Warehouse relocation to Europe. We sell hepatitis C drugs in Russia at the purchase price - warehouse liquidation Go to website
Renal artery stenosis (RAS) is a serious disease accompanied by narrowing of the lumen of the vessel supplying the kidney. The pathology is the responsibility of not only nephrologists, but also cardiologists, since the main manifestation is usually severe hypertension, which is difficult to correct.
Patients with renal artery stenosis are predominantly older people (after 50 years), but stenosis can also be diagnosed in young people. Among older people with vascular atherosclerosis, there are twice as many men as women, and with congenital vascular pathology, females predominate, in whom the disease manifests itself after 30-40 years.
Every tenth person suffering from high blood pressure has stenosis of the main renal vessels as the main cause of this condition. Today, more than 20 different changes are already known and described, leading to narrowing of the renal arteries (RA), an increase in pressure and secondary sclerotic processes in the parenchyma of the organ.
The prevalence of pathology requires the use of not only modern and accurate diagnostic methods, but also timely and effective treatment. It is recognized that the best results can be achieved with surgical treatment of stenosis , while conservative therapy plays a supporting role.
Role of the kidneys
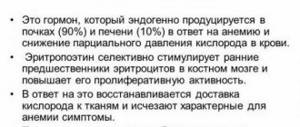
Regulation of the level of Na and K ions in the body. Maintaining and regulating the pH level in the blood (acid-base balance). Regulating the volume of circulating blood (due to the absorption of excess fluid and its removal; removal of excess amounts of microelements that retain fluid). Endocrine function. The kidneys produce biologically active substances that affect the formation of red blood cells. Regulation of the blood coagulation system. The function is ensured by the action of biologically active substances produced by the kidneys. Participation in metabolic processes (protein, carbohydrate, lipid). Excretory function. Removal from the body: breakdown products of substances during the digestion of food and as a result of metabolic processes; excess volumes of water; medicinal and harmful substances. Maintaining blood pressure levels. Protecting the body from harmful substances.
The mass of the kidneys is about 0.4% of the total mass of the human body. However, at the same time, they allow about 20% of the blood through themselves, which leaves the heart cavity into the bloodstream through the aorta.
The kidneys have a system for regulating blood flow, and this system is not affected by changes in systemic blood pressure.
Kidney resection: main methods
When treating this organ, doctors resort to open or laparoscopic surgery. In the first case, excision of part of the kidney occurs through an incision in the lumbar region. But laparoscopic partial nephrectomy is more often performed. Reviews about this method of treatment are usually positive. This operation allows you to avoid huge wounds on the patient’s body. During this procedure, a small incision is made into which microsurgical instruments and a television camera are inserted using a special flexible tube (catheter).
The choice of type of operation depends on the availability of appropriate equipment in the hospital and the qualifications of the surgeons. Of course, most doctors prefer laparoscopy, because after it the patient recovers faster.
Features of blood circulation
The blood supply to the kidneys is the most abundant. No other organ has such volumes of blood flow. Nutrition of the kidneys occurs through the renal arteries, which originate from the abdominal aorta.
Blood supply to the kidneys
The renal arteries are short. When they enter the kidney, they immediately divide into smaller vessels called arterioles (located in the interpyramidal space).
The arcuate artery passes between the cortex and medulla of the kidney. From it, to supply the cortex, arteries branch off and pass through the interlobular space.
The intralobular arteries originate from the interlobular arteries, then they branch into the afferent arterioles of the glomerulus.
From the proximal part, the afferent glomerular arterioles go to the interstitial and intermediate nephrons, to their renal corpuscles. From the distal sections, the arterioles go to the juxtamedullary nephrons.
There are two types of blood circulation in the kidney. One is called cortical, the second is called juxtaglomerular.
Cortical is the blood circulation in the area of the Malpighian tubules.
The Malpighian glomerulus consists of many loops of capillaries. They have higher pressure than other capillary networks. It is about 80 mm. rt. Art.
The uniqueness of blood circulation here is that both the inflow and outflow vessels are called arterioles. No other human organ has such a feature.
The main process of plasma filtration and urine formation occurs in the Malpighian glomeruli. The afferent arteriole is wide and short, and the efferent arteriole is much narrower.
Kidney arteries
The efferent vessel forms a second network of renal capillaries by branching. Another network of capillaries is located around the convoluted proximal and distal renal tubules. In this network the pressure is about 10–15 mm. rt. Art.
The juxtamedullary circulation is located in the zone of large glomeruli at the border of the cortex and medulla. At the site of nutrition of the juxtamedullary glomeruli, the afferent and efferent arterioles are approximately the same size.
The pressure in the juxtamedullary capillaries is no more than 40 mm. rt. Art. The blood flow slows down here, the blood is slowly filtered, and a small amount of urine is formed.
The efferent arteriole does not branch and does not form a peritubular network. It descends through parallel straight arteries into the medulla - this is how it is nourished.
In the medulla, the arteriole breaks up into capillaries, which then flow into venules, and then into venous vessels. Small venous vessels connect to form the renal veins, and the renal veins join the inferior vena cava system.
About 80% of all incoming blood is filtered in the Malpighian glomeruli, and about 20% passes through the juxtamedullary glomeruli.
To maintain optimal conditions for urine formation, the kidneys carry out self-regulation. If blood pressure in the afferent vessel increases, muscle fibers contract and the amount of incoming blood decreases. Consequently, the pressure also decreases.
Stress
If there is a decrease in blood pressure, then the afferent vessel, on the contrary, expands and blood flow increases.
The pressure in the glomeruli is maintained at a constant level; only in situations of stress (emotional stress, shock of various etiologies) can blood flow decrease.
The entire volume of blood passes through the filtration system in five minutes. Due to this, the maximum amount of excess, unnecessary substances is removed from the body.
To assess blood flow speed, the following examinations are performed:
radioisotope renography; computed angiography; nuclear magnetic resonance; duplex ultrasonography.
The kidneys perform a number of important functions to maintain normal functioning of the body. Therefore, blood circulation is very complex.
If the blood supply to the kidneys is disrupted, then not only their functionality suffers, but also the functions of many systems.
The kidneys are the main organ of excretion. The blood supply to the kidneys plays a special role in the functioning of the entire body and has a characteristic vascular network. The circulatory system in the body is necessary not only to supply nutrients, but also to ensure the process of urination. It is impossible to correctly assess the structure and function of the kidneys without understanding the characteristics of its blood supply.
Manifestations of SPA
For a long time, SPA can exist asymptomatically or in the form of benign hypertension. Vivid clinical signs of the disease appear when the narrowing of the vessel reaches 70%. Among the symptoms, the most typical are secondary renal arterial hypertension and signs of parenchymal dysfunction (decreased urine filtration, intoxication with metabolic products).
A persistent increase in pressure, usually without hypertensive crises, in young patients prompts the doctor to think about possible fibromuscular dysplasia, and if the patient has crossed the 50-year mark, most likely atherosclerotic damage to the renal vessels.
Renal hypertension is characterized by an increase in not only systolic but also diastolic pressure, which can reach 140 mmHg. Art. and more. This condition is extremely difficult to treat with standard antihypertensive drugs and creates a high risk of cardiovascular disasters, including stroke and myocardial infarction.
Among the complaints of patients with renal hypertension are:
Severe headaches, tinnitus, flashing “spots” before the eyes; Decreased memory and mental performance; Weakness; Dizziness; Insomnia or daytime sleepiness; Irritability, emotional instability.
A constant high load on the heart creates conditions for its hypertrophy; patients complain of chest pain, palpitations, a feeling of interruptions in the functioning of the organ, shortness of breath appears, and in severe cases, pulmonary edema develops, requiring emergency care.
In addition to hypertension, heaviness and pain in the lumbar region, blood in the urine, and weakness are possible. In case of excess secretion of aldosterone by the adrenal glands, the patient drinks a lot, excretes a large amount of unconcentrated urine not only during the day, but also at night, and convulsions are possible.
At the initial stage of the disease, kidney function is preserved, but hypertension already appears, which, however, can be treated with medications. Subcompensation is characterized by a gradual decrease in kidney function, and in the stage of decompensation, signs of renal failure are clearly visible. Hypertension in the terminal stage becomes malignant, the pressure reaches maximum values and is not “knocked down” by medications.
SPA is dangerous not only for its manifestations, but also for complications in the form of cerebral hemorrhages, myocardial infarction, pulmonary edema due to hypertension. In most patients, the retina of the eyes is affected, and its detachment and blindness are possible.
Chronic renal failure, as the final stage of pathology, is accompanied by intoxication with metabolic products, weakness, nausea, headache, a small amount of urine that the kidneys can filter on their own, and an increase in edema. Patients are susceptible to pneumonia, pericarditis, inflammation of the peritoneum, damage to the mucous membranes of the upper respiratory tract and digestive tract.
General concepts and features of human blood supply
The kidney is an organ in which toxic substances are formed that require removal from the body. The kidneys occupy the main place in regulating the water-salt balance. That is why they require a fairly enhanced blood supply. Short renal arteries diverge from the aorta to the kidneys, and at the renal hilum they are divided into interlobar ones. In the kidney itself, the interlobar arteries are divided into large arcuate vessels that supply blood to the medulla and cortex of the organ.
The large circle of blood circulation of the kidney, the cortical circle, consists of blood vessels that feed the cortex. Branching out, they pass into small interlobular arteries, which in turn end in glomerular arterioles. Branching into capillaries forms vascular glomeruli, concentrated near the cortical nephrons, and passes into the efferent arterioles. The circumference of the efferent arterioles is smaller than that of the afferent arterioles, due to which high pressure is created in the vascular glomeruli. As a result of this process, compounds from the plasma pass into the renal channels. This is how phase 1 of urine formation occurs.
The blood circulation of the second, small circle is formed by the efferent vessels. The efferent arterioles do not diverge, forming networks. To nourish the medulla, they descend into it through straight, parallel vessels. In the medulla, they are divided into capillaries that entwine the nephrons to form venous capillary networks. The pulmonary circulation (justcamedullary) is located on the line of connection between the medulla and the cortex. The afferent and efferent capillary vessels at the site of supply to the juxtamedullary nephrons do not differ in circumference. Low pressure is created inside them, blood flow slows down, which promotes the absorption of fluid and substances found in the tubules back into the blood. This is how phase 2 of urine formation occurs.
Return to contents
How long is the postoperative period after partial nephrectomy?
The postoperative period depends on the type of resection used and the presence or absence of complications. In the absence of complications, with laparoscopy it lasts 5-7 days, with general surgery (abdominal) - 12 days. With complications, everything is very individual and depends on their complexity and the body’s resistance. And also the period during oncological operations may be different and individual. It all depends on how the tumor was removed. Sometimes, for example, to approach an organ, excision of a rib is required. In this case, rehabilitation may be longer – up to 30 days.
Regulating blood supply to the kidneys
The renal blood supply is characterized by a high level of self-regulation of blood flow, which is responsible for its stability, the process of formation of primary urine in a wide range of blood pressure. A signal from the sympathetic vasoconstrictor nerves is sufficient for the afferent or efferent arterioles to change their diameter. The walls of the blood supply tubes consist of muscle fibers, which, by contracting or relaxing, change the lumen of the arterioles. The blood supply to the kidneys decreases, which leads to a short-term decrease in the amount of urine excreted or the absence of its entry into the bladder in any stressful situation for the human body: pain, physical activity, and others. At this moment, resistance increases in the renal arterioles, blood pressure rises and filtration occurs.
The blood supply in the kidneys is characterized by a high level of self-regulation of blood flow.
When blood circulation is weakened, for a short time the kidneys can independently replenish the missing pressure and support the function of urine formation. But the lack of long-term assistance will lead to depletion of their capabilities and will result in disruption of the blood circulation, filtration process and pathological complications.
Return to contents
Possible complications of kidney segment resection
Considering the complexity of the operation, which is performed to preserve the functionality of the organ, there are frequent cases of complications, including severe ones. If a significant amount of discharge appears in the drainage tube, obstruction of the urinary canal and fistulas may be suspected. Fistulas form quite rarely, and more often during wedge-shaped resection with suturing of the damage with mattress sutures. A phenomenon such as urinoma can occur after kidney resection is performed due to insufficient drainage of the kidney.
A common complication is the development of wound infection. Rare complications that develop as a result of the removal of a significant amount of tissue include the formation of blood clots in the kidney artery. Such a complication is usually a consequence of damage to the intima. In approximately 3% of cases, after removal of a kidney segment, it becomes necessary to completely remove the remaining organ tissue, since this part becomes completely non-functional and non-viable.
Renal vascular disorders and diseases
Complications of renal blood flow are divided into congenital and acquired. Congenital pathologies are affected by improper development of internal organs during the period of intrauterine development of the fetus. Genetic predisposition, poor lifestyle of the mother, poor environmental environment can provoke the appearance of an additional renal artery or a large number of arterioles, the formation of stenosis, and aneurysm.
Return to contents
Consequences of congenital anomalies
A pathologically formed capillary system is dangerous due to changes in blood circulation, causing complications of kidney function and bladder pressure. Improperly developed arteries connect to the ureter and can lead to a situation where they compress it. Impaired outflow from the kidney leads to a gradual enlargement of the organ due to the accumulation of urine.
A poor environmental environment can provoke congenital anomalies.
The growing pelvis compresses the body of the kidney on one side, and on the other, the connecting capsule puts pressure on it. Compression leads to the destruction of nephrons, which provokes kidney failure. This condition leads to a progressive expansion of the pelvis and calyces of the organ and can lead to its atrophy.
The development of complications described above is not the only one that occurs with a congenital anomaly of the organ and arterioles. The microcirculation of the organ is disrupted, the likelihood of developing urolithiasis, the inflammatory process of the urinary organs increases, disrupting the normal functioning of the kidneys and immediate medical intervention is required.
Return to contents
Renal artery stenosis
Stenosis is a narrowing of the lumen of blood vessels. In a healthy state, blood passing through the kidneys is filtered to form primary urine. With stenosis, much less blood flows to the kidney, increasing pressure but worsening filtration. This pathology disrupts the functioning of the organ, which over time may lose the ability to form and excrete urine.
Atherosclerosis, diabetes mellitus, aneurysm, inflammatory processes, arterial neoplasms are possible causes of the development of stenosis. Regardless of the reason that provoked the stenosis, it negatively affects not only the functioning of the kidneys, but also the entire body as a whole. The main consequences of stenosis:
hormonal imbalance; protein loss; fluid separation disorder; change in the volume of general plasma circulation. Return to contents
Preparation and performance of resection
Despite the fact that kidney resection is much easier to tolerate for most patients than organ removal, in terms of the operation, such an intervention is still a rather complex undertaking. Preparing patients for surgery is standard. First of all, the patient is examined by an anesthesiologist, since the entire procedure to remove a segment of the kidney is carried out under general anesthesia. In addition, before kidney resection is prescribed, a number of tests and studies may be required to assess the condition of the kidney and identify other existing serious pathologies and diseases. Such studies include:
- Ultrasound.
- CT scan.
- MRI.
- Renal perfusion.
- Renal angiography.
- Tests for syphilis, HIV, hepatitis.
During the operation, the patient is placed on his side to give the surgeon greater access. Next, the body is fixed using devices available on the surgical table. After administering anesthesia, a 10 to 12 mm incision is made, through which the surgeon gains access to the organ. Next, the pedicle and blood vessels leading to the kidney are clamped to reduce the risk of extensive bleeding. Next, the entire damaged area is removed. Lastly, a drainage tube is installed to control the discharge during the postoperative period.
Diagnosis of disorders
High blood pressure is a possible symptom of the disease.
Based on many years of experience, doctors have learned to identify functional disorders by characteristic but subtle symptoms:
high blood pressure; increased number of red blood cells; decreased daily urine volume.
Signs cannot 100% diagnose the disease; they only give rise to speculation. Therefore, optical methods have been developed to detect and confirm kidney pathologies:
Ultrasound. To examine the kidneys, a regular ultrasound is sufficient; to examine the arterioles and capillaries, you will need a special Doppler ultrasound device. The scanner allows you not only to see a picture of what is happening, but also to estimate the speed of movement of the liquid. Arterial stenosis, identification of accessory arteries are diagnoses with which he copes well. The Doppler device has a disadvantage - it will not be able to detect fluid with a low rate of movement, which is typical for acute stenoses. Examination using contrast agents is a group of diagnostic methods. The use of iodine-based products allows the use of conventional radiography, fluoroscopy or MRI to detect arterial stenosis and other disorders. The use of drugs containing gallium when MRI is performed makes it possible to determine the structure of the organ. Today, these methods are the most accurate and progressive in diagnosing kidney diseases. Return to contents
How to detect renal artery stenosis?
Examination of a patient with suspected stenosis of the left or right renal artery begins with a detailed clarification of complaints, the time of their onset, and the response to conservative treatment of hypertension, if it has already been prescribed. Next, the doctor will listen to the heart and large vessels, prescribe blood and urine tests and additional instrumental examinations.
stenosis of both renal arteries on angiography
During the initial examination, it is already possible to detect an enlargement of the heart due to hypertrophy of the left parts, and an increase in the second sound above the aorta. A murmur is heard in the upper abdomen, indicating narrowing of the renal arteries.
The main biochemical indicators in SPA will be the level of creatinine and urea, which increase due to insufficient filtration capacity of the kidneys. Red blood cells, white blood cells, and protein casts can be found in the urine.
Of the additional diagnostic methods, ultrasound is used (the kidneys are reduced in size), and Doppler measurements make it possible to record the narrowing of the artery and changes in the speed of blood movement through it. Information about the size, location, and functionality can be obtained through radioisotope research.
Arteriography is recognized as the most informative diagnostic method, when the location, degree of VA stenosis and hemodynamic impairment are determined using contrast radiography. CT and MRI may also be performed.
How to improve kidney hemodynamics?
Not drinking enough water has a negative impact on kidney function.
As a result of complications of kidney function, toxins accumulate in the body, which is the basis for deterioration in well-being. Poor nutrition, insufficient drinking, and medications negatively affect kidney function. The use of medications and herbal medicine improves blood circulation and restores organ functions.
Before using a drug that improves blood flow, it is necessary to find out the cause of the underlying disease, and at the same time restore the blood supply to the organ. If you are required to consult a doctor, a treatment regimen is drawn up:
vascular medications (“Rovatinex”, “Trental”); antioxidants and membrane stabilizers (B vitamins, vitamin D, “Mexidol”, “Berlition”, “Cytoflavin”); special dietary nutrition; cleansing procedures for the intestines.
Folk remedies will help improve kidney function:
Lingonberry decoction. 2 tbsp. l. lingonberry leaves for 2 tbsp. water, cook for 15 minutes, take 100 ml of decoction 4 times a day before meals. Licorice herb. 2 tbsp. l. pour 300 ml of boiling water, let it brew and take throughout the day. Celery, parsley. It is useful to drink juice, add to salads. Ginger. Tea with ginger throughout the day.
Herbal therapy should continue for at least a year. A course of 1 to 3 weeks is allotted for taking one drug, then it needs to be changed. After 2 -2.5 months a break is taken. To control the situation, it is necessary to do a urine test and be sure to consult a doctor on the amount of daily fluid intake.
Do you know enough about the peculiarities of blood circulation in the kidneys? Kidneys are one of the most important organs, so the quality of work of the entire body as a single system directly depends on blood circulation. Their main task is to regulate the following processes:
metabolism of fats, carbohydrates and proteins; removal or accumulation of important substances, such as sugar, amino acids, salts, etc.; breakdown and excretion of biologically active substances; removal of nitrogen metabolism products; maintaining water-salt balance.
Rehabilitation after kidney resection
After surgery, a long recovery period is required, which can last about a year. Quite often, patients complain of pain after kidney resection, which can only be eliminated by administering painkillers. To prevent the development of negative consequences after surgery, you should follow some recommendations:
- Drink plenty of water.
- Be examined after resection every three months.
- Avoid physical activity, as in the first days after discharge the patient feels a loss of strength and extreme fatigue. It is necessary to rest as much as possible.
- Avoid stressful situations and nervous tension.
- Consult your doctor about your dietary habits. After all, each individual case has its own recommendations; everything will depend on the severity of the disease, age and complexity of the operation.
- After removing part of the kidney, communication with sick people and hypothermia should be avoided, since the body is not protected from infections during this period.
- After surgery, a person must monitor the condition of the sutures.
Features of kidney blood circulation
Since a huge amount of substances that require excretion are formed in the kidneys, and they play a large role in the regulation of water-salt metabolism, they require the most enhanced blood circulation. Blood flows to the kidneys through the renal arteries branched from the aorta, which are divided into interlobar ones at the hilum of the kidney. They are divided into arcuate arteries - fairly large vessels that approach the medulla and cortex of the organ. The vessels feeding the cortex (about 80–90% of the total) make up the so-called cortical, or systemic, circulation of the kidney. They, in turn, are divided into smaller interlobular arteries, from which one afferent arteriole departs to each glomerulus. They branch into capillaries that form the so-called vascular glomeruli around the renal corpuscles of the nephrons and then collect into the efferent glomerular arterioles.
Kidney circulation diagram
Due to the fact that the diameter of the efferent vessels is almost half that of the afferent vessels, extremely high pressure is created in the small glomerular capillaries. As a result of this, compounds from the blood plasma pass into the kidney tubules, that is, the 1st phase of urine formation occurs.
The efferent arterioles are also divided into capillaries, called secondary, which intertwine the tubules of each nephron and thereby form a peritubular capillary network. Since the diameter of the lumens of the vessels is not much different, a relatively low pressure is created in the secondary capillaries, due to which the liquid from the tubules and the substances contained in it are absorbed back into the blood and thus the 2nd phase of urine formation occurs.
Recovery after kidney resection
Rehabilitation of the patient, after removal of part of the organ, begins in the intensive care unit. A day later, if all is well, the patient is transferred to the general ward. Further recovery includes the following components:
- from taking painkillers and anti-infective drugs;
- daily dressing;
- on the second day after surgery, you can start moving and pacing to prevent adhesions, stagnation of blood and fluid in the wound cavity;
- food is allowed on the second day after resection;
- the catheter is removed on day 3;
- drainage, depending on the patient’s condition, is removed on days 3-5;
- sutures are removed after 12 days. If you used kergut threads, this is not necessary - they dissolve on their own;
- For 90 days you need to avoid physical activity, hypothermia, and wear a bandage.
With laparoscopic resection, recovery is much faster:
- drainage is not installed, since blood loss is minimal;
- the catheter is not installed;
- bandaging, as such, is not required. Small seams are disinfected and the patch is changed;
- Self-absorbing sutures are used during laparoscopy;
- no bandage needed.
Such a patient can be discharged after 5 days.
Kidney tuberculosis symptoms and treatment
Infectious lesions of the parenchyma caused by mycobacteria are called kidney tuberculosis. The incubation period lasts 2-3 years, the mycobacterium enters a healthy organ along with the blood or lymphogenous route.
Mycobacterium tuberculosis is Koch's bacillus, or MBT. The main route of infection is airborne droplets from a sick person.
Tuberculosis is contagious regardless of whether it has spread to the lungs or whether there is a form of kidney damage. Women and men develop the disease with the same frequency. Children get sick less often. Quite often the disease also affects the genitals.
How the disease develops
The disease is formed under the influence of both external and internal factors. If a person comes into contact with an infected person, they may become ill. But when immunity is high, it is able to suppress the development of the disease. Pulmonary tuberculosis reaches the kidneys through the bloodstream. The decisive role is played by the features of blood circulation that contribute to the appearance of primary foci of infection:
- There are a large number of arteries inside the organ.
- The vessels are closely adjacent to the interstitial tissue.
- Blood flows slower inside the glomeruli.
At the beginning of the development of the disease, the cortical layer is affected. As the pathology progresses, tissue breakdown occurs. The parenchyma is damaged and cavities are formed. In advanced cases, purulent melting of the tissues of the diseased organ begins, and neighboring organs become inflamed.
6 main symptoms
Signs of the disease are divided into two groups - direct and indirect. Indirect signs are listed below. If the following manifestations are observed in combination, it is necessary to undergo examination at a medical institution:
- General weakness, loss of strength.
- Chronic fatigue syndrome.
- Body temperature is higher than normal.
- Nausea.
- Low blood pressure.
- Indigestion, diarrhea or constipation.
Kidney tuberculosis can be determined by a number of direct signs:
- Frequent urge to urinate at night indicates the presence of neoplasms in the parenchyma, which can put pressure on the bladder.
- Anomalies of carbohydrate metabolism - carbohydrates are used as the main source of energy, as there is a deficiency of proteins.
- Bloody particles in the urine.
- Colic, lower back pain.
- Sick skin color.
- Sudden weight loss.
Stages of disease development
There are only four stages of the disease:
- The first, or latent stage - the tissues are not damaged, symptoms practically do not appear.
- The second, or initial destruction, is when the processes of inflammation and tissue death of the renal papillae begin, and a pathological cavity is formed - a cavity. Signs of intoxication appear.
- The third, or cavernous, is a large cavity or several cavities in one of the renal segments. The quality of life noticeably decreases, the disease progresses.
The fourth, or stage of polycavernous tuberculosis - the cavities of several or all segments of the kidneys are affected. The most dangerous stage. The diseased organ is completely destroyed - it turns into a large bubble with a thin wall of surviving tissue or becomes dotted with cavities with thin bridges. One of the most dangerous complications can be kidney failure.
Diagnostics
To avoid complications, it is important to undergo regular examination at a medical facility. At the initial stage of whitening it will not be difficult to overcome. First of all, the patient must know which doctor to see. A phthisiatrician specializes in the treatment and diagnosis of tuberculosis. The specialist will interview the patient to identify one or another type of infection. Next, an examination is carried out, after which tests and laboratory tests are prescribed:
- General urine test - sediment is checked for the presence of mycobacteria.
- Blood test - shows an increase in leukocytes and a decrease in hemoglobin levels, indicating inflammatory processes.
- X-ray examination – several procedures are necessary. In this way, it is possible to identify tuberculosis lesions that remain motionless, unlike stones.
- Cystoscopy is an examination of the inner wall of the bladder using a cystoscope. Tuberculous tubercles and ulcers are detected. The procedure is considered quite painful.
- Bacteriological analysis is carried out to identify MBT.
- Ultrasound is a painless way to identify areas that are saturated with lime or have undergone fibrosis.
Doctors do not recommend that women plan a pregnancy until they are cured. If the disease is diagnosed in a pregnant woman, the question of terminating the pregnancy may be raised.
Causes of the disease
Infection usually occurs if the patient's lungs are already affected. In this case, the immune system is weakened. But there are situations when kidney tuberculosis begins in a healthy person on the very first day after communicating with a patient. Factors contributing to the development of the disease are listed:
- Improper lifestyle - smoking, excess alcohol, unbalanced diet, lack of physical activity.
- Living in areas with unfavorable environmental conditions, working in hazardous industries.
- Hypothermia.
- Injuries to the organs of the urinary system and those located nearby.
- Insufficient production of lymphocytes that form the immune defense.
- Urological problems, genital infections.
- Malfunctions of the endocrine system.
Classification of the disease
In addition to the fact that the disease can manifest itself in four stages, there are also two forms of this disease. When the disease occurs in an acute form, it is called miliary. It has no obvious manifestations. But the destruction of the kidney tissue does not occur, and the disease does not spread to other organs formed by the parenchyma. A distinctive feature is uniform rashes in the urinary area.
Our readers successfully use Renon Duo to treat kidneys. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
The second form - caseous, or chronic, is considered more dangerous. The disease develops gradually, ulcerative decay is observed, and the disease affects neighboring organs. The process of tissue necrosis gradually begins.
- Papillitis - pathologies of the renal papillae are detected. The tissues of the organ are destroyed, and blood appears in the urine. The manifestations resemble a common cold.
- Fibrous-cavernous - one of the kidneys begins to shrink as a result of an increase in the number of connective tissue cells.
- Defoliation is extremely rare. The affected areas are soaked in calcium salts. Subsequently, round formations are identified - tuberculomas.
The disease can only be cured in a hospital setting, so the patient must be hospitalized in a timely manner. The doctor chooses one of two ways - medication or combination therapy - surgery and prescription of drugs. Herbal remedies can be used at the same time, but they do not replace traditional treatment. Taking medications without permission is ineffective and can lead to a deterioration in your general condition.
Medicines should be taken under the supervision of a doctor. If treatment is started, pathogenic organisms will become resistant to pills and injections. The following drugs will help defeat kidney tuberculosis:
- Streptomycin is a first-generation aminoglycoside or a more modern analogue, gentamicin.
- Rifampicin has a wide spectrum of activity, but rapid development of resistance has been noted.
- Thioacetazone is rarely used due to its high toxicity.
If traditional treatment does not produce results, they proceed to surgical intervention. The diseased organ may be partially or completely removed. The most gentle method is to remove the affected area - the cavity. In this case, the organ is left.
Prevention and prognosis
The medical prognosis is favorable if the disease is diagnosed at the very beginning of its development. Then you can save the organ and return to normal life. But in any case, it is easier to insure against illness than to undergo long-term treatment in a hospital. In severe stages, in the fibrous-cavernous form, tissue necrosis is observed. The prognosis is usually unfavorable.
In order to prevent illness, walking in the fresh air and exercising in the morning are beneficial. It is important to give up bad habits - smoking and alcohol. Introducing plenty of fruits and vegetables into the diet, as well as hardening, will help improve immunity. You should also limit, or better yet stop, communication with patients with tuberculosis of any form. In winter, it is important to wear warm clothes and not get too cold.
What are the complications after kidney removal?
Any surgical intervention into the human body and removal of an organ can have complications and serious consequences. After kidney removal, the following are possible:
- negative consequences from improper anesthesia - heart complications, coma and even death;
- damage to organs adjacent to the kidney that will need to be corrected - sutured or dried out;
- increased hemorrhage as a result of damage to blood vessels;
- internal bleeding;
- postoperative infection and wound suppuration;
- stomach ulcer;
- intestinal obstruction;
- hernias and adhesions;
Recurrence in a second organ is a popular complication.
rus-urologiya.ru
Therapy methods
Treatment is aimed at treating the underlying renal pathology and relieving symptoms. The only way to reduce renal pressure is with medications:
- Diuretics.
- ACE inhibitors.
- Beta blockers and calcium channel blockers.
Usually in a system and on a long-term basis. The patient becomes a kind of hostage to the pills until etiological treatment is carried out (elimination of the underlying disease).
It is important to restore normal hemodynamics, water balance in the body, remove excess fluid, normalize cardiac activity, and the nature of glomerular filtration.
Among the ways to radically eliminate renal manifestations, conservative and surgical techniques can be distinguished. The selection of a specific regimen is made by the doctor.
The list of drugs is wide: non-steroidal anti-inflammatory drugs, glucocorticoids in different dosages, antibacterial agents and antiseptics for internal use, etc.
- Pyelonephritis is treated with anti-inflammatory drugs and antibiotics.
- For glomerulonephritis, immunosuppressants are used, but with caution.
- Nephritis is eliminated in the same way as pyelonephritis, but surgical intervention is possible.
Surgical treatment is indicated in a strictly limited number of cases, if there is no other option.
Similar chapters from other books
BLOOD SUPPLY AND INNERVATION OF THE KIDNEY
3. BLOOD SUPPLY AND INNERVATION OF THE KIDNEY The renal artery, entering the portal of the kidney, being a branch of the abdominal aorta, is divided there into two branches: anterior and posterior. Sometimes there are additional branches. The blood flow in the kidneys is very intense: up to 1.5 tons of blood passes through the kidneys per day.
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE URETERS
4. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE URETER The ureter (ureter) emerges from the hilum of the kidney and flows into the bladder. The purpose of the ureter is to remove urine from the kidney to the bladder. The average length of the ureter is 30 cm, the diameter is about 8 mm, and
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE BLADDER
5. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE BLADDER The bladder (vesica urinaria) is an unpaired organ in which urine accumulates and is subsequently excreted. The capacity of the bladder is from 300 to 500 ml. The following are distinguished in the bladder:
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE VAGINA
1. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE VAGINA The vagina (vagina) is an unpaired tube-shaped organ, which is located in the pelvic cavity from the genital slit to the uterus. The vagina is up to 10 cm long, the wall thickness is from 2 to 3 mm. From below, the vagina passes through
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE UTERUS
2. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE UTERUS The uterus (uterus) is a hollow, unpaired muscular organ, pear-shaped, in which the development and gestation of the fetus occurs. The uterus is located in the pelvic cavity, located in front of the rectum and behind the urinary tract.
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE PROSTATE GLAND
1. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE PROSTATE Gland The prostate gland (prostata) is an unpaired glandular-muscular organ, consisting of individual acini, secreting substances that are a component of sperm. The prostate gland weighs up to 25 g and the following
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE TESTICES AND THEIR APPENDIXES
2. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE TESTLES AND THEIR APPENDIXES The testis (testis) is a paired sex gland of mixed secretion; forms sperm and releases hormones into the blood. The testicles are located in the scrotum. The testicles are separated by a septum, oval in shape and smooth.
STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE PENIS AND URETHER CHANNEL. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE Scrotum
3. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE PENIS AND URETHER CHANNEL. STRUCTURE, BLOOD SUPPLY AND INNERVATION OF THE Scrotum The penis (penis) is intended for excretion of urine and ejection of semen. The following parts are distinguished in the penis: body (corpus penis), glans
BLOOD SUPPLY AND INNERVATION OF THE HEART
3. BLOOD SUPPLY AND INNERVATION OF THE HEART The arteries of the heart originate from the aortic bulb (bulbus aortae). The right coronary artery (a coronaria dextra) has a large branch - the posterior interventricular branch (ramus interventricularis posterior). The left coronary artery (a. coronaria sinistra) is divided into envelope (r. circumflexus) n
Blood supply and innervation of the eye
6. Blood supply and innervation of the eye Blood supply to the eye is provided by the ophthalmic artery, a branch of the internal carotid artery. The outflow of venous blood is carried out by the vortex and anterior ciliary, and then by the orbital veins - superior and inferior. Superior vein
Blood supply to the body
Blood supply to the body In humans and other mammals, the circulatory system is divided into two circulation circles. The large circle begins in the left ventricle and ends in the right atrium, the small circle begins in the right ventricle and ends in the left
1.7. Blood supply to the central nervous system
1.7. Blood supply to the central nervous system Blood supply to the brain. It is carried out by paired internal carotid (a. carotida interna) and vertebral (a. vertebralis) arteries. The internal carotid artery originates from the common carotid artery, and the vertebral artery originates from the subclavian artery. B
Blood supply to the brain
Blood supply to the brain The life and activity of the brain depend on the continuous flow of oxygen and blood to neurons, dendrites, neuroglia and brain centers. It is also necessary to have special mechanisms to regulate blood pressure fluctuations,
Blood supply to the head and oral cavity
Kidney meridian (zu-shaoyin-shen-jing; foot line of the kidneys, small yin) (VIII; R)
Kidney meridian (zu-shaoyin-shen-jing; leg line of the kidneys, small yin) (VIII; R) The meridian is paired, symmetrical, centripetal, belongs to the yin system, has 27 points of influence. The time of maximum activity of the meridian is from 17 to 19 frequencies, the time of minimum activity is from
Herbal medicine for kidney and urinary tract diseases
Herbal medicine for kidney and urinary tract diseases
Glomerular filtration rate is 125 ml/min in men and 110 ml/min in women. The average total volume of plasma in the human body is approximately 3 liters, which means that all plasma is filtered by the kidneys about 60 times per day. The ability of the kidneys to filter such a huge volume of plasma allows them to excrete a significant amount of metabolic end products and very accurately regulate the elemental composition of the internal fluids of the body.
To continue downloading, you need to collect the image:
The blood supply to the kidneys is different from the blood supply to all other organs. Blood is needed not only to nourish the organ. It also ensures the process of urination.
Moreover, the kidneys are not only organs of the urinary system; they also perform a number of other functions.