Metabolic nephropathy: what is it?
A key factor in the development of pathology is a violation of metabolic processes in the body.
There is also dysmetabolic nephropathy, which is understood as a number of metabolic disorders accompanied by crystalluria (the formation of salt crystals detected during a urine test). Depending on the cause of development, there are 2 forms of kidney disease:
- Primary - occurs against the background of progression of hereditary diseases. It promotes the formation of kidney stones and the development of chronic renal failure.
- Secondary - manifests itself with the development of diseases of other body systems, and can occur during the use of drug therapy.
Important! Most often, metabolic nephropathy is a consequence of calcium metabolism disorders, oversaturation of the body with phosphate, calcium oxalate and oxalic acid.
Clinical guidelines
If diabetic nephropathy has been diagnosed in children, clinical recommendations will vary depending on the nature of the disease. In severe cases, the patient experiences progression of acute renal failure, as well as acute or chronic inflammation of the interstitial tissue and tubules of the filtration organ of the second and third degree. However, in this combination the disease is quite rare.
The main cause of its occurrence is considered to be congenital metabolic disorders. The main recommendation in terms of the therapeutic approach is mandatory hospitalization of the patient in a specialized nephrology department for further inpatient treatment.
The principle of kidney damage in dismetabolic nephropathy. Source: detskiebolezni.com
If the patient’s condition is moderate, then medical measures can be carried out both on an outpatient basis and in a hospital setting. Otherwise, if dysmetabolic nephropathy, combined with oxaluria, uraturia or a combination thereof, occurs in a mild form, it is subject to treatment on an outpatient basis.
Regardless of the type of pathological process, the main task is to increase the water load on the body. An additional 500-1000 ml is added to the age-specific fluid intake norms. For children 1-2 years of age, it is recommended to consume 1.3-1.5 liters per day, 4-6 years old - 1.8-2.0 liters per day, over 10 years old - from 2 to 2.5 liters. However, it is worth remembering that the entire volume of liquid is taken into account, and not just water, tea, juices and other drinks.
Specialists should pay attention to the fact that patients in the first year of life almost always receive the required volume of fluid, since their development process is controlled by pediatrics. As for older children, they often eat irregularly, so on average they receive no more than 1.7 liters of fluid per day. This becomes the main cause of metabolic disorders.
The complex of basic therapy necessarily includes dietary correction. If dysmetabolic nephropathy occurs against the background of oxaluria, then it is necessary to exclude from the diet all foods that are saturated with oxalic acid, for example: cocoa, chocolate, beets, celery, spinach, sorrel, parsley, rhubarb.
Table of alkaline and acidic valences of products. Source: j96242r7.beget.tech
It is necessary to limit the consumption of foods with an average content of oxalic acid (carrots, chicory, green beans, onions, tomatoes, tea). It is allowed to eat dishes that contain ingredients with a minimum content of this substance. This includes white cabbage, apricots, bananas, and potatoes. Mushrooms, eggplants, zucchini, peas, cucumbers, and pumpkin are also allowed.
The restriction also includes foods that contain high levels of vitamin C (rose hips, sweet peppers, currants, sea buckthorn, cauliflower and Brussels sprouts, oranges, rowan). Since this element is not produced in the human body, its intake cannot be completely excluded. This should be taken into account when developing a dietary menu.
According to medical studies, it was possible to establish that after regulating the patient’s diet, the level of oxalates excreted along with urine decreases by about 40%, and sometimes more. If sodium benzoate is administered, it will block the endogenous synthesis of oxalates from glycine (the process of glycine metabolism changes). For better transformation of glycine into hippuric acid, cranberries and lingonberries should be present in the diet.
If uricosuric nephropathy is diagnosed, it is recommended to develop a dietary principle taking into account the limited intake of purine substances into the body. Therefore, it is worth minimizing dishes that contain sardines, mackerel, herring and offal. The average purine content is found in lentils, beef, rabbit, river and lake fish.
Recommended mineral waters. Source: natalikorotova.blogspot.com
It must be remembered that urate and oxalate crystals can precipitate in an acidic environment. Therefore, it is important to consider the acidic and alkaline valencies of foods. The first type predominates in products of animal origin, as well as cereals, and the second type predominates in fruits and vegetables. Accordingly, a dairy-vegetable diet is recommended.
In order to achieve maximum alkalization of the environment, it is necessary to regularly drink mineral waters such as Narzan, Essentuki and Borjomi. They have an average level of mineralization, according to age-related doses. The course lasts 2-3 weeks. It is also recommended to take 5-15 ml 1-3 times a day of vegetable oils in the form of dressings for dishes.
General understanding of nephropathy
Nephropathy in most cases develops as a consequence of other diseases. It is characterized by bilateral kidney damage, can be a congenital anomaly arising from a genetic failure, or manifest itself as a complication of a disease of another organ.
External factors can also influence the occurrence of pathology. For example, nephropathy can occur after inhaling toxic substances. The filtration function of the kidneys is impaired. There is a high risk of developing further renal failure.
Classification
Doctors distinguish several types of dysmetabolic nephropathy. The baby’s attitude towards one type or another is determined by the presence of crystals of certain types of salts in the child’s urine.
Types of dysmetabolic nephropathy found in young children:
- uraturia , this is the name of the type of disease in which a high content of urates, the so-called uric acid salts, is detected in the child’s urine;
- oxalurgy , such a disease is detected quite easily. The disease is determined by the presence of a large amount of oxalates in the child’s urine. Based on statistical data, this type of illness is the most common;
- phosphaturia , with this type of disease, the presence of phosphates is revealed in the tests of a small patient.
- cystine nephropathy , determined by an increased content of cystine in the child’s urine. Cystine is a product of methionine metabolism;
- oxalate-phosphate-urate – mixed type of disease. This type of disease is much less common than the types mentioned above.
Taking into account various factors, nephropathy also has two types:
- primary - is hereditary. Often this type of nephropathy leads to renal failure and nephrolithiasis;
- secondary - implies dysmetabolic disorders that develop against the background of damage to important systems and organs.
Development factors
The following pathologies are predisposing factors to the development of metabolic nephropathy:
- infection of the genitourinary system;
- endocrine disorders (disorders of the thyroid, pancreas);
- growth of malignant neoplasms;
- metabolic disorders caused by genetic predisposition;
- exposure to radiation on the body during treatment or when living in an environment with an increased radioactive background;
- the presence of parasites in the digestive organs (worms, lamblia);
- urinary dysfunction (stagnation or uncontrolled urine output);
- taking medications without direct indications.
Among metabolic nephropathies, there are subtypes that are characterized by the presence of salt crystals in the urine. Children more often have calcium oxalate nephropathy, where a hereditary factor influences the development of the disease in 70-75% of cases. In the presence of chronic infections in the urinary system, phosphate nephropathy is observed, and in the case of impaired uric acid metabolism, urate nephropathy is diagnosed.
Mechanism of development and manifestation of nephropathies
An adult can “write off” the signs of the disease as manifestations of pyelonephritis or cystitis. Children under 5 years of age may have no symptoms at all.
It is worth paying attention to the following changes:
- The urine changes color and sediment appears in it.
- I am worried about pain in the lumbar spine.
- A person quickly gains weight, his face changes due to severe swelling.
- Frequent urge is bothersome, but urination is useless.
- The level of blood pressure decreases, hypotension is observed.
Much depends on the cause of the condition; the patient may experience:
- signs of pyelonephritis, cystitis, if these diseases lead to the development of nephropathy;
- symptoms of diabetes mellitus and disorders of the endocrine system, if the condition is not corrected with medications;
- manifestations of disturbances in the functioning of the organs of the digestive system, provided that the diseases led to such complications;
- There may be symptoms of vegetative-vascular dystonia and frequent headaches.
If the disease is diagnosed in a child under 5 years of age, then parents pay attention to the sediment that appears in the pot.
Structural changes in organs are considered echo signs of dysmetabolic nephropathy; echo signs can be seen during an ultrasound examination.
Symptoms
As a rule, the disease has a polymorphic pattern of manifestations:
- metabolic disorder,
- inflammatory diseases of the kidneys and urinary system,
- increased urine production,
- formation of stones in the organs of the urinary system,
- pain in the abdomen and lower back,
- increased fatigue and weakness,
- swelling,
- itching and redness of the reproductive organs,
- urinary retention.
According to the results of laboratory diagnostic tests, urine tests show an excess number of leukocytes, red blood cells, casts, proteins, phosphates, urates and oxalates.
- Classification of diabetic nephropathy by disease stages
Etiology and pathogenesis of the disease
Most often, the development of the disease is provoked by the following pathological processes:
- diseases of the endocrine system,
- oncological diseases,
- infection of the urinary system,
- parasitic diseases of the gastrointestinal tract,
- the use of radiation for the treatment of tumor and non-tumor diseases,
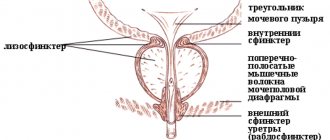
- difficulty urinating due to stagnation of urine in the bladder due to narrowing of the urethra, untimely emptying of the bladder, unintentional urination,
- uncontrolled use of drugs,
- a disorder of metabolic processes in the body, most often the metabolism of calcium, oxalic acid.
Most often, metabolic nephropathy occurs in children and can be accompanied by neurocirculatory dysfunction, allergic reactions, excess body weight and low blood pressure.
Children with this pathology are most often born if, during the period of gestation, there was insufficient oxygen supply to the fetus or late toxicosis.
What it is?
Kidney pathology, in which the structure of kidney tissue changes due to disturbances in salt metabolism, is called dismetabolic nephropathy.
Salts, which are formed in the body as a result of the metabolic system, are present in the urine and blood of any person, but if there are no serious metabolic disorders, these substances are formed in certain acceptable quantities and in dissolved form (in this state they are held by special enzymes).
If these enzymes are not produced enough, the salts begin to crystallize and turn into a sediment that is deposited in the kidney tissues. Over time, such deposits clog the renal canals, in which inflammatory processes begin .
In addition to dismetabolic nephropathy, when salts are formed in the blood, there is a type of pathology called metabolic nephropathy . In this case, sediment forms in the urinary fluid, but deposits along the urinary tract also enter the kidney tissue, disrupting their structure.
Disease code according to ICD-10 N16.3.
Symptoms and types of disease
Impaired kidney function due to metabolic failure leads to the following manifestations:
- development of inflammatory processes in the kidneys and bladder;
- polyuria - an increase in the volume of urine excretion by 300-1500 ml above normal;
- the occurrence of kidney stones (urolithiasis);
- the appearance of edema;
- disturbance of urination (delay or frequency);
- the appearance of pain in the abdomen, lower back;
- redness and swelling of the genitals, accompanied by itching;
- deviations from the norm in urine analysis parameters: detection of phosphates, urates, oxalates, leukocytes, protein and blood in it;
- decreased vitality, increased fatigue.
As the disease develops, a child may experience signs of vegetative-vascular dystonia - vagotonia (apathy, depression, sleep disturbances, poor appetite, feeling of lack of air, lump in the throat, dizziness, swelling, constipation, tendency to allergies) or sympathicotonia (hot temper, absent-mindedness, increased appetite, numbness of the limbs in the morning and heat intolerance, tendency to tachycardia and increased blood pressure).
Pathogenesis
The disease is often diagnosed in people who previously suffered from kidney diseases of an infectious or inflammatory nature and not only:
- metabolic disorders associated with incomplete absorption of salts, disruption of the urinary system organs increase the risk of developing the disease;
- Inflammatory processes in the intestines and organs of the digestive system can also lead to such complications.
More often the disease is diagnosed in adolescents, as well as in adults.
Until adolescence, it can occur without severe symptoms, but hormonal changes aggravate the situation, leading to the development of signs of pathology.
Causes of secondary nephropathy
Secondary dysmetabolic nephropathy can be caused by concomitant diseases: diabetes mellitus, pyelonephritis, chronic pancreatitis, erythremia, biliary dyskinesia, genitourinary tract infections, myeloma, hemolytic anemia, diseases of the gastrointestinal tract or central nervous system.
It can also occur against a background of magnesium or potassium deficiency, excess vitamin D, poor diet, deteriorating environmental conditions, and frequent emotional stress.
Treatment of the disease
For a disease such as dysmetabolic nephropathy in children, treatment involves the following:
- drinking normal amounts of water;
- diet therapy;
- normalization of lifestyle;
- specific methods of therapy.
To reduce the concentration of soluble substances in the urine, the child needs to drink as much water as possible.
It is best to give your child water before bed. It is advisable that the water be without gases.
For oxalurgy
When treating oxalurgy, the following foods should be excluded from the diet: carrots, chocolate, cocoa, sorrel, beets, cranberries, spinach, and aspic.
It is advisable to eat as much cabbage and potatoes as possible.
Such products can reduce the intake of oxalates in the body. Pears, dried apricots and prunes will also have a positive effect on the patient’s body.
As for medications, when treating oxalate nephropathy, the child is prescribed the following medications:
- Cyston;
- Pyridoxine;
- vitamins A, E, as well as vitamin B6;
- magnesium oxide.
For uraturia
When treating uraturia, the following foods should be excluded from the diet: beans, peas, cocoa, nuts, kidneys, liver.
A small patient is recommended to consume at least 2 liters of water per day. Infusions such as oat decoction, birch leaf decoction, clover decoction, and dill decoction will have a beneficial effect on the body.
Herbal preparation Cyston
The diet for dysmetabolic nephropathy in children of the urate type is based on the consumption of plant and dairy products.
In addition to changes in diet, the child is prescribed the following medications:
- Cyston;
- Etamide;
- Phytolysin;
- Allopurinol;
- Etamide.
The consumption of citrate mixtures, such as Solimok, Magurlit and Blemaren, is often prescribed.
For phosphaturia
With this type of disease, the child is strictly contraindicated in consuming foods high in phosphorus. These products include: cheese, caviar, chicken, liver, chocolate, and peas.
For cystine nephropathy
Treatment for this type of disease involves a strict diet and consumption of huge amounts of fluid.
In case of cystine nephropathy, consumption of fish, meat, cottage cheese and eggs is contraindicated.
Every day, the child should drink at least 2 liters of water per day.
A strict diet, as a rule, must be followed for at least a month and a half. In addition to a high fluid regimen and diet, drug treatment is also necessary.
Drug therapy for cystine nephropathy includes consumption of:
- vitamin A;
- Blemarena;
- citrate mixture.
In rare cases, cystinosis may require a kidney transplant. This operation is usually performed before chronic renal failure develops. This operation can significantly increase life expectancy by more than 10 years.
Diagnostics
One of the main tests indicating the development of metabolic nephropathy is a biochemical urine test. It allows you to determine whether there are abnormalities in the functioning of the kidneys, thanks to the ability to detect and determine the amount of potassium, chlorine, calcium, sodium, protein, glucose, uric acid, cholinesterase.
- Nephropathy: what it is, classification, causes, diagnosis, symptoms and treatment
Important! To carry out a biochemical analysis, you will need 24-hour urine, and to ensure the reliability of the result, you need to refrain from drinking alcohol, spicy, fatty, sweet foods, and foods that color the urine. The day before the test, you should stop taking uroseptics and antibiotics and warn your doctor about this.
The degree of change in the kidneys, the presence of an inflammatory process or sand in them will help to identify diagnostic methods: ultrasound, radiography.
Prognosis and prevention
If you follow the diet described above, as well as with drug therapy, urine returns to normal.
However, it is worth noting that if treatment is not effective, the child may develop urolithiasis and kidney inflammation. Often a complication in such a case is pyelonephritis.
To avoid identifying a disease such as dysmetabolic nephropathy in a child’s body, it is necessary to pay individual attention to the child’s urinary system.
To prevent all possible relapses of the disease, it is recommended to undergo preventive courses of antimicrobial therapy using phytouroseptics and uroseptics. Also, prevention of dysmetabolic nephropathy implies compliance with the correct drinking regime and proper diet.
To avoid detection of a disease such as dysmetabolic nephropathy, the child needs to consume only healthy foods. It is also very important to undergo a complete examination of the body at least once a year.
Examination stages
If there is a suspicion of a disease such as metabolic nephropathy, the therapist, after an initial examination, prescribes an examination and consultation with a urologist or nephrologist. Urine tests are carried out using various methods: according to Zimnitsky, Addis-Kakovsky, Nechiporenko, pH is determined, sediment is examined. It is important to identify which salts are excessively produced by the body.
If there are signs of infection, urine culture is performed to determine sensitivity to the antibiotic. A clinical blood test and biochemistry will provide a lot of information about the condition of the entire body and kidneys. An ultrasound of the abdominal cavity is required. In some cases, radioisotope diagnostics is prescribed.
Diagnostic measures
To establish a diagnosis, ultrasound examination of the kidneys and bladder may be useful.
There may be no changes in the kidneys of children during ultrasound diagnostics; in adult patients, there are multiple salt inclusions and microliths. In addition, a number of specific and nonspecific tests are prescribed, some of which confirm the diagnosis of dysmetabolic nephropathy, others help identify concomitant pathology:
• study of general and biochemical urine analysis; • blood biochemistry: urea, creatinine, uric acid, sugar, calcium, etc. • flora culture and sensitivity to antibiotics; • Nechiporenko's test, • study of anti-crystal-forming properties of urine (ACOSM); • testing urine for calciphylaxis and peroxides; • test for cystine in urine.
Additionally, studies may be prescribed: excretory urography, scintigraphy, retrograde uretero- and pyelography, computed tomography and magnetic resonance imaging. This instrumental diagnosis is carried out to clarify the cause, and is more often used for nephrourolithiasis.
A set of measures for treatment
Treatment of dysmetabolic nephropathy (regardless of its type) includes a whole range of measures:
- making an accurate diagnosis based on the necessary medical examinations;
- taking medications prescribed by a specialist;
- specific therapy (physical therapy);
- a diet that helps reduce salt load;
- rationing of fluid (water) consumption;
- lifestyle change.
Important! Under no circumstances should you interrupt the prescribed course of treatment, even if your urine tests are normal!
Causes of the disease
The main causes of dysmetabolic nephropathies in children include:
- metabolic disease;
- poor nutrition;
- deficiency of vitamins B6, A, E, hypovitaminosis;
- hypervitaminosis of vitamin D.
Most often this is observed after treatment of rickets in a child. Other reasons:
- deficiency of magnesium and potassium, excessive intake of calcium into the body;
- neuro-arthritic diathesis, stress;
- inflammation of the intestines, chronic pancreatitis;
- liver diseases;
- acute infectious diseases;
- stagnation of urine;
- oncology, radiation therapy;
- taking medications.
Prevention
In preventing the development and exacerbation of nephropathy, drinking regimen is important. Drinking enough water allows you to better flush out salts from the kidneys through urine. It is very important to eat right, not to use contraindicated foods, and to normalize the amount of salt in the diet. Any inflammatory or infectious diseases, especially those of the genitourinary system, have an adverse effect. They should be avoided, and if an illness occurs, be treated promptly by seeking advice from a specialist.
Maintaining a daily routine, alternating periods of work and rest, and standardized physical activity - all this helps maintain the immune system and fight the disease. It is important to perform personal hygiene procedures, this helps to avoid pathogens from entering the organs of the urinary system in an ascending manner. With metabolic nephropathy, you should monitor the condition of not only the kidneys, but also the endocrine organs, and seek medical help at the first signs.
Causes
Dysmetabolic nephropathy in childhood can develop as a result of long-term use of certain groups of drugs (sulfonamides, cytostatics, diuretics), with excessive physical exertion and intoxication.
Precipitation of salts can occur in the absence of pathological causes when exposed to certain external factors :
Internal provoking factors can also serve as:
- hormonal imbalances,
- prolonged adherence to bed rest during illness,
- infectious lesions of the urinary tract,
- congenital pathologies of the ureters and kidneys.
All this leads to the accumulation of salts in the kidney tissues in the form of precipitation.
Causes and risk factors
- Kidney nephropathy symptoms, treatment and types
Depending on the etiology, the disease can have two forms:
- Primary. The disease is hereditary in nature and is characterized by the rapidity of development and the depth of damage to the renal structures, up to renal failure.
- Secondary. It occurs in the course of life due to certain disruptions in the body associated with calcium metabolism disorders, an excess in the body of oxalic acid salts, calcium oxalates and phosphates - insoluble compounds that settle in the kidney structures and other urinary organs.
The secondary form of metabolic nephropathy can be asymptomatic for a long time, destroying the kidneys, and also leading to urolithiasis. In addition, the disease often progresses against the background of other pathologies of the urinary system.
The reasons why secondary metabolic nephropathy occurs:
- malfunctions of the organs and glands of the endocrine system - diabetes, obesity;
- infection of the genitourinary tract;
- pathological changes in the organs of the urinary system (ureters, urethra, bladder), leading to stagnation of urine and the development of inflammatory processes, as well as kidney damage;
- diseases of the digestive system;
- helminthic infestations;
- the presence of malignant tumors in the body;
- poor nutrition.
Failure of metabolic processes can occur due to uncontrolled use of medications, as well as after radiation therapy.
The causes of this kidney disease in an infant may be associated with the pathological course of pregnancy in the mother (preeclampsia, preeclampsia), which inevitably leads to oxygen starvation of the fetus and disturbances in its development.
An unfavorable environmental situation, consumption of food rich in artificial additives, dyes, products with GMOs, and widespread use of chemicals in everyday life significantly aggravate the risks of developing a dangerous pathology.
Drug treatment
Regardless of the form of the pathological process, it is customary to take metabolic and membrane protective therapy as the basis for drug treatment. If the disease occurs against the background of oxalosis, then the patient definitely needs to take vitamins B1, 6, which will help improve the process of glycine metabolism.
These substances can be obtained both from complex medications in which they are present, and from highly specialized products. It must be taken orally, and always in a higher dosage from 20-60 to 100 mg per day. The procedure is best performed in the morning or afternoon, and the average course of therapy is 14-21 days.
Vitamin preparation in original packaging. Source: gosapteka.pro
Most often, therapy consists of the drug Magne B6, which additionally contains magnesium and pyridoxine. In children it is allowed from 12 years of age. You should drink 1-2 tablets three times a day. The duration of the course is 14-21 days. Using the same scheme, you can take Multi Tabs B-complex. But the duration of treatment will be 60-90 days.
Patients with oxaluria and uraturia must take vitamins A and E, in a dosage appropriate to their age group. A medication such as AEvit is often used. To restore the water-electrolyte balance and acid-base environment, a solution of Dimephosphone in a 15% concentration is introduced into the complex.
The dosage is calculated according to body weight (1 ml per 5 kg of weight). Allowed for use by adults and children at 30-50 mcg/kg. The duration of treatment ranges from three weeks to two months. Since the solution has a bitter aftertaste, it can be washed down with milk, tea, or fruit juice to make it easier to take.
Among the effective metabolic agents, the Elkar solution at 20% concentration has proven itself well. Each milliliter of the product contains 200 mg of active ingredient. Produced in bottles of 25, 50 and 100 ml. Inside there is a clear, odorless liquid containing L-carnitine, which is identical in chemical and biological properties to the natural substance.
It takes an active part in various metabolic processes occurring in the body. Thanks to it, the functioning of mitochondria is restored and energy metabolism within cells improves. The drug is characterized by a good level of absorption into the intestine after oral administration.
The drug Elcar for the treatment of DN. Source: lekarstva.plus
The highest level of concentration of the active substance in the blood plasma is observed after 180 minutes, and the therapeutic effect lasts for nine hours, after which the drug is excreted by the kidneys. It is allowed to be used to treat children starting from the first year of life. The dose is individual and depends on age, the course of therapy is 30 days. The drug has no contraindications for use.
To prevent pathological changes in the renal vessels, it is necessary to control and maintain blood sugar levels at a normal level. For this purpose, it is recommended to introduce medications into the therapeutic complex, the action of which is aimed at reducing the production of glucose by the body.
With the development of microalbinuria, it is imperative to carry out treatment aimed at eliminating the symptoms of arterial hypertension. For this purpose, inhibitors of angiotensin-converting enzymes are used. In most cases, preference is given to prescribing Enalapril in small doses. The patient is also recommended to adhere to a protein diet.
What is dysmetabolic nephropathy?
This disease is caused by metabolic disorders, resulting in changes in the composition of urine. It contains an increased content of protein, red blood cells, leukocytes and salts. The latter lead to the formation of stones and the development of urolithiasis, damage to the renal structures, and impaired renal function.
Dysmetabolic nephropathy in children is accompanied by structural changes in the kidneys
Unfortunately, in recent years, dysmetabolic nephropathy (DN) has become younger. It is diagnosed even in children of the younger age group, at the age of 4–5 years, which significantly worsens the prognosis.
Preventive actions
If dysmetabolic nephropathy in children is identified in a timely manner, clinical recommendations are followed, drug treatment tactics are followed, as well as dietary nutrition, then in the future one can count on a favorable prognosis. Positive dynamics are recorded by observing stable normal indicators of the biochemical composition of urine.
Canephron is used as part of complex drug treatment as a herbal medicine. Source: gloriamed.ru
In case of deviation from therapeutic tactics, neglect of taking medications and poor nutrition, the child will subsequently develop urolithiasis and pyelonephritis. If cystinosis occurs, then the only option is to perform a kidney transplant.
As medical practice shows, such measures cannot exclude a fatal outcome, since cystine crystals are also deposited in the graft. This causes death in patients aged 15 to 19 years. Patients with this diagnosis are monitored by a pediatrician and nephrologist.
IgA nephropathy
- the most common of all glomerulopathies. It was first described by Berger and Englet back in 1968. IgA nephropathy can occur at any age, but children and young people (between 10 and 30 years) are most often affected. However, it can also occur in children under 10 years of age; IgA nephropathy has been described in 3-year-old children. In most cases, the disease progresses slowly, but the risk of chronic renal failure leading to end-stage renal failure is still quite high.
Epidemiology of IgA nephropathy in children
Due to the lack of serological markers of IgA nephropathy
The diagnosis can only be confirmed with a kidney biopsy, so the extent of the disease is not precisely known. Although indications for kidney biopsy may vary from country to country, IgA nephropathy is reported to be more common in Japan and Australia and less common in North America.
The existence of a hereditary predisposition to IgA nephropathy
, but the genes responsible for this predisposition have not been precisely identified. IgA nephropathy is rare in American blacks; the incidence is higher among whites, Asians, and American Indians living in New Mexico. Several familial cases have been described. Men get sick 2-6 times more often than women.
Apparently IgA nephropathy
should be considered as a syndrome and not as a separate disease. In most cases it is idiopathic (primary), although secondary forms also exist. In secondary IgA nephropathy, deposits of immune complexes, which mainly include IgA, are found in the glomeruli in most cases. Renal dysfunction is usually not severe.
Perhaps these data will help shed light on the pathogenesis of idiopathic IgA nephropathy. IgA nephropathy can be accompanied by a number of chronic diseases and conditions. Among them are cirrhosis and other severe liver damage; previous portacaval shunting; celiac disease and other enteropathies; Crohn's disease; chronic obstructive pulmonary diseases, including chronic obstructive bronchitis; cystic fibrosis; idiopathic interstitial pneumonia; monoclonal gammopathy with IgA secretion; some types of cancer; mycosis fungoides; infectious diseases, including HIV infection, mycoplasma infection, toxoplasmosis and leprosy; dermatitis herpetiformis; seronegative spondyloarthropathy; recurrent mastitis; episcleritis.
In addition to IgA nephropathy
pronounced IgA deposits appear to occur only in lupus nephritis, but a number of other characteristic signs of IgA nephropathy make it possible to distinguish these diseases from each other.
Glomerulonephritis, morphologically resembling IgA nephropathy
, develops in 75% of children with hemorrhagic vasculitis. Many experts consider such glomerulonephritis and IgA nephropathy to be different manifestations of the same disease - therefore, they may have a common pathogenesis. Indeed, the geographic distribution of these diseases is similar, both are rare in American blacks, both have known familial cases (including in identical twins), and some patients with idiopathic IgA nephropathy developed hemorrhagic vasculitis after several years.
Of all forms of IgA nephropathy
the most common is idiopathic IgA nephropathy; glomerulonephritis with hemorrhagic vasculitis is slightly less common and in children usually resolves without treatment.
Pathogenesis of IgA nephropathy in children
Despite an impressive number of studies, the pathogenesis of IgA nephropathy
still remains a mystery. It is generally accepted that this is an immune complex disease in which immune complexes are deposited mainly in the mesangium of the glomeruli. It is not yet clear whether immune complexes enter there from the bloodstream or are formed in the glomeruli themselves.
Version: Clinical guidelines of the Russian Federation (Russia)
Exhibition "Healthcare"
May 15-17, Almaty, Atakent
Free ticket using promo code KIHE19MEDE
International exhibition "Healthcare"
May 15-17, Almaty, Atakent
Free ticket using promo code KIHE19MEDE
Mode and amount of fluid consumed
Oddly enough, the most effective and universal remedy for the treatment of metabolic disorders of the kidneys is water. It is this that helps reduce the concentration of salts dissolved in urine.
Depending on the degree of pathological changes in the kidneys and the individual physiological characteristics of the patient, the attending physician prescribes both the total daily amount of required fluid and the mode (that is, schedule) of its consumption. In any case, the recommended volume of water will be significantly more than for a healthy person.
For some types of nephropathy, doctors may recommend a course of medicinal mineral waters (for example, for oxalate - “Slavyanovskaya” or “Smirnovskaya”).
Methods of therapy
The disease is not dangerous, but causes discomfort. Therefore, you need to follow your doctor's recommendations. Treatment of dysmetabolic nephropathy in children and adults has its own specifics. The decisive factor for prescribing therapy is the type of pathology.
Treatment of children
If oxaluria is detected in a child, frequent fluid intake is prescribed. If salts are deposited in the kidneys, you need to drink at least 1.5 liters of water per day. Water is given to the child at night.
For this, the best remedy is mineral water. You can give your child compote or cranberry juice. Herbal tea has a positive effect.
Dysmetabolic kidney nephropathy - what is it?
Metabolic nephropathy includes kidney diseases caused by metabolic disorders (metabolism) and the accumulation of salts (oxalic, uric or phosphate) or amino acids in the body. This illness may be:
- congenital (primary), associated with genetic disorders (inherited) or pathological course of pregnancy;
- acquired (secondary), caused by an increased intake of certain substances into the body, concomitant diseases of other organs (or long-term use of medications for their treatment).
Sources used:
- https://tvoyapochka.ru/bolezni/metabolicheskaya-nefropatiya
- https://uromir.ru/nefrologija/porazhenie/metabolicheskaja-nefropatija.html
- https://mfarma.ru/mochepolovaya-sistema/bolezni-pochek/metabolicheskaya-nefropatiya
- https://www.syl.ru/article/388810/dismetabolicheskaya-nefropatiya-priznaki-simptomyi-i-lechenie-dieta
- https://pochki2.ru/bolezni/vetabolicheskaya-nefropatiya.html
- https://m.baby.ru/wiki/lecenie-i-kliniceskie-rekomendacii-pri-dismetaboliceskoj-nefropatii-u-detej/
Uratnaya
This type of disease is not as common as oxaluria.
This type is characterized by a high concentration of uric acid in the baby’s urine. Uraturia can be a genetic pathology or will develop in parallel with pyelonephritis and anemia.
The main reasons for its appearance are:
- Poor nutrition.
- Long-term treatment with any medications, for example, diuretics.
If treatment for this type of disease is not started in time, then a large amount of uric acid can affect the development of gouty arthritis.
The symptoms that appear are unclear and if the level of salt in the urine is low, the child will not be able to feel it. As he gets a little older and with an increased amount of salt, the child will become excitable and become much more whiny and capricious. Over time, salts begin to be deposited in the joints, and a rash appears on the skin that will constantly itch. In some cases, the child may begin to choke. This condition manifests itself in the form of seizures.
You can determine the appearance of this type of disease by looking closely at the baby’s urine; it will change its color and become reddish-brown. But still, with a routine urine test, it will be much easier to establish or refute pathology. In addition, you may also need the result of a blood test.
Therapy of urate pathology is carried out in compliance with the following rules:
- Following a strict diet. Sometimes by changing your diet you can get rid of the disease.
You should not give your baby: strong broths, chocolate, tea, fatty meat and fish, flour.
For breakfast, you can eat lean boiled fish or meat, but no more than twice a week.
Also suitable are dairy products, melon, watermelon, sweet berries, vegetable soups without meat, and a lot of fresh vegetables.
You need to consume more fluids so that the urine is not highly concentrated. You need to drink at least one and a half liters of water per day.
For urate dysmetabolic nephropathy, doctors prescribe therapy with drugs such as Cyloric, allopurinol, milurite, only the full course of treatment must be completed.
In addition to the use of medications, dysmetabolic nephropathy in children is treated with the prescription of vitamin complexes, which contain a high concentration of vitamins B and C. They will help restore and support the metabolic processes taking place in the baby’s body, which will greatly alleviate his condition.
When dysmetabolic nephropathy is detected in children, it is necessary to strictly select your baby’s food and treat this pathology. This is the only way to restore health and maintain it for a long time.
Treatment
Therapy is not based on medications alone. The basis is a change in diet and drinking regime. Clinical recommendations are as follows:
- increasing the volume of fluid consumed to 1.5–2 liters per day;
- forced urination every 2 hours to cleanse the kidneys;
- diet.
Without dietary nutrition, recovery is impossible. The selection of a diet is carried out by a doctor based on the type of disease. If you have oxalate deficiency, you should give preference to cabbage and potatoes. It is these vegetables that reduce oxalate levels. It is useful to eat dried fruits and drink mineral water. You need to give up rich meat broths, beets, carrots, oxalic acid, which is contained in sorrel, as well as products containing cocoa.
Clinical guidelines play an important role in treatment
If the urate content increases, you should exclude meat dishes, animal by-products and legumes. Dairy products and plant foods are beneficial. With phosphate DN, it is worth limiting the consumption of phosphate foods, such as legumes and chocolate. Acidification of urine is done using mineral water. Taking vitamin C is also justified.
If you have cystinosis, you should not eat foods rich in sulfur and methionine. Therefore, fish and meat foods are excluded from the child’s diet, and cottage cheese and eggs are prohibited. Dietary nutrition should be followed for at least a month. You can return to the regular menu only after your doctor’s approval.
In the treatment of diseases of the urinary system, it is the drinking regime that is important. The more often you urinate, the less likely it is for salt deposits and stone formation.
Along with dietary nutrition, drug treatment is carried out, which involves the use of antioxidants, herbal medicines and vitamins. Medicines are prescribed by a doctor.
In the absence of proper and effective treatment, consequences may arise in the form of urinary or cholelithiasis, pyelonephritis, cystitis, arthropathy, gout. The most severe complication is renal failure.
Symptoms
The disease is characterized by a latent course, that is, the disease may not make itself felt for a long time. More often it is discovered by chance during an examination. It is the change in urine that is the first sign of DN. Not only its composition changes, but also its color. It becomes cloudy; if it sits in a pot for a long time, sediment will form and a coating may remain on the walls, which is difficult to remove without household chemicals.
As stones form, symptoms become more pronounced
Main signs of the disease:
- headache;
- fatigue;
- muscle weakness;
- pain in the lower back, in the kidney area;
- low-grade body temperature;
- redness in the genital area, itching, discomfort;
- bloating;
- allergic skin rashes;
- lowering blood pressure;
- vegetative-vascular dystonia;
- excess weight.
The accumulation of salts is accompanied by inflammation, the process of stone formation begins, urination becomes painful, and enuresis is possible.
Description of the treatment process
Treatment recommendations boil down to maintaining proper nutrition and drinking regimen, and taking medications. Features of therapy may differ depending on the type of nephropathy (urate, phosphate, etc.).
Medicines for a child of any age should be prescribed only by a doctor. This treatment is supervised by a specialist.
Depending on the type of nephropathy, the following drugs can be used:
Any dysmetabolic nephropathy requires sufficient water load, which allows reducing the amount of salts in the urine. Forced emptying of the bladder according to a special regime is effective - every 2 hours.
Different types of nephropathy in a child require a different diet. For example, if oxalates predominate in the body, exclude the following foods:
- meat broth;
- aspic;
- beets and carrots;
- sorrel, spinach;
- currants and cranberries;
- cocoa.
On the contrary, potatoes, cabbage, dried apricots and prunes, and pear will be useful for oxalates.
With phosphate nephropathy, there are no significant dietary restrictions, but it is worth reducing your intake of:
- milk and products containing it;
- pickles and smoked meats;
- sweets, baked goods.
Meat, fish, cereals, vegetables and fruits with sourness are useful for phosphaturia.
If cystinosis is diagnosed, it is necessary to reduce the consumption of protein-containing foods. At an advanced stage of development, the diet is not effective. In this case, organ transplantation is performed.
In case of urate, it is necessary to exclude the following foods from the diet:
- meat and meat broth;
- nuts and legumes;
- sweets, baked goods;
- cocoa;
- fatty, fried, spicy foods.
Dairy products, cereals, vegetables and fruits will be useful for urates.