under certain circumstances, inflammation is even visible in the photo: The maxillary sinus, in case of damage, has pronounced swelling. This symptom requires an immediate visit to a qualified doctor and taking the measures recommended by a specialist. Although, even in the absence of visual signs, it is necessary to promptly treat sinusitis. Otherwise, there is a risk of complications.
Causes of pathology
Many factors can trigger the process of hypoplasia. These include the following:
- Infection of the fetus during intrauterine development; Abuse of alcohol, nicotine, drugs, medications by a woman during pregnancy; Intoxication of the body of a pregnant woman during pregnancy; Hereditary predisposition to vascular pathology.
The lifestyle mentioned above during pregnancy is unacceptable. Some cases suggest that the presence of these factors is not necessary for hypoplasia to occur. It can start on its own spontaneously, regardless of the predisposing cause, even in a newborn. Provoking conditions that accelerate the appearance of hypoplasia are the following:
- Subluxation of the cervical vertebra; Spondylolisthesis leading to deformation of the spinal canal; Osteochondrosis, in which bone growths compress the arteries; Ossification that affects the spinoccipital membrane; Thrombosis of an internal anomalous vessel; Atherosclerotic changes.
Right frontal sinus cyst
A right sinus cyst can be recognized primarily by pain in the right frontal lobe, nasal congestion, and headache. It needs to be treated as quickly as possible. If the pathology is not treated in a timely manner, a fistula may develop, which is an opening through which pus and serous contents flow. Overflow may occur into adjacent areas. The most dangerous are considered to be effusion into the brain and orbit. Often, a cyst can be cured with conservative methods (only if treatment is started in a timely manner).
In other cases, surgical treatment is indicated.
Often diagnosis is based on subjective sensations. It is also possible that the pathology is discovered by chance during the diagnosis of another disease. The main diagnostic method is x-ray. During treatment you have to deal with ophthalmologists and neurologists. If the information obtained during the X-ray examination is not enough, CT and MRI are performed. Additionally, various procedures are used to restore local immunity. The swelling is removed and the frontal sinuses are washed. Often, cystic contents are emptied spontaneously through the nose. It must be borne in mind that clinical recovery does not occur in such a situation. Relapses are often observed; the cyst continues to fill with new contents. After spontaneous bowel movement, further treatment is necessary. The goal of such treatment should be to reduce the hypertrophied mucous membrane. This allows you to eliminate numerous symptoms of the disease. A frontotomy was previously performed. Today this method is practically not used because it is highly traumatic. Bleeding and postoperative complications often occur. The recovery period lasts a very long time. Cases of postoperative stenosis occur.
[], []
Hypoplasia of the left vertebral artery
Vascular pathology of the brain can spread to both one and another PA. In the case of left-sided hypoplasia, symptoms do not appear immediately. Pathology of cerebral vessels is compensated for a long time by the body’s mechanisms. Therefore, arterial dysfunction slowly sets in, which is manifested by difficulty in the passage of nutrients, blood stagnation, and ischemia.
Symptoms are gaining momentum along with age-related changes in tissues and organs. The main sign of damage to this branch of the VA is pain that spreads throughout the cervical spine. Trying to compensate for the reduced blood flow, the body creates anastomoses - vascular anastomoses. This allows blood to bypass the main path affected by hypoplasia. A change in condition for the worse usually leads to a decrease in the functionality of the anastomosis. Compensation is disrupted.
Malignant tumors of the maxillary sinus
In the vast majority of cases (80-90%), these tumors are epitheliomas; 10-12% are sarcomas, usually occurring in children and young people.
Symptoms and clinical course
extremely varied and depend on the stage and location of the tumor.
Latent stage
It is asymptomatic and most often goes unnoticed.
Stage of tumor manifestation
, in which the tumor, having reached a certain size, can be detected in the superolateral region of the nose or in the heteromandibular region.
The extraterritorialization stage
(Fig. 1) is characterized by the tumor extending beyond the maxillary sinus,
the metastasis stage
(can occur in the stage of tumor manifestation).
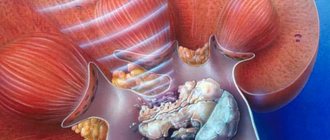
Rice. 1.
Extensive cancerous tumor of the left maxillary sinus with invasion into the orbit and other surrounding tissues
Exterritorialization stage
manifested by tumor growth into the orbit, manifesting itself on the affected side as diplopia, exophthalmos, ophthalmoplegia, ophthalmodynia, optic neuritis, chemosis and often orbital phlegmon.
Tumors of the maxillary sinus in the latent period are practically not recognized due to the fact that they pass in this period under the sign of a secondary inflammatory process, mistaken for a banal chronic sinusitis. In the advanced stage, the primary direction of tumor spread is the facial area.
The tumor can spread into the nasal cavity, causing obstruction, and affecting the olfactory nerves. Tumor growth through the posterior wall of the sinus leads to damage to the anatomical formations located in the pterygopalatine fossa, manifested by damage to the pterygoid muscles (trismus), nerve formations of the pterygopalatine ganglion (Slader syndrome: frequent sneezing, constant burning, boring pain in the inner corner of the eye, in the eye apple, nose, upper jaw, palate, unilateral lacrimation). In advanced cases, the tumor spreads to the cells of the ethmoid bone and adjacent areas (Fig. 2).
Rice. 2.
X-ray of right maxillary sinus cancer arising from the lateral wall of the sinus. The tumor has penetrated into the anterior and posterior cells of the ethmoid bone, the retrobulbar region and the pterygopalatine fossa
Complications
: “cancerous” cachexia, meningitis, hemorrhage, aspiration and metastatic bronchopulmonary lesions.
Diagnosis
causes difficulties in the latent period. In subsequent stages, the presence of characteristic oncological and clinical signs in combination with radiological (see Fig. 2) or CT data does not cause difficulties.
Differential diagnosis
carried out with common sinusitis, paradental cyst, benign tumors.
Forecast
plays an important role in determining treatment tactics and assessing its expected result; for widespread tumors and metastases - unfavorable.
Treatment
of malignant tumors of the upper jaw is carried out according to the same schemes as for lesions of the nasal cavity.
For tumors arising from the ethmoid labyrinth, a partial resection of the upper jaw is performed, limited to removing its upper part, the lower and medial wall of the orbit, the entire ethmoid bone, preserving the cribriform plate, as well as the own nasal bone on the affected side.
For tumors arising from the sinus itself, a total resection of the upper jaw is performed. This operation is the only option that allows you to completely remove the tumor of the upper jaw, but only if the tumor has not spread beyond the upper jaw.
For tumors arising from the alveolar process, partial resection of the lower part of the upper jaw is used; the extent of surgical intervention is determined by the extent of the tumor.
After surgery for cancer of the upper jaw, radiation therapy is performed. According to various authors, favorable results with this combination treatment are observed on average in 30% of cases. In other cases, relapses occur in the area of the ethmoid bone, orbit, base of the skull, pterygopalatine region, deep parts of the soft tissues of the face, etc. At the same time, chemotherapeutic antitumor agents are used.
Right transverse sinus disease
The sinus is the venous drainage. At its core, it is a collector that connects the internal vessels of the brain with external ones. The right transverse provides reverse suction of cerebrospinal fluid. From the collector, the blood flow rushes into the jugular veins and then moves into the intracranial space.
Disease of the right transverse sinus leads to a decrease in the venous lumen. This condition can cause a direct threat of hemorrhagic cerebral infarction. With hypoplasia of the left sinus, ophthalmological complications often occur. The venous drainage, located symmetrically to the right, when disrupted, causes swelling of the optic nerve head. The patient tends to complain of headaches, dizziness, and fatigue.
Features of therapy
To get rid of hyperplastic sinusitis, complex treatment is necessary. It includes the following steps:
- Eliminating the causes of inflammation.
- Therapy with antibiotics and anti-inflammatory drugs.
- Removal of mucous contents by rinsing.
- Instillation of vasoconstrictor drugs.
- Physiotherapy.
- Washing with antiseptics using a puncture.
If conservative treatment does not bring results, surgery is indicated, during which the overgrown tissue is removed. It should be remembered that it is simply impossible to completely cure chronic forms of sinusitis. Vasoconstrictor drugs have only a temporary effect. It is quite difficult to cure the disease. It is necessary to completely restore the basic functions of the nose and damaged mucous membranes.
A visit to physiotherapeutic procedures such as electrophoresis and UHF is recommended. It should be remembered that attending such sessions is often recommended after complete recovery to maintain immunity. Vitamin therapy and immunotherapy are used as additional methods
During the course of treatment it is extremely important to maintain a daily routine
Consequences of hypoplasia
The outcome of the disease and its complications are individual in each case. Sometimes a defective vessel does not make itself felt throughout life, while patients do not have severe symptoms. In other cases, cerebral vascular hypoplasia turns into a serious challenge for a person and can cause death or disability. The consequences of hypoplasia include:
- Increased risk of aneurysm and stroke; Hypertonic disease; Decreased general health with severe weakness.
The quality of life of such patients steadily suffers. There is no better way to help than to see a doctor in a timely manner and follow all his recommendations.
Signs of abnormal development
The absence of one of the organs affects the work of the other with increased load. Because of this, agenesis may often not be noticed in a newborn, and the anomaly will be detected only after some time with the help of diagnostic measures (computed tomography, ultrasound or urography).
The child may exhibit the following external signs:
- some puffiness of the skin of the face;
- slightly flat nose - the bridge of the nose is wider than usual, together with a flat back;
- the lobes of the frontal zone are quite convex;
- ears located below normal levels or with deformed areas.
Agenesis on the left side has more pronounced symptoms:
- the volume of urine per day is significantly increased;
- frequent urge to urinate;
- feeling of nausea, possibly vomiting;
- persistent hypertension;
- pain syndrome in the groin area.
In males, agenesis is more common due to the structural features of the genitourinary system. Specific symptoms are expressed due to the absence of a duct, which is responsible for the removal of seminal fluid and is caused by pain in the groin area during ejaculation, the sacral region, sexual dysfunction (impotence) and infertility are possible.
In most cases, female agenesis is accompanied by various pathologies of the uterus; vaginal underdevelopment or organ hypoplasia is possible.
Diagnostics
The gold standard for diagnosing renal agenesis is x-ray examination , which includes excretory urography, angiography of the renal vessels and cystoscopy. Radioisotope and ultrasound examinations are less informative and more expensive.
On excretory urography, contrast does not appear on the side of aplasia, which indicates the absence of renal vessels.
Cystoscopy reveals no ureteric orifice and reveals unilateral atrophy of the vesical triangle.
Ultrasound examination and vascular angiography show no signs of blood circulation and the ureter is underdeveloped or absent. The pedicle and pelvis are absent or incorrectly formed. The contralateral kidney is hypertrophied due to a compensatory mechanism.
Using laboratory research methods, such as general and biochemical analysis of blood and urine, it is possible to suspect kidney aplasia only at the stage of formation of chronic organ failure.
On palpation, the only kidney is enlarged in size and rarely painful.
Classification
Due to pathology:
- Hereditary.
- Acquired.
Clinical classification:
- Acute form. The clinical picture develops quickly, over the course of one month.
- Subacute. The development of symptoms is observed from a month to six months.
- Chronic form. The disease progresses slowly, over six months or longer.
According to the severity of granulocytopenia and thrombocytopenia, they are distinguished:
- Easy. At this level, platelets are more than 20*109/l, granulocytes are more than 0.5*109/l.
- Heavy. Platelets less than 20*109/l, granulocytes less than 0.5*109/l.
- Very severe. The first indicators are less than 20*109/l, the second indicators are less than 0.2*109/l.
Treatment and prevention
If the only healthy kidney functions normally, there are no symptoms and a characteristic enlargement of the organ is observed, then doctors will not take any additional actions to improve the functioning of the urinary system. The nephrologist will only prescribe dynamic monitoring of the kidney’s ability to produce and excrete urine, regular urinalysis and ultrasound examination.
Preventive actions are also provided that are aimed at preserving the functionality of the kidney:
- a diet that helps reduce the load on the only healthy organ is prescribed by a doctor, taking into account the individual characteristics of the patient;
- restrictions associated with contact sports (boxing, wrestling) to protect a healthy organ from injury and unnecessary damage;
- try not to lift heavy objects;
- maintain a constant body weight, avoid sudden weight loss;
- give up alcohol abuse and nicotine addiction;
- support the immune system with vitamins and minerals;
- avoid hypothermia to avoid the occurrence of infectious processes.
In the absence of function of the second kidney or with severe development of agenesis, when a healthy organ cannot cope with its work, intoxication with decay products and toxic substances occurs. In this case, hemodialysis and kidney transplantation are prescribed.
Tired of fighting kidney disease?
SWELLING of the face and legs, PAIN in the lower back, CONSTANT weakness and fatigue, painful urination? If you have these symptoms, there is a 95% chance of kidney disease.
If you care about your health , then read the opinion of a urologist with 24 years of experience. In his article he talks about RENON DUO capsules.
This is a fast-acting German remedy for kidney restoration, which has been used all over the world for many years. The uniqueness of the drug lies in:
- Eliminates the cause of pain and brings the kidneys to their original state. German capsules eliminate pain already during the first course of use and help to completely cure the disease. There are no side effects and no allergic reactions.