EXCRETORY ORGANS
In the process of life activity in the human and animal bodies, significant amounts of decomposition products of organic compounds are formed, some of which are not used by cells. These breakdown products must be removed from the body.
The end products of metabolism secreted by the body are called excreta, and the organs that perform excretory functions are called excretory or excretory. The excretory organs of humans and animals include the lungs, gastrointestinal tract, skin, and kidneys.
Lungs – contribute to the release of carbon dioxide (CO2) and water into the environment in the form of vapor (about 400 ml per day).
The gastrointestinal tract secretes a small amount of water, bile acids, pigments, cholesterol, some drugs (when they enter the body), heavy metal salts (iron, cadmium, manganese) and undigested food residues in the form of feces.
The skin performs an excretory function due to the presence of sweat and sebaceous glands. Sweat glands secrete sweat, which contains water, salts, urea, uric acid, creatinine and some other compounds.
The main organ of excretion is the kidneys, which excrete with urine most of the end products of metabolism, mainly containing nitrogen (urea, ammonia, creatinine, etc.). The process of formation and excretion of urine from the body is called diuresis.
KIDNEY PHYSIOLOGY
The kidneys play an exceptional role in maintaining the normal functioning of the body. The main function of the kidneys is excretory. They remove decay products, excess water, salts, harmful substances and some medications from the body. The kidneys maintain the osmotic pressure of the body's internal environment at a relatively constant level by removing excess water and salts (mainly sodium chloride). Thus, the kidneys take part in water-salt metabolism and osmoregulation.
The kidneys, along with other mechanisms, ensure the constancy of the blood reaction (blood pH) by changing the intensity of the release of acidic or alkaline salts of phosphoric acid when the blood reaction shifts to the acidic or alkaline side.
The kidneys are involved in the formation (synthesis) of certain substances, which they subsequently remove. The kidneys perform a secretory function. They have the ability to secrete organic acids and bases, K + and H + ions. The participation of the kidneys not only in mineral, but also in lipid, protein and carbohydrate metabolism has been established.
Thus, the kidneys, regulating the amount of osmotic pressure in the body, the constancy of the blood reaction, carrying out synthetic, secretory and excretory functions, take an active part in maintaining the constancy of the composition of the internal environment of the body (homeostasis).
The structure of the kidneys. In order to more clearly understand the work of the kidneys, it is necessary to become familiar with their structure, since the functional activity of the organ is closely related to its structural features. The kidneys are located on both sides of the lumbar spine. On their inner side there is a depression in which there are vessels and nerves surrounded by connective tissue. The kidneys are covered with a connective tissue capsule. The size of an adult kidney is about 11x5 cm, the average weight is 200-250 g.
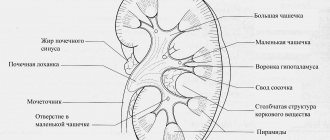
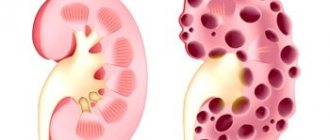
In a longitudinal section of the kidney, 2 layers are distinguished: the cortex is dark red and the medulla is lighter (Fig. 1).
Rice. 1. The structure of the kidney. A - general view; B — a section of renal tissue enlarged several times; 1 - capsule of the renal glomerulus;
2 - convoluted tubule of the first order; 3 - nephron loop; 4 - convoluted tubule of the second order; 5 - collecting tube.
A microscopic examination of the structure of mammalian kidneys shows that they consist of a large number of complex formations, the so-called nephrons. The nephron is the structural and functional unit of the kidney. The number of nephrons varies depending on the type of animal. In humans, the total number of nephrons in the kidney reaches an average of 1 million.
The nephron is a long tubule, the initial section of which, in the form of a double-walled cup, surrounds the arterial capillary glomerulus, and the final section flows into the collecting duct.
The following sections are distinguished in the nephron: 1) the renal (Malpighian) corpuscle consists of the vascular glomerulus and the surrounding capsule of the renal glomerulus (Shumlyansky-Bowman) (Fig. 2);
Rice. 2. Scheme of the structure of the renal corpuscle. 1 - bringing vessel; 2 - efferent vessel; 3 - capillaries of the glomerulus;
4 - capsule cavity; 5 - convoluted tubule; 6 - capsule.
2) the proximal segment includes the convoluted (convoluted tubule of the first order) and straight parts (thick descending limb of the nephron loop (Henle); 3) thin segment of the nephron loop; 4) distal segment, consisting of a straight (thick ascending limb of the nephron loop) and a convoluted part (second-order convoluted tubule). The distal convoluted tubules open into collecting ducts (Fig. 3).
Rice. 3. Diagram of the structure of the nephron (according to Smith).
1 - glomerulus; 2 - proximal convoluted tubule; 3 - descending part of the nephron loop; 4 - ascending part of the nephron loop;
5 - distal convoluted tubule; b - collecting duct. Circles show a diagram of the structure of the epithelium in various parts of the nephron.
Kidney anatomy
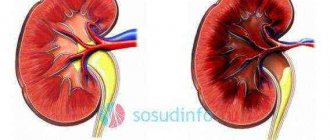
The kidneys are a paired organ that maintains the necessary internal environment of the body through the process of urine formation. Anatomy and physiology of the kidneys states that normally there should be two kidneys in the human body. These organs are located on both sides of the spinal column in the area of the third lumbar and 11th thoracic vertebra.
It is worth knowing: anatomically, the right organ is located slightly lower than the left, since it is adjacent to the liver.
The organs have a bean-shaped configuration. The approximate dimensions of a healthy adult kidney are 50-60 mm in width, 100-120 mm in length, and 30 mm in organ thickness. One kidney weighs approximately 150-280 g.
To supply the organ with blood, the renal arteries, which arise directly from the aorta, approach it. Inside the kidney, these arteries branch into many arterioles that supply the renal glomeruli. The nerves enter the kidney from the celiac plexus. They are needed to regulate the activity of the organ and ensure the sensitivity of the renal capsule.
There are two renal layers:
- Cerebral. This layer consists of nephron loops and collecting ducts. These tubes unite with each other in the medulla and form the so-called renal pyramids. Each of the pyramids ends with a papilla, which opens into the cups and pelvis.
- The cortical layer is represented by vascular glomeruli and renal capsules. The cortex contains the distal and proximal parts of the renal tubules.
Kidney unit
The main structural unit of the organ is the nephron. It consists of a glomerulus of blood vessels and a whole system of tubes and tubules. The vascular tangle is a large network of tiny capillaries, which is surrounded by a two-layer capsule called Bowman's capsule. The inner layer of the capsule is made up of epithelial cells, and the outer layer is made up of membranes and tubules.
The vascular tangle includes an efferent and afferent arteriole. Between these arteries is the juxtaglomerular apparatus. The cross-section of the afferent arteriole is twice as large as the cross-section of the efferent artery, so the pressure necessary for fluid filtration is constantly maintained inside the renal glomerulus.
The internal cavity of the capsule is transformed into a nephron tubule. This tubule consists of a section that begins directly at the capsule and is called proximal, as well as a loop and a distal segment of the tubule. The last section joins the collecting duct. Several of these tubes merge into single ducts, which open into the renal pelvis.
Depending on the location and structure of the tubular system, the following types of nephrons are distinguished:
- Cortical. These include intracortical and superficial. The last group is the smallest, accounting for only 1%. Superficial nephrons are distinguished by a small filtration volume, a shortened loop of Henle, and a superficial location of the glomeruli in the cortex. Intracortical nephrons are the most numerous group. They account for about 80% of the total. This group of nephrons is localized in the middle of the cortex. All main functions of filtering urine fall on the intracortical nephrons. The blood in the glomeruli of these nephrons flows under significant pressure due to the twice as large cross-section of the afferent arteriole.
- Juxtamedullary are a small group. It accounts for approximately 20% of the total number of nephrons. Most juxtamedullary nephrons are located in the medulla, but their capsule is located at the border of the cortex and medulla. In the nephrons of this group, the loop of Henle reaches almost to the renal pelvis. These nephrons perform concentrating functions in relation to urine. Juxtamedullary nephrons have the longest loop of Henle, and the cross-section of the efferent and afferent arterioles is the same.
Anatomy, physiology and age-related characteristics of the kidneys
Human kidneys (paired organs) are bean-shaped, weighing 120-200 g each. The dimensions of the kidney are 12x6x3 cm. The kidneys are located on the posterior abdominal wall on the sides of the spine at the level from the XII thoracic to the I-II lumbar vertebrae. The right kidney lies slightly lower than the left. In front of the kidneys are the peritoneum and the internal organs located at this level (stomach, duodenum, flexures of the colon, liver, pancreas and others).
The anterior part of the kidney is isolated
and
the posterior surface
and two edges -
a convex lateral
and
a concave medial.
On the medial edge there is a depression -
the renal gate,
which leads into
the renal sinus.
Through the gate, the artery and nerves enter the kidney; the renal vein, lymphatic vessels and ureters exit the kidney.
The renal sinus contains the major and minor calyces, the renal pelvis and adipose tissue. The outside of the kidney is covered with a dense fibrous capsule;
the kidney is surrounded by
a fatty capsule.
On a longitudinal section of the kidney, two layers are clearly distinguished: the outer or peripheral cortical layer and below it the inner medulla, divided into 8-12 pyramids.
The morphological and functional unit of the kidney is the nephron. Nephron
consists of a renal or Malpighian corpuscle and a urinary tubule about 50-70 mm long.
Malpighian body
contains a vascular glomerulus (about 50 capillary loops), covered externally by a double-walled Shumlyansky-Bowman capsule. The diameter of the renal corpuscle varies from 150-250 microns. The inner wall of the capsule, consisting of single-layer squamous epithelium, is closely adjacent to the walls of the capillaries of the vascular glomerulus, forming a biological filtering membrane. Between it and the outer wall of the capsule there is a slit-like cavity into which blood plasma filters from the capillaries of the glomerulus, called primary urine.
Vascular glomerulus
is a cluster of capillaries located between two arterioles, afferent and efferent, the so-called. "wonderful network"
Urinary tubules
begin from the slit-like cavity of the capsule, which directly passes into
the proximal
(first-order tubule) convoluted tubule, located in the renal cortex. Heading into the medulla, the proximal tubule straightens, makes a loop of Henle and continues into the distal tubule, which opens into the collecting duct. The collecting ducts pass through the renal medulla and open at the tips of the papillae. The final urine is collected in the renal pelvis, where the large renal calyces open, of which there are 2-3 in humans. Urine enters the cavity of the large renal calyces from several small calyces; the number of small renal calyces in one kidney ranges from 5 to 15. The large renal calyces, merging with each other, form one common cavity - the renal pelvis. The minor calyces, major calyces and the renal pelvis, according to most authors, are classified as the urinary tract.
The kidneys perform a number of excretory
and
homeostatic functions
in the human body. These include: 1) maintaining normal levels of water, salts and some substances (glucose, amino acids) in the body; 2) regulation of blood pH, osmotic pressure, ionic composition and acid-base balance; 3) excretion of protein metabolism products and foreign substances from the body; 4) regulation of blood pressure, erythropoiesis and blood coagulation; 5) secretion of enzymes and biologically active substances (renin, bradykinin, prostaglandin, etc.); 6) formation of urine.
In newborns and infants, the kidney is round. Its surface is lumpy due to its lobular structure, which is associated with insufficient development of the cortex at this age. The lobed structure of the kidney lasts up to 2-3 years. The length of the kidney in a newborn is 4 cm, the weight of the kidney is 12 g. In infancy, the size of the kidney increases approximately 1.5 times, and the weight reaches 37 g. During the period of first childhood, the length of the kidney is on average 8 cm, and the weight is 56 g In adolescents, the length of the kidney already reaches 10 cm, and the weight is 120 g.
Kidney growth occurs mainly in the first year of a child’s life. In the period of 5-9 years and especially in 16-19 years, the size of the kidney increases due to the development of the cortex, which continues until the end of adolescence. Brain growth stops by age 12. The mass of the renal cortex increases due to the growth in the length and width of the convoluted tubules and the ascending part of the nephron loops. The thickness of the cortex in an adult compared to that of a newborn increases approximately four times, and the thickness of the medulla increases only by two times.
The fibrous capsule of the kidney becomes clearly visible by the age of five, and by the age of 10-14 years, its structure is close to the fibrous capsule of an adult. The fat capsule begins to form only during the period of first childhood, while continuing to gradually thicken. By the age of 40-50, the thickness of the fatty capsule of the kidney reaches its maximum values, and in old age it becomes thinner and sometimes disappears.
With age, the topography of the kidneys changes. In a newborn, the upper end of the kidney is projected at the level of the upper edge of the XII thoracic vertebra, and in infancy (up to 1 year) - already at the level of the middle of the body of the XII thoracic vertebra. The lower end of the kidney is at the level of the lower edge of the first lumbar vertebra, in a one-year-old child it is 1/2 vertebra higher, which is associated with the rapid growth of the spinal column. After 5-7 years, the position of the kidneys relative to the spine approaches that of an adult.
Over the age of 50, especially in old and malnourished people, the kidneys may be lower than at a younger age. At all periods of a person’s life, the right kidney is located slightly lower than the left.
13.3. Mechanisms of urine formation
During the day, a person consumes approximately 2.5 liters of water, including 1500 ml in liquid form and about 650 ml with solid food. In addition, about 400 ml of water is formed in the body during the breakdown of proteins, fats and carbohydrates. Water is excreted from the body mainly through the kidneys - 1.5 liters per day, as well as through the lungs, skin and partly with feces.
In the process of urine formation in the nephrons of the kidney, there are two phases. The first filtration phase is the formation of primary urine in the glomeruli of nephrons. In the second phase, reabsorption, reabsorption of water and other substances occurs in the nephron tubules, resulting in the formation of concentrated, so-called secondary urine.
In the renal glomeruli, water and substances dissolved in it are filtered through the wall of the capillaries and the inner layer of the capsule into the capsule cavity. Filtration is determined, on the one hand, by the amount of hydrostatic pressure that promotes the exit of liquid from the capillaries, and on the other hand, by the amount of oncotic pressure created by large molecular proteins dissolved in the plasma, which prevent the exit of liquid from the capillaries. Hydrostatic pressure outside the capillaries counteracts the filtration process. In the renal capillaries of the glomerulus, the hydrostatic pressure reaches 70 mm Hg. Art., the value of oncotic pressure is on average 30 mm Hg. Art., and the hydrostatic pressure of the filtrate in the capsule cavity is 20 mm. rt. Art. Thus, the effective filtration pressure is 70 – 30 – 20 = 20 mmHg. Art., which is enough to form 120 ml of filtrate, or primary urine, in 1 minute. The filtration membrane is formed by the endothelium of the capillaries, the porous basement membrane and the single-layer epithelium of the inner layer of the capsule. More than 1 liter of blood (1.2 liters) flows through the kidneys within 1 minute. During the day, up to 1700-1800 liters of blood passes through the kidneys. Thus, in 24 hours all the blood flows through the capillaries of the glomeruli more than 200 times. This blood comes into contact with the inner surface of the capillaries, the area of which in the glomeruli of the kidneys is 1.5-2 m2. In this case, the amount of primary urine produced reaches 150-180 liters per day. Thus, from 10 liters of blood flowing through the kidneys, 1 liter of primary urine is filtered, containing all the components of blood plasma, amino acids, glucose, vitamins and salts, as well as metabolic products - urea, uric acid and other substances, except high molecular weight proteins.
In the second phase of urine formation - reabsorption - from the cavity of the glomerular capsules, primary urine, similar in composition to the blood plasma, enters the nephron tubules, where reabsorption (reabsorption) of amino acids, glucose, vitamins, most of the water and salts occurs into the blood. As a result of tubular reabsorption during the day, up to 1.5 liters of secondary (final) urine are formed from 150-180 liters of primary urine. Secondary urine through the urinary tract (renal calyces, pelvis, ureter) enters the bladder and is excreted from the body. The tubules absorb 99% of the water contained in the primary urine, as well as the substances necessary for the body dissolved in it. About 85% of the volume of primary urine is reabsorbed in the proximal tubules (amino acids, glucose, low molecular weight proteins, fatty acids, sodium and potassium salts, etc.). Therefore, secondary urine differs sharply from primary urine. It does not contain sugar, amino acids, or many salts. At the same time, in secondary urine the concentration of sulfates, phosphates, urea, uric acid and other substances that are not absorbed into the blood is sharply increased. Thus, the concentration of urea in secondary urine is 67 times higher than in the blood, creatinine – 75 times, and sulfates – 90 times higher. The absorption of most substances in the nephron tubules is an active physiological process, which consumes the energy of the epithelial cover and other structures of the walls of the nephron tubules.
In the nephron tubules, along with reabsorption, a number of substances are also released into the urine. These are many medications, especially some antibiotics (penicillin), ammonium, some acids and other substances.
Urine is a light yellow liquid. It contains 95% water and 5% solids, including urea (2%), uric acid (0.05%), creatinine (0.075%), potassium and sodium salts. During the day, 25-30 g of urea and up to 25 g of inorganic substances are excreted from the body in the urine. In case of kidney disease, during short-term heavy physical exertion, protein may appear in the urine, which should not be in it. The reaction of urine depends on food. When eating predominantly meat foods, the urine has an acidic reaction, while when eating vegetables, it is alkaline or neutral. The appearance of blood in the urine (red, pink color) may be the result of damage to the mucous membrane, hemorrhages in the organs of the urinary system. Eating fresh carrots and beets can also cause urine to turn pink.
13.4. Regulation of urine formation
Regulation of urine formation is carried out by neurohumoral
way.
The highest subcortical center for the regulation of urine formation is the hypothalamus.
Impulses from the kidney receptors travel through the sympathetic nerves to the hypothalamus, where
antidiuretic hormone (ADH)
or
vasopressin is produced,
which enhances the reabsorption of water from primary urine and is the main component of humoral regulation.
Increased reabsorption of water when its intake into the body is insufficient leads to a decrease in diuresis; urine is characterized by a high concentration of substances contained in it. When there is excess water in the body, the osmotic pressure of the plasma drops. Through osmo- and ionoreceptors of the hypothalamus and kidneys, a reflex decrease in the production of ADH occurs and its entry into the blood. In this case, the body gets rid of excess water by excreting large amounts of low-concentration urine. The nervous regulation of urine formation is less pronounced than the humoral one,
and is carried out both by conditioned reflex and unconditioned reflex pathways. It mainly occurs due to reflex changes in the lumen of the renal vessels under the influence of various influences on the body. The kidneys have a high ability for self-regulation. Switching off the higher cortical and subcortical regulatory centers does not lead to the cessation of urine formation.
The kidneys are involved in maintaining a constant volume and composition of the internal environment. They ensure the release of excess water from the body in the form of hypotonic urine when the water content is increased or retain water and excrete urine that is hypertonic in relation to the blood plasma when the body is dehydrated.
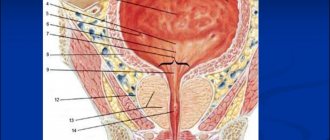
13.5. Anatomy, physiology and age-related features of the urinary tract (ureters, bladder, urethra)
Pelvis,
gradually narrowing, it passes into the ureter.
ureter
is a cylindrical tube with a diameter of 6-8 mm, a length of 25-35 cm, located retroperitoneally. The ureter has abdominal and pelvic parts. The wall of the ureter is formed by the mucous membrane, submucosa, muscular and adventitial membranes. The mucous membrane, thanks to the submucosa, forms numerous folds that can straighten out. The muscular layer of the ureter consists of two layers of smooth muscle cells.
The reservoir of urine is the bladder.
In an adult, it lies in the small pelvis behind the pubic symphysis.
Bubble capacity - up to 500 ml. The bladder has an apex, body
and
bottom.
The lower section of the bladder, tapering, passes into the urethra.
The wall of the bladder is formed by the mucous membrane, submucosa, muscular and adventitial membranes and is partially covered by the peritoneum. The mucous membrane, thanks to the submucosa, forms numerous folds, which straighten out when the bladder fills. The muscular lining of the bladder consists of three layers exchanging bundles - internal and external longitudinal and middle - circular. The interweaving of muscle bundles promotes uniform contraction of its walls during urination, pushing urine into the urethra.
It is a tube, the length of which depends on age and gender. The mucous membrane of the urinary tract is covered with stratified transitional epithelium, which, when the wall is stretched, becomes double-layered. The surface of the mucous membrane is covered with a cuticle, which protects the mucous membrane from the effects of urine.
The urine formed in the kidneys from the renal calyces, then the pelvis enters the ureters. Through the ureters, thanks to their peristaltic movements, urine is carried drop by drop into the bladder, where it accumulates until the bladder is filled. The external and internal sphincters of the urethra are contracted at this time, and the exit from the bladder is closed.
Emptying the bladder occurs reflexively. When urine accumulates in it in an amount of up to 250-300 ml, it begins to noticeably press on the walls of the bladder with a force of about 12-15 cm of water column, causing the urge to urinate. Nerve impulses generated in the receptors of the bladder walls are sent to the urination center located in the sacral part of the spinal cord. From this center, signals are sent along the fibers of the parasympathetic pelvic nerves to the walls of the bladder, which cause simultaneous contraction of the muscles of the bladder walls and the opening of the sphincters of the urethra. This expels urine from the bladder. The higher centers of urination are located in the frontal lobes of the cerebral hemispheres; they also regulate the process of urination.
A conditioned reflex delay in the urge to urinate for some time is developed in the process of raising a child. Newborns do not have voluntary urinary retention. The ability to regulate voluntary urination appears only towards the end of the child’s first year of life. In the second year, this ability becomes stable. The influence of the autonomic (autonomic) nervous system provides not only the excretion of urine from the body. Nerve impulses can increase or decrease the formation of urine, increase or decrease the excretion of substances contained in the blood in the urine.
A slowdown or cessation of urination can occur with severe painful stimulation. The formation and excretion of urine is affected by the amount of fluid you drink, the consumption of salty foods, and physical work.
In a newborn, the ureters have a tortuous course. The length of the ureter reaches 5-7 cm. By the age of four, its length increases to 15 cm. The muscular layer in early childhood is poorly developed.
The bladder in newborns is fusiform, in children of the first years of life it is pear-shaped. During the period of second childhood (8-12 years), the bladder is ovoid, and in adolescents it has a shape characteristic of an adult. The capacity of the bladder in newborns is 50-80 ml. By the age of five it can hold 180 ml of urine, and after 12 years - 250 ml. In a newborn, the circular muscle layer in the wall of the bladder is poorly expressed, the mucous membrane is well developed.
The apex of the bladder in a newborn reaches half the distance between the navel and the pubic symphysis. At the age of 1-3 years, the bottom of the bladder is located at the level of the upper edge of the pubic symphysis. In adolescents, the bottom of the bladder is at the level of the middle, and in adolescence - at the level of the lower edge of the pubic symphysis. Subsequently, the bottom of the bladder lowers depending on the condition of the muscles of the urogenital diaphragm.
Chapter 14. AGE ANATOMY AND PHYSIOLOGY OF SKIN
Physiology
When studying the kidneys, the anatomy and physiology of which are discussed in this article, it is necessary to understand the process of urine formation, since it is the main renal function. Thanks to the formation of urine, it is possible to maintain homeostasis - the so-called constancy of the environment inside the human body. The process of urine formation occurs at the level of nephrons and efferent tubules. Urine formation itself can be divided into several stages:
- blood plasma filtration;
- reverse absorption or so-called reabsorption;
- secretion of urine.
Let's look at each stage in more detail:
- The process of urine formation begins with the vascular glomerulus. Due to the presence of a certain pressure in the renal glomerulus, mineral salts, glucose, water and other substances are filtered into the capsular cavity through the thinnest capillary walls. The resulting filtrate is called primary urine. During the day, about 180-200 liters of such primary urine are produced.
- Next, from the organ capsule, primary urine enters the tubular system. Here, the reabsorption of a significant part of the water, as well as substances and compounds useful and important for the body, occurs. Liquid absorption is quite abundant - up to 60-80 percent. But protein and glucose are completely reabsorbed, up to 80 percent of sodium, about 95 percent of potassium, urea (about 60%), as well as a significant amount of phosphates, chlorine ions, amino acids and other substances beneficial to the body are also absorbed. In this case, creatinine is not completely reabsorbed. As a result of the reabsorption process, the volume of urine is reduced to 1.7 liters. This urine is called secondary urine.
- The last stage of urine formation is secretion. At this stage, metabolic products are transported from the blood to urine. The secretion process occurs in the upper part of the tubules and partially in the area of the collecting ducts. As a result of tubular secretion, toxins and foreign substances are removed from our body, for example, paints, penicillin and other compounds, as well as compounds and substances that are formed in the tubular epithelial layer (for example, ammonia). The secretion process also captures potassium and hydrogen ions.
Important: due to the ongoing processes of filtration, reabsorption and secretion, the kidneys can perform a detoxification function. The organ is an active participant in the process of maintaining water and electrolyte balance, as well as acid and alkaline balance.
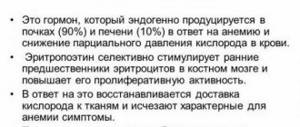
The kidneys are involved in the process of maintaining the necessary vascular tone, which is important for the regulation of blood pressure, as well as the concentration of hemoglobin in red blood cells. All this is possible due to the fact that the kidney can produce renin, erythropoietin and prostaglandins in the medulla.
Basic kidney functions
The main functions of the kidneys include:
- urinary function, which consists in the fact that the kidneys excrete metabolic products and all foreign compounds from the human body, as well as those substances that are presented to him in excess. The end products of human metabolism are urea, uric acid, ammonia, etc.;
- homeostatic function - the kidneys are responsible for maintaining the homeostasis of the human body, as they allow regulating the composition and volume of fluid, acid-base balance;
- endocrine function - the kidneys synthesize hormones that enter the systemic circulation (vasoconstrictors and vasodilators).
The urinary and homeostatic functions of the kidneys are carried out as a result of the implementation of four associated processes that have a certain sequence. These processes include: glomerular filtration, tubular reabsorption, tubular secretion and intrarenal metabolism.
Finished works on a similar topic
- Course work: Physiology of the kidneys 460 RUR.
- Abstract Physiology of the kidneys 240 rub.
- Test work: Physiology of the kidneys 230 rub.
Receive completed work or specialist advice on your educational project Find out the cost
Regulation of urine formation
Regulation of the process of urine formation is carried out through humoral and nervous pathways. Regulation of urine formation due to the nervous system occurs as a result of changes in the tone of the afferent and efferent arterioles. As a result of stimulation of the nervous system (sympathetic), the tone of smooth vascular muscles increases. As a result, the pressure increases and glomerular filtration accelerates. When the parasympathetic nervous system is excited, the opposite process occurs.
Humoral regulation of the process of urine formation is carried out due to hormones produced by the pituitary gland and hypothalamus. Thanks to thyroid-stimulating and somatotropic hormones, the amount of urine produced increases significantly. And under the influence of antidiuretic hormone produced by the hypothalamus, the amount of urine excreted decreases due to an increase in the intensity of the reabsorption process in the renal tubules.