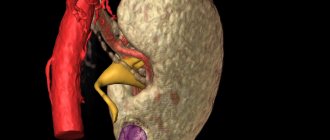
Retroperitoneal fibrosis is a chronic inflammatory process in the fibro-fatty tissue of the retroperitoneal space. This condition causes kidney damage, ureteral obstruction and pelvic organ disease. The pathology is most often diagnosed in men 30–60 years old; patients complain of pain in the lower back and groin, increased blood pressure, and difficulty urinating. In 30% of patients, a tumor-like formation is palpable in the pelvic region. A nephrologist explains in detail how kidney fibrosis manifests itself, what it is and what complications can develop.
Renal fibrosis: overview characteristics
The consequence of inflammatory or infectious diseases can be kidney fibrosis (retroperitoneal fibrosis, formerly known as Ormond's disease). The disorder is a consequence of interstitial fibrosis and one of the main mechanisms for the development of chronic renal failure (CKD).
It is important to know! Renal fibrosis develops at any age, including newborns and the elderly, but generally occurs between 30 and 60 years of age. For the most part, this is a male disease, since, according to statistics, women are susceptible to it half as often.
Conditions and stages of development
There are a number of reasons for the formation of excess connective tissue, which is kidney fibrosis. Each degree of pathology has a different effect on the functional changes of the organ. In diseases with a small amount of affected kidney tissue, fibronization processes are a normal protective response of the body, the purpose of which is to limit the source of inflammation. At this stage, the disease does not pose serious threats and can only partially reduce the functionality of the organ.
The second period is more difficult - the work of the kidney slows down or stops altogether, depending on the strength and duration of the influence of the aggressor factor, the timeliness of treatment with medicinal or surgical methods. The final stage is the development of chronic renal failure, and then the death of the patient.
Classification
There are many types of classifications, the first of which divides the disease into two forms:
- Primary – idiopathic fibrosis, which is a combination of pathology with autoimmune processes that arise against the background of decreased immunity, allergies or long-term use of certain medications.
- Secondary - accompanied by the destruction of the internal structure of damaged kidneys, as a result of which the connective tissue grows and affects not only the kidneys, but also other nearby organs (pancreas, ureters, intestines).
In accordance with the localization of the foci of the disease, right and left fibrosis are distinguished. Rarely, the pathology spreads to both kidneys. Since the exact reasons for the appearance and development of renal fibrolipomatosis have not been established, scientists put forward different versions. Some are inclined to believe that the disease is caused by various inflammatory processes (pyelonephritis, endometritis, pancreatitis), others blame mechanical damage to the kidneys.
Nature of manifestations
At each stage of the disease, symptoms intensify and their number increases. First, a dull aching pain occurs in the lumbar region. Often it goes away on its own over time, which allows pathology to develop, because the patient does not attach importance to periodic discomfort. But soon the pain returns, bringing with it uremia and impaired renal function. Later other signs appear:
- high blood pressure;
- loss of appetite;
- itching;
- swelling;
- elevated temperature;
- weakness;
- drowsiness;
- intoxication.
Over time, when irreversible processes begin, the urinary canals, lungs and even the stomach will be affected. Failures can also occur in other organs.
Types of complications
Without the use of proper control methods, a complication such as chronic renal failure develops, and soon after this, kidney fibroma. These are small single or multiple formations (polycystic) of a benign nature, the causes of which have not yet been clearly established (they occur more often in women). In the first few days, cysts are often mistaken for cancer, because the pathologies look similar in the pictures.
Another result of the progressive disease is varicose veins - narrowing of blood vessels. In turn, the consequence of this is the formation of trophic ulcers - skin defects that do not heal for a long time.
Even after carrying out the necessary medical actions, a relapse of the disease may occur, accompanied by failures in the system of filtration and removal of metabolic products, as well as urinary retention and general intoxication of the body against this background. Fibroids subsequently cause additional discomfort.
Fibrolipomatosis, which occurs in the renal sinuses (pedunculitis), often occurs - penetration of urine into the interstitial tissue, and from there into the blood.
Attention! The consequences also do not bypass the patient’s intestines - obstruction causes a delay in processed products, which ultimately results in intoxication.
All of the complications described above require long-term and scrupulous treatment, and in the absence of it they can cause the death of the patient.
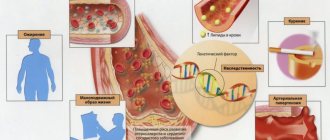
Causes
The disease usually occurs in people suffering from chronic pancreatitis. Other reasons for the development of pancreatic fibrolipomatosis may be diabetes, other endocrine diseases, as well as toxic damage to the body. Excessive drinking and smoking not only contribute to the development of pathology, but also stimulate other dangerous processes.
For example, you should be wary of gallstone disease. In 9 out of 10 cases it is the cause of the development of chronic pancreatitis. Also, fibrolipomatosis can appear due to various injuries or mechanical wounds, infections, taking certain medications, pathologies of the cardiovascular system, which disrupt hormonal levels, disrupt the metabolism in the body, and interfere with the proper blood supply to internal organs.
Diagnostic examination
This kidney disease is very difficult to diagnose at an early stage. The symptoms are not pronounced, as a result of which suspicions of violations in the patient arise only in later periods, when the situation is seriously complicated. Progression of the disease can be observed within a couple of months (from the beginning of the growth of connective tissue) or occur gradually (2-10 years). It is possible to see problems at the stage of their appearance by chance, during other examinations not related to the kidneys.
Diagnostics is carried out in two ways:
- by studying urine and blood tests (general examination, biochemistry);
- using instrumental diagnostics - ultrasound, MRI, CT.
A common practice is fluoroscopy, which reveals changes in the ureters and renal pelvis. Both methods demonstrate that there are problems that need to be immediately investigated and corrected.
Diagnostics
Diagnosis is carried out using ultrasound.
Ultrasound diagnostics is aimed at assessing several parameters of the pancreas:
- current size and shape of the organ;
- location in the abdominal cavity;
- echogenicity (degree of homogeneity and structure of pancreatic tissue).
Fibrolipomatosis is a constant companion of pancreatitis. It can accompany a person all his life, practically without bothering him, reminding him of himself with infrequent exacerbations. For this reason, the disease progresses very slowly. Unfortunately, even modern medicine cannot always detect fibrolipomatosis in a sick person in a timely manner.
It will be very good if the doctor notices on an ultrasound that the patient has increased echogenicity, which occurs against the background of impaired metabolism or inflammation of the pancreas. Also, the presence of this pathology is indicated by organ obesity.
Complex treatment
As soon as there are suspicions of renal fibrosis, sinus fibrolipomatosis or lipomatosis, it is necessary to immediately undertake an in-depth diagnosis of the disease, and then begin treatment. Timeliness and efficiency are the key to success, because delaying therapy can only aggravate the situation and lead to a lot of complications.
After successful treatment of acute fibrosis, both surgically and medicinally, it is still necessary to strictly visit the doctor and carry out a list of certain tests in order to avoid subsequent relapses.
Operation
When fibrosis is detected at later, serious stages, accompanied by the manifestation of some (or many) complications, changes in the internal structure, degradation of kidney functionality, drug therapy is no longer enough. Surgical intervention of varying degrees is used, depending on the severity of the disease:
- removal of overgrown tissue to free the ureter;
- liberation of the kidney from metabolic products;
- insertion of a stent to restore normal urine and blood flow;
- amputation of the entire affected organ or part of it (in advanced cases and provided that at least one kidney is functioning normally);
- removal of the ureter.
In the period before and after surgery, drug therapy also takes place, and it is aimed at reducing the growth of connective tissue.
Drug therapy
Treatment in the initial stages is much easier and more pleasant, since there is no need for surgical intervention. Therapy for acute fibrosis includes steroid hormones, drugs whose action is aimed at relieving the symptoms of inflammation and pain. In the chronic course of the disease, treatment is indicated, the purpose of which is to destroy genitourinary infections.
Early fibrosis involves the use of various absorbable agents aimed at stopping the growth of connective tissues and the formation of scars. In any case, it is important to establish the source of the disease (aggressive factors) and, if possible, stop their effect on the patient’s body.
Traditional methods of treatment also relieve fibrotic manifestations. Compresses from decoctions and various infusions help eliminate pain and slow down the development of the disease. It is equally important to follow a diet throughout the entire period of treatment and maintain the drinking regimen recommended by the doctor.
Disease prognosis
Predicting the development of fibrosis is problematic; it is necessary to take into account the nature of the disease, the condition of the kidneys and urinary system, and take into account the complications that arise. Conservative therapy can only bring temporary effect. However, a more reliable method of treatment is surgery, in which the ureter is moved. If you take steroid hormones after surgery, the prognosis will be more comforting. But surgery also does not guarantee that a relapse will not occur in a few months or years. With fibrosis, a fatal outcome also occurs, most often in the case of renal failure. If treatment is applied on time, the prognosis may be more comforting. If it was possible to prevent changes in the kidneys and the onset of renal failure, then this increases the chances of a successful outcome to 60%.
Treatment prognosis and disease prevention
The process of the appearance of this disease has not been reliably studied, and therefore there is no list of unambiguous methods for preventing the disease. Doctors advise to treat chronic infections carefully and responsibly, monitor the strengthening of the immune system, and lead a healthy lifestyle. And if the first signs of exacerbation appear, in no case should you ignore the body’s signals; you should listen to them and immediately seek help from specialists. It would also be a good idea to periodically donate blood and urine for general analysis for reasons of prevention, be examined by the doctor assigned to the patient, and also undergo a course of vitamin therapy.
The prognosis for treatment at any stage of fibrosis can be positive if everything is done comprehensively, correctly and in a timely manner.
It is important to know! It is important to remember that neither medication, nor surgery, nor, especially, traditional treatment alone will help if the patient continues to be exposed to adverse factors.
Therefore, along with laboratory and instrumental diagnosis of the disease, the doctor needs to carefully study the patient’s medical history, which will help determine the most likely foci and causes of the disease and subsequently build the correct treatment strategy.
Disease prognosis
Predicting the development of fibrosis is problematic; it is necessary to take into account the nature of the disease, the condition of the kidneys and urinary system, and take into account the complications that arise. Conservative therapy can only bring temporary effect. However, a more reliable method of treatment is surgery, in which the ureter is moved. If you take steroid hormones after surgery, the prognosis will be more comforting. But surgery also does not guarantee that a relapse will not occur in a few months or years. With fibrosis, a fatal outcome also occurs, most often in the case of renal failure. If treatment is applied on time, the prognosis may be more comforting. If it was possible to prevent changes in the kidneys and the onset of renal failure, then this increases the chances of a successful outcome to 60%.
Preventive recommendations
Until now, doctors have not established clear preventive rules regarding this disease. Considering that about 80% of cases of tumor appearance are considered acquired, the best option is to lead a healthy lifestyle and avoid excessive stress on the organs of the excretory system.
Recommendations:
- drink at least 1.5 liters of liquid daily, avoid carbonated drinks and coffee;
- It is prohibited to abuse alcoholic beverages;
- normalize your diet, stick to your diet;
- do not allow hypothermia of the genitourinary system;
- promptly treat diseases of the excretory system, kidneys, and other ailments of an infectious nature.
Angiomyolipoma of the left kidney is a benign formation, but can develop into a malignant tumor. If negative symptoms appear, consult a doctor, start therapy, take care of your health!
A specialist will tell you more about what renal angiomyolipoma is in the following video:
Manifestation of the clinical picture
The symptoms of angiomyolipomas directly depend on the size of the tumor. For small (up to 4 cm) tumors, in 80% of cases the disease is asymptomatic.
When the size increases beyond 5 cm, more than 70-80% of patients begin to feel the clinical manifestations of the disease, forcing them to see a doctor, namely:
- dull pain in the lower back and lateral areas of the abdomen, aggravated by turns and bending; according to various sources, the pain symptom is observed in 40-70% of patients;
- frequent and sudden changes in blood pressure levels – in 12% of cases;
- palpable (in some cases by the patient himself) neoplasm – in 22%;
- weakness.
When the tumor size reaches 10 cm in 80% of patients, normal renal symptoms occur.
Bleeding (blood in the urine) due to rupture of a tumor or its vessel usually occurs with large tumors. However, in some cases, hemorrhagic manifestations can be observed even with relatively small sizes of AML.
Tumor rupture is accompanied by internal hemorrhage, severe acute pain and hemorrhagic shock (pallor, arterial hypotension, tachycardia, dizziness, fainting). A picture emerges of a growing palpable tumor.
What is pancreatic lipofibrosis?
Pathologies such as lipomatosis and pancreatic fibrosis together form lipofibrosis. The reasons for the appearance are almost the same:
- Lipomatosis. Lipomas (fat formations) appear on the parenchyma of the gland if its dead cells are replaced by adipose tissue.
- Fibrosis. Dead areas of parenchyma are replaced by fibrous or scar tissue (a type of connective tissue).
Such diffuse tissue changes occur when pancreatic functions are impaired. The term “diffuse” is used by doctors during ultrasound examination of a diseased organ. By it they do not mean a disease that needs to be treated, but a uniform proliferation of connective or fatty tissue throughout the gland. It replaces dead areas so that the organ maintains its volume and integrity.
With diffuse changes in the pancreas, there are no neoplasms, but they can appear if a person does not fundamentally change his lifestyle. One of the possible pathologies is cystic fibrosis of the pancreas.