According to statistics, one person in a thousand suffers from pyelonephritis in the world. What is pyelonephritis and how long does it take to treat? This is a kidney disease that is of bacterial origin. Inflammatory processes gradually affect all parts of the kidneys - renal tubules, calyces, pelvis. The main cause of inflammation is infection. Most often, there is an ascending route of infection; much less often, infection occurs through the blood or lymph. Pathogenic bacteria such as Escherichia coli and streptococcus are the most common causative agents of infection.
Due to the anatomical structure of the body, women get sick more often than men. The most common causes of pyelonephritis are:
- Hypothermia;
- Past infectious and viral diseases;
- Escherichia coli, helminthic parasites;
- Exercise stress.
How long does it take to treat pyelonephritis?
The most common question patients ask: “How long does it take to treat pyelonephritis?” It all depends on how timely the patient presented, what type of pyelonephritis was diagnosed and how accurately the patient follows all the instructions and procedures.
Often, this disease is asymptomatic or with mild symptoms, so many patients do not pay special attention to the first signs and the disease progresses, which leads to more serious problems with the functioning of the organ. As a result, people turn to a doctor when their health condition no longer allows them to lead their usual rhythm of life and serious complications arise.
There are two main types of pyelonephritis - acute and chronic. Depending on what type the patient has, the duration of therapy in the hospital takes so long.
If the patient came for the first time with this diagnosis and the disease is in an acute form, then treatment of this type is more successful and the treatment time is much shorter.
Symptoms of acute pyelonephritis:
- High temperature, but without chills and aching joints;
- The pain in the lower back is not severe, it can radiate to the right hypochondrium;
- Nausea, vomiting;
- Frequent or, conversely, rare urination;
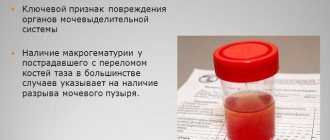
- Change in the color and odor of urine.
The treatment of acute pyelonephritis includes several mandatory points:
- Strict bed rest;
- Strict adherence to the diet (restriction of salt and protein);
- Antibiotics selected by the attending physician for 10 days;
- Compliance with the water regime, the volume of liquid is at least 2 liters in fractional portions.
For the chronic type of this disease, treatment will take a longer time, at least one year. If the diet is violated or the doctor’s instructions are not followed, treatment can drag on for years. Typically, chronic pyelonephritis occurs as a result of untreated acute pyelonephritis, non-compliance with diet, refusal to take medications and herbal remedies, and hypothermia.
Symptoms of the chronic type are not so obvious; all patients may have different symptoms. A urine test does not always show changes or abnormalities in the organs of the urinary system. The diagnosis can only be confirmed using ultrasound.
Symptoms of chronic disease:
- High blood pressure
- Fatigue and decreased performance
- Possibly shortness of breath
- Stool disorders
- Dull, mild pain in the lumbar region
Basic methods of complex treatment of chronic form:
- Antibacterial therapy from 1 to 5 weeks. However, the course of therapy will need to be carried out systematically as prescribed by the doctor monitoring you;
- Treatment with mineral water for 4 to 6 weeks. The course will need to be repeated after the break. During the year you need to conduct 2-3 courses;
- Physiotherapy in consultation with a doctor;
- Phytotherapy;
- A course of vitamins.
All chronic treatment tactics are designed for duration and repetition of the course of treatment. Your kidneys will hurt constantly if you do not repeat several courses of therapy within a year, depending on the condition, in a clinic or hospital. Monitoring of treatment only by ultrasound every six months.
There are many cases when patients take pills in large quantities and complain that recovery does not occur, but you need to be treated not only with medications. Treatment of chronic pyelonephritis should be comprehensive. There are examples when a patient cured it with Nephrodilin in 3 weeks. Or using herbal decoctions in addition to the main treatment, patients got rid of the diagnosis in 3 years. Depending on the stage of the disease, the effectiveness of treatment, and individual characteristics, the recovery time of patients may vary.
With advanced pyelonephritis, complications will certainly begin.
Possible complications and pathologies:
- The inflammatory process will lead to the formation of ulcers;
- Formation of a carbuncle. In this case, only surgical intervention will help;
- Kidney abscess;
- Acute renal failure;
- Sepsis.
Etiology and pathogenesis
With the development of acute inflammation, some people prefer to self-medicate, which is fraught with the development of purulent pyelonephritis. There are a number of provoking factors that contribute to the development of the disease:
- Escherichia coli is one of the most common pathogens;
- reduced body resistance, in which pathogenic mycobacteria rapidly develop (anemia, diabetes, autoimmune diseases);
- inflammation of the reproductive and urinary system;
- urolithiasis disease;
- abnormal arrangement of organs and vessels of the urinary system;
- oncological formations;
- the presence of blood clots in the renal vessels.
Possible renal pathologies
The disease may appear as a carbuncle on the organ.
Acute purulent disease manifests itself in the following form:
- Apostematous pyelonephritis. Changes occur in the calyx and pelvis, small pustules begin to form.
- Abscess of a paired organ. The kidney is enlarged in size, and small ulcers merge with each other.
- Kidney carbuncle. It is a large abscess.
How long are they in the hospital?
If you are interested specifically in how many days pyelonephritis is treated, then, for example, treatment of the acute form in adults takes place within 30 days. The course of therapy in a hospital under the supervision of a physician should be at least 7-14 days. After discharge, the patient receives consolidation therapy for half a month in the clinic at his place of residence. The most difficult thing for many patients after discharge from the hospital is to continue treatment at home. You must strictly follow the diet prescribed by your doctor.
Acute pyelonephritis is treated in most cases with a favorable outcome. Also, during the year you need to be observed by a nephrologist or urologist at the clinic at your place of residence and comply with all prescribed standards of treatment. In the chronic form of pyelonephritis, treatment in a hospital occurs only during exacerbation. The duration of hospitalization in this case depends on the level of exacerbation.
What to do to avoid getting sick?
Simple tips will help prevent the development of pathology or not get sick again.
Due to the fact that acute purulent kidney disease leads to consequences such as complete destruction of the organ, renal-liver failure, bleeding, infection of vital organs, anemia and other troubles, it is necessary to take preventive measures .
Simple tips will help prevent the development of pathology or not get sick again:
- thorough sanitation of any foci of inflammation;
- timely visit to the doctor;
- control of blood sugar and cholesterol levels;
- control of the general condition of the body;
- diet, not only food, but also drink.
Of course, you will have to change your lifestyle, for example, start moving more, stop abusing sweets and smoked foods. However, if the diagnosis of pyelonephritis has already been made, you can no longer neglect your own health, otherwise all this could end much worse than an attack of purulent acute pyelonephritis.
Sick leave
The risk group most often affected by pyelonephritis is the adult population, specialties whose work involves hypothermia, low temperatures, and outdoor work. Sick leave for pyelonephritis must be issued for the duration of treatment in the hospital. After discharge from the hospital, you are required to undergo an examination by a nephrologist or urologist at the clinic at your place of residence. He can also issue you a sick leave certificate for the duration of treatment, but the period of treatment at home is no more than 5-7 days. The kidneys recover from acute pyelonephritis after one month of effective treatment.
If the attending physician detects complications or worsening of the condition, he will recommend that you continue treatment in a hospital. With the chronic type of pyelonephritis, sick leave for incapacity for work is not given only if clinical tests and ultrasound show an exacerbation of the disease and incapacity for work is lost. And in this case, hospitalization will be recommended.
Definition of disease. Causes of the disease
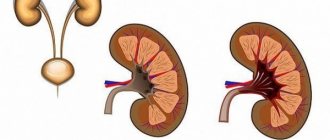
Acute pyelonephritis is an inflammatory disease of the kidneys of a bacterial cause with predominant damage to the pelvis, calyces and interstitial tissue of the renal parenchyma. The International Classification of Diseases abandoned the term “acute pyelonephritis”, replacing it with “acute interstitial nephritis”. [3]
Pyelonephritis should be distinguished from glomerulonephritis. Both forms of nephritis are characterized by inflammation of the kidney parenchyma, but with pyelonephritis, the interstitial tissue is affected, and with glomerulonephritis, the glomeruli of the kidneys. Therefore, pyelonephritis is called “interstitial nephritis”, from the word “interstitium” - interstitial tissue, and glomerulonephritis can be called “glomerular nephritis”, from the word “glomerulus” - renal glomerulus. [2]
The cause of pyelonephritis is a bacterial infection. Among the causative agents of the disease, the leading one is Escherichia coli. Less common are other microbes such as Proteus, Enterococcus, Pseudomonas aeruginosa and Staphylococcus. [4]
ESBL+ bacteria pose a particular danger. The abbreviation "ESBL" stands for "extended spectrum beta-lactamases." ESBLs are a group of bacterial enzymes that allow bacteria to ignore antibiotics. Thanks to ESBLs, bacteria break down and neutralize several groups of antibacterial drugs, including penicillins and cephalosporins. Not all microbes can produce such enzymes; quite often this ability was observed in Escherichia coli and Klebsiella pneumoniae. Modern microbiological laboratories always mark such microbes with either the Russian abbreviation ESBL+ or the English analogue ESBL+. According to European data, ESBLs produced by Escherichia coli occur in 10% of cases, and Klebsiella pneumoniae produces ESBLs in 20% of cases. Thus, the problem of ESBL+ bacteria has important clinical significance. [8]
Acute pyelonephritis can occur at any age and in any gender. Most often, the disease occurs in women of active reproductive age, which is explained by the structural features of the female genitourinary system. However, pyelonephritis is often detected in children and mature men, so the age and gender of the patient cannot be used as a differential sign of this disease.
Is it possible to die
The disease pyelonephritis itself is not fatal, but if not treated on time, you can die from any disease. I want to live as long as possible, follow the diet, doctor’s prescriptions and supportive therapy, undergo scheduled examinations and tests on time.
In case of non-compliance with treatment standards, possible complications and pathologies are inevitable, which result in renal failure and can lead to death.
“How to live now with such a diagnosis?” you ask. Yes, in this case you need to be patient and persistent if you want a complete cure or long-term remission.
“People, how do you live?” is a desperate question from many sick people. Yes, of course, a complete cure may take more than one year. We must not forget about the required volume of water that you need. Nowadays there are a lot of fashionable thermoses and accessories for water, you can combine the useful and the pleasant. Avoid hypothermia, strengthen your immune system to reduce the risk of contracting viral diseases. Get scheduled check-ups with your doctor on time. Select herbal medicines in consultation with your doctor, taking into account their action and effect on your body. Drink herbal teas that help your kidneys.
Life does not end with a diagnosis of chronic pyelonephritis, it is curable. Live as you lived before, but taking precautions. Remember the catchphrase: “Water does not flow under a lying stone!” The duration of your life is in your hands.
In case of mild exacerbation and no signs of urinary tract obstruction, treatment is carried out in a “hospital at home”. In this case, doctors go to the patient’s home. Another option is day hospital therapy. In case of acute and obstructive pyelonephritis and exacerbation of its chronic form, treatment is carried out only in a hospital setting.
Forecasts and preventive recommendations
With immediate qualified treatment, the prognosis will be favorable. There are also a few simple rules that will help you avoid serious complications. If there are congenital pathologies, they require monitoring and timely correction. And also do not forget about a healthy lifestyle; during the off-season, the body needs an abundant supply of vitamins. People prone to frequent relapses of urinary system diseases require regular monitoring by a specialist, at least twice a year.
Indications for hospital treatment
Only in a hospital it is possible to track the dynamics of processes occurring during treatment. Indications for mandatory hospitalization of the patient:
- exacerbation of chronic pyelonephritis with dysuria, pollakiuria, fever;
- obstruction of the urinary tract;
- acute primary and secondary pyelonephritis;
- serous form of kidney inflammation;
- acute pyelonephritis of a single or only functioning kidney;
- suspicion of purulent complications;
- exacerbation of the disease with signs of renal failure;
- acute inflammation of the kidneys due to diabetes mellitus or immunodeficiency.
Forecast. Prevention
The prognosis for pyelonephritis is favorable. Most acute pyelonephritis is successfully treated on an outpatient basis, and only a small proportion of cases require hospitalization. Nevertheless, a certain percentage of deaths remains. The reasons for the unfavorable course of the disease are age over 65 years, the addition of acute renal failure, untimely detection of purulent complications requiring surgical intervention, and severe concomitant diseases such as decompensated diabetes mellitus. [5]
Drawing up an individual prevention plan begins with studying the history of a specific disease. In particular, it is necessary to answer the question of how the bacteria entered the kidney: through blood or urine? With the hematogenous route of infection, it is necessary to sanitize the foci of chronic infection existing in the body, eliminate hypothermia and carry out the prevention of seasonal colds. In the case of urinogenic infection, it is necessary to prevent inflammatory diseases of the bladder.
In the case of a secondary form of acute pyelonephritis, it is advisable to restore the normal outflow of urine from the affected kidney.
Regardless of the route of microbes entering the kidney, all patients are recommended to consume a sufficient amount of fluid and a variety of urological herbal preparations. [4]
Treatment regimen for pyelonephritis in a hospital setting
There is a difference between outpatient and inpatient treatment. In the latter case, the patient is provided with rest, his nutrition is monitored, and his blood pressure is periodically measured. Antibiotics in a hospital can be administered using droppers, which cannot be done independently at home. In addition, doctors, if necessary, take tests from the patient to monitor the progress of treatment. The general treatment regimen includes:
- taking antibiotics for 4-6 weeks;
- strict bed rest;
- diet;
- drinking at least 2 liters of liquid in small portions.
After discharge, the patient continues to take antibiotics, but in tablets, and receives maintenance therapy in the clinic at his place of residence.
Patient mode
When a person first encounters acute pyelonephritis or its exacerbation, bed rest must be observed for 3-5 days. The motor mode is built taking into account the following principles:
- Activity increases if low back pain has decreased, dysuria has improved, and the temperature has decreased.
- Throughout the entire period of exacerbation, the patient needs to spend at least 3-4 hours in bed during the day and 10 hours at night.
- After the end of the relapse, a day's rest of 1.5-2 hours is recommended.
Drug therapy
For acute pyelonephritis, etiotropic and symptomatic therapy is carried out. The first is taking antibiotics to suppress the growth of bacteria, which cause kidney inflammation. Symptomatic treatment helps eliminate the signs of pyelonephritis. The main groups of medications prescribed by a doctor:
Average duration of use
Broad-spectrum antibiotics
Therapeutic diet
The diet for acute pyelonephritis should include a sufficient amount of proteins, fats and carbohydrates. The menu is built primarily from easily digestible products. Basic principles of the diet:
- Limit spicy, sour foods, alcohol, preservatives, fried foods, rich broths.
- For seasonings, use only red bell pepper or tomato puree.
- For arterial hypertension, reduce the daily amount of salt to 3-4 g.
- In addition to water, use a decoction of horsetail, cranberry juice, infusion of black currant leaves, birch, rose hips or strawberries.
- Consume fermented milk products: kefir, cottage cheese, sour cream.
- Include fruits and vegetables, cereals, and boiled meat in the menu.
- Stick to a daily caloric intake of 2500 kcal.
Physiotherapy
The indication for physiotherapy is to relieve the inflammatory process. They are not performed in case of active pyelonephritis, at the terminal stage of inflammation, or polycystic kidney disease. Basic methods of physiotherapy:
- ultrasound therapy;
- diathermy of the renal area;
- paraffin, mud and ozokerite applications to the kidney area;
- sodium chloride and carbon dioxide therapeutic baths;
- ultra-high frequency therapy;
- magnetic therapy;
- ultrasound procedures;
- laser therapy for each kidney;
- electrophoresis of antimicrobial drugs.
Additional treatments
For some individual manifestations of acute pyelonephritis, doctors resort to additional treatment methods. Their list includes the following procedures:
- Functional passive stimulation of the kidneys. Indication: deterioration of the process of urinary excretion. In the morning on an empty stomach, the patient takes 1-2 tablets of Furosemide. The procedure is performed 1-2 times a week.
- Taking non-steroidal anti-inflammatory drugs (NSAIDs). Indications: persistent leukocyturia, bacteriuria. The patient is prescribed 25 mg of Voltaren or Indomethacin 3 times a day for 6-8 weeks.
Surgical intervention
The main indication for surgery is secondary pyelonephritis. It occurs as an acute nonspecific inflammatory process against the background of other pathologies of the urinary system. Main types of surgical intervention:
- Catheterization of the ureter. This is the installation of an external or internal stent to restore urine passage.
- Percutaneous puncture nephrostomy. It is carried out for relatively long-term drainage of the kidneys, helps to avoid open surgery and, after 3-4 weeks, remove the stone using minimally invasive methods.
For some patients with acute pyelonephritis, doctors prescribe open surgery. Main indications for endoscopic operations:
- acute purulent pyelonephritis;
- negative dynamics of adequate antibiotic therapy;
- impossibility of draining the kidney using minimally invasive methods.
If other methods have failed, treatment for acute pyelonephritis is nephrectomy. This is an operation to remove a kidney, which is performed in the following cases:
- with signs of renal vessel thrombosis;
- with purulent inflammation of a non-functioning kidney;
- with multiple confluent carbuncles of the kidney;
- with purulent destruction of more than 2/3 of the kidney;
- purulent intoxication, toxic shock, decompensation of concomitant diseases.
Diagnostics
Diagnostics begins in the doctor’s office, who collects all the information about the patient, palpates the abdominal cavity, determining the surface condition of the organ, its size, and pain. Next, the patient needs to undergo general blood and urine tests, which, in case of inflammation, will show significant deviations from the norm in the indicators of leukocytes, red blood cells, and if acute purulent pyelonephritis has formed, there are impurities of pus, blood and cloudy sediment in the urine. Bacterial culture will help identify the pathogen. This is important when choosing an antibiotic and prescribing a course of treatment.
Instrumental
Acute pyelonephritis is diagnosed using ultrasound, which is used to confirm the diagnosis and during treatment to determine the effectiveness of therapy. An ultrasound can show the condition of the tissues of the organ, its size, the presence of foci of inflammation and their location. If there is insufficient data from this type of study and the doctor cannot make an accurate diagnosis, the patient is advised to undergo a urographic examination, MRI or CT scan of the kidneys.
Urography is performed using contrast, which is concentrated in the kidneys, which makes it possible to assess the condition of the organ, their size, the presence of inflammation and erosion. With an MRI or CT scan, the doctor receives the most accurate images of the kidneys, and all changes in them, foci of inflammation and other pathologies are visible. Differential diagnosis is needed in order to exclude other diseases that have symptoms similar to those of acute pyelonephritis. This is appendicitis if the pain is localized on the right, cholecystitis, cholangitis and andexitis.