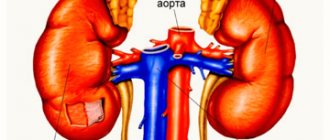
Aldosterone is one of the important hormones synthesized in the adrenal glands, without which the coordinated functioning of the endocrine system as a whole is essential. Fluctuations of this hormone (lack, excess) lead to functional failure and the development of a whole complex of symptoms that are unfavorable for patients. This is hyperaldosteronism , the mechanism and provoking factors, which can be very different.
An endocrinologist examines the pathology and prescribes effective treatment. The choice of tactics directly depends on the type, origin, severity of the pathology, and existing problems in patients with the urinary and cardiovascular systems.
What is hyperaldosteronism?
Hyperaldosteronism is a set of syndromes with different pathogenesis and symptoms or disease caused by hypersecretion, increased production (metabolic disorder) of mineralocorticoid aldosterone in the adrenal cortex.
Patients often experience Conn's syndrome, a benign tumor of the adrenal cortex. The risk group includes women over 40 years of age.
Clinically, the pathology manifests itself as arterial hypertension, which accounts for up to 70% of all known cases. In a complicated course against the background of severe hypokalemia, arrhythmia may develop with a fatal outcome.
The main method of exposure is surgery (adrenalectomy) to remove the affected adrenal gland. If tumor-like formations produced by aldosterone occur, artery stenting is performed. For secondary hyperaldosteronism, endovascular balloon dilatation is performed.
If the aldosterone-producing formation is benign and adrenal cancer is not confirmed during the diagnosis, then the prognosis is quite favorable. After drug treatment, patients quickly recover.
Prevention
The development of the disease is usually slow but progressive. Removal of aldosteroma in the early stages of the disease can lead to complete recovery. With advanced vascular and renal lesions, they can be irreversible even after removal of the tumor. With a full-blown clinical picture of Conn's syndrome, patients are unable to work. After tumor removal, ability to work is determined by the severity of remaining renal and vascular disorders.
Temporary improvement in the condition of patients can be achieved by using spironolactone - veroshpiron 25-50 mg 4 times a day, as well as when taking potassium - up to 10 g of potassium chloride per day. This therapy is recommended during preoperative preparation.
The only radical treatment method is removal of the aldosteroma. An abdominal approach is recommended, allowing exploration of both adrenal glands. Due to the possibility of atrophy of the second adrenal gland, if, along with aldosterone, the tumor also produces an increased amount of cortisol, surgery, as with other hormonally active tumors of the adrenal cortex, is preferably performed with the administration of glucocorticoids. Sometimes after surgery long-term treatment with deoxycorticosterone or additional salt intake is required.
Causes
reasons for the development of pathology . Basic:
- adenoma of the adrenal cortex caused by hypersecretion of aldosterone;
- bilateral hyperplasia of endocrine gland tissue
- hypertension;
- liver cirrhosis due to increased renin production;
- dehydration of the body;
- abuse of a number of medications (laxatives, diuretics);
- the use of oral contraceptives by women, which can lead to the development of a secondary form of the disease;
- adrenal cortex carcinoma;
- hereditary factor in case of detection of excess aldosterone production against the background of autosomal dominant inheritance;
- disruption of metabolic processes involving aldosterone;
- abuse of hormonal drugs containing estrogen;
- menopause in women with hormonal imbalance.
Secondary hyperaldosteronism develops due to:
- abuse of medications (diuretics, hormones containing estrogen);
- hyperproduction syndrome, ACTH;
- heart failure (congestion);
- arterial, renal hypertension;
- essential hypertension of the hyperrenin form.
Provoking factors for the development of the condition
A disease such as hyperaldosteronism often provokes the development of diseases aggravated by heredity, adenoma of the adrenal cortex, leading to primary aldosteronism in 70% of cases. The provoking factors of the disease are systemic. As a rule, this is the development of pathologies in the thyroid gland, intestines, and ovaries in women.
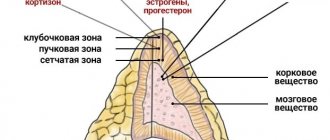
Features of primary aldosteronism
In diseases of the adrenal glands, primary hyperaldosteronism syndrome develops. It is associated with increased formation of the cortical hormone – aldosterone. Due to excess of its content in the blood, the following changes occur:
- increased reabsorption of sodium and water (delayed excretion) in the renal tubules;
- loss of potassium in urine;
- increase in circulating blood volume;
- decreased secretion of renin by the kidneys;
- alkalization of blood;
- increased sensitivity of arteries to adrenaline and norepinephrine;
- increase in peripheral vascular resistance;
- arterial hypertension;
- nephropathy due to potassium deficiency;
- muscle weakness.
Jerome Conn in 1955 described the symptoms of hyperaldosteronism in adrenal adenoma and reported the results of successful treatment after its removal. Therefore, primary aldosteronism began to be called Conn's syndrome.
There are clinical forms of adrenal gland lesions in addition to aldosteroma, as well as secondary ones, in which there is an increase in renin without diseases of the adrenal glands. The response increase in aldosterone synthesis is caused by low sodium levels, decreased renal blood flow, liver cirrhosis, kidney tumors, and failure of kidney function.
We recommend reading the article about surgical removal of the adrenal glands - adrenalectomy. From it you will learn about indications for removal of the adrenal glands, contraindications, types of adrenalectomy, surgical technique and recovery after.
And here is more information about the functional autonomy of the thyroid gland.
Symptoms
Symptoms directly depend on the type of pathology. With hyperaldosteronism, signs characteristic of Conn's syndrome are observed (photo above), especially at the early stage of uncontrolled production of the hormone aldosterone against the background of dystrophic changes in the adrenal cortex. Main symptoms:
- arterial hypertension;
- constantly elevated diastolic pressure;
- decreased vision;
- vascular lesions of the fundus;
- dysfunction of nervous and muscle tissue due to lack of potassium in the body;
- weakness, rapid fatigue;
- pseudoparalytic states;
- headache;
- water-electrolyte imbalance;
- hypochondria;
- asthenia syndrome (psycho-emotional disorder);
- cephalgia;
- cardialgia;
- tachycardia;
- myasthenia gravis;
- paresthesia, numbness of the upper extremities;
- convulsive muscle twitching;
- sagging head syndrome;
- polyuria due to changes in the renal tubules with urine output of no more than 3 liters per day.
Diagnostically revealed:
- low concentration of potassium and increased concentration of sodium ions in the urine;
- high PH level due to the accumulation of alkaline metabolic products in the blood;
- high aldosterone levels;
- low level of renin in the blood, unregulated even by medications;
- left ventricular hypertrophy during an ECG.
Secondary hyperaldosteronism is a kind of compensation for the primary one and it often happens that there are no characteristic symptoms. In case of fluid retention and sodium accumulation in the kidneys, patients experience:
- swelling;
- hypernatremia;
- frequent urge to go to the toilet at night;
- increased anxiety;
- sweating;
- hypochondria;
- high blood pressure;
- low potassium levels in the blood;
- signs of alkalosis.
A feature of secondary aldosteronism is an excess of sodium in the urinary system, which provokes an increase in blood pressure and an increase in circulating blood volume. At a time when there is a catastrophic lack of potassium in the body. This leads to weakening of muscles and chronic constipation in patients.
With the development of primary pathology, stagnation of sodium ions and fluid in the body is observed. Due to this, blood pressure increases, the heart hurts, vision decreases, and the volume of urine excreted per day increases . Convulsions and pseudoparalysis in one muscle group may be observed periodically . Episodes – psycho-emotional instability, heart failure . At the same time, pressure indicators are consistently high and can cause oxygen starvation of tissues and chronic renal failure.
REFERENCE! It happens that with hyperaldosteronism, blood pressure readings are absolutely normal. Although this develops a secondary form - Barter syndrome. The secondary form of pathology is considered a compensatory mechanism under the influence of various types of pathologies.
The symptoms of the main provoking disease are clinically manifested:
- kidney dysfunction;
- neuroretinopathy;
- fundus hemorrhage;
- atrophy of the heart muscle;
- nephrogenic diabetes.
It happens that symptoms are practically absent or hypertension is pronounced in Barter syndrome. Most often, with secondary hyperaldosteronism, diseases of the heart, liver and kidneys begin to progress, manifesting themselves in the form of heart failure, arterial hypertension, nephrotic syndrome, and cirrhosis of the liver.
On a note! Secondary hyperaldosteronism does not lead to electrolyte imbalance.
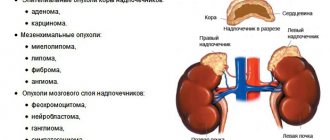
Forms of primary aldosteronism - causes and symptoms
The pathological condition is characterized by six forms of the disease. Each has its own cause of development and symptoms. Doctors distinguish the following types of pathology in the case of primary hyperaldosteronism:
| Form of the disease | Causes | Features of the disease, symptoms |
| Aldosterone-producing adenoma (Conn's syndrome) | Development of aldosteroma - benign adenoma |
|
| Idiopathic hyperaldosteronism (IHA) | Hyperplasia of the adrenal cortex, having a small-nodular or large-nodular form |
|
| Primary unilateral adrenal hyperplasia |
|
|
| Familial hyperaldosteronism Type I (glucocorticoid-suppressed hyperaldosteronism) Type II (glucocorticoid-unsuppressible hyperaldosteronism) | Hereditary pathology caused by the formation of a defective enzyme as a result of gene mutation 11b-hydroxylase, aldosterone synthetase |
|
| Aldosterone-producing carcinoma |
|
|
| Aldosteronectopic syndrome with extra-adrenal localization of aldosterone-producing tumors (in the thyroid gland, ovaries, intestines) |
|
|
Types and stages of the disease
Hyperaldosteronism is divided into:
- primary aldosteronism in the case of increased activity of the cellular structures of the zona glomerulosa, excessive production of aldosterone in the adrenal cortex;
- secondary aldosteronism, complicated by excessive secretion of aldosterone production against the background of disorders occurring in neighboring organs (kidneys, liver, heart).
Varieties of the primary form of the disease, according to the classification:
- diffuse, focal hyperplasia.
- aldosterone-producing adenoma.
- Conn's syndrome.
- glucocorticoid dependent form.
- pseudohyperaldosteronism in the case of non-uptake of aldosterone by the renal tubules.
- Itsenko-Cushing syndrome.
- familial type 1,2, not affected by glucocorticoids.
- aldosterone-producing carcinoma of the adrenal cortex.
adrenal, idiopathic hyperaldosteronism occurs .
Pathogenesis
The pathogenesis of this pathological process (both primary and secondary aldosteronism) has been fairly well studied.
In the primary form, the following occurs in the body:
- due to the increased amount of aldosterone, sodium reabsorption in the kidney tubules begins to increase, resulting in an increase in the excretion of potassium from the body along with urine;
- insufficient potassium leads to muscle weakness and symptoms of kidney dysfunction;
- dystrophic changes occur in the kidney tubules, which makes it impossible to respond to antidiuretic hormone;
- intracellular potassium begins to be replaced by hydrogen and sodium compounds, which leads to the development of intracellular acidosis and alkalosis.
Ultimately, all this leads to tubular nephropathy.
The pathogenesis of secondary aldosteronism is based on an increase in plasma renin activity and aldosterone levels as a result of one or another etiological factor.
Diagnostics
The examination of patients begins with identifying the provoking causes that led to the development of the disease. In most cases, patients have clearly increased excoriation of aldosterone in the blood or urine, and renin (a component of the renin-angiotensin system) is practically inactive. Although this is not a factor in confirming the pathology, since in elderly patients suffering from hypertension this is a completely acceptable phenomenon.
At the initial stage, the state of the renin-angiotensin-aldosterone system is examined to identify the concentrate of renin and aldosterone in the urine , blood after exercise or at rest in patients.
The doctor-endocrinologist studies the anamnesis, medical history, and draws up a protocol for the subsequent development of a treatment program. Conducts a physical examination of the condition of the skin, measures blood pressure. Next, patients are referred to an ophthalmologist for a fundus examination.
Diagnostics for identifying primary hyperaldosteronism is differential with the aim of identifying the etiology and form of pathology. It is based on a blood and urine test for biochemistry. Samples are taken in laboratory conditions:
- spironolactone with the administration of Spironolactone for 3 days or Captopril to determine the rhythm of aldosterone at rest or when walking in patients;
- with the administration of Dox (10 mg) every 12 hours for 3 days;
- PCR tests for suspected familial form of pathology;
- ECG;
- duplex scanning of blood vessels;
- angiography.
Patients are redirected to a neurologist or cardiologist. If a familial form of pathology is suspected, a genetic examination is performed.
Additional measures to identify the location of the source of the disease:
- MRI for suspected adenoma;
- CT to detect aldosterone-producing adenoma;
- adrenal scintigraphy as an informative method for adenoma, large nodular hyperplasia;
- venography to study the concentration of renin and aldosterone.
Symptoms
Symptoms of the secondary type of this endocrine disease are nonspecific, since the clinical picture will largely depend on the underlying factor.
In general, the symptoms of aldosteronism are as follows:
- Due to fluid retention in the body, swelling appears, which in the initial stages of the development of the disease is insignificant and is present only in the morning. However, as the disease worsens, swelling is permanent.
- Muscle weakness. In the later stages of pathology development, the patient is practically immobilized.
- Fatigue even with full and long rest.
- Increasing malaise.
- High blood pressure, which does not stabilize even after taking medications of the appropriate spectrum of action.
- Headaches, dizziness.
- Constant feeling of thirst.
- Frequent urination, especially at night.
- For short periods of time, paralysis of the limbs, numbness of certain parts of the body. Also, from time to time the patient may feel tingling in the fingers.
- Deterioration of vision.
- Yellowness of the skin.
- Acute heart pain, and during diagnosis an enlargement of the ventricles of the heart will be detected.
- Convulsive attacks.
As the disease progresses, symptoms will appear more frequently and more severely.
It is important to understand that recovery is only possible if treatment is started in a timely manner. The occurrence of such symptoms requires immediate medical attention.
Treatment
The treatment regimen is drawn up based on the reasons that caused the increase in aldosterone levels in the adrenal glands. If the pathology is not aggravated and surges in blood pressure are caused by Conn's syndrome, then the basis of therapy is medications. If after completing a course of therapy there is no improvement, then perhaps an endocrinologist will suggest surgical intervention. The main goal of the intervention, if primary hyperaldosteronism is established, is to prevent the development of a hypertensive crisis and the manifestation of complications from neighboring organs (heart, kidneys, liver).
When a patient is diagnosed with hypothyroidism of the thyroid gland, regardless of the identified form of hyperaldosteronism, the mandatory treatment program includes a gentle diet including foods rich in potassium. The use of table salt will need to be limited.
Detection of elevated testosterone levels in women must be stabilized with hormonal agents. If congestion in the kidneys is observed, then use potassium supplements.
Features of treatment:
- stabilization of pressure indicators;
- restoration of water-salt balance.
REFERENCE! Surgical correction is inevitable in case of ineffective use of potassium-containing diuretics. For Liddle syndrome or a tumor-like tumor in the adrenal glands, the best treatment option is transplantation of the diseased kidney.
Drug treatment
Conservative therapy for hyperaldosteronism includes the following medications:
- diuretics ( Spironolactone, Amiloride );
- glucocorticoids ( Hydrocortisone, Dexamethasone ) to eliminate signs of metabolism and normalize blood pressure;
- ACE inhibitors in case of diagnosis of bilateral adrenal hypoplasia;
- calcium channel antagonists;
- diuretic potassium-sparing drugs (injections) to restore potassium levels in the body.
Treatment for secondary hyperaldosteronism is symptomatic. If blood pressure fluctuates, patients are advised to take cardiovascular medications to normalize them. If the level of potassium in the blood predominates, then drugs to stabilize the levels are Triamterene .
When a glucocorticoid-dependent form of pathology is detected, the basis of treatment is prescribed Dexamethasone and diuretics (Spironolactone) with an antiandrogenic effect, a dose of 150-200 mg per day.
REFERENCE! Many drugs cause side effects. In men - the development of gynecomastia and decreased libido, in women - the manifestation of menstrual disorders. Doses are selected exclusively by the attending physician. Possible combinations are beta-blockers + calcium antagonists or the administration of Spironolactone in small doses.
Surgery
Surgery for this disease, in particular Conn's syndrome, can prolong patients' life by almost 5-6 times, and prevent the development of complications from target organs (heart, kidneys, brain and fundus vessels). This is the best therapeutic option, especially if medications in advanced cases become powerless, and the tumor has reached a large size and compresses peripheral vessels in nearby organs.
Surgical intervention is a tough method, therefore, before removing tumors in the adrenal glands, a number of preparatory procedures are supposed to be carried out. It is important for patients:
- stop eating carcinogenic, fatty, fried, salty foods for 3-4 days;
- give an enema in the evening to cleanse the intestines;
- take a laxative.
The main methods of surgical intervention, taking into account the weight, age, and concomitant diseases of patients:
- The traditional option involves opening the peritoneal cavity and excision of the tumor along with metastases.
- Laparoscopy is a low-traumatic method by introducing a laparoscope through a small puncture into the walls of the peritoneum to remove the affected lesion.
- Adrenalectomy to remove the adrenal gland if a bilateral hyperplastic form of pathology is detected, followed by hypokalemia.
- Stenting of the focal artery
- Endovascular balloon dilatation.
If adrenal hyperplasia is detected, then it is possible to carry out bilateral removal of the organ with subsequent restoration of the normal concentration of potassium in the blood, prescribing in addition medications - Spironolactone, Amiloride, Aminoglutethimide , but in excessive doses.
After surgery, patients are advised to undergo replacement therapy with intravenous administration of Hydrocortisone (30-40 mg) every 6-8 hours
On a note! Not every form of hyperaldosteronism is amenable to surgery to remove the affected adrenal gland. For example, for bilateral hyperplasia, surgery is prescribed only if medications are ineffective. In case of carcinoma, additional chemotherapy cannot be avoided.
If the form of the disease is glucocorticoid-dependent, then surgery is not performed. The main goal is for patients to follow clinical recommendations to normalize blood pressure using Dexamethasone administered intravenously. The course of treatment is 1 month. Next - a recovery period of up to 5 days under the strict guidance of an endocrinologist with measurements of aldosterone and renin by donating blood.
In order to restore the activation of the body's defenses and support the immune system, all patients are additionally prescribed:
- physiotherapy after surgery, which has proven highly effective in combination with medications to enhance regenerative processes in tissues and provide a stimulating (anti-inflammatory) effect;
- UHF with the effect of heat on the body at different temperatures to form the body’s resistance to infectious diseases;
- electrophoresis with the influence of different voltage frequencies to stimulate the functions of the nervous system, stabilize the production of necessary hormones by the endocrine glands, and normalize the water-electrolyte balance;
- magnetotherapy with the influence of frequency alternating current on the composition of cells and tissues to stabilize the liquid medium with a sedative, antispasmodic effect;
- ultrasound with a beneficial effect on tissues and cellular structures.
In the secondary form of pathology, the development of therapy as such is not carried out. It is important to direct measures to eliminate provoking factors and the underlying disease.
The occurrence of the disease Hyperaldosteronism secondary
Secondary hyperaldosteronism is observed when:
- heart failure,
- liver cirrhosis,
- chronic nephritis (promotes the development of edema).
The rate of aldosterone production in patients with secondary aldosteronism is often higher than in patients with primary aldosteronism.
Secondary aldosteronism is usually combined with the rapid development of hypertension or occurs as a result of edematous conditions. During pregnancy, secondary aldosteronism is a normal physiological response to estrogen-induced increases in blood renin substrate levels and plasma renin activity.
In hypertensive conditions, secondary aldosteronism develops as a result of primary hyperproduction of renin (primary reninism) or due to its hyperproduction, which is caused by a decrease in renal blood flow or renal perfusion pressure. Secondary renin hypersecretion results from narrowing of one or both main renal arteries caused by atherosclerotic plaque or fibromuscular hyperplasia.
Overproduction of renin by both kidneys occurs with severe arteriolar nephrosclerosis (malignant hypertension) or due to narrowing of the deep renal vessels (acceleration phase of hypertension).
Alternative methods at home
If the disease is mild, and also after surgery, with the permission of the attending physician, alternative folk methods for a beneficial effect on the structures of the tissues (cells) of the thyroid gland can be used to help. Homemade recipes will help:
- stabilization of blood pressure levels;
- restoration of hormonal levels;
- have a positive effect on the adrenal glands;
- improving blood supply;
- regeneration processes in cells and tissues of the adrenal gland.
Best remedies:
- fresh burdock, crush the leaves in a blender, add water (3 cups), leave, take 1/4 cup 2 times a day;
- medicinal lungwort (30g) pour boiled water (1 l), leave, take 1-2 tbsp. before meals 3 times a day;
- geranium (leaves), 2-3 pcs. grind into a paste, pour boiling water (1 cup), take 1/3 cup 2 times a day.
Nutrition and supplements
Patients are prescribed a salt-free diet with the inclusion of foods rich in potassium in the diet:
- prunes;
- beans;
- beans;
- pine nuts;
- mustard;
- raisin;
- dried apricots;
- sea kale.
It is important to limit salt intake and exclude spicy, fatty and specific foods from the diet.
Herbs
To reduce the severe symptoms of the disease and stabilize overall well-being, you can use infusions and decoctions of medicinal herbs: lungwort, geranium, fresh burdock .
With hyperaldosteronism, high synthesis of aldosterone in the blood is observed. If there are suspicions of dysfunction of the thyroid gland, then, of course, you should not hesitate to contact an endocrinologist; it is necessary to undergo diagnosis at an early stage of the disease.
Diagnosis of the condition
Examination of patients is aimed at confirming the diagnosis and identifying the cause of hyperaldosteronism. For this purpose they prescribe:
- blood test - increased aldosterone, sodium and low renin, potassium;
- urine analysis - low density, increased excretion of potassium salts and aldosterone;
- Ultrasound of the adrenal glands is necessary to detect adenoma or hyperplasia, cancer;
- tomography (CT or MRI), scintigraphy of the adrenal glands with questionable ultrasound data;
- selective venography with the study of aldosterone in the venous blood of the adrenal glands.
Ultrasound of the adrenal glands
Prognosis for patients
Hyperaldosteronism is a progressive disease. May lead to serious consequences:
- decreased vision up to complete blindness;
- diabetes;
- cardiac ischemia;
- paresthesia;
- arterial hypertension;
- oncology;
- hypertrophy of the left ventricle, heart;
- bilateral hyperplasia of the adrenal cortex.
If the secondary form of pathology often goes away on its own, you just need to recover from the underlying disease, but with the primary form, the prognosis is ambiguous. It will directly depend on the degree of damage to important systems: urinary, cardiovascular and the severity of the underlying disease.
The prognosis is unfavorable for adrenal cancer, carcinoma. Adenoma is considered a benign tumor. Successfully treated with chemotherapy. The main thing for patients is not to let the pathology progress, not to start the process. If metastases are detected, then you can hardly count on a long life without constantly painful symptoms, because a severely damaged adrenal gland practically does not recover. In case of diffuse nodular hyperplasia, in order to achieve long-term stable remission, patients must be constantly examined by doctors and treated with drugs: steroidogenesis inhibitors, Spironolactone.
Causes
Its true distribution is difficult to assess, since there is evidence that in a certain percentage of patients with hypertension and the basis of the disease is primary hyperaldosteronism.
In more than 85% of patients, the morphological substrate of primary hyperaldosteronism is tumors of the adrenal cortex - aldosteromas. The rest have bilateral adrenal hyperplasia.
A characteristic feature of aldosterone is the production of aldosterone, regardless of the stimulating effect of the reninangiotensin system. An increase in the concentration of aldosterone in the blood leads to a decrease in the production of renin by the juxtaglomerular apparatus of the kidneys, a decrease in the content of renin and angiotensin II in the blood. At the same time, some patients showed a decrease in aldosterone production by the tumor when dexamethasone was administered and an increase in aldosterone production under the influence of potassium load. This indicates that the functional “autonomy” of the aldoster may be incomplete, affecting only regulatory relationships with the juxtaglomerular apparatus of the kidneys.
Tumors of the adrenal cortex are predominantly benign, although aldosterone-producing adrenal cancer has been observed in rare cases. Approximately 9/10 aldosteromas are unilateral, solitary tumors, but multiple and bilateral adenomas also occur. The tumors are enclosed in a connective tissue capsule and appear yellow or orange when cut. The size of aldosteromas is usually small, the diameter for the most part does not exceed 4 cm, although there are also large tumors. The histological structure of aldosterae is heterogeneous - the cells of some tumors are similar to the cells of the zona fasciculata, others - to the reticularis or glomerulosa. The second adrenal gland in patients with aldosteroma may be unchanged, but in some cases, when the tumor produces corticosterone and cortisol along with aldosterone, atrophy of the second adrenal gland is observed. In rare cases of primary aldosteronism with bilateral adrenal hyperplasia, there was thickening of the zona glomerulosa.
Principles of treatment of secondary hyperaldosteronism
The goal of treatment is to eliminate and minimize the manifestations of the underlying disease.
To normalize potassium levels in the body, the patient is recommended to follow a low-salt diet with limited sodium-containing foods.
The main treatment is symptomatic. It is carried out using the following medications:
- Spironolactone. Recommended for the correction of electrolyte disturbances.
- Asparkam. Prescribed in addition to diuretics to restore potassium levels.
- Triamterene. It is a potassium-sparing diuretic used when potassium levels are normal in the setting of hyperaldosteronism.