Features of formations in the adrenal glands
Adrenal cancer is usually diagnosed in the following categories of patients:
- children under 5 years of age;
- adults aged 40-50 years;
- women over 55 years of age (included in the high-risk zone).
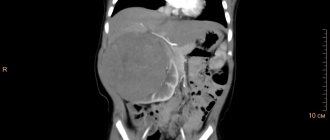
Most often, cancer is detected in the right organ. When the neoplasm reaches the last stage of development, it metastasizes to the liver and neighboring organs.
Approximately 70% of patients are diagnosed with carcinoma, or a benign tumor. It develops in the adrenal cortex and covers most of the organ. Carcinoma often disrupts the process of hormone synthesis, which affects the condition of the entire body.
About 30% of patients with adrenal cancer are diagnosed with glucosteroma, or malignant neoplasm. Women are at risk for developing such a tumor. They are diagnosed with it 5 times more often than men.
Depending on the location of the pathology and its characteristics, the nature of the clinical picture is determined.
Differential diagnosis
ACR should be differentiated from Itsenko-Cushing's disease, primary and secondary type ral cholesterol, and benign tumors of PN.
Secondary hyperaldosteronism refers to conditions in which increased formation of aldosterone is associated with prolonged stimulation of its secretion by angiotensin. Secondary aldosteronism is characterized by increased levels of renin, angiotensin and aldosterone in the blood plasma. Activation of the renin-angiotensin system occurs due to a decrease in effective blood volume while simultaneously increasing the negative balance of sodium chloride.
Secondary aldosteronism develops with nephrotic syndrome, liver cirrhosis in combination with ascites, idiopathic edema, which often occurs in premenopausal women. congestive heart failure, renal tubular acidosis, as well as Barter syndrome (dwarfism, mental retardation, the presence of hypokalemic alkalosis with normal blood pressure). In patients with Barter syndrome, hyperplasia and hypertrophy of the juxtaglomerular apparatus of the kidneys and hyperaldosteronism are detected.
Excessive potassium loss in this syndrome is associated with changes in the ascending tubule and a primary defect in chloride transport. Similar changes also develop with long-term use of diuretics. All of the above pathological conditions are accompanied by an increase in aldosterone levels; blood pressure is usually not elevated.
Screening
There is currently no screening for ACR.
As a rule, ACC and NP tumors are detected either during examination for emerging hormonal disorders in the presence of a hormonally active tumor, or by chance, if increased secretion of hormones by the tumor is not observed. The general algorithm for diagnosing AKR is presented in the diagram (Fig. 7.2).
Rice.
7.2. Diagnosis scheme for adrenocortical cancer Notes: 1. To convert the cortisol level from mcg% to nmol/l and the daily excretion of free cortisol in urine from mcg/day to nmol/day, the presented values should be multiplied by 2.759. If at a certain stage of the survey it is proposed to use several methods, you should act in accordance with their numbering.
2. ACCS - test of blood taken from the inferior petrosal sinuses on both sides (parallel measurement of ACTH level in blood plasma taken from the inferior petrosal sinuses and peripheral vein).
Indications for consultation with other specialists
Since ACR is often accompanied by the production of hormones from the NP cortex, all patients with suspected this pathology are advised to consult an endocrinologist.
An example of a diagnosis: stage II adrenal cancer T2NXM0.
Causes of cancer development
Medical research cannot yet provide an exact answer as to why cancer develops in the adrenal glands. The main factors that trigger the transformation of healthy cells into malignant ones include hereditary predisposition. However, other reasons can lead to the appearance of a tumor in internal organs, including:
- heavy consumption of unhealthy food, which contains carcinogens;
- alcohol abuse, smoking;
- a sedentary lifestyle, which contributes to the development of stagnant processes in the body;
- the presence of tumors in the body that have metastasized to the adrenal glands;
- course of adenomatous polyptosis;
- long-term use of medications (oral contraceptives);
- congenital pathologies such as Beckwith-Wiedemann or Li-Fraumeni diseases.
It is important to understand that the above factors predispose to the development of a pathological process in the adrenal glands. However, their exposure does not always provoke the occurrence of malignant neoplasms.
Classification according to the TNM system
T - primary tumor
- T1 - tumor ≤5 cm, no invasion;
- T2 - tumor >5 cm, no invasion;
- T3 - local invasion into the surrounding fatty tissue;
- T4 - the tumor grows into neighboring organs.
N - regional lymph nodes
- N0 - no metastases in regional lymph nodes;
- N1 - there are metastases in regional lymph nodes.
M - distant metastases
- M0 - no distant metastases;
- M1 - there are distant metastases.
Grouping by stages
The classification according to ENSAT (European Network for the Study of Adrenal Tumors) seems to be more clinically adapted and modern:
- Stage I
– T1 N0 M0 - Stage II
– T2 N0 M0 - Stage III
– T1-2 N1 M0,T3-4 N0-1 M0 - Stage IV
– T1-4 N0-1 M1 [4].
Laboratory diagnostics:
- Determination of cortisol in the early morning hours against the background of a suppressive test with 1 mg of dexamethasone;
- In the absence of physiological suppression of cortisol levels, determination of adrenocorticotropic hormone in the morning.
- Determination of (nor)metanephrine in 24-hour urine or plasma.
Instrumental diagnostics:
- Ultrasound;
- MRI;
- CT (gold standard);
- Osteoscintigraphy for suspected metastatic lesions of skeletal bones;
- For tumor sizes up to 4 cm, it is recommended to perform positron emission tomography with 18-fluorodeoxyglucose (PET18FDG).
It should be noted that puncture biopsy of adrenal tumors did not demonstrate an improvement in the results of differential diagnosis; on the contrary, it led to an increase in complications, false-positive and false-negative conclusions. At the moment, puncture is advisable only if metastatic lesions of the adrenal glands are suspected, where the sensitivity of cytological examination is 80–86% [3].
Classification of the disease
The clinical picture depends on the location of the cancer. A malignant tumor grows in the cortex or medulla of the adrenal glands. The first group of cancer includes:
- adenoma;
- carcinoma.
Tumors growing in the medullary globus are classified into:
- ganglioma;
- pheochromacythroma;
- neuroblastoma.
Adenoma is one of the benign neoplasms. It is more common than other types of adrenal cancer, affecting mainly the left organ. Adenoma in approximately half of cases turns into a malignant tumor. It is considered a hormone-dependent neoplasm, and therefore its appearance affects the functioning of internal organs.
The adenoma provokes the active production of hormones, which leads to the appearance of female characteristics in men, and masculine characteristics in women. The danger of this type of neoplasm is that its development is asymptomatic, and it unexpectedly develops into cancer.
Pheochromacytoma is also a hormonally active form of adrenal cancer. It occurs in one in 10,000 patients. Pheochromatytoma most often appears in older people. It is difficult to diagnose this tumor, since its symptoms are characteristic of many other pathologies.
Neuroblastomas are predominantly diagnosed in children. It has a negative effect on the sympathetic nervous system, which is responsible for the reflex actions of internal organs: contraction of the heart muscle, etc.
Anatomical structure of the adrenal glands
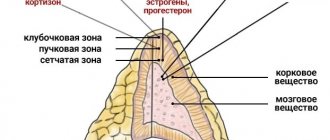
The adrenal gland is a paired endocrine gland consisting of a cortex and medulla.
The cortex (NP cortex) is formed in the 5th week of the intrauterine period from mesodermal cells located near the germ of the gonads and kidneys. The medulla is a derivative of ectodermal neural crest cells. In the 2nd month of the prenatal period, the adrenal glands are a formation that is larger in size than the kidneys. The main part of the adrenal gland is the embryonic (fetal) cortex, which undergoes atrophy and regression within a year after birth.
In the postnatal period, the permanent cortex of the NP begins to develop, in which by the third year of life three zones are clearly defined: the glomerular zone, adjacent to the capsule of the NP, the fasciculate zone, and the reticular zone, bordering the medulla. The cortex accounts for about 80% of the NP mass. In an adult, NPs have the shape of a triangle, measuring 4x2x0.3 cm and weighing 5-7 g.
The cortical and medulla layers of the NP can become sources of tumor development (Fig. 7.1).
Rice. 7.1. Anatomy of the adrenal glands
The function of the cortex is to produce certain steroid hormones: cortisol, aldosterone, androgens and estrogens. In men, most of the androgens are produced by the testes. In women, the majority of estrogen is produced by the ovaries. It should be noted that male and female NPs produce small amounts of both hormones. The medulla of the NP produces nervous system hormones - norepinephrine and epinephrine (adrenaline) - and can become the source of the development of tumors such as pheochromocytoma and neuroblastoma.
The zona glomerulosa is the thinnest layer of the adrenal cortex, which is represented by small epithelioid cells containing a small amount of weakly stained cytoplasm. Large, lipid-rich, as well as vacuolated cells and syncytium are also found here, forming clusters such as glomeruli.
Electron microscopic examination reveals elongated mitochondria in the cells of this zone, which contain lamellar cristae, which is a distinctive feature of mitochondria in the zona glomerulosa. The cells of this zone are responsible for the formation of mineralocorticoids, and in particular aldosterone. It is believed that the cells of this layer can be stem cells for the formation of the next two zones.
Most of the NP cortex is represented by zona fasciculata cells, which are characterized by a radial arrangement and are at right angles to the NP capsule. These are large cubic and polygonal cells; some of them have two cores. The cytoplasm of the cells is vacuolated and contains a large amount of lipids.
Electron microscopy reveals an agranular endoplasmic reticulum or agranular endoplasmic reticulum in the cells of this zone. Mitochondria, although different in size, are larger compared to the mitochondria of the glomerular and reticular zones. They are characterized by tubular and vesicular cristae, which are protrusions of their own membrane, or the presence of free vesicles in the mitochondrial matrix.
Cholesterol, which NPs are rich in, is found mainly in the cells of this zone in greater quantities than in any other tissue of the body. In the inactive phase, this layer is represented mainly by light, spongy, lipid-rich cells. When stimulated with adrenocorticotropic hormone (ACTH)
When the cholesterol contained in the cells is spent on the formation of corticosteroids, the cells of the zona fasciculata become compact. The cells of the zona fasciculata mainly produce glucocorticoids.
The inner layer of the cortex, adjacent to the medulla, is called the reticular or reticular zone, which consists of intertwined irregularly shaped strands of small cells containing pigment, a small number of lipid droplets and well-stained cytoplasm. The mitochondria of the cells of this zone are close to the mitochondria of the zona fasciculata, although they differ in a more elongated shape and contain flattened cristae. This zone is responsible for the formation of sex hormones - androgens, estrogens and a small amount of progesterone.
The medulla of the NP contains large secretory cells grouped into oval-shaped formations or cords that connect to each other. These cells contain delicate granules containing epinephrine and norepinephrine, turn brown when treated with chromatin-oxidizing reagents, and are called chromaffin cells.
The blood supply to the NP cortex is carried out by three large and many small arterial vessels. The superior adrenal artery is a branch of the inferior phrenic artery, the middle adrenal artery arises directly from the aorta, and the inferior - from the renal artery.
The outflow of venous blood occurs through the central vein. The central vein of the right NP (about 1 cm long) flows into the inferior vena cava, and the vein of the left NP, which is slightly longer than the right (2-4 cm), flows into the renal vein. Lymphatic vessels, spreading throughout the NP tissue, form plexuses under the capsule and in the medulla.
Symptoms of the disease
The development of adrenal cancer goes through several stages. At the initial stages, when the size of the tumor does not exceed 5 cm, the pathological process in the organ is asymptomatic.
The first signs indicating damage to the adrenal glands appear when the tumor grows beyond the capsule.
If a patient develops a hormonally active neoplasm, he will experience the following symptoms:
- osteoporosis (in children);
- obesity;
- muscle weakness;
- arterial hypertension;
- hypertensive crisis.
Women exhibit male characteristics such as:
- rough voice;
- active growth of hair and muscle mass;
- change in facial features.
In men, the reverse process occurs, in which the voice becomes softer.
Less commonly, a cancerous tumor provokes:
- convulsions;
- partial or complete paralysis of the limbs;
- increase in blood pressure.
Due to the fact that adrenal cancer increases the production of corticosteroid hormones, the patient exhibits specific symptoms that make it possible to suspect the presence of a malignant neoplasm:
- dysfunction of the digestive system (vomiting, nausea, dyspepsia);
- lack of appetite, which leads to sudden weight loss;
- frequent neuroses, panic attacks, anxiety and apathy (nervous system disorders);
- anemia;
- pain syndrome (occurs with metastases);
- lack of potassium in the body;
- exhaustion of the body;
- decreased sex drive;
- acne eruptions of atypical form.
If a malignant neoplasm activates the production of cortisol, the following phenomena are observed:
- weight gain;
- the appearance of multiple bruises on the skin;
- swelling of tissues in the upper body;
- psychoses, sudden changes in mood.
Each type of adrenal tumor is characterized by its own clinical picture. With pheochromocytoma, the functioning of the cardiovascular system is disrupted, which manifests itself in the form of high blood pressure, frequent shortness of breath and rapid heartbeat. Also, the development of this tumor is accompanied by active sweating.
Neuroblastoma causes bone pain and intestinal problems.
Metastatic lesion of the adrenal glands
Epideitology
NPs rank fourth after the lungs, liver and bones in terms of the incidence of metastases.
The latter are found in them in 9-27% of cases of malignant neoplasms of other organs; often metastases are bilateral (41% of cases). Based on the results of 13,906 autopsies, the incidence of metastases in the NP was 3.1%. Most often, lung cancer (up to 40%) and breast cancer (20-35%) metastasize to the NP. less commonly, kidney cancer (1.2-10%), melanoma (1-8.6%), cancer of the gastrointestinal tract, pancreas, and seminoma. Metastases can be solitary and multiple. Large metastases may be accompanied by necrotic changes. When more than 90% of the adrenal tissue is destroyed by metastases, patients develop adrenal insufficiency.
It has been established that the likelihood of metastatic damage to the NP in renal cell carcinoma depends on the stage of the primary tumor and its location in the upper pole of the kidney. The occurrence of a tumor thrombus in the renal vein can also be a harbinger of metastasis in the NP. The presence of a tumor thrombus in the right renal vein is detected in only 20% of corresponding metastases in the right NP, whereas in the presence of a tumor thrombus in the left renal vein, metastases in the NP are detected in 67%.
Bilateral metastases occur in approximately half of patients with metastatic lesions of the NP and, as a rule, are a reflection of an advanced metastatic process. Metastases in the NP are in most cases combined with metastases to other organs. However, isolated metastases to the adrenal gland are not always a manifestation of the primary tumor.
Thus, in a study that included 330 patients, 9.6% of patients with non-small cell lung cancer were found to have isolated space-occupying lesions in the NP according to CT data. In 65% of cases, a benign adenoma was verified based on the results of aspiration biopsy, open biopsy, or CT scan during follow-up. In other cases, the presence of metastases was confirmed using CT-guided aspiration biopsy. According to autopsy data, a higher incidence of benign NP tumors was established in patients with renal cell carcinoma compared to the general population.
Unlike primary NP tumors, metastases are non-encapsulated formations. Typically, metastases in the NP indicate dissemination of the primary tumor and a poor prognosis. However, in some cases of isolated metastatic NP tumors in patients who have undergone radical treatment for the primary tumor, removal of the affected NP offers hope for long-term survival.
Clinical picture
In most cases, metastatic NP tumors are asymptomatic, have no clinical manifestations and are detected incidentally during a follow-up examination.
Thus, according to one study, only 20 out of 464 (4.6%) patients with malignant neoplasms had clinical manifestations of metastatic lesions of the NP. According to other data, the frequency of asymptomatic metastases to the adrenal glands was 61%. Large metastases usually manifest as pain. Other possible signs of malignant tumors - weight loss, weakness, anorexia, etc. are characteristic of any generalized tumors. Adrenal insufficiency is observed in 25% of patients with clinical manifestations of metastases in the NP and occurs exclusively with bilateral lesions.
The most common tumor that leads to the development of overt hypocortisolism is non-Hodgkin large cell lymphoma. Less commonly, it is caused by metastases of bronchogenic lung cancer or tumors of other localizations. Clinically significant hemorrhage due to adrenal metastases is extremely rare. In isolated cases, there may be indications for immediate laparotomy for the purpose of hemostasis.
Diagnostics
The main importance in the diagnosis of metastatic tumors of NP belongs to the data of the anamnesis, as well as basic imaging methods (ultrasound, CT and MRI).
The presence of an appropriate medical history in a cancer patient simplifies the diagnosis of metastatic lesions of the NP when identifying an incidental formation in the NP. Phase-antiphase MRI has established itself as a reliable method for differential diagnosis between asymptomatic nodes accidentally detected during a regular examination and metastases in the NP. Puncture of NP formation followed by cytological or morphological examination makes it possible to clarify the presumed diagnosis, however, according to many researchers, it should be performed only in patients with an established primary tumor if metastatic lesions of the NP are suspected. since puncture of a hormonally active adrenal tumor can lead to increased release of hormones synthesized by the tumor.
If the histological structure of the primary tumor does not have any similarity with the cellular elements of the NP (for example, in a lung tumor), morphological verification of metastases is not difficult. At the same time, the problem of differentiating metastases of renal cell clear cell carcinoma from the most common benign tumor of the adrenal gland - clear cell adrenocortical adenoma - remains quite difficult even for a pathologist.
Microscopic examination of kidney cancer metastases in the NP in most cases reveals a massive expansion of metastasis, up to complete replacement of the adrenal gland with a tumor. In-depth histological analysis requires the use of innovative technologies in histomorphological studies, and above all in immunohistochemical studies. However, due to the rarity of adrenal metastases, the use of needle biopsy in all patients with hormonally inactive adrenal tumors to detect metastases would lead to a large number of unnecessary biopsies.
Positron emission tomography (PET)
allows you to differentiate benign NP neoplasms from malignant ones with high sensitivity and specificity (up to 100%). Given the non-invasiveness and high accuracy of PET, this method can replace needle biopsy in the diagnosis of metastatic lesions of the NP. The use of PET opens up the possibility of early detection of other hidden metastases and will eliminate the need for MRI of the brain and bone scintigraphy. The main disadvantages of PET are limited availability and high cost.
Treatment
Until relatively recently, the detection of metastases in the NP indicated the incurability of a patient with generalized metastasis of the primary tumor, however, the accumulated experience of operations with satisfactory long-term results on the lungs and liver regarding metastases detected in them served as the basis for revising the pessimistic attitude towards operations for metastatic tumors of the adrenal gland.
Metastatic lesions of the NP are an indication for adrenalectomy (open or laparoscopic) provided there are no other distant metastatic foci of the primary tumor. Since metastatic lesions of the NP are a manifestation of the generalization of the underlying disease, in the postoperative period it is advisable to carry out adjuvant chemotherapy or radiation therapy, taking into account the sensitivity of the primary tumor.
Forecast
A relapse-free period lasting more than 6 months, according to most authors, is the main, relatively favorable prognostic factor for metastatic adrenal tumors.
It probably serves as a kind of marker of the biological aggressiveness and malignancy of the primary tumor. Patients whose histological type of metastatic adrenal tumor is adenocarcinoma have a longer life expectancy compared to those whose primary tumor was of a different histological type. In patients with an unknown location of the primary cancer and metastatic lesions of the ulcer, the prognosis is extremely unfavorable; the average life expectancy after adrenalectomy is about 7 months. On average, the 5-year survival rate of patients after surgical treatment for metastatic lesions of the NP reaches 29-42%.
IN AND. Chissov, B.Ya. Alekseev, I.G. Rusakov
Published by Konstantin Mokanov
Diagnosis of formations in the adrenal glands
If adrenal cancer is suspected, the following diagnostic measures are prescribed:
- Chest X-ray . Allows to identify metastases in the lungs.
- PET . Provides information about the current stage of development of the tumor, its size and location.
- MRI . Prescribed when it is suspected that metastases have penetrated the spinal cord or brain.
- Ultrasound . Allows detection of adrenal cancer and liver metastases.
- CT scan Creates a visual image of the tumor, through which it is possible to evaluate its structure.
- Histological examination . Allows you to determine the nature of the tumor.
Additionally, urine and blood tests are performed, which show excess levels of certain hormones.
Classification according to the TNM system
T - primary tumor
- T1 - tumor ≤5 cm, no invasion;
- T2 - tumor >5 cm, no invasion;
- T3 - local invasion into the surrounding fatty tissue;
- T4 - the tumor grows into neighboring organs.
N - regional lymph nodes
- N0 - no metastases in regional lymph nodes;
- N1 - there are metastases in regional lymph nodes.
M - distant metastases
- M0 - no distant metastases;
- M1 - there are distant metastases.
Grouping by stages
The classification according to ENSAT (European Network for the Study of Adrenal Tumors) seems to be more clinically adapted and modern:
- Stage I
– T1 N0 M0 - Stage II
– T2 N0 M0 - Stage III
– T1-2 N1 M0,T3-4 N0-1 M0 - Stage IV
– T1-4 N0-1 M1 [4].
Clinical picture
Treatment tactics are selected based on the nature of the pathology, its size, and stage of development. The treatment regimen also takes into account the individual characteristics of the patient.
Basically, to suppress the tumor process, surgery is used, during which the affected tissue is removed. For adrenal cancer, the following techniques are used:
- Laparoscopy . The tumor is removed through small incisions using a special instrument.
- Transabdominal therapy . Involves making a large incision in the abdominal cavity.
- Thoracobdominal therapy . It is prescribed when the cancerous tumor has grown to a large size. During the operation, the abdominal cavity and chest are cut.
In advanced cases and for medical reasons, when surgical intervention is impossible due to the individual characteristics of the patient (age, etc.), radiation and chemotherapy are prescribed. Both treatment methods cause serious consequences in the form of nausea, vomiting, headaches and other phenomena.
Hormonal therapy is prescribed if other treatment methods are contraindicated for the patient. It is also used to normalize hormonal balance after surgery. Drugs are selected depending on the concentration of which substance is exceeded in the body.
Treatment
The goals of treatment are to remove the primary tumor and correct the hormonal imbalance caused by the increased production of hormones by the primary tumor.
Indication for hospitalization
ACR therapy should be carried out in a specialized oncology hospital. Hospitalization of the patient is mandatory.
Surgery
Surgical treatment is the main method of treatment for patients with ACC.
In patients with ACC with increased aldosterone production, preoperative therapy with aldosterone antagonists (veroshpiron, etc.) can reduce blood pressure, restore potassium levels in the body, and also normalize the renin-angiotensin-aldosterone system, the function of which is inhibited in this disease. The standard treatment for ACC is surgical removal of the adrenal gland (adrenalectomy) and regional lymph nodes (LNs)
. Regional lymph nodes for the right NP are retrocaval, laterocaval and interaortocaval. For the left NP - preaortic, lateraortic. interaortocaval and retroaortic. In case of generalized disease, removal of all metastatic foci is indicated if possible.
If indicated, resection of the ipsilateral kidney or nephrodrenalectomy can be performed simultaneously with adrenalectomy. resection of the pancreas, liver, etc. Relapses of ACC after radical adrenalectomy are observed in 35-85% of cases. The surgical approach that can be formed when performing adrenalectomy depends on the size and location of the tumor, data from the main imaging methods, and the experience and preference of the surgeon.
The standard is an oblique or median laparotomy, as when performing a transabdominal nephrectomy. The peritoneum is opened along Told's line, access is made to the retroperitoneal space and the adrenal gland. It should be remembered that the adrenal vein on the left departs from the left renal vein, and on the right from the inferior vena cava.
The NP vessels are mobilized, crossed with clamps and ligated. To cross the vessels of the NP, you can also use the LigaShure bipolar coagulation device, which allows you to safely cross blood vessels with a diameter of up to 0.5 cm. Then the NP is mobilized along the lateral, upper, lower and posterior surfaces, and removed within the capsule along with the surrounding tissue.
When removing hormonally active ACR, special care must be taken, since active mobilization of the adrenal gland can lead to the release into the blood of a large amount of hormones or their precursors, secreted in large quantities by the tumor. Early mobilization and division of the PN vessels is the main goal of surgical intervention in this situation.
Laparoscopic adrenalectomy is an alternative to open surgery and has a number of undoubted advantages. Due to less tissue trauma during laparoscopic surgery, the period of convalescence and the duration of taking narcotic analgesics are reduced, and a better cosmetic effect is achieved. The duration of laparoscopic adrenalectomy is slightly longer than the duration of open surgery in a series of studies by a number of authors, but the amount of blood loss is significantly less than with open adrenalectomy. Oncological results of laparoscopic surgery do not differ significantly from open surgery.
List of necessary instruments to perform laparoscopic adrenalectomy:
I. Equipment and apparatus
Standard operating room equipment:
Laparoscopic stand. Laparoscopic color 3-processor video camera. Laparoscope 10 mm 30° or 0°. Color monitor. Light source. Flexible light guide. Insufflator. Device for monomolar and bipolar coagulation. Apparatus for irrigation and aspiration. Argon plasma coagulation apparatus.
II. Consumable tools:
Laparoscopic stylets with trocars 5, 10 and 12 mm. Laparoscopic scissors. The clamp is laparoscopic. Coagulation electrodes are monopolar and bipolar. Argon plasma coagulation electrode. Bipolar coagulation clamp 5 and 10 mm. Laparoscopic dissector. Device for extracting the removed drug.
When performing laparoscopic adrenalectomy, the patient is placed on the side or half of the side opposite to the operation. At the level of the xiphoid process, a cushion is placed under the patient. During surgery on the left NP, as a rule, 4 trocars are installed. A puncture of the anterior abdominal wall is performed in the paraumbilical region along the edge of the left rectus abdominis muscle. A trocar for the laparoscope is installed in the same area. Additionally, 3 more trocars are installed.
One is in the left hypochondrium along the midclavicular line, the second is in the left iliac region along the midclavicular line, and another one, which is used for traction of the kidney, is in the left lateral region along the posterior axillary lyce (Fig. 7.3a). During surgery on the right NP, a trocar for the laparoscope is installed in the paraumbilical area along the edge of the right rectus abdominis muscle.
Manipulation trocars are installed in the right hypochondrium and right iliac region along the midclavicular line. A trocar for traction of the liver is installed in the right lateral region along the posterior axillary line. Additionally, to retract the liver, you can install another trocar in the right hypochondrium along the midclavicular line (Fig. 7.3b). The main stages of laparoscopic adrenalectomy do not differ significantly from the stages of open surgery.
Rice. 7.3. Diagram of trocar installation: a - during surgery on the left adrenal gland; b — during surgery on the right adrenal gland
After completion of adrenalectomy, regional lymphadenectomy is performed. Depending on the side of the lesion, the corresponding groups of lymph nodes are removed.
Medicinal and radiation baking
Adrenocortical cancer is a tumor resistant to radiation or chemotherapy, so the use of these types of therapy is ineffective.
Therefore, aggressive surgical tactics in patients with ACC, including when relapses occur, are the most rational. The best candidates for repeat surgery for recurrent ACC are patients with no distant metastases. A number of clinical studies have shown that the survival rate of patients with relapses of ACC after repeated surgical interventions is significantly higher than in the group of patients receiving chemotherapy. Thus, in an observation that included 179 patients with ACC, relapses were noted in 52 (37%) patients. In a group of 20 patients who underwent removal of a recurrent tumor, the median survival was 15.8 months; in the group of chemotherapy without surgery (32 patients) it was only 3.2 months.
However, ACC is an extremely aggressive tumor, so many patients are initially generalized already at the initial diagnosis. The maximum possible cytoreductive operation is a mandatory stage of treatment for this group of patients. At the second stage, chemotherapy is indicated. The main goals of chemotherapy are to suppress the hormonal activity of the tumor, as well as to achieve cytostatic and cytotoxic effects.
The main cytotoxic agents used for the treatment of ACC are mitotane, metyrapone, aminoglutethimide and ketoconazole. Metyrapone inhibits hydroxylation processes in ACC cells and also blocks the conversion of substance S into cortisol and 11-deoxycorticosterone into corticosterone. The drug is used to relieve the main symptoms of Cushing's syndrome. Recommended doses of the drug are 1-3 g per day.
When co-administered with aminoglutethimide in the presence of a tumor with excessive production of mineralocorticoids, the daily doses of both drugs may be reduced. Aminoglutethimide inhibits the activity of cytochrome p-450 and disrupts the synthesis of the aromatic ring of steroids. The drug is prescribed in a dose of 250-500 mg 4 times a day. The effectiveness of the drug in reducing cortisol concentrations in patients with ACC is assessed on the 10-14th day of therapy.
The drug does not have a significant effect on suppressing tumor progression. Mitotane causes atrophy and necrosis of the glandular tissue of the NP. The mechanism of its action on the NP cortex is still not completely clear, however, according to a number of studies, the drug inhibits several enzyme systems, including 11-β-hydroxylation. Disruption of this process leads to a decrease in free cortisol in the blood serum and urine and an increase in its precursor, 11-dioxycortisol.
In addition to disrupting steroid synthesis, mitotane has a cytotoxic effect on ACC cells. The recommended dose is 8-10 g per day in 3-4 doses. The severity of mitotane side effects most often depends on the dose; Almost half of the patients receiving the drug experienced weakness, drowsiness, disorientation, lethargy, and headaches.
More severe neurotoxic effects of mitotane (ataxia and dysarthria) have also been described. Most cases develop gastrointestinal symptoms, including loss of appetite, nausea and diarrhea. It has recently been shown that constant monitoring of serum mitotane levels allows for long-term maintenance of its therapeutic concentrations, while reducing the incidence of side effects.
In addition to the listed drugs, other cytotoxic agents are also used to treat patients with adrenocortical cancer. The effectiveness of some of them is presented in table. 7.2.
Table 7.2. Results of chemotherapy for adrenocortical cancer
The role of radiation therapy in patients with ACC is insignificant, since the tumor is extremely radioresistant. In some studies, intraoperative irradiation of the tumor bed was performed for locally advanced tumors. However, data on improvements in survival, local tumor control and relapse prevention are unknown. The use of external beam radiation therapy is justified in patients with ACC with metastatic bone lesions for palliative purposes to eliminate pain,
The use of transarterial embolization and radiofrequency ablation are experimental techniques that can be used in patients with unresectable tumors, in carefully selected patients, as well as in patients with liver metastases. Thus, in a series of observations of 15 patients with metastatic or unresectable ACC, in 8 (53%) patients who underwent radiofrequency ablation, stabilization of these lesions was observed over 10 months. However, no data have been obtained to increase the survival rate of this group of patients.
Approximate periods of incapacity for work
The duration of a patient's hospital stay in the absence of treatment complications is 7-14 days. The patient is disabled for 20-30 days after surgery.
Evaluation of treatment effectiveness
The effectiveness of the therapy is assessed based on the patient’s hormonal status, the disappearance of clinical symptoms of increased hormone production, as well as indicators of overall disease-free survival of patients.
Medical prognosis
Life expectancy after treatment of neoplasms directly depends on the stage of development at which the tumor process is diagnosed. A positive prognosis is made for benign adrenal cancer.
Successful treatment of adrenal cancer is possible if it is carried out when the tumor has reached the first or second stage of development, then the survival rate is very good. The later prognosis is disappointing. About 20% of patients live 5 or more years of life when treatment was carried out at the third stage of tumor development. In advanced cases, this figure decreases to 10%.
Prognosis for adrenal cancer
Survival after surgery largely depends on the extent and nature of the spread of the disease. Cancer can affect not only this organ, but also some neighboring parts of the body. To avoid this, the disease should be detected at the first stage, only in this case the treatment result will be achieved quickly. High-quality treatment in the first two stages of the spread of the disease guarantees survival for approximately eighty percent of patients. At the fourth stage of an adrenal tumor, a positive result can be recorded in a smaller number of patients due to the extensive spread of metastases to neighboring organs and parts of the body.
With early diagnosis and timely treatment, a favorable outcome can be achieved. This can be achieved through the use of therapeutic anticancer drugs, which must also be used without fail.
No system has been developed that would completely prevent the development of this pathology. However, to maintain health, any person needs to lead a healthy lifestyle, eat right and exercise in moderation. In order to detect the development of the disease in a timely manner, it is necessary to carry out preventive examinations. At the first symptoms, you should immediately seek advice from a specialist in this field.
Treatment[edit | edit code]
The main form of treatment for ACC is surgery. The operation should be carried out in the usual way (cavity surgery). Laparoscopic operations are prohibited, every patient should know this, otherwise there is a risk of tumor contamination.
Adjuvant (preventive) therapy after surgery is carried out with the drug mitotane (chloditan, lysodren), which is included in most chemotherapy protocols for ACR.
Currently, the greatest experience in the use and monitoring of patients taking mitotane in Russia is the Endocrinology Research Center of the Ministry of Health of the Russian Federation and the Russian Oncology Research Center named after Nikolai Nikolaevich Blokhin. The greatest experience in the treatment of ACR in Russia has been accumulated at the Russian Cancer Research Center named after. Blokhin, at least 400 people were treated there.
Mitotane is currently registered in the Russian Federation (Mitotane tablets 500 mg, LP-004684 dated 02/05/2018). Previously, Mitotane was also produced under the trade name Chloditan in what is now Ukraine, where the drug was no longer produced due to the decline of the pharmaceutical industry in the 1990s throughout the post-Soviet space.
As for the effectiveness of using mitotane, controversy surrounding it continues to this day. Mitotane is believed to be effective in 30% of cases. Self-administration of this drug is unacceptable and can only be done under medical supervision, since mitotane suppresses the functioning of a healthy adrenal gland and the use of mitotane without replacement therapy (one of the replacement therapy drugs is Cortef) can lead to the death of the patient.
Scientific research on adrenocortical cancer is not carried out in Russia; the most well-known centers for the study of ACC at the moment are the University of Michigan, as well as the National Institutes of Health in the USA and the University of Würzburg in Germany.
The vast majority of cancer hospitals around the world are faced with this disease, sometimes only once in a decade, so attempts are being made in the Internet community to create forums or groups that bring together patients diagnosed with adrenocortical cancer to exchange treatment experiences and maintain morale in the fight against this disease. A group called “Adrenocortical cancer - adrenal cortex cancer” has been created on the social network Facebook, where patients from Russia, Ukraine, and other neighboring countries, their relatives and friends become participants and do not feel lonely, and also receive important information about where to get the necessary treatment. There are now more than 100 participants registered in this group.
Therapy methods
Radical and conservative methods are used to treat malignant neoplasms. In the early stages of cancer development, it is advisable to perform surgical intervention. To achieve the maximum therapeutic effect, surgical treatment is combined with radiation, chemotherapy and immunotherapy.
Surgical intervention
Surgical treatment involves removal of the adrenal gland. This operation is called adrenalectomy. Today, minimally invasive surgical techniques are especially popular. To carry out this manipulation, the specialist uses special microsurgical instruments. Blood loss and pain during the operation are minimal, so it is much easier for the patient to endure it.
Blood loss and pain during minimally invasive surgery are minimal, so it is much easier for the patient to tolerate it
Radiation therapy
In this case, the action of high doses of ionizing radiation is used, which kills oncogenic cells, however, the possibilities of such treatment for ACC are limited. The fact is that carcinogenic cells are quite resistant to X-ray irradiation. Most often, radiation therapy is prescribed after surgery to prevent recurrence of the pathology.
Chemotherapy
In this case, doctors use a group of drugs that have a detrimental effect on cancer cells. The following medications are used in the treatment process: Etoposide, Cisplatin, Doxorubicin, Streptozocin, Vincristine. These drugs block the uncontrolled, atypical division of oncogenic cells.
Chemotherapy improves the general condition of the patient, but such treatment does not lead to complete recovery.