Kidney tumors account for 2-3% of all malignant neoplasms. Most often they occur between the ages of 40-60 years. Among all kidney tumors, 80-90% are renal cell carcinoma. In recent years, the likelihood of its detection has been increasing, which is associated both with the increase in the number of all malignant tumors and with early preclinical diagnosis. Recognizing malignant formations, first of all, is made possible by constantly improving and widely used ultrasound examinations of the kidneys.
The first report on the use of ultrasound in the diagnosis of kidney tumors was published in 1963 by J. Donald. Since then, the accuracy of ultrasound diagnosis of kidney tumors has increased from 85-90% to 96-97.3%. When using modern technologies operating in tissue and second harmonic modes, as well as color Doppler and dynamic echo-contrast angiography, the sensitivity of ultrasound (US) is 100% with a specificity of 92 and a predictability of a positive test of 98% and a negative test of 100%.
In the literature, there are often publications devoted to errors not only in ultrasound, but also in other methods of radiation diagnostics. There is a point of view that up to 7-9% of all volumetric processes in the kidneys cannot be differentiated from operations for cysts, tumors, abscesses, etc. . The picture of a kidney tumor with ultrasound and other radiation diagnostic methods can be simulated by many processes. Among them: various kidney anomalies; “complex” or mixed cysts; acute and chronic nonspecific inflammatory processes (carbuncle, abscess, chronic, including xanthogranulomatous pyelonephritis); specific inflammatory processes (tuberculosis, syphilis, fungal infections of the kidneys); changes in the kidneys with leukemia and lymphoma, including HIV infection; kidney infarctions; organized hematomas and other reasons.
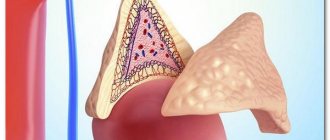
In this message we will only talk about kidney anomalies, which in the literature are defined by the term pseudotumors. With them, clinical manifestations are almost always absent or determined by concomitant diseases, and establishing the correct diagnosis is possible only by radiological diagnostic methods (Fig. 1).
Rice. 1.
Variants of pseudotumors that mimic a tumor.
A)
Fetal lobulation, “humpbacked” kidney.
b)
Hypertrophy of Bertin's column, enlarged “lip” above the renal hilum.
Materials and methods
For 1992-2001 177 patients with different structures of the renal parenchyma according to the type of renal pseudotumors were observed. All of them underwent repeated ultrasound scans of the kidneys, Doppler ultrasound (USDG) of renal vessels - 78, including using the second and tissue harmonic modes - 15, excretory urography (EU) - 54, X-ray computed tomography (X-ray computed tomography) - 36, renal scintigraphy or emission computed tomography (ECT) with 99 m Тс - 21.
Research results
Fetal lobulation of the kidney (see Fig. 1) with multiple protrusions along the lateral contour of the kidney was not considered in this report, since it did not require differential diagnosis with a kidney tumor. Among 177 patients with renal pseudotumors, 22 (12.4%) had a variant of the lobulated kidney - “humpbacked” kidney” (Fig. 2).
Rice. 2.
Pseudotumor “humpbacked” left kidney.
A)
Echograms.
b)
A series of computed tomograms.
In 2 (1.2%) patients, an enlarged “lip” above the renal hilum was noted (Fig. 3a-c).
Rice. 3 (a-c).
Pseudotumor is an enlarged “lip” of the kidneys on both sides.
A)
Echogram.
b)
Excretory urogram.
V)
Contrast-enhanced CT.
The most common cause of pseudotumor was “hypertrophy” of Bertin’s columns or “bridges” of the renal parenchyma - in 153 (86.4%) patients (Fig. 3 d-e). “Bridges” of the parenchyma were noted not only with various duplications of the renal pyelocaliceal systems, but also with their various fusions and incomplete rotations of the kidneys.
Rice. 3 (d-f).
Pseudotumor Bertin's hypertrophy (incomplete “bridge” of parenchyma) in the middle section of the right kidney.
G)
Echogram.
d)
Excretory urogram.
e)
Contrast-enhanced CT.
37 (21%) patients required differential diagnosis of pseudotumors and renal tumors. For this purpose, first of all, repeated “targeted” ultrasound scans were carried out using various additional ultrasound techniques in a urological clinic, as well as other methods of radiation diagnostics mentioned above. In only one patient with a pseudotumor of the kidney, an exploratory lumbotomy with intraoperative ultrasound-guided biopsy was performed to exclude the diagnosis of a tumor. In the remaining 36 patients, the diagnosis of renal pseudotumors was confirmed using radiation studies and ultrasound monitoring.
Difficulties and errors in radiological diagnostics for renal pseudotumors usually arose in the first pre-hospital stages of diagnosis. In 34 (92%) patients, they were associated with both objective difficulties in interpreting unusual echographic data, and their incorrect interpretation due to insufficient qualifications of specialists and the relatively low level of diagnostic equipment. In 3 (8%) patients, erroneous interpretation of X-ray computed tomography data was noted when there was a discrepancy between them and the data of repeated ultrasound scans and X-ray computed tomography in the urology clinic.
Kidney tumors that were combined with a pseudotumor in one kidney were verified in 2 patients after nephrectomy, and pseudotumors were verified in one patient during ultrasound-guided biopsy during exploratory lumbotomy; for the rest - with ultrasound monitoring for periods from 1 to 10 years.
Discussion
One of the most common causes simulating a kidney tumor on ultrasound, the so-called pseudotumor, is most often defined in the literature by the term hypertrophy of Bertin's column.
As is known, along the periphery of an ultrasound section of the kidney, the cortex forms invaginations in the form of columns (columnae Bertin) between the pyramids. Often Bertin's column extends quite deeply beyond the internal contour of the parenchyma into the central part of the kidney - into the renal sinus, dividing the kidney more or less completely into two parts. The resulting peculiar parenchymal “bridge” is the unresolved parenchyma of the pole of one of the kidney lobules, which merge into the kidney of an adult during the process of ontogenesis. The anatomical substrate of the “bridges” is the so-called connective tissue defects of the parenchyma or prolapse of the latter into the renal sinus. It consists of the cortex, Bertin's columns, and renal pyramids.
All elements of the “bridge” are normal parenchymal tissue without signs of hypertrophy or dysplasia. They represent a duplication of the normal renal cortex or an additional layer of it located lateral to the calyces. The latter is a variant of the anatomical structure of the parenchyma, in particular, the corticomedullary relationship between the parenchyma and the renal sinus. They can be most clearly seen on ultrasound and computed tomographic sections of the kidney.
The absence of hypertrophy or dysplasia of the parenchyma with the so-called hypertrophy of Bertin’s columns or “bridges” of the parenchyma was confirmed by histological studies of biopsy material in one patient with “bridges” of the parenchyma, which were taken before explorative lumbotomy for a kidney tumor, as well as in two patients during a morphological study of the kidneys, removed due to a combination of a tumor and a pseudotumor (“bridges” of parenchyma) in one kidney.
In this regard, in our opinion, the term hypertrophy of Bertin's columns, which is most often found in the literature, does not reflect the morphological essence of the substrate. Therefore, we, like a number of authors, believe that the term “bridge” of parenchyma is more correct. We used it for the first time in the domestic literature on ultrasound diagnostics in 1991. It should be noted that the term “bridge” of parenchyma had other names in the literature (table).
Table
. Terms used to describe the “bridges” of the renal parenchyma (according to Yeh HC, Halton KP, Shapiro RS et al., 1992).
| Origin or nature of the fabric | Terms | Authors |
| Hypertrophied or unusually wide tissue | Hypertrophied Bertin's column | Lafortune M et al., 1986 Wolfman NT et al., 1991 Leekman RN et al., 1983 |
| Focal cortical hyperplasia | Popky G.L. et al., 1969 | |
| Wide arcade | Hodson CJ et al., 1982 | |
| Incorrectly positioned or displaced tissue | Lobar dysmorphism | Carghi A et al., 1971 Dacie JE, 1976 |
| Incorrect position of the renal lobe | Carghi A et al., 1971 | |
| Cortical folds | King MC et al., 1968 | |
| "Kidney" within a kidney | Hodson CJ et al., 1982 | |
| Cortical intussusception and prolapse of Bertin's columns | Lopez FA, 1972 | |
| Mass or pseudo mass | Renal pseudotumor | Felson B et al., 1969 Lopez FA, 1972 |
| Glomerular zone of pseudotumor | Hartman GW et al., 1969 | |
| Renal-cortical nodule | Wolfman NT et al., 1991 | |
| Primary cortical nodule | Thornbury JR et al., 1980 | |
| Intermedial cortical mass | Netter F et al., 1979 | |
| Embryonic anomaly | Aberrant lobule of renal tissue | Meaney T.F., 1969 |
| Benign cortical caesura | Flynn VJ et al., 1972 | |
| Cortical islet of the kidney | Flynn VJ et al., 1972 | |
| Developed (perfect) anomaly | Failed attempt at duplication of renal parenchyma | Dacie JE, 1976 |
| Supernumerary share | Accessory renal lobe | Palma L.D. et al., 1990 |
Many years of experience in excretory urography have shown that the collecting system has an extremely large number of structural options. They are practically individual not only for each person, but also for the left and right kidneys in the same subject. With the development and increasingly widespread use of ultrasound and X-ray CT, which makes it possible to trace both the internal and external contours of the renal parenchyma, in our opinion, a similar situation is emerging with regard to the variants of the anatomical structure of the renal parenchyma. A comparison of echo and computed tomographic data with urographic data for various types of renal pseudotumors showed that there is a relationship between the anatomical structure of the parenchyma and the renal collecting systems. It is expressed in the congruence of the medial contour of the parenchyma in an echo or computed tomographic image with the lateral contour of the pyelocaliceal systems, conventionally drawn on excretory urograms or on contrast-enhanced computed tomograms. This symptom can be traced with the usual structure of the parenchyma and pyelocaliceal systems, as well as with the “bridge” of the kidney parenchyma, which is a variant of the anatomical structure. With a kidney tumor, which is an acquired pathological process, the congruence of the contours of the parenchyma and the renal pyelocaliceal systems is disrupted (Fig. 4).
Rice. 4.
A symptom of congruence of the contours of the parenchyma and the renal pyelocaliceal system with an incomplete “bridge” of the parenchyma (explanation in the text).
conclusions
Thus, the typical echographic images of a “bridge” of the renal parenchyma, a “humpbacked” kidney and an enlarged “lip” above the renal hilum without signs of dilation of the pyelocaliceal systems, first identified by ultrasound, do not require further examination.
If differential diagnosis of pseudotumors and renal tumors is necessary, which was required in 37 (21%) patients, we propose the following algorithm for their diagnosis (Fig. 5).
Rice. 5.
Radiation diagnostic algorithm for renal pseudotumor.
- Repeated ultrasound by qualified specialists of a higher class using ultrasound, mapping techniques, tissue and second harmonics.
- X-ray computed tomography with contrast enhancement or excretory urography with comparison of uro- and echographic data and data from repeated “targeted” ultrasound.
- The methods of choice are renal scintigraphy or emission computed tomography with 99 m Tc (false-negative results are possible for small tumors).
- If there is still suspicion of a malignant tumor, a biopsy under ultrasound guidance (only a positive result has diagnostic value).
- If the biopsy result is negative or the patient refuses a biopsy and surgical revision of the kidney, ultrasound monitoring is performed at least once every 3 months in the first year of observation, and then 1-2 times a year.
Literature
- Demidov V.N., Pytel Yu.A., Amosov A.V. // Ultrasound diagnostics in urology. M.: Medicine, 1989. P.38.
- Hutschenreiter G., Weitzel D. Sonographic: einewertwolle erganzung der urologichen Diagnostic // Aktuel. Urol. 1979. Vol. Bd 10 N 2. P. 45-49.
- Nadareishvili A.K. Diagnostic capabilities of ultrasound in patients with kidney tumors // 1st Congress of the Association of Ultrasound Diagnostics in Medicine: Abstracts of reports. Moscow. October 22-25, 1991. P.121.
- Buylov V.M. Complex application and algorithms of ultrasound scanning and x-ray diagnostics for diseases of the kidneys and ureters: Dis. ... doc. honey. Sci. M., 1995. P. 55.
- Modern ultrasound diagnostics of volumetric formations of the kidneys / A.V. Zubarev, I.Yu. Nasnikova, V.P. Kozlov et al. // 3rd Congress of the Association of Ultrasound Diagnostics Specialists in Medicine: Abstracts of reports. Moscow. October 25-28, 1999. P. 117.
- US, CT, X-ray diagnosis of Renal Masses / RK Zeman, JJ Croman, AT Rosenfield et al. // Radiographics. 1986. Vol.6. P. 351-372.
- Thomsen HS, Pollack HM The Genitourinary System // Global TextBook of Radiology. (Ed.) Petterson H. 1995. P. 1144-1145.
- Lopatkin N.A., Lyulko A.V. Anomalies of the genitourinary system. Kyiv: Zdorovya, 1987. pp. 41-45.
- Mindel HJ Pitfalls in Sonography of Renal Masses // Urol. Radiol. 1989. 11. 87. N 4. R. 217-218.
- Burykh M.P., Akimov A.B., Stepanov E.P. Echography of the kidney and its pyelocaliceal complex in comparison with data from anatomical and x-ray studies // Arch. Anat. Gistol. Embryol. 1989. T.97. N9. P.82-87.
- Junctional Parenchyma: Revised Definition of Hypertrophic Column of Bertin / H-Ch. Yeh, PH Kathleen, RS Shapiro et al. // Radiology. 1992. N 185. R. 725-732.
- Bobrik I.I., Dugan I.N. Anatomy of the human kidneys during ultrasound examination // Doctor. case. 1991. N 5. P. 73-76.
- Khitrova A.N., Mitkov V.V. Renal ultrasound: Clinical guide to ultrasound diagnostics. M.: Vidar, 1996. T. 1. S. 201-204, 209, 212.
- Builov V. Junctional parenchyma or hypertrophic column of Bertini: the congruence of their contours and calyceal-pelvic system // Abstracts of ECR "99, March 7-12. 1999. Vienna Austria.-Europ. Radiol. Supp.1. Vol.9. 1999. S.447.
- Builov V.M., Turzin V.V. Echotomography and excretory urography in the diagnosis of “bridges” of the renal parenchyma // Vestn. radiol.radiol. 1992. N 5-6. pp. 44-51.
- Builov V.M., Turzin V.V. Diagnostic value of atypical “bridges” of parenchyma during sonography of the kidneys // 1st Congress of the Association of Ultrasound Diagnostics in Medicine: Abstracts of reports. Moscow. October 22-25, 1991. P. 121.
- Buylov V.M. Questions of terminology and a symptom of congruence of the contours of “hypertrophied” columns of Bertini or “bridges” of the parenchyma and pyelocaliceal systems of the kidneys // Vestn. rentgenol. and radiol. 2000. N 2. P. 32-35.
- Buylov V.M. Algorithm for radiodiagnosis of renal pseudotumors // Abstracts of reports. 8th All-Russian Congress of Radiologists and Radiologists. Chelyabinsk-Moscow. 2001. pp. 124-125.
Bertini pillars or columns. Why do you need that?
— @kasaton, they were found in the child, only the nephrologist from the clinic said that in 63 years of her work she had heard about them for the first time, and gave a referral to the Filatov hospital. I would like to know who has encountered this and what it is
— @marishes, well, I’ll say that either you had a CT scan, or a really good ultrasound specialist and they got the device. These columns are a normal structure of the renal cortex, sometimes one of them is somewhat “thicker” and with a truly well-performed ultrasound is visible as a bridge. Of course, there are also complete/incomplete bridges as a development option - then they will perform excretory urography (a series of X-rays with contrast), I think they will simply redo the ultrasound and everything will calm down
If the uzist is questionable and the device is so-so, then a column could actually be called incomplete doubling or other developmental anomalies. If you redo it, it won’t matter, especially if there is no clinic and the tests are not bad
First they did it in a regular clinic, where they discovered just a neoplasm, and then they changed it at the oncology center, where they have a good ultrasound specialist and a device, and they already said that it was a Bertini column and sent it to a nephrologist, but she doesn’t know what it is. Just live with this, won't it go away over time? @kasaton,
— @marishes, something with the comments, I just got a notification. Well, that means my first guess was correct - he’s a good uzologist