Causes of pheochromocytoma
to contents
What hormones does pheochromocytoma produce when it is first diagnosed?
Pheochromocytoma is a tumor of the adrenal medulla that produces catecholamine hormones: adrenaline, norepinephrine and dopamine. The biological effects of these hormones determine all the symptoms of the disease, which I will talk about later.
This is a fairly rare type of tumor. Prevalence - 2: 1000 in the population. Of all patients with arterial hypertension, pheochromocytoma is found in 0.3-0.7%. This tumor has been described in all age categories, from newborns to the elderly. Most often occurs in women 30-50 years old.
to contents
Extra-adrenal localization of pheochromocytoma
In 10% of cases, pheochromocytoma is formed not in the adrenal medulla, but in the structures of the sympathetic nervous system (nerve ganglia). For example, in the nodes of the retroperitoneal space, chest, aorta, celiac node, bladder, hilum of the liver and kidneys. In this case, we are talking about extra-adrenal localization.
to contents
Is pheochromocytoma a malignant or benign tumor?
In 10% of cases, pheochromocytoma affects both adrenal glands and is hereditary. These are usually large benign tumors (up to 15 cm) and grow slowly.
In 6-10% these are still malignant forms of the tumor. The cause of pheochromocytoma, as well as most tumors, is currently unknown.
to contents
Pheochromocytoma of the adrenal gland: ICD code 10
According to the classification of diseases, pheochromocytoma is assigned the code E27.5
to contents
Adrenal adenoma in women: symptoms, ICD 10 code, removal and treatment with folk remedies
The adrenal glands are responsible for metabolism in the body and for adapting the body to unfavorable external conditions. Benign tumors that arise in this organ usually do not pose a mortal danger to humans. One of the popular ones is adenoma.
Concept
This is a benign formation that forms in the adrenal cortex. Most often appears in one of the organs.
The tumor is a small formation, inside of which there is the same type of content. The development of the disease occurs gradually. The greatest danger is the possibility of degeneration of a benign tumor into a malignant one.
Benign neoplasms in the adrenal glands according to ICD-10 have code D35.0. According to WHO statistics, the disease occurs in every 20 adults. Adenomas frolicking in children are also mentioned in the medical literature.
The disease is more often found in women over forty years of age. It is noted that the formation has clear edges; the capsule is examined using diagnostic equipment.
The weight of the tumor ranges from 10 to 100 g. The larger the formation, the greater the likelihood of its transformation into a malignant tumor.
Classification
There are three types of adenoma based on morphological characteristics:
- Adrenocortical. Occurs most often. It is a capsulated node. Under a microscope, it can be revealed that the tumor is created from polygonal cells.
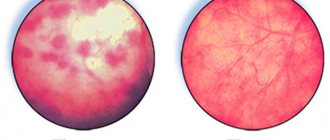
- Pigmented. It contains dark-colored cells. That's why the tumor itself is purple. The size of such a formation can reach 2-3 cm. Sometimes accompanied by Cushing's syndrome. On computed tomography, the tumor has high radiation density with a fibrous capsule. The mass of the formation does not exceed 35 g.
- Oncocytic. It is rare and often functionally inactive. It has a reddish-brown or ivory color. Consists of large cells with granular cytoplasm. The latter are a consequence of the increased number of mitochondria.
Causes
The exact reasons for the formation of adenoma have not been established. People who smoke are at risk, since nicotine provokes the formation of tumors.
The cause of growth is hormonal changes. Therefore, the disease is more often found in women taking hormonal contraceptives.
Among the reasons for the formation is:
- polycystic ovary syndrome,
- diabetes mellitus second degree,
- excess body weight,
- disruptions in the functioning of the cardiovascular system,
- injuries to internal organs,
- insufficient production of hormones.
Symptoms of adrenal adenoma
At first, when a tumor forms, there are no symptoms. Since the adrenal glands are responsible for the production of hormones, the following occurs:
- Kohn's syndrome. Aldosterone levels increase.
- Cushing's syndrome. Cortisol increases.
Over time, there is an increase in body weight due to hormonal disorders, and a regular increase in blood pressure. Most often, symptoms manifest as a whole complex.
If the tumor is large, an excess amount of body hair appears, women experience menstrual irregularities, and problems with conception appear. In men, the figure takes on feminine forms, the mammary glands increase significantly.
Patients note:
- arrhythmia,
- trembling of limbs,
- frequent urination,
- weakening of muscles,
- skin atrophy,
- convulsions.
Hormonal changes lead to nervous disorders. There is a sharp change in mood, depression, and tearfulness.
Diagnostics
The studies take place under the supervision of a radiologist and endocrinologist. Held:
- CT scan,
- MRI,
- endocrine tests.
The first two types of research make it possible to timely identify malignant changes, as well as determine the location and type of tumor. Hormone tests measure the levels of hormones produced by the adrenal glands.
Additionally, a biopsy and brain tomography are prescribed. A biopsy reveals the origin of the tumor and determines its structure.
Modern research methods can detect tumors as small as 5 mm.
In 13% of cases, even small adenomas degenerate into cancer, so it is necessary to carry out diagnostic measures in a timely manner.
In the video, ultrasound diagnosis of an adenoma of the right adrenal gland:
Treatment of adrenal adenoma
Small hormonally inactive tumors require only dynamic monitoring. If the formation is larger than 4 cm or produces hormones, surgical treatment is used.
Adenoma removal occurs in two ways:
- Laparoscopy. Effective for small tumors located on one side only. This is a minimally invasive technique, so the patient stays in the hospital for about six days. The sutures heal quickly.
- Abdominal surgery. It is used for bilateral damage to the adrenal glands. Patients require long-term recovery after manipulation.
After the operation, hormone therapy is started, aimed at restoring hormonal balance. In rare cases, radiation and chemotherapy are prescribed.
Doctors who practice traditional methods of treatment recommend using herbs. Snowdrop tincture will help reduce the size of the formation. They are placed in a jar and filled with water. Infuse for about 40 days. Take 20 drops twice a day.
Geranium, from which a decoction is made, stimulates the adrenal glands. Reducing hormonal production is possible with the help of mulberry. The decoction is drunk instead of water.
In conclusion, we note that preventive measures are aimed at preventing the recurrence of the tumor. To do this, you need to periodically donate blood for hormones and do an ultrasound. These procedures are prescribed twice a year.
For small adenomas the prognosis is favorable. If a benign tumor begins to transform into a malignant one, the prognosis depends on the origin, stage and presence of concomitant pathologies.
Source: https://gidmed.com/onkologiya/lokalizatsiya-opuholej/endokrinnye-zhelezy/adenoma-nadpochechnika.html
Pheochromocytoma: symptoms and signs of the disease
Signs of pheochromocytoma are due to the biological effects of catecholamines. Biological effects of catecholamines:
- They are neurotransmitters (transmitters of nerve impulses) in the nervous system.
- They activate the breakdown of fats, while fats act as “energy fuel” for muscles.
- Reduce insulin secretion (have a counter-insular effect).
- They release glucose from the depot, which is glycogen in the liver.
to contents
Forms of adrenal tumor - pheochromocytomas
According to the clinical course, the main forms of pheochromocytoma can be distinguished:
- Paroxysmal, i.e. sudden with characteristic crises (this is a classic course).
- Constant, i.e. a persistent increase in blood pressure without crises.
- Mixed, i.e. crises against the background of constant high blood pressure.
- Latent, i.e. asymptomatic, which occurs in 1-2% of cases.
to contents
Pheochromocytoma: what patients look like (photo)
The clinical picture of pheochromocytoma is divided into several groups (syndromes):
- Cardiovascular syndrome or what causes increased blood pressure. It manifests itself as an increase in blood pressure to high numbers, pain in the heart, rapid pulse (tachycardia), and various heart rhythm disturbances (arrhythmias). Arterial hypertension in pheochromocytoma is entirely due to the action of excess amounts of adrenaline and norepinephrine on the receptors of blood vessels and the heart, which causes spasm and increased heartbeat.
- Neuropsychiatric syndrome. Outside of a crisis, frequent headaches, hand tremors (tremors), sweating, fatigue, and a sharp decrease in memory are disturbing.
- Abdominal syndrome. The symptoms are similar to those for diseases of the gastrointestinal tract - nausea, sometimes vomiting, abdominal pain, constipation, and during a crisis there may be a picture of an “acute” abdomen.
- Endocrine metabolic syndrome. Symptoms: weight loss, impaired carbohydrate metabolism, and possibly even the development of secondary diabetes.
- Hematological syndrome. On the blood side, there is an increase in the total number of leukocytes (hyperleukocytosis), an increase in glucose, which can return to normal 5 hours after the crisis, and an increase in blood clotting.
- Tumor syndrome. It manifests itself as pain in the lumbar region on the side of the tumor.
If you want to see photos of patients in the hope that you will find some specific external manifestations, then you will be disappointed, because such patients do not look any different from healthy people. Unless they express subjective complaints related to one or another syndrome described above.
to contents
Adrenal adenoma in women: symptoms, diagnosis and treatment
Adenoma of the left or right adrenal gland in women is a serious pathology: the symptoms and treatment of the disease depend on its type and stage.
Timely diagnostic and treatment measures can stop the development of the disease and prevent the occurrence of complications.
What kind of pathology is this and which doctor should I contact?
Adrenal adenoma is a benign neoplasm located on the adrenal cortex, filled with homogeneous contents.
It can affect one adrenal gland or both at once.
The danger of the disease is that if left untreated, a benign tumor can develop into a malignant one . The disease develops more often in women than in men. In rare cases, it occurs in children.
An endocrinologist is involved in diagnosing and treating this disease . ICD code: D35.0.
Classification
There are several types of the disease. Taking into account the general morphological characteristics of adenoma, the following types are distinguished:
- Adrenocortical. It resembles the shape of a nodule that is placed in a capsule. There is a light liquid inside. As the disease progresses, it becomes more numerous.
- Oncocytic. It is formed from large cells and has a granular structure. The formation is quite large in size.
- Pigmented. So named because it contains a dark purple-colored liquid. Its quantity increases with the development of the disease.
There are different types of pathology based on the size of the formation :
- Picoadenoma. In this case, the dimensions of each side do not exceed three mm.
- Microadenoma. The tumor size does not exceed 10 mm.
- Macroadenoma. Sometimes more than 10 mm.
- Giant adenomas. They are very rare, lead to a severe course of the disease, from 40 mm in diameter. It is quite difficult to cure a patient with such an adenoma.
According to experts, tumors larger than 30 mm are malignant in 95% of cases.
That is why education should not be allowed to grow. The sooner it is eliminated, the better.
Adenomas are also distinguished by color :
- Clear cell. The neoplasm is light in color and contains a white, slightly yellowish liquid inside. Sometimes it is almost transparent.
- Dark cell. They have a dark tint. Inside there is a dark-colored liquid, often dark yellow and dark brown.
Symptoms of the disease
Vary depending on the gender of the person .
Among women
In females, the disease manifests itself as follows:
- increase in body weight.
- the muscles and bones of the limbs become weak.
- menstrual irregularities.
- infertility.
- weakness.
- dizziness.
- improper metabolism.
- the face becomes round, the cheeks increase in size.
- the voice becomes low.
- body hair grows rapidly.
in men
Symptoms of the disease in men include:
- disruption of the digestive system.
- increase in body weight.
- thinning of the skin.
- bones and muscles become weak, making it difficult for them to withstand daily physical activity.
- decreased erection.
- impotence.
- reduced performance.
Read our article about the symptoms of chronic prostatitis in men.
causes of disease in women and men
The disease appears for various reasons. In women, adenoma develops according to the following factors and ailments:
- Hereditary predisposition.
- Hormonal disbalance.
- Taking oral contraceptives.
- Poor nutrition.
- Stress.
- Bad habits.
Men face pathology for the following reasons:
- Smoking.
- Drinking alcoholic beverages.
- Poor nutrition.
- Genetic predisposition.
- Hormonal imbalance.
How to treat?
Specialists prescribe medications to patients that normalize hormonal levels . If it stabilizes, the swelling will go away. Such drugs include:
- Cyclodinone.
- Regulon.
- Mercilon.
- Logest.
To restore hormonal levels, injections may also be prescribed on an individual basis after studying the patient’s tests. The missing hormones are administered through injections in the hospital in strictly designated quantities. It is impossible to predict the hormone administered; it all depends on the stage of the disease.
The missing hormone may vary from person to person.
Other medications are powerless in treating adenoma. In the early stages, experts prescribe the use of folk remedies . Some infusions also help normalize hormonal levels.
An infusion of snowdrop flowers is effective . To do this, mix a glass of boiling water and two tablespoons of the plant. It is necessary to insist for four hours, then filter the solution. Drink it half a glass 2 times a day.
It is recommended to use lungwort infusion . To do this, mix 200 ml of boiling water and a teaspoon of the plant. The mixture is infused for one hour, then it is filtered and consumed 1/3 cup in the morning and evening.
If the disease does not go away even after this, specialists prescribe surgery . The operation involves removal of the adenoma. It is performed under anesthesia for 1-1.5 hours. The person recovers for two weeks, but still sees a doctor for another month and follows his advice.
Consequences of the operation that the patient may encounter during the rehabilitation period are:
- Weakness.
- Pain in the abdomen, back, limbs.
- Lack of appetite.
- Pallor.
Learn more about adrenal adenoma, treatment and diet from the video:
Source: https://opochke.com/nefrologiya/nadpochechniki/adenoma-u-zhenshhin-simptomy-i-lechenie.html
Pheochromocytoma and pregnancy
The tumor was first described in a woman in labor 60 years ago, when a 28-year-old woman died 3 hours after childbirth. An autopsy revealed a pheochromocytoma. It often happens that the manifestation of a tumor is confused with late gestosis, preeclampsia in a pregnant woman. And during childbirth, internal bleeding is mistakenly diagnosed, and after childbirth - uterine rupture and air embolism.
Even with today's medical advances, this pathology poses a serious danger to the life of not only the mother, but also the fetus. Therefore, the doctor is required to promptly identify the cause of toxicosis during pregnancy and prescribe effective treatment. Only in this case can the probability of maternal mortality decrease from 58% to 12%, and newborn mortality from 56% to 40%.
In addition, it is extremely contraindicated to give birth naturally with pheochromocytoma, therefore a cesarean section is performed.
to contents
Reasons for development[ edit | edit code]
The cortex and medulla can together serve as excellent soil for the formation of the disease adrenal adenoma. The reasons for the development are not fully known.
Experts say that smokers have an increased chance of developing adrenal adenoma. The reasons for the further development of the disease lie in the purpose of the cortical layer on which the adrenal adenoma is formed. The reasons are as follows: the adrenal cortex is necessary for the production of a number of steroids: androgens in men, estrogens in women. Adrenal adenoma, which is caused by the appearance of tumor cells on the cortex, begins to affect the amount of hormones produced by the adrenal gland. [2]
Pheochromocytoma in children
The first report of pheochromocytoma in a child was in 1904. Boys get sick more often than girls. It is more common in children over 8 years of age.
At the very beginning of the disease, symptoms are nonspecific, and the correct diagnosis is rarely made. Symptoms of pheochromocytoma, such as fatigue, are accompanied by nausea, vomiting, loss of appetite, weight loss, and pale skin.
Subsequently, a severe hypertensive crisis suddenly occurs, which is accompanied by headache, severe pallor, severe sweating, rapid heartbeat, nausea, and vomiting. Sometimes loss of consciousness, convulsions, foam at the mouth, and involuntary urination occur.
The attack lasts from 10-15 minutes to 1-2 hours. Blood pressure increases and reaches 170-270/100-160 mm Hg. Art. Over the next few days, there is a moderate, persistent increase in blood pressure, heart rate, and sweating.
A repeated crisis does not keep itself waiting and repeats after 1-6 months with an even greater increase in blood pressure, already up to 300/260 mm Hg. Art. and pulse up to 200 beats per minute. Subsequently, such conditions become more frequent up to 2-3 times a week, and in some children up to several times a day.
In most children, blood pressure was measured in isolated cases and, as a rule, only a year after the onset of obvious symptoms of the disease. Due to late diagnosis, these children begin to develop irreversible processes in the myocardium, as well as in the fundus.
How to identify this disease in a timely manner, read the article “Diagnostics of pheochromocytoma” .
to contents
Normal anatomy of the adrenal glands
The right adrenal gland is slightly smaller than the left and has the shape of a triangle, the left one resembles a crescent. The adrenal gland has anterior, posterior and inferior surfaces. The anterior surface is in contact with neighboring organs; as a rule, one groove runs along it - the gate ( hilus
), through which the main vein, v., leaves the adrenal gland
.
centralis . The posterior surface is loosely delimited from the diaphragm. The lower (renal) surface is somewhat concave and adjacent to the upper pole of the kidney. The front and back surfaces are separated by a sharp edge.
The adrenal glands have a deep topographic and anatomical location. They are located in the retroperitoneal fatty tissue under the diaphragm between the layers of the perirenal fascia at the superomedial surface of the poles of the kidneys, located on the sides of the spinal column at the level of the ThXI-XII and LI vertebrae. The projection of the adrenal glands onto the anterior abdominal wall corresponds to the epigastric region, partially to the right and left hypochondrium (Fig. 41-1).
Rice. 41-1. Topographic-anatomical location of the adrenal glands: 1 – right renal vein; 2 – renal artery; 3 – inferior adrenal artery; 4 – middle adrenal artery; 5 – superior adrenal artery; 6 – central adrenal vein; 7 – adrenal gland; 8 – inferior vena cava; 9 – aorta.
The main sources of arterial blood supply are the middle, superior and inferior adrenal arteries, which arise from the aorta, inferior phrenic and renal arteries, respectively. The outflow of venous blood from the adrenal glands occurs through the central veins, emerging onto the anterior surface of the adrenal gland, often at the border of the middle and upper third, and flowing into the lateral or posterior wall of the inferior vena cava at an angle of 80-90°. The walls of the veins are thin, almost devoid of muscle elements. Their length does not exceed 8-10 mm, and their diameter is often greater than their length. There are various features of the flow of the central vein of the right adrenal gland: into the hepatic, cava, renal veins or into the angle between the cava and renal veins. There are cases when two, and sometimes three large veins emerge from the right adrenal gland, which flow into the inferior vena cava. The central vein of the left adrenal gland in all cases enters the anterior surface of the adrenal gland at the border of the middle and lower third and, heading down, flows into the renal vein at an angle of 30-35°. The length and width of the left adrenal vein is significantly greater than the right one. Its greatest extent (up to 3-4 cm) is noted in people of brachymorphic physique, the smallest (up to 2.0-1.8 cm) - dolichomorphic. In almost all patients, the inferior phrenic vein flows into the central vein of the left adrenal gland at a distance of 0.5 cm from its exit from the adrenal gland.
Hypertensive crisis with pheochromocytoma
The increase in blood pressure in this disease is of a crisis nature, that is, the pressure rises sharply and suddenly. The numbers are very high and reach values above 200 mmHg. Since catecholamines are quickly destroyed and their release from the adrenal glands stops, the attack can stop on its own, but you shouldn’t wait for it.
Attacks can recur in different ways, for some once every six months, and for others 2-3 times a week. There are no specific features of a crisis caused by pheochromocytoma. It can masquerade as ordinary hypertension and is accompanied by the same symptoms, only intensified.
to contents
Treatment
If a patient has been diagnosed with a tumor in the adrenal glands, then it is necessary to conduct medical tests to determine the exact diagnosis and the extent of damage to the gland and other organs.
Treatment for tumors on the adrenal gland depends on the type of tumor.
The main type of treatment for tumor pathologies is surgery. The operation is performed if the size of the tumor is more than 3 cm, it is hormonally active and has signs of malignancy.
After surgery, the patient is prescribed a course of hormonal therapy to restore the functioning of the gland and normalize hormone levels.
But this type of treatment is not suitable for all categories of patients. The operation is not performed if:
- the patient has pathologies for which surgical intervention is contraindicated;
- the disease has progressed so much that metastases have appeared in organs distant from the lesion;
- Due to his advanced age, the patient may not be able to tolerate the intervention.
In critical cases, when tumor removal is impossible, only courses of chemotherapy are used. With this method of treatment, the tumor is treated with drugs that kill cancer cells.
A catecholamine crisis should not be confused with a hypertensive crisis!
Catecholamine crisis is the most severe complication of pheochromocytoma, which occurs in approximately 10% of patients, more often in children than in adults. There are 4 stages of catecholamine crisis :
- Initial: a sharp increase in blood pressure, a feeling of anxiety, severe weakness, chilliness, increased heart rate, body temperature may rise.
- Peak development: sweating, shortness of breath, severe headache, decreased hearing and vision, convulsions, acute myocardial infarction or cerebral stroke may develop.
- Reverse development: decreased blood pressure, frequent urination, a state of euphoria, weakness, even asthenia.
- Post-crisis: collapse (a sharp decrease in blood pressure) or uncontrolled hemodynamics may develop, i.e., a chaotic alternation of episodes of low and high blood pressure that is difficult to treat.
If there is a tendency towards low blood pressure, then this is an ominous harbinger of death and is no longer supported by the administration of drugs that raise blood pressure.
A catecholamine crisis can occur after a stressful situation, a heavy meal or, conversely, during fasting, during hypothermia, after a change in body position in space.
But despite the severity and danger of this condition, it is possible to independently stop the catecholamine crisis. However, due to the high mortality rate, in each case the maximum number of measures is taken in the shortest possible time.
to contents
Causes of the disease
The reason that causes the growth of adenoma in the tissues of the adrenal glands is not exactly known to doctors. Research into this pathology is still underway. Experts identify a number of factors that can provoke the disease:
- hereditary predisposition;
- active production of hormones;
- decreased protective functions of the body;
- being in a stressful state for a long time;
- high blood pressure;
- previous heart disease - heart attack, stroke;
- metabolic disorders;
- injury or surgical intervention of neighboring tissues or organs;
- endocrine system disease – diabetes mellitus;
- excess body weight;
- abuse of nicotine and alcoholic beverages;
- age after 30 years.
Pheochromocytoma: prognosis for life
If the tumor is benign, then the prognosis for life is favorable. After removal of the tumor, it is possible to normalize blood pressure and get rid of negative symptoms. The 5-year survival rate for benign tumors reaches 95%, and for malignant tumors – 44%.
Relapses occur rarely, in only 12% of cases, but in order to detect them in time, an annual examination by a specialist is recommended. Read about how to get rid of a dangerous disease in the article “Effective treatment of pheochromocytoma” .
Diagnostics
To identify an adenoma in the adrenal gland, it is necessary to carefully examine it.
Often formations are detected accidentally during instrumental diagnostics of the abdominal organs:
- CT scan,
- MRI,
- Ultrasound.
To find out the hormonal activity of the tumor, you need to undergo laboratory tests:
- daily urine to determine cortisol levels,
- blood test for hormones,
- dexamethasone examination (to diagnose Itsenko-Cushing syndrome),
- blood plasma examination to detect the breakdown of catecholamines.
Laparoscopy and collection of material for histological examination are carried out in case of active growth of adenoma and if a malignant process is suspected.
Forecast
The prognosis for an adrenal tumor largely depends on its type and the patient’s health status. If the formation is benign, the likelihood of a complete cure for the patient will be much higher than with cancer.
In the absence of cancer cells, removal of a high-grade adrenal tumor results in a complete cure for the patient. But even in this case, complications are possible: disturbances in the functioning of the heart, slowing of growth in children.
If the formation is malignant, then the treatment prognosis is much worse. Even in the absence of metastases, survival is about 2%. And if metastases have managed to affect neighboring organs, then the prognosis is disappointing.
Prevention
Since the causes of the development of adrenal tumors have not been fully established, prevention comes down to preventing recurrences of removed tumors and possible complications. After adrenalectomy, control examinations of patients by an endocrinologist are necessary once every 6 months. With subsequent adjustment of therapy depending on well-being and research results. For patients after adrenalectomy for adrenal tumors, physical and mental stress, the use of sleeping pills and alcohol are contraindicated.