The most common congenital anomalies of the kidneys in children include dystopia, bilateral aplasia and duplication, a defect in relationships and forms, and a violation of the development of parenchyma.
Less commonly diagnosed are multicystic cysts, dysplasia, hypoplasia, solitary and parapelvic cysts, calyx-medullary anomalies and pelvic diverticulum. Sometimes the defects can be combined.
The first signs of bud formation appear in the fetus by the end of the 4th week of development. By the end of the second month, a secondary kidney is formed, that is, something that, gradually developing along with the fetus, turns into kidneys that function in a person throughout his life.
These kidney embryos form in the small pelvis, gradually rising upward and reaching their usual position at the level of the XII thoracic vertebra.
Congenital malformations of the kidneys are quite rare, but this problem still exists, and therefore requires the most careful study.
Below are the most common kidney anomalies in children.
general information
It is possible to suspect the presence of pathological changes in the fetus during the formation of paired organs even at the intrauterine stage of development. When performing a routine ultrasound at 13–15 weeks, the presence of anomalies is noticeable. During this period, a woman can still terminate her pregnancy.
Some defects are combined with each other, which negatively affects the condition of the fetus and its development. In this case, the child is considered non-viable.
If anomalies for one reason or another were identified after birth, then they are considered dangerous if they are bilateral in nature or combined with other defects.
If we evaluate the pathogenesis, then such conditions are diagnosed in newborns in 30–40% of cases. We are talking about the proportion of kidney anomalies, among other congenital malformations.
In pediatrics, such changes in the structure of organs are considered one of the most common. Therefore, their relevance is undeniable.
But if we talk about anomalies of the urinary system as a whole, they rarely lead to death, only if the blood filtration process has been disrupted. In this case, disturbances affect the functioning of the entire body.
Danger of dysplasia
A deadly pathology that rarely goes without transplantation is underdevelopment of the kidneys as a result of dysplastic tissue damage. With dysplasia, the size of the organ is smaller than usual. Improper growth and pathological intrauterine formation of the kidneys negatively affects the structure of the parenchyma and the functionality of the organ in the future.
Dysplasia can be dwarf and vestigial. In the first case, the small size of the organ and the absence of a ureter are implied. Rudimentary dysplasia involves stopping the development of the kidneys in the first trimester of pregnancy. Instead of a kidney, the fetus has a small amount of connective tissue in the form of a cap on the ureter. A newborn child with such a pathology is doomed.
The prognosis for abnormalities of kidney development is favorable if the functions of the urinary system remain normal. The exceptions are gross defects and bilateral anomalies, which require urgent organ transplantation or permanent hemodialysis procedures. Prevention of deviations in the development of the excretory system is carried out during pregnancy.
Causes
There are several factors that can influence the process of kidney formation, these include:
- Infectious or inflammatory diseases that the mother suffered in the 1st trimester of pregnancy.
- Systemic diseases (with damage to the urinary system or urinary system) diagnosed in a woman during pregnancy.
- Taking antibacterial drugs or ATP inhibitors.
- Poor lifestyle, bad habits: smoking, drinking alcohol or drugs during pregnancy.
All this can affect the process of embryonic formation of the fetus. But if the defects are combined with each other, then genetic changes are considered the cause of their occurrence.
Various factors can lead to the appearance of genetic changes, from incest to Rh-conflict pregnancy.
It is worth paying attention to the hereditary factor, but such a relationship in this case is considered not decisive, but predisposing. That is, if there are people in the family with malformations of the urinary system, then there is a risk of similar anomalies in the fetus.
But only a consultation with a geneticist, a thorough analysis of family diseases and the collection of the necessary information can determine exactly why the defects arose.
STRUCTURE OF CAKUT SYNDROME IN 100 CHILDREN
Rice. 1. Structure of CAKUT syndrome.
Figure 1. Spectrum of CAKUT-syndrome.
Glomerular filtration rate (GFR) in patients was determined by creatinine clearance using the Schwartz calculation formula. The degrees (1-5) of vesicoureteral reflux were identified according to the Heikel-Parrkulainen (1959) classification, types of reflux nephropathy according to the results of static nephroscintigraphy according to I. Goldraich (1983), 4 stages of hydronephrosis.
CKD was classified into stages C1-5 according to the K/DOQI classification (2002) and RJ Hogg, S. Furth, KV Lemley et al. end National Kidney Foundation's Kidney Disease (2003). It is recommended in pediatric nephrological practice to stratify the 5 stages of CKD without descriptive characteristics and division into stages 3 ZA and 3B (Table 2).
Study data are presented as arithmetic mean ± standard deviation (M±SD). To compare quantitative data, the Mann-Whitney U test or Student's t test was used. Fisher's exact test was used to compare qualitative data. The strength of the relationship between quantitative characteristics was assessed using Spearman's rank correlation coefficient (Rs) or Pearson's correlation coefficient (r). The null statistical hypothesis about the absence of differences and connections was rejected at p<0.05.
Classification and types
There are various kidney defects, there are several types. Such a classification is necessary for making a diagnosis and conducting quality therapy.
Splice
A defect in which both organs are connected into one, but at the same time have their own vessels and waste in the ureters. More often, this pathology is diagnosed in boys; of the total number of children born with kidney anomalies, it is 14%.
Fusion is accompanied by a number of characteristic signs and often has other (concomitant) changes in the work or condition of the paired organs.
Characteristic features include:
- pain in the lumbar spine;
- disturbance of urine outflow;
- specific signs of pyelonephritis or hydronephrosis.
The occurrence of symptoms is due to the presence of another disease; nephropathy during fusion develops with:
- pyelonephritis;
- hydronephrosis;
- renal failure;
- ICD (urolithiasis).
Treatment of the disease is carried out exclusively by surgery. Drug therapy for this malformation performs an auxiliary function and is aimed at eliminating unpleasant symptoms.
Small cystic or polycystic infantile type
Severe pathology, which is combined with damage to the liver and bile ducts. Children born with such a developmental defect are not viable.
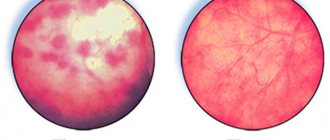
If you perform an autopsy or do an ultrasound, the kidneys will resemble a sponge with small pores. Their surface, structural and glomerular tissues, are replaced by cystic formations.
The organs cannot perform the filtration function. In combination with liver damage and provided that the pathological changes affected both organs at once, the child or fetus is recognized by doctors as incapable of life.
Macrocystic adult education
With such pathological changes, large cysts are found on the surface of organs.
They are connected by healthy tissue, the kidneys can function and do their job not fully.
Often the defect P is combined with polycystic liver or pancreas. Inherited by a dominant trait.
Cysts are large in size, but filled with transparent contents, and fluid accumulates in their cavities. In the absence of adequate therapy, formations can fester, open, and degenerate into an abscess.
Dysplasia
If it is not combined with other pathological changes in tissues, then it is not considered a serious defect, but in combination with hyperplasia and bilateral damage, it significantly reduces the viability of the child.
Pathological changes directly affect the kidney tissue; microscopic examination can reveal particles of cartilage tissue, glomerular, embryonic, and nephroblastoma.
Stenosis (narrowing) of the ureter is often observed, which complicates the outflow of urine.
Hypoplasia
This is a congenital reduction in the mass and size of organs, that is, they are poorly developed and do not correspond to the size of the fetus or infant.
Hypoplasia can be unilateral or bilateral; with a unilateral type, children experience vicarious hypertrophy of a normal (healthy) kidney.
Quantity anomalies
Agenesis is the complete absence of 1 or 2 kidneys at once. At the same time, changes also affect the child’s face: his nose is wide, the suprafrontal lobes protrude forward, and the ears are low. Babies born with this anomaly are not viable.
Aplasia is unilateral - a baby is born with 1 paired organ, while he also lacks 1 ureter, and often the vas deferens on the same side. This pathology does not have a serious impact on the viability of the child.
Accessory kidney - the presence of 3 organs that have their own blood supply, a ureter connected to the bladder. The third kidney is located much lower, it is fully functional, carries out its work, but is often smaller in size.
With such a defect, the ureter can be connected to the vagina or rectum, so when urinating, “cutting” of urine is clearly visible. There are no other complaints, the anomaly is diagnosed accidentally.
Duplication of the kidney - one of the organs is significantly increased in size, while both the upper and lower lobes are clearly visible, the division takes place along the scar.
Other defects and anomalies
These include changes in the location of organs, that is, dystopia, it happens:
- Iliac - with the location of the organ in the supply fossa, provided that the vessels depart from the common artery.
- Pelvic – the organ is located in the pelvis, between the bladder and rectum. This arrangement disrupts the functioning of both the bladder and rectum.
- Thoracic is a rare malformation in which the kidney is located in the chest, predominantly on the left side.
- Crossed - when 2 organs are located on the same side and are fully functional.
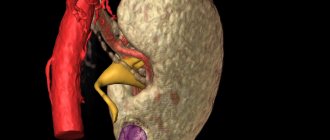
Ultrasound description of a horseshoe kidney
Boy, 9 years old. Weight 26 kg, height 132 cm.
The right kidney is 87×33 mm, parenchymal thickness is 12 mm, cortico-medullary differentiation is preserved. ChLS are not expanded. There are no stones. The blood flow is traced to the capsule.
The left kidney is 82x30 mm, parenchymal thickness is 12 mm, cortico-medullary differentiation is preserved. ChLS are not expanded. There are no stones. The blood flow is traced to the capsule.
The kidneys are located in a typical location. The right kidney is displaced anteriorly. Physiological mobility is preserved. The lower contours are not traced, the dimensions are determined conditionally. When scanning in the periumbilical region above the spine, a structure up to 13 mm thick and up to 56 mm long is detected, connecting the lower poles of the kidneys, regarded as the isthmus of a horseshoe kidney.
Conclusion: Echo signs of an anomaly in the relative position of the kidneys - a horseshoe kidney.
Symptoms of manifestation
There are several specific signs that help identify the presence of malformations or suspect certain changes in the structure of the kidneys.
Specific symptoms include:
- disturbance of urine outflow;
- the appearance of the first signs of pyelonephritis;
- changes in the composition of blood and urine;
- increase in blood pressure level.
Much depends on what kind of benefit is observed in the baby; if we are talking about a changed position of the kidney, then symptoms may be completely absent.
Some of the anomalies develop so slowly that the first signs of changes begin to bother a person already at a fairly mature age.
Stages of development
At the initial stage, pathological symptoms are completely absent. Nothing bothers the child; parents cannot independently determine the presence of a developmental defect, so they are not aware of its existence.
Later, if the condition progresses, the flow of urine is impaired. Fluid stagnation leads to the appearance of signs of pyelonephritis: body temperature rises, pain in the lumbar region worries, and the volume of urine excreted changes.
With more severe anomalies, the following are observed: hematuria, proteinuria, fluid retention, increased blood pressure, tissue swelling. The baby eats poorly and develops delayed.
If the defects are genetic in nature and combined with other changes in the body, then there is a high risk of damage to the lungs and brain. The baby's vitality is declining and he needs a transplant.
Vascular disorders
In ICD-10, the code for an abnormality of kidney development, the cause of which is poor blood supply to the organ, is code Q63.8 “Other specified congenital abnormalities.” It is because of problems with blood vessels that the full outflow of urine from the organ is disrupted, as a result of which pyelonephritis often occurs, blood pressure rises, and kidney failure develops.
When diagnosing a congenital anomaly of the renal vessels, first of all it is necessary to differentiate it from tuberculosis, hematological and hepatological diseases. Vascular disorders are usually an accompanying phenomenon for the defect of the kidney itself. Conventionally, renal vascular pathologies are divided into anomalies of veins and arteries. A defect in the formation of the main vessels of the excretory system can be:
- formation of multiple vessels;
- the appearance of an accessory artery, which is already the main one and is attached to the organ at the top or bottom;
- the presence of an additional blood vessel of a similar size;
- fibromuscular stenosis (narrowing of the lumen of blood vessels due to intensive proliferation of cystic and muscle tissue);
- artery having a knee-shaped shape;
- aneurysms.
Venous defects are multiple and accessory veins, as well as a variant arrangement of vessels emerging from the front and back of the organ in a ring-shaped form. An anomaly is considered to be the extracaval entry, the retroaortic placement of the left renal vein, and the connection of the right testicular vein to the renal vessel. To detect such deviations, Doppler ultrasound is prescribed. Based on the results of the study, the doctor will be able to give an objective assessment of the condition of the renal vessels.
Therapy methods
There are several options for influencing congenital anomalies; in some cases, it is advisable to use drug therapy, while in others only surgery can correct the situation.
Drug therapy
Fusion of the kidneys - if it occurs without pronounced signs, then it does not require specific therapy. The patient remains under the supervision of a urologist; if stones or pyelonephritis are detected, adequate therapy is provided.
Adult-type polycystic disease - drug therapy is not effective for obvious reasons (cysts cannot be resolved)
Hypoplasia - drug therapy is aimed at improving the function of a healthy kidney; it is developed on an individual basis, due to the complexity of the defect.
Treatment with medications is only permissible if one organ is of normal size and is functioning at full capacity.
One-sided aplasia - implies adherence to diet and drinking regime. No specific medications are required.
Surgical intervention
During fusion, if one of the organs partially or completely stops functioning, it is removed.
In case of adult-type polycystic disease, a puncture is performed to open the cyst cavity and remove the contents. If cancer is suspected, secretions can be sent for histological examination:
- Dysplasia - drug treatment is not carried out due to ineffectiveness, urgent transplantation is required, hemodialysis is performed during the waiting period.
- Hypoplasia – when the first signs of pyelonephritis or a strong increase in blood pressure appear, nephrectomy is permissible.
- Accessory kidney - if necessary, the organ is removed, the decision is made on an individual basis, since nephrectomy is a complex operation, additional risks and the likelihood of complications are weighed.
- Pelvic dystopia - removal of the organ is required, since it disrupts the functioning of the intestines and bladder, and also leads to the appearance of unpleasant symptoms.
ethnoscience
If the fetus or infant has defects, such therapy is not carried out due to zero effectiveness.
Asymmetric renal fusions on ultrasound
The kidneys are connected at opposite ends, the two renal pelvises are on the same side of the spine, but the openings of the ureters in the bladder are located in their usual places.
In the case of an S- and I-shaped bud, the longitudinal axes of the fused buds are parallel, and the axes of the buds forming an L-shaped bud are perpendicular. The pelvis of the S-shaped kidney faces in opposite directions, while the I- and L-shaped kidneys are located medially.
Take care of yourself, Your Diagnosticer !
Tags: video pearl lectures kidneys ultrasound
Complications and consequences
Anomalies rarely lead to severe complications unless they are combined with other defects. Various changes can lead to:
- to a child’s developmental delay;
- to kidney failure;
- to the development of chronic pyelonephritis;
- to disruption of urine outflow;
- to frequent bacterial or inflammatory diseases.
However, consequences arise only if parents refuse therapy or surgery. If medical or surgical treatment is carried out in a timely manner, the risk of developing severe complications is extremely low.
DISCUSSION
The terminology used in the pediatric nephrology literature is CAKUT isolated and syndromic. In our study of 100 children with combined congenital anomalies of the kidneys and urinary tract, isolated CAKUT was diagnosed in 94% and syndromic in 6%. According to the literature, different frequencies of detection of isolated (60-80%) and syndromic variants (20%) are given. The severity of combined congenital anomalies of the kidneys and urinary tract in children with oculocerebro-renal Lowe syndrome was noted.
We have shown that among isolated CAKUT, vesicoureteral reflux (51%) and ureterohydronephrosis (33%) predominate. The results we obtained coincide with the data published by the authors. H. Cordell et al. (2016) in a large-scale study of isolated CAKUT syndrome indicate a high incidence of VUR (62%). In case of syndromic CAKUT in 6 patients, among combined congenital anomalies, in half of the cases we diagnosed PMR and ureterohydronephrosis, respectively.
Among the anomalies of kidney development in CAKUT in 100 children, kidney hypoplasia (39%), anomalies in the number of kidneys (22%), and anomalies in the location of the kidneys (20%) were most often diagnosed. M.S. Ignatova et al. indicate that there is no uniform data on the etiology and structure of CAKUT in the domestic literature.
Literature data indicate that syndromic CAKUT has a more severe course than isolated CAKUT. We identified the features of the course of syndromic CAKUT with an outcome in CKD C3-C5 in all 6 children aged 2 to 12 years.
According to A. Vivante et al. (2014), CAKUT with a family history of diseases of the genitourinary system is more severe than in children without a family history. The same data were obtained by P. Danziger et al. (2016) based on the results of a large-scale study. According to the results of our study, a family history of kidney disease was detected in 16%; all cases were identified only with isolated CAKUT.
Statistically reliable data on the relationship between the presence of a family history and the severity of CAKUT have not been obtained.
Signs of CKD are established in 100% of patients with CAKUT. As is known, in practical clinical guidelines for CKD: assessment, classification, stratification K/DOQI (2002), RJ Hogg et al. (2003), A.V. Smirnov et al. a classification is presented highlighting 5 stages of CKD, which is based on the assessment of GFR; in nephrological practice it is intended for adults and children over 2 years of age, taking into account the age-related characteristics of GFR. In our study, when stratifying the severity of CKD C1-C5 in 85 children (aged 2 to 17 years), a predominance of C1 was found to be 74%.
Preventive measures
As part of preventive procedures it is worth:
- eat right during pregnancy;
- regularly visit a gynecologist and do an ultrasound;
- do not take antibacterial drugs as prophylaxis and without a doctor’s prescription;
- avoid infectious and inflammatory diseases;
- lead a healthy lifestyle, give up bad habits.
Unfortunately, modern medicine cannot influence the genetic level of fetal development; for this reason, when identifying anomalies, it is worth consulting with a geneticist. Donate blood for a screening test and do an ultrasound again.
Kidney malformations are very common in pediatrics, but one should not assume that a child with a similar diagnosis is 100% disabled.
Modern medicine makes it possible to rid a child of pathology using various methods. This will allow him to lead a normal life in the future, develop and be no different (in terms of physical development) from his peers.
Location anomalies
As the fetus develops, the developing buds move from the pelvis to the lumbar region, gradually reaching the desired level. If at the stage of development their movement was disrupted, this is dystopia. It happens:
- sacrolumbar;
- pelvic-sacral;
- chest;
- ileal
Dystopia can be either unilateral or bilateral, when movement disorders affect only one side of the body or both at once.
The choice of treatment is individual. Its tactics are determined by when the organ stopped moving.
Treatment varies depending on the clinical manifestations and complications present. To make a diagnosis, they turn to ultrasound examination and radiography. Symptomatic treatment is carried out, in some cases there is an urgent need for surgical interventions.
Prevention of diseases of the urinary system
Congenital malformations of the urinary system occur in 6% of pathological studies of children under 1 year of age. Medical genetic counseling, prenatal diagnostics, preventive methods aimed at improving the health of the expectant mother herself make it possible in 50-70% of cases to prevent the birth of children with severe congenital and hereditary diseases, and in some forms - to carry out successful preventive treatment, and then in your home The long-awaited healthy baby will appear!
Remember that your baby's health is in your hands! Attentive parents themselves may suspect something is wrong. Here are a few symptoms to look out for to help identify kidney or urinary tract disease early and prevent serious complications from developing:
- Monitor the number of times you urinate and the volume of urine produced. During the first 1-3 days of life, a newborn baby urinates 3-5 times a day - this is a physiological transition state of the urinary system. From 4 days to 6 months, the frequency of urination reaches 20-25 times a day, after 6 months and up to 1 year - 10-14 times. By the age of 5, the number of urinations is reduced by 2 times. Frequent urination and the urge to urinate (without urination itself) is a reason to urgently consult a doctor. If the child urinates little and rarely or does not urinate at all (the volume of urine in the first 3 days of life is about 50-100 ml, up to 6 months - on average 180-190 ml, 6 months - up to 2 years - 230-300 ml, 3-4 years - about 400-500, from 5 to 7 - 500-700 ml, over 7 - 800-1000 ml), he has nocturia (the predominance of the amount of urine excreted at night over the daytime volume; normally the daytime is 2/ 3 total amount of urine per day), polyuria (increase in the volume of daily urine by more than 2 times), daytime or nighttime urinary incontinence (this applies to children over 3-4 years old) - contact a specialist!
- Pay attention to the color of the urine and its clarity. While the child is small, this is not difficult. Normally, the color of urine is light yellow; in the morning the urine is the richest. Cloudy urine, blood in the urine, etc. may be symptoms of serious illnesses.
- Examination of the external genitalia is of no small importance. In newborn boys, you need to pay attention to the location of the urethra. If the baby suddenly develops redness and swelling of the scrotum on one or both sides, during swaddling or when touching the scrotum, the child cries and becomes restless, do not hesitate and do not self-medicate, but urgently contact a pediatrician or pediatric urologist. In girls, you need to pay attention to the outer labia. There should be no swelling, redness, etc., there should be no discharge (physiological discharge from the genital tract is light, mucous is observed in girls during the newborn period, in infancy, they are caused by the presence of placental and maternal hormones in the girl’s body, in the future discharge will appear only at puberty). With adult children the situation is more complicated, but a child who grows up in an atmosphere of trust and care will definitely complain if something is wrong.
- Pay attention to unexpected weight gain in your baby or to pronounced and long-lasting “traces” from the elastic of panties or socks - this could be swelling.
- Pay attention to your child's complaints. Pain in the lower back, side, above the pubis, during urination, and in young children also abdominal pain, especially intense and recurring, should cause serious concern among parents.
- If a child becomes lethargic, pale, refuses to eat, his temperature rises to high levels (38-40°C), and at the same time, there are no visible manifestations of a cold, and antipyretic drugs give only a short-term effect - take a general urine test of your child. baby.
Svetlana Kirilina, PhD, pediatric nephrologist