What is adrenal neuroblastoma
The average age of development of adrenal neuroblastoma is 2-3 years, accounting for 14% of all cancers in children.
The danger is a rapid deterioration of the general condition, an aggressive effect on the body, causing the formation of metastases in the circulatory system with damage to the lymph nodes, internal organs, and bone marrow. Every third cancer diagnosed in a child is adrenal neuroblastoma. More often girls get it. 75% of cases of this type of cancer are detected in children under the age of five.
Experts can already detect a tumor in the adrenal gland as a result of screening in the second and third trimester of pregnancy. The disease actively manifests itself at an early age in pathological conditions in not fully mature nerve cells that mutate and subsequently divide into tumor-like formations.
Cases where adrenal neuroblastoma disappears on its own are rarely encountered in medical practice. The disease develops quickly and aggressively, occupying a large area in the retroperitoneal space.
Fetal neuroblastoma. Possibilities of prenatal diagnostics and prognosis
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
Introduction
Fetal neuroblastoma is a tumor arising from undifferentiated neural tissue of the adrenal glands in the retroperitoneum or from sympathetic ganglia in the abdomen, chest, pelvis, head and neck. More than 90% of neuroblastomas in fetuses arise in the adrenal glands [1]. It is one of the most common extracranial tumors of childhood, occurring in 1:10,000 to 1:30,000 live births [2, 3]. Neuroblastomas account for 50% of all tumors in the first year of life [4]. At the same time, malignant tumors of the adrenal glands in children occupy the third place in frequency after leukemia and tumors of the central nervous system, accounting for 8-10% of all malignant diseases in children, causing 15% of deaths from cancer in the pediatric population. The etiology of neuroblastomas is unclear, with most cases occurring sporadically.
Usually the lesion is isolated, involving one adrenal gland; bilateral lesions are rare [5]. Sometimes antenatal metastases appear in the liver, skin, bone marrow and rarely in the placental villi [6]. In this case, the placenta looks voluminous, but metastatic foci may not be detected macroscopically and are diagnosed only by histological examination. Placental villous vessels contain clusters of neuroblastoma cells, but stromal invasion is extremely rare [7]. Cases of metastasis to the umbilical cord with subsequent fetal death have been described [8]. Neuroblastomas are predominantly composed of neuroblasts. Macroscopically, the tumor foci are well defined, but can infiltrate surrounding tissues; there is no capsule.
A combination of neuroblastomas with various conditions is known, in particular with Hirschsprung disease, fetal alcohol syndrome, DiGeorge syndrome, Von Recklinhausen disease, Beckwith-Wiedemann syndrome.
An early case of diagnosis of neuroblastoma at 19 weeks of gestation has been described in the literature, but usually prenatal diagnosis is made by ultrasound examination between 26 and 39 weeks of gestation [8].
The first report on prenatal diagnosis of neuroblastoma dates back to 1983 [9]. The ultrasound picture depends on the size, location and secretory activity of the tumor. Neuroblastomas are often not diagnosed prenatally due to their small size. During ultrasound examination, neuroblastoma is visualized as a formation located retroperitoneally, between the kidney and the diaphragm, displacing the kidney downward and laterally. Its structure is mixed, with solid and cystic components [10, 11]. In large lesions, degenerative signs can be detected: cystic changes, hemorrhages, calcifications [11, 12]. Hydronephrosis and polyhydramnios, as well as fetal hydrops, sometimes occur.
Anterior displacement of the inferior vena cava by a visualized mass should be regarded as a sign of the retroperitoneal origin of this mass [13]. In addition, if the adrenal tumor is large, it can displace surrounding organs.
Color Doppler mapping helps to identify the tumor-supplying vessel arising directly from the aorta, but such a single vessel may not be visualized [13].
As a rule, antenatal diagnosis of metastases is extremely rare, since no specific lesions of the placenta are noted during ultrasound examination; only nonspecific thickening is described [14]. Fetal MRI can be informative in diagnosing metastases.
Hemorrhagic adrenal tumors may be complicated by fetal anemia, nonimmune hydrops fetalis, or massive liver invasion [10]. Various explanations for the etiology of hydrops fetalis have been proposed: excess production of catecholamines, leading to hypertension and heart failure in the fetus; involvement of the liver in the pathological process, causing impaired venous return and the development of hypoproteinemia [14]; invasion of erythropoietic tissue by tumor cells, leading to the development of severe anemia or even hypersecretion of aldosterone by the adrenal cortex. In addition, the occurrence of hydrops fetalis secondary to the appearance of metastases in the placenta has been described. Placental edema due to the mechanical effect of a large mass may develop in some cases of neuroblastoma without metastasis to the placenta [6].
In addition, large adrenal tumors can lead to dystocia during labor [8].
Maternal complications should also be kept in mind. Very rarely, overproduction of catecholamines by a tumor of the fetal adrenal gland can cause excessive sweating, the development of hypertension and preeclampsia in the mother, and maternal mirror syndrome when the placenta is damaged [12, 14, 15]. In addition, the development of such maternal complications is usually associated with a high rate of neonatal mortality, reaching 70% [1].
Sonographic staging of the tumor process in the fetus is difficult, but there are reports that in the absence of symptoms of preeclampsia in the mother, the risk of a widely disseminated process is low [8].
The prognosis for neuroblastoma depends on the time of diagnosis, the location of the primary lesion and the stage of the disease. The prognosis is better in children under 1 year of age with low stages of the tumor (about 90% survive) [16]. For neuroblastoma diagnosed prenatally, the prognosis is usually favorable, with 90-96% of children surviving [1]. However, if the placenta is affected, the prognosis is unfavorable; antenatal fetal death or the death of the child soon after birth often occurs [12, 14].
Detection of calcifications in the tumor by ultrasound is associated with a better prognosis, probably due to the fact that calcifications are evidence of tumor necrosis that has occurred [12].
Neuroblastoma in situ may not manifest itself clinically and may even undergo spontaneous regression [17, 18].
The course of the disease in patients with neuroblastoma diagnosed prenatally is usually favorable, especially with isolated damage to the adrenal glands [8]. The treatment method (with good results) is surgical removal of the tumor immediately after birth [19], chemotherapy is indicated only in cases of significant progression of the disease [20]. Patients with “favorable” signs of the disease (small tumor size, its cystic structure, lack of progression) should be carefully observed and undergo surgical treatment only if there is no regression of the tumor [11].
Materials and methods
As an illustration, we present one of our clinical observations.
Clinical observation
Patient T., 40 years old, applied for a routine screening ultrasound examination at 32 weeks. In previous studies, no pathology was detected at 13 and 19 weeks.
The spouses are healthy and have no occupational hazards. Heredity is not burdened. This is my fifth pregnancy. There is a history of two normal births, two medical abortions. The patient was registered with the antenatal clinic from 6 weeks. The pregnancy proceeded without significant complications. Only at 6-7 weeks was the threat of miscarriage diagnosed.
Ultrasound examination was carried out using a SonoAce-X8 ultrasound scanner (Medison).
results
Ultrasound examination revealed one living male fetus. The gestational age was 31 weeks 4 days. Fetometric indicators corresponded to this period, with the exception of abdominal circumference exceeding the 95th percentile due to hepatomegaly. No disturbances in feto-placental blood flow were detected. No pathological changes in the placenta and amniotic fluid were noted.
Under the diaphragm on the right, a hyperechoic tumor-like formation of a somewhat heterogeneous solid structure, with clear, even contours, measuring 50x38x35 mm was visualized. Adjacent to the lower pole of this formation was the right kidney, which had normal size, shape and structure. The inferior vena cava was displaced anteriorly and to the left. Severe hepatomegaly was noteworthy, and the structure of the liver was not homogeneous. It contained multiple hyperechoic inclusions measuring up to 17 mm, surrounded by a thin hypoechoic peripheral rim. Color Doppler imaging (CDC) demonstrated intense peripheral vascularization of the tumor (Fig. 1-3).
Rice. 1.
Neuroblastoma of the right fetal adrenal gland. Pregnancy 31 weeks 4 days.
Rice. 2.
Blood flow in fetal neuroblastoma. Color Doppler mapping. The feeding vessel is clearly visible, enveloping the formation along its periphery. The intact fetal kidney is adjacent to the lower pole of the formation.
Rice. 3.
Metastases in the fetal liver. Cross section of the fetal abdominal cavity. Hepatomegaly. In the structure of the fetal liver, round inclusions of slightly increased echogenicity (arrows) are determined, with a hypoechoic rim - metastases.
The diagnosis was made: pregnancy 31 weeks 4 days. Tumor of the fetal right adrenal gland with metastases to the liver. Dynamic ultrasound monitoring of the growth rate of the tumor and the occurrence of possible complications is recommended.
At 32 weeks 4 days, antenatal fetal death was diagnosed. A stillborn child was born, male, weighing 2480 g, length 45 cm.
Discussion
In the presented observation, the picture of adrenal neuroblastoma was not quite classical. The fact that this is a suprarenal formation is obvious, since it was adjacent to the kidney, which had a normal shape, size and structure. The tumor had a capsule and a homogeneous hyperechoic structure, which is not typical for adrenal neuroblastoma. Therefore, differential diagnosis was carried out with hemorrhage into the adrenal glands, Wilms tumor, extralobar pulmonary sequestration, and retroperitoneal teratoma.
Hemorrhage into the adrenal glands, as a rule, looks like an echogenic or heterogeneous formation; sometimes it can be completely anechoic and is characterized by a change in the ultrasound picture during dynamic examination, gradually turning into an anechoic cystic formation, in which, over time, thickening of its wall is noted [13] and calcifications are formed. . Power Doppler demonstrates the complete avascularity of such a formation. In our case, the formation had increased echogenicity and a somewhat heterogeneous structure. During CDB, predominantly peripheral blood flow was recorded in the tumor.
Wilms tumor affects the kidney (usually the right one), which in the presented case was intact.
Extralobar pulmonary sequestration is a predominantly left-sided suprarenal formation with a clear outer contour, usually a hyperechoic, homogeneous structure of irregular shape. This pathology is detected already in the second trimester of pregnancy, with color circulation the feeding vessel is determined.
Teratomas (including retroperitoneal localization) are always represented by formations of a heterogeneous solid-cystic structure due to their histological structure.
Thus, the formation we discovered was attributed to an adrenal tumor even in the absence of the classic picture of neuroblastoma. The large size of the tumor and the absence of significant complications such as polyhydramnios, congestive heart failure, and impaired feto-placental blood flow were noteworthy. At the same time, the relatively early manifestation (detection of this complex of changes as early as 31 weeks), the not entirely typical ultrasound morphology of the tumor, the presence of severe hepatomegaly and multiple metastases allowed us to conclude that the disease was malignant, which apparently caused the antenatal death of the fetus. As a result, the diagnosis was confirmed by pathomorphological examination. In a premature male fetus, the abdomen is enlarged. On the right, in the retroperitoneal space, a round formation (tumor) measuring 50×35×30 mm and elastic consistency is detected. A kidney is adjacent to the tumor in front and below, tightly fused to it. The tumor comes from the right adrenal gland, which is located on its upper pole in the form of a “cap”. On section, the tumor is homogeneous, yellowish-gray. The left adrenal glands and kidney are of normal appearance. The liver is significantly enlarged, occupies about 1/2 of the volume of the abdominal cavity, the lobes are not clearly differentiated. The surface of the liver is brownish-red. The sections reveal multiple dense elastic nodes with a diameter of up to 15 mm of pale yellow color (Fig. 4, 5).
Rice. 4.
Organocomplex, front view. 1 - liver; 2 - tumor with the right adrenal gland; 3 - heart.
Rice. 5.
Organocomplex, rear view. 1 - tumor with the right adrenal gland; 2 - right kidney; 3 - left adrenal gland; 4 - left kidney; 5 - liver; 6 - metastases to the lungs.
On the visceral pleura, multiple yellow lesions with a diameter of up to 4 mm and a thickness of less than 1 mm are detected. The lung tissue is airless, flabby, without visible focal changes.
On microscopic examination, the tumor consists of small monomorphic cells with round hyperchromic nuclei and a narrow rim of cytoplasm. Nucleoli are well defined in the nuclei; mitotic figures are few in number. The cells predominantly form solid growth fields. A neuropil is defined between the cells. Any characteristic structures in the tumor cannot be traced, possibly due to autolytic changes (Fig. 6).
Rice. 6.
Microscopic specimen of fetal adrenal neuroblastoma. Small monomorphic cells with round hyperchromic nuclei and a narrow rim of cytoplasm. Hematoxylin and eosin staining, x200.
In all parts of the liver, the growth of a tumor is determined, similar in structure to the tumor emanating from the adrenal gland.
Liver tissue is almost undetectable—autolysis is pronounced.
Autolytic changes are also evident in the lung tissue. Several small foci of tumor growth are detected both in the lung tissue and in the pleura.
Based on macroscopic and microscopic examination, a pathological diagnosis was made: neuroblastoma of the right adrenal gland with metastases to the liver and lungs.
conclusions
Diagnosis of any tumor is possible, since it is easy to detect a space-occupying formation. However, most neuroblastomas are diagnosed only in the third trimester of pregnancy, which indicates the importance of this screening period. Most neuroblastomas detected prenatally belong to stage 1 of the disease and, in the absence of complications and early surgical treatment of newborns, have a favorable prognosis. In our case, the rapid progression of neuroblastoma and metastasis caused an unfavorable outcome. The presented case demonstrates that adrenal neuroblastoma can be classified as a group of congenital pathologies with an ambiguous prognosis. If fetal neuroblastoma is detected, dynamic ultrasound monitoring should be performed. However, if a large neuroblastoma is detected, with the presence of metastases, even in the absence of other visible complications, early delivery should be recommended, and in this case, a cesarean section would be more careful.
Literature
- Woodward PJ, Sohaey R., Kennedy A., Koeller KK A comprehensive review of fetal tumors with pathologic correlation // RadioGraphics. 2005. V. 25. P. 215-242.
- Moore S., Satge D., Sasco A., Zimmermann A., Plaschkes J. The epidemiology of neonatal tumors. Report of an international working group // Pediatr. Surg. Int. 2003. N 19. P. 509-519.
- Sandrasegaran K., Lall C., Aisen A. Fetal magnetic resonance imaging // Curr. Opin. Obstet. Gynecol. 2006. N 18. P. 605-612.
- Castel V., Grau E., Noguera R., Martinez F. Molecular biology of neuroblastoma // Clin. Transl. Oncol. 2007. V. 9. N 8. P. 478-483.
- Papathanasiou N., Gaze M., Sullivan K. et al. 18F-FDG PET/CT and 123I-Metaiodobenzylguanidine Imaging in High-Risk Neuroblastoma: Diagnostic Comparison and Survival Analysis // J. Nucl. Med. 2011. V. 52. N 4. P. 519-25.
- Fox H., Sebire N. Pathology of the Placenta (3rd edn). Saunders: London, 2007. 576 p.
- Perkins D., Kopp C., Haust M. Placental infiltration in congenital neuroblastoma: a case study with ultrastructure // Histopathology. 1980. V. 4. P. 383-389.
- Jennings R., LaQuaglia M., Leong K. et al. Fetal neuroblastoma: prenatal diagnosis and natural history // J. Pediatr. Surg. 1993. V. 28. N 9. P. 1168-74.
- Fenart D., Deville A., Donzeau M., Bruneton J. Neuroblastomer.etrop.eritoneal diagnostiqu.e in utero. A propos d`un cas.// J. Radiol. 1983. N 64. P. 359-361.
- Heling K., Chaoui R., Hartung J. et al. Prenatal diagnosis of congenital neuroblastoma. Analysis of 4 cases and review of the literature // Fetal Diagn. Ther. 1999. N 14. P. 47-52.
- Soo-Hyun Lee, Jeong Yeon Cho, Mi Jin Song et al. Prenatal Ultrasound Findings of Fetal Neoplasms // Korean J. Radiol. 2002. V. 3. N 1. P. 64-73.
- Sebire NJ, Jauniaux E. Fetal and placental malignancies: prenatal diagnosis and management // Ultrasound Obstet. Gynecol 2009. V. 33. P. 235-244.
- Tihonenko I., Jeanty Ph. Fetal tumors. DVD, 2010.
- Allen A., Dress A., Moore W. Mirror syndrome resulting from metastatic congenital neuroblastoma // Int. J. Gynecol. Pathol. 2007. N 26. P. 310-312.
- Acharya S., Jayabose S., Kogan S. et al. Prenatally diagnosed neuroblastoma // Cancer 1997. N 80. P. 304-310.
- Grosfeld J., Rescorla F., West K., Goldman J. Neuroblastoma in the first year of life: clinical and biological factors influencing outcome // Semin. Pediatr. Surg. 1993. N 2. P. 37-43.
- Granata C., Fagnani A., Gambini C. et al. Features and outcome of neuroblastoma detected before birth // J. Pediatr. Surg. 2000. N 35. P. 88-91.
- Sofka C., Semelka R., Kelekis N. et al. Magnetic resonance imaging of neuroblastoma using current techniques // Magn. Reason. Imaging. 1999. V. 17. N 2. P. 193-198.
- Kamil D., Tepelmann J., Berg C. et al. Spectrum and outcome of prenatally diagnosed fetal tumors // Ultrasound Obstet. Gynecol. 2008. N 31. P. 296-302.
- Ho P., Estroff J., Kozakewich H. et al. Prenatal detection of neuroblastoma: a ten-year experience from the Dana-Farber Cancer Institute and Children's Hospital // Pediatrics. 1993. V. 92. N 3. P. 358-64.
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
Diagnostic measures
Identifying the stage of a neoplasm requires a comprehensive examination.
Effective treatment is possible with early detection of the pathology. In this regard, it is of great importance that parents and their children seek medical help in a timely manner. To detect a tumor focus, methods such as ultrasound of the abdominal and thoracic cavity, radiography, computer and magnetic resonance imaging are used. If neuroblastoma is located in brain structures, electroencephalography may be performed.
The main method for detecting a tumor is a biopsy of the tumor followed by morphological examination. The doctor studies the structure of the tumor tissue and determines the degree of its differentiation.
Types of pathology
There are several types of hyperplasia, it all depends on which part of the adrenal gland is involved in the enlargement process. Enlargement of the adrenal glands can be nodular, diffuse, nodular, micronodular. Below is more detail about each type.
Nodular enlargement of the adrenal glands
With this type of hyperplasia, the formation of one or more nodular formations is observed. There is an expansion of lobular nodes up to 4 cm. This form of the pathological process is observed in 40% of patients in whom an enlarged adrenal gland was detected.
Nodular hyperplasia is considered the most common form of adrenal enlargement
Nodular hyperplasia can form on both the right and left adrenal glands, and can also be bilateral. Simply put, during diagnostic manipulations, the enlargement process will be observed from one gland or from two at once. As soon as this diagnosis has been made, it is necessary to urgently begin treatment measures.
According to statistical data, most often this form of the pathological process occurs in older people and belongs to the hereditary category. Symptoms of the disease include:
- convulsive episodes, muscle weakness;
- caries, which is difficult to treat;
- frequent headaches;
- obesity;
- disorders of the urinary system;
- mental disorders;
- rapid hair growth;
- small tumors and rashes on the skin;
- diabetes.
Diffuse enlargement of the adrenal glands
In the diffuse form of hyperplasia, the shape of the adrenal glands remains unchanged, but they are proportionally enlarged. Typically, this type of pathological process is combined with nodular enlargement and can only be detected using magnetic resonance imaging. Ultrasound diagnostics for diffuse enlargement is not prescribed, as it is not very informative.
To determine pathological enlargement of the endocrine glands, it is best to use MRI
Clinical manifestations of the pathological process may not appear for a long time. For each patient, a specific treatment regimen with medications is selected that must be taken for life. Medicines belong to the group of sex hormone substitutes. With constant use of hormonal drugs, it is not difficult for a woman to become pregnant and give birth to a healthy child.
The main features include:
- dystrophic disorders;
- excess weight;
- abnormal menstruation;
- reproductive dysfunction;
- panic attacks;
- in men, testicles shrink;
- fast fatiguability;
- painful sensations behind the sternum;
- muscle spasms;
- an irresistible feeling of thirst.
Nodular enlargement of the adrenal glands
Nodular hyperplasia has a second name - focal nodular hyperplasia. The characteristic features of this process are that hepatocytes (cellular structures of the liver) begin to increase in volume, and as a result, deviations from the norm and vascular changes are formed. There is no consensus among experts for what reasons and what leads to the development of this pathological process.
But there is an assumption that this is somehow connected with disorders in the vascular system, or changes begin with the incorrect use of hormonal drugs. To diagnose the disease, magnetic resonance and computed tomography, as well as ultrasound methods are used. In addition, if nodular hyperplasia is suspected, renal material must be taken (biopsy).
A biopsy is prescribed for patients in whom nodular adrenal enlargement is suspected
Most often, nodular focal enlargement of the endocrine glands is observed in young children and adolescents; it is rare at older ages. Early diagnosis and timely treatment increase the chances of a full recovery. The clinical picture consists of the following symptoms:
- muscle atrophy in the lower extremities;
- emotional instability, drowsiness;
- the skin on the face turns purple or marbled;
- obesity in the chest, face, abdomen and neck;
- male pattern hair growth;
- diabetes;
- heart rhythm disturbances;
- painful sensations in the bones.
Micronodular enlargement of the adrenal glands
Micronodular enlargement of the endocrine glands develops with prolonged influence of the adrenocorticotropic hormone on the paired organ. This, in turn, leads to the development of adrenal adenoma. Unfortunately, very often, doctors make the wrong diagnosis and confuse this pathology with a tumor formation.
Morbidity
It is detected mainly in the second and third stages during a comprehensive examination of the child. In newborns, the disease is practically asymptomatic.
Doctors detect a tumor by chance during an ultrasound, x-ray examination, or with completely other pathologies. The tumor grows rapidly, affecting the spinal cord in a short period of time.
Neuroblastoma occurs rarely in the fetus. A specialist can determine it during an ultrasound examination in the second and third trimester.
The earliest detection was dated to the 26th week of pregnancy. In an unborn child, the tumor formation is concentrated on one side, so doctors cannot make any predictions until the moment of birth. The tumor may progress in size and may also disappear completely without any medical intervention.
Prognosis and life expectancy
At the initial stages of development, adrenal neuroblastoma in children is treatable in all cases. Stage 3, with proper treatment, has a favorable prognosis - more than 65% of sick children successfully got rid of the tumor. Life expectancy after complete recovery also has a favorable prognosis - the child can fully develop and live for many years. Stage 4S is successfully overcome by the child’s body in 75% of cases. When diagnosed with stage 4 neuroblastoma, the prognosis is disappointing - no more than 20% of children live longer than 5 years after treatment.
Treatment methods
A treatment plan is developed for each child individually, depending on the symptoms present, the stage of development of the tumor and its location. Chemotherapy drugs, radiation, or surgery may be used. In addition, symptomatic treatment is prescribed, aimed at eliminating individual clinical manifestations.
Surgeries allow you to completely remove the tumor focus. They are performed at the first or second stage of neuroblastoma. In the presence of metastases or localization of the tumor in the deep structures of the brain, surgical intervention is ineffective. Chemotherapy may be used before and after surgery.
The choice of treatment modalities influences survival. In this regard, treatment measures are chosen by the oncologist after examining the child.
Chemotherapy drugs are a class of drugs that target tumor cells. Healthy tissues are not sensitive to them, but during long-term therapy they are also damaged by chemotherapy.
Radiation therapy is based on the ability of ionizing radiation to suppress the division of tumor cells and lead to their destruction. Local effects are used, which reduces the likelihood of side effects and protects healthy tissue. Radiation therapy is the standard treatment for neuroblastoma located in the cerebellum, since surgery is not possible in this case.
Treatment of neoplasm
The most common ways to get rid of a tumor are surgery and chemotherapy. Radiation treatment in young children is used very limitedly, as unfavorable long-term results are noted.
Removal of the adrenal gland (unilateral adrenalectomy) together with neuroblastoma is performed at the first and second stages of the disease. If the tumor size approaches 10 cm, chemotherapy is preliminarily indicated. Vincristine, Doxorubicin, Cisplatin are used for it. Such medications help reduce tumors and reduce the risk of relapse after surgery.
At the third stage, preoperative administration of antitumor drugs is a mandatory stage of treatment.
At the fourth stage, if removal is possible after surgery, additional radiation is performed or drips with chemotherapy drugs are continued. Such massive administration of cytostatics causes inhibition of hematopoiesis.
Therefore, children are prescribed transfusions of donor blood and its components, and are given antibiotics and antifungal agents to prevent infectious complications. In some cases, a bone marrow transplant is recommended.
New treatments for neuroblastoma include:
- anti-relapse course of Roaccutane for 3 months. It helps turn remaining cells into differentiated ones;
- introduction of metaiodobenzylguanidine, which contains a radioactive isotope of iodine. Neuroblastoma selectively accumulates it;
- Immunotherapy is the use of monoclonal antibodies specific to tumor cells.
Causes
The main cause of adrenal neuroblastoma is a genetic mutation of cells that grow uncontrollably and penetrate vital organs. One of the risk factors is exposure to carcinogenic factors on the body.
The tumor grows in neuroblasts - fibers that are not fully formed during the period of intrauterine development of the fetus. Neuroblasts are then transformed into nerve fibers that form the adrenal glands.
The maturation of neuroblasts or their spontaneous resorption occurs in proportion to the growth of the newborn. Some neuroblasts mutate, which leads to the appearance of a malignant formation.
On this topic
The danger of Hürthle-Ashkenazi cells in the thyroid gland
Most researchers assume that modification of cells with the production of oncological neuroblasts occurs at the stage of intrauterine development and either progresses, forming a tumor, or disappears on its own.
One of the main risk factors is hereditary predisposition. If a close relative in your family had cancer in childhood, there is a high probability of “transmission” of the disease.
- The adrenal glands are not visualized on ultrasound. What does it mean?
The etiology of adrenal neuroblastoma in young children has not yet been identified. Doctors cannot draw any conclusions regarding the causes of the disease in the fetus in the embryonic stage.
Most often, the formation appears for no apparent reason; in rare cases, a hereditary connection becomes a factor contributing to the disease. The period of detection of cancer in children is in the first year of life.
The pathological process begins with defective maturation of embryonic cells as a result of their mutation. Despite the development of irreversible processes, nerve fibers continue to divide, forming a malignant formation in the adrenal gland.
A tumor that appears in the first year of a child’s life can resolve on its own, turning into a benign form and disappearing over time.
METABOLIC PATHOLOGY
CONGENITAL ADRENAL HYPERPLASIA
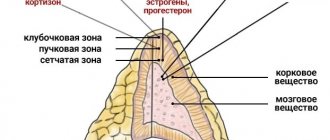
Congenital adrenal hyperplasias are a group of autosomal recessively inherited defects of adrenal enzymes. The enzyme deficiency is most often 21-hydroxylase, which converts 17-hydroxyprogesterone to 11-deoxycortisol. The consequences of this enzyme defect in the biochemical synthesis of cortisol lead to underdevelopment of the genitals in girls or salt-wasting crisis in newborns of either sex. The diagnosis is confirmed by the detection of elevated serum levels of 17-hydroxyprogesterone and karyotype examination. However, sonographic analysis of the adrenal glands also shows effectiveness in making a presumptive diagnosis, which may be useful while the official results are being prepared.
In the largest study to date, abnormal adrenal manifestations were identified in 92% of infants with untreated congenital adrenal hyperplasia. The most common sonographic finding is a lobulated, serrated, or cerebellar margin of the adrenal gland. Affected glands also often have increased echogenicity, with loss of a continuous central echogenic cortical stripe, which is replaced by a dotted echogenic pattern. In this case, the adrenal glands are, as a rule, enlarged (Fig. 23) with one transverse dimension of more than 4 mm.
Fig.23. Thickened adrenal margin (cross) in the case of congenital adrenal hyperplasia.
WOLMAN'S DISEASE
Wolman's disease (primary familial xanthomatosis) is caused by a deficiency of the enzyme acid lipase, which breaks down triglycerides and cholesterol esters. A defect in this enzyme consequently leads to increased levels of complex lipids, which are deposited in the liver, spleen, lymph nodes, adrenal cortex and intestines. It is an autosomal recessive disease that is a developmental disorder, organomegaly and muscle cachexia. Deposition of complex lipids in the adrenal glands can form fatty acid accumulations that eventually become calcified. The zona reticularis and internal fascicular layers become calcified, with preservation of the glomerular zone. The causes of adrenal calcification are shown in Box 1, but in Wolman's disease the calcification is bilateral and the glands retain their triangular configuration, allowing it to be distinguished from other causes.
| Box 1 Causes of adrenal calcification in children |
|
Diagnostics
If you suspect a child has neuroblastoma, you should immediately consult a doctor and undergo all necessary examination procedures. Diagnostic methods for detecting adrenal neuroblastoma:
- urine analysis for the presence of tumor markers and catecholamines;
- general and detailed blood test;
- radiography;
- ultrasonography;
- MRI;
- positron emission tomography;
- CT scan;
- biopsy of tumor tissue and bone marrow.
Primary diagnosis is carried out using urine and blood tests. If the suspicion of neuroblastoma is confirmed, additional studies are prescribed that make it possible to detect its location, the number of metastases, the size and nature of the tumor. Based on the test results, the doctor prescribes the necessary treatment procedure.
Return to contents
Diagnosis of adrenal tumors
Examination of patients with adrenal tumors, in addition to routine laboratory tests (general, biochemical blood tests, coagulogram, general urine test), should include tests aimed at identifying increased hormone production. To identify Cushing's syndrome, a dexamethasone test (1 mg) and determination of cortisol excretion in urine (24 hours) are used.
For hyperaldosteronism, the concentration and ratio of aldosterone and renin are assessed; during virilization - serum levels of adrenal androgens (androstenedione, dihydroepiandrosterone sulfate) and testosterone, as well as excretion of 17-ketosteroids in the urine (24 hours); during feminization - the concentration of estradiol and estrone in plasma. To exclude pheochromocytoma, it is necessary to assess the daily excretion of catecholamines (epinephrine, norepinephrine, dopamine) and their metabolites in the urine (especially metanephrine and normetanephrine), as well as the level of serum metanephrine and catecholamines.
Differential diagnosis of adrenal tumors is carried out with neuroblastoma and nephroblastoma in children and hamartomas, teratomas, neurofibromatosis, amyloidosis and adrenal granulomas in adults.
Symptoms
The initial stage of the disease does not manifest itself in any way. From time to time, ailments that occur in a child are perceived by doctors as symptoms of other health problems.
With progression, children develop local redness or bluish discoloration of individual areas of the skin, indicating the presence of metastases.
The main symptoms of adrenal neuroblastoma:
- Unreasonable increase in temperature.
- Constant feeling of fatigue.
- Frequent drowsiness.
- Increased sweating.
- Lump in the abdominal area.
- Enlarged lymph nodes.
- Loose stools.
- Sharp pain in the abdomen.
- Weight loss.
- Constant feeling of nausea.
- Poor appetite.
- Unpleasant sensations in the bones.
On this topic
How to prevent the development of adrenal glands
The resulting cancer cells promote the production of hormones, causing excessive pressure on the internal organs. A growing malignant formation in the peritoneum has a negative impact on the functioning of the entire gastrointestinal tract.
- What does an ultrasound scan of the adrenal glands show and how to properly prepare for the study?
Damage to the bone marrow by metastases leads to excessive fatigue, pain and weakness in the child. Even minor cuts and wounds lead to profuse, difficult-to-stop bleeding.
Symptoms of neuroblastoma of the right and left adrenal gland
The early stages of the tumor do not differ in the specificity of manifestations, which leads to the detection of the disease only during metastasis. A child with neuroblastoma may be moody, weak, and slowly gain weight. A third of patients experience elevated body temperature, significant weight loss, nausea, and vomiting. With intensive growth, the formation can be palpated in the form of a dense node.
The most typical symptoms are usually the spread of malignant cells to various organs and systems.
This results in:
- pain in the bones, lumbar region, abdomen;
- enlarged lymph nodes;
- protrusion of the liver from under the edge of the right costal arch, yellowing of the skin;
- decrease in the number of blood cells - anemia, increased bleeding, severe weakness, frequent infectious diseases;
- bluish or reddish skin nodules.
Due to the increased content of adrenaline, norepinephrine and dopamine (catecholamines in the medulla), children may experience attacks of high blood pressure. Both arterial and intracranial indicators increase. This is manifested by severe headache, pale skin, sweating, diarrhea, and rapid heartbeat.
Symptoms
As a rule, this disease in the initial stages of its development is practically not manifested by clinical factors, so the course of the disease can be attributed to other ailments. And only at the third stage the symptoms have the most pronounced signs.
- The child has an increase in temperature. It is accompanied by lethargy and rapid fatigue.
- Problems with the functioning of the gastrointestinal tract begin, with nausea and vomiting noted.
- The child loses appetite and weight.
- Increased sweating is noted.
- Blood clotting is reduced, so even a minor cut can lead to significant blood loss.
In addition to these signs, other symptoms should be noted. As the tumor grows, there are disturbances in the baby’s physical development, difficulty breathing, and pain throughout the body. There are also problems with urination and defecation, the swallowing process is disrupted, and swelling and numbness of the extremities are bothersome.
In the last stages of development, when metastasis of the body has begun, the lymph nodes and liver become significantly enlarged, hemorrhages appear on the skin, and compactions appear in the retroperitoneal region. They can be easily felt during palpation. This indicates that the disease is progressing and there is a danger of damage to the spinal cord.
Neuroblastoma is also dangerous and has serious complications: disruption of the musculoskeletal system, compression of the spinal cord and brain, resulting in paralysis, impaired brain activity, and the development of paraneoplastic syndrome.
How does a tumor manifest itself?
In the early stages, it is quite difficult to detect a tumor due to the absence of characteristic symptoms. Therefore, the tumor is perceived instead of other diseases characteristic of children. Signs appear at the location of the tumor or already during the period of metastasis. As a rule, the primary node is detected in the retroperitoneum, in the adrenal glands, and extremely rarely - in the neck or in the mediastinum.
Symptoms of the disease appear depending on the release of hormones by the cells of the neoplasm or its constant pressure on an organ located nearby. Tumor growth can affect the functioning of the excretory system: intestines and bladder. Compression of blood vessels leads to swelling of the scrotum or lower extremities.
Another sign is the appearance of reddish or bluish spots on the baby’s skin. They indicate that epidermal cells are being damaged. If the tumor penetrates the bone marrow, the child becomes weaker and often gets sick. Even a minor wound can cause extensive bleeding in the baby. These signs are a reason to immediately consult a doctor and undergo an examination.
Neuroblastoma of the retroperitoneum
Neuroblastoma, formed in the retroperitoneal space, is characterized by rapid development. Within a short period of time, the tumor penetrates into the spinal canal, where a dense neoplasm is formed, which is easily detected by palpation. At first it is asymptomatic, but when the tumor grows, the following signs appear:
- swelling of the body,
- dense formation in the abdominal cavity,
- weight loss,
- pain in the lower back,
- elevated temperature,
- numbness of the lower extremities,
- increased body temperature,
- disorder of the excretory system and intestines.
Classification
Doctors identify the main stages of the development of the disease, allowing them to determine the optimal methods for treating and restoring the body.
Stage 1
A tumor-like formation not exceeding 5 cm in size, which generally makes it possible to perform surgery with complete removal of the tumor. At the first stage, there are no enlarged lymph nodes or metastases.
Stage 2 (2A and 2B)
2A is characterized by partial operability of the tumor with no metastases.
At 2B, metastases develop that affect the lymphatic system.
- Adrenal glands: symptoms and causes of the disease, their diagnosis and treatment
Stage 3
The appearance of a bilateral malignant tumor indicates the transition of the disease to the third stage, qualifying as:
- T1 and T2 - a formation measuring no more than five or five to ten centimeters.
- N1 - damage to lymph node metastases.
- M0 - no distant metastases.
When qualifying stage N, specialists do not determine the presence/absence of metastases.
Stage 4 (4A and 4B)
An enlarged tumor with the formation of metastases in the bone marrow, lymph nodes, and internal organs.
Stage 4A - tumor size no more than 10 cm, with the impossibility of determining the presence/absence of metastases.
Stage 4B - multiple formation of tumors.
Epidemiology
The incidence of adrenal cancer is 0.6-1.67 per 10 6 people per year. The ratio of women to men is 2.5-3:1. The highest incidence of adrenal cancer is recorded at the age of under 5 and at 40-50 years.
There are several types of functional adrenal tumors. The most common are Pheochromocytoma, Cushing's Syndrome and Aldosterone. Pheochromocytoma is a benign tumor of the adrenal gland that secretes adrenaline and norepinephrine hormones. These hormones are responsible for regulating heart rate and blood pressure, among other functions. Pheochromocytomas occur most often in young, middle-aged adults between the ages of 30 and 30.
The most common symptom of pheochromocytoma is high blood pressure, which is sometimes extreme. Symptoms include spells with a sudden onset of high blood pressure, anxiety and emotional stress. Rapid pulse Palpitations Headache Nausea Vomiting Sticky skin. . In addition to a complete medical history and physical examination, diagnostic procedures for pheochromocytoma may include.
Diagnosis of the condition
In order to detect a tumor, tomography (CT, MRI, positron emission) and ultrasound of the abdominal organs are performed. To clarify the type of neoplasm, a biopsy is indicated. In later stages, foci of metastasis are often in the bone marrow and bone tissue, so a trepanobiopsy of the ilium is performed. Helps to identify cell proliferation:
- skeletal scintigraphy;
- general radionuclide scan with metaiodobenzylguanidine;
- X-ray or tomography of the chest;
- Ultrasound of the liver.
For laboratory diagnostics, content tests are used:
- catecholamines, blood ferritin;
- catecholamine metabolites (homovanillic and vanillylmandelic acid) in urine;
- for neuron-specific blood enolase (with its growth, an aggressive course of the tumor often occurs);
- blood cells, ESR.
Adrenal adenoma
The most common formation is hormonally active. This is a collective concept for all benign adrenal tumors. The main symptom is increased production of hormones. Such tumors. An adenoma is discovered by chance when examining other abdominal organs on CT and MRI.
This helps explain how many people are diagnosed with this type of tumor and overall survival. Or, use the menu to select another section to continue reading this guide. What is pheochromocytoma? Pheochromocytoma is a rare type of tumor. It grows in the middle of the adrenal glands. Your body has 2 adrenal glands. They are located on top of each kidney. Each layer of these glands produces different hormones. The mid-adrenal gland makes adrenaline and norepinephrine. These hormones help maintain heart rate and normal blood pressure.
There are several main types of adenomas:
- adrenocortical is a dense node resembling a capsule;
- oncocytic has a peculiar granular structure;
- pigmented is the rarest and does not manifest itself in any way.
Symptoms of adrenal adenoma:
- hormonal changes occur in the body;
- men become more feminine;
- women suffer from infertility, notice excessive hair growth, as well as an increase in muscle tissue;
- a characteristic feature is increasing osteoporosis;
- overweight;
- high blood pressure.
Before starting treatment, a special diagnosis is carried out to rule out. The patient is observed for some time and, if necessary, surgery is performed. The treatment is quite simple, so the prognosis is favorable. The main thing is not to let the adenoma progress!
Pheochromocytoma causes the adrenal glands to produce too much of these hormones. What causes pheochromocytoma? It is not known what causes this type of tumor. Who is at risk for pheochromocytoma? Pheochromocytomas occur equally in men and women. If anyone in your family has this type of tumor, you are more likely to get it. This tumor does not appear to be affected by environment, diet or lifestyle. If you have this tumor, you should consider genetic testing.
What are the symptoms of pheochromocytoma? The most common symptom of pheochromocytoma is high blood pressure. It may be constant or sometimes high. Sometimes the tumor can cause high blood pressure, which can be life-threatening. This is a very rare cause of high blood pressure. But this must be considered when medications are not enough to control high blood pressure. Other symptoms are less common. They can be triggered when you are under stress or when you change positions.
Diagnostics
If a child exhibits one of the symptoms characteristic of adrenal neuroblastoma, you should immediately contact a pediatrician for further examination, including a urine test, a complete blood count, a blood test for tumor markers, ultrasound of internal organs, MRI, CT. For a detailed examination of the tumor, a tissue biopsy is performed.
On this topic
How to identify and treat papillary thyroid carcinoma
The primary diagnostic examination consists of mandatory blood and urine tests.
Confirmation of the presence of neuroblastoma determines the appointment of additional, more in-depth studies that make it possible to establish the location of the malignant tumor, the presence or absence of metastases, their size, as well as the nature of the tumor itself.
Causes of the pathological process
There are many reasons that lead to the development of hyperplasia, but the most important are:
- genetic predisposition;
- constant exposure to stress factors;
- congenital enlargement of glands.
The adrenal glands have two layers: the cortex and the medulla. There are a number of diseases that can lead to their increase and occurrence in different areas. Accordingly, the causes, namely pathologies that lead to increased cell growth, can be divided into two groups, according to localization in different layers.
Stress is the most important damaging factor, since the adrenal glands are very susceptible to it
Diseases such as neuroblastoma, ganglioma, and pheochromocytoma develop in the medulla. And in the cortex:
- adenoma;
- hemorrhages;
- angioma;
- fibroma;
- cystic formations.
The genetic factor is characteristic of all pathological processes. Therefore, if there have been previous cases of hyperplasia in your family, then it is better to play it safe and undergo timely examinations at the clinic. The adrenal glands are very sensitive to stressful situations, so you should refrain from emotional conflicts, nervous tension and other negativity. If you do not protect yourself from stress factors, then a malfunction of the paired organ will soon occur.
In a small child, congenital pathology is most often observed. It develops if his mother was in a state of constant stress during pregnancy, and also at this time experienced an enlargement of the endocrine glands. In addition, severe toxicosis in the expectant mother, reduced levels of the hormone hydrocortisone and the use of certain medications can lead to a congenital form of hyperplasia.
Stages of oncological pathology
Like all cancers, neuroblastomas are classified according to the stage of the malignant process. This is of great importance in oncology. The stage allows you to assess the prognosis of the disease, as well as determine treatment tactics. However, it should be taken into account that neuroblastoma is a unique tumor, prone to the ability to regress on its own and become a benign process. Such “miracles” can happen at any stage. Therefore, the diagnosis of “neuroblastoma” is not always a death sentence.
The first stage of the disease (T1N0M0) is characterized by the presence of a primary tumor lesion measuring 5 cm or less. In this case, regional lymph nodes are not affected, and there are no metastases to other organs. At the second stage (T2N0M0), only the primary tumor focus increases. Its size ranges from 5 to 10 cm. There are no signs of malignant cells spreading throughout the body.
The third stage of neuroblastoma is characterized by damage to nearby lymph nodes. In this case, regional metastases may be single (T1-2N1M0) or their localization cannot be determined (T3NxM0).
The most dangerous is advanced neuroblastoma in children. Stage 4 of the oncological process is characterized by the presence of multiple malignant foci (T4NxMx) or damage to other organs (T1-3NxM1). Tumor metastases are most often found in the bones, skin and liver.
Types of treatment
Treatment of the baby is carried out in coordination with several oncologists at the same time. The surgeon, chemotherapy and radiologist decide together how the treatment should be carried out. The option is selected based on the patient’s condition and prognosis at the time of the final diagnosis. Treatment is carried out using one or several methods simultaneously:
Medication. The specialist prescribes potent medications, which, if taken in the wrong dosage or not, can cause harm to the baby’s health. Self-administration of medications is prohibited.
Surgical . The most common and effective method of treatment, especially in the initial stages of the disease. In some cases, complete removal of the tumor is possible. Can be successfully used for metastasis.
In some cases, surgery is performed after a course of chemotherapy to permanently remove the accumulation of defective cells.
Chemotherapy . It is carried out using cytostatic agents. Under their influence, neoplasms are destroyed or stop growing. Chemotherapy is carried out in the following ways:
- intravenous administration of the drug,
- taking medications orally,
- intramuscular injections.
When the drug enters the body, the tumor cells die. In some cases, it is recommended to administer the drug into the spinal canal or directly into the affected organ - regional chemotherapy. In some cases, the simultaneous use of several drugs is indicated - combination chemotherapy.
Radiation therapy and high dose chemotherapy with stem cell transplantation . A method in which a high dosage of drugs is prescribed. Their intake leads to the destruction of hematopoietic cell stems and replacement with new ones. They are collected either from the child's bone marrow or from a suitable donor, and then frozen. At the end of the course of chemotherapy, the cells are administered to the patient intravenously. They mature and new, absolutely healthy ones are formed from them.
Radiation therapy. This method uses high-frequency X-rays. As a result of exposure, you can completely get rid of malignant cells and stop their growth. There are two types of radiation therapy: external and internal. With external, the beams of the device are directed directly at the tumor; with internal, radioactive substances are injected into the tissues located next to the tumor or directly into it using devices (needles, catheters, tubes).
Treatment with monoclonal antibodies . These are antibodies that are obtained in a laboratory from one of the types of cells. They are able to recognize specific formations on tumor cells, intertwine with them, and then destroy them and block further growth. Monoclonal antibodies are introduced into the child's body in an invasive manner.
Forecast
The favorable prognosis after treatment largely depends on the stage of the cancer.
The earlier adrenal cancer is detected, the greater the chance of a full recovery. The third stage, like the first two, has a good prognosis for patients in almost 65% of cases - after recovery, children lead a normal lifestyle and develop fully.
Stage 4S in more than 75% of cases is overcome independently by the child’s body without medical intervention.
The prognosis is disappointing for a patient at the fourth stage - up to 20% of children can live no more than five years after tumor removal and subsequent treatment.
Treatment
A correct and timely diagnosis in most cases gives a positive prognosis. As a rule, the course of therapy is selected depending on the stage of development of the oncology; it can be medication, radiation therapy, chemotherapy, or surgery.
Typically, surgery is performed in all cases of neuroblastoma. The first three stages, using chemotherapy and subsequent removal of the tumor, and then a mandatory course of radiation therapy, are treatable, and the child almost always returns to normal life.
But the last stage is quite difficult for therapy, and the risk of losing the child is very high.
Because the survival rate of children after surgery is insignificant, and very few children live more than five years after treatment. Share:
Clinical picture of retroperitoneal neuroblastomas
Neuroblastoma of the retroperitoneal space in children is detected in approximately 30% of cases. Diagnosing a tumor in this area can be difficult. Often it has no clinical manifestations in the early stages of the disease. The symptoms that may occur are often confused with signs of other pathologies of the digestive tract, as they are not specific to cancer. Such manifestations include:
- The appearance of a noticeable tumor on the anterior surface of the abdomen. Neuroblastoma is dense in consistency and resembles a node.
- Constant increase in body temperature.
- Abnormal stool – diarrhea or constipation.
- Pale skin due to anemic syndrome. Despite the fact that a decrease in hemoglobin levels is almost always observed in cancer, it can also occur in inflammatory pathologies of the gastrointestinal tract.
How do retroperitoneal neuroblastomas manifest in children at later stages? Symptoms of a tumor are often diagnosed when the form of cancer is already widespread. Signs of neuroblastoma include severe periodic pain in the spine and limbs. This syndrome is caused by tumor metastases to bone tissue. Also a symptom of the progression of retroperitoneal cancer is the occurrence of edema not associated with kidney disease. Another sign of a malignant lesion is a decrease in body weight. When cancer grows into the urinary organs, dysuric symptoms are observed.
Symptoms of adrenal pathology
Adrenal neuroblastoma in a child causes fatigue, fever, hyperhidrosis, and indigestion.
Neuroblastoma does not appear in the first stages of its development or does not produce pronounced symptoms. Often, in the initial phase of development, malaise is observed, but until the age of 2, this symptom is attributed to other diseases or developmental features of the infant at this stage of life. Stage 3 neuroblastoma produces vivid symptoms. Scientists identify the main symptoms, such as:
- pathological fatigue;
- increase in temperature indicators;
- pain syndrome in bone tissue;
- digestive disorders (nausea, vomiting);
- weight loss;
- increased sweating.
Cancer cells produce hormones. An expanded malignant formation in the retroperitoneal cavity can negatively affect the functioning of the intestines and stomach. If the metastases reach the bone marrow, the child becomes lethargic and weakened. Blood clotting is impaired, and even a small cut leads to large blood loss.
Neuroblastoma in children: symptoms, causes, pathology photos
The clinical picture of the disease is associated not only with the localization of the tumor focus, but also with the cellular elements from which the malignant formation was formed. What does neuroblastoma look and feel like in children? Symptoms, photos of the tumor, or more precisely, in medical terms, X-ray images, computed tomography data can be different. Clinical manifestations often depend on location. Therefore, having received an image of a malignant tumor, the doctor has the opportunity to guess what symptoms characterize this tumor and why it is dangerous in the future.
The main reason for the development of neuroblastomas is incomplete cell differentiation. They, in turn, can be different. Depending on this, the following forms of pathology are distinguished:
- Medulloblastoma. This tumor is formed from cerebellar cells. The pathological process is characterized by rapid spread and high mortality. It is impossible to get rid of the tumor, since it is localized deep in the brain. The main symptoms of the disease are impaired balance and coordination of movements in the child.
- Retinoblastoma. Some authors identify this form of cancer as a separate disease. However, although the tumor causes vision loss, it is made up of nerve cells (the retina). The pathology is asymptomatic. The only clinical manifestation of the disease is the tumor being visible through the pupil. This phenomenon is called the “cat's eye” symptom. It is characterized by the fact that when a light flux is pointed at the eye, the pupil turns white.
- Neurofibrosarcoma. This tumor originates from undifferentiated sympathetic fiber cells. It often appears at a late stage. Metastases are found in lymph nodes and bone tissue.
- Sympathoblastoma. Characterized by increased production of catecholamines. It can be localized in the adrenal glands or sympathetic formations (nerve fibers, nodes).
What does neuroblastoma look like in children? Photos of the tumor differ in each specific case. Pathological formation can be visualized on the stomach, back, chest. It is impossible to diagnose a tumor only by external signs and its palpation. For this purpose, it is necessary to perform a morphological study.
VASCULAR PATHOLOGY
NEONATAL HEMORRHAGE
Idiopathic neonatal hemorrhage is characteristic and is 4 times more common than neuroblastoma. Its development is associated with prematurity, prolonged labor, sepsis and coagulation abnormalities. The source of hemorrhage in newborns is considered to be rapid involution of the fetal cortex. Although neonatal hemorrhage is often identified incidentally, such infants may present with symptoms of jaundice, anemia, low blood pressure, and/or a palpable mass if the hemorrhage is particularly large, although even with major hemorrhages, adrenal insufficiency is rare. Neonatal adrenal hemorrhages are more common in the right gland because of direct compression on it by the adjacent large portion of the liver, and because of the propensity for any transmitted increased venous pressure to be transmitted directly to the organ through the right adrenal vein. Venous drainage from the left adrenal gland provides some protection from increased venous pressure because it occurs more indirectly through the left renal vein.
On ultrasound examination, acute adrenal hemorrhage in newborns takes the form of an irregular echogenic formation that disrupts the normal architecture of the adrenal gland (Fig. 19).
Rice. 19. Neonatal hemorrhage into the adrenal glands.
Blood flow is not determined by color Doppler ultrasound. As the disease progresses and the clot liquefies, the echogenic formation becomes smaller and more hypoechoic, and cystic changes may develop (Fig. 20), with possible revisualization of the normal appearance of the adrenal glands.
Fig.20. Liquefaction of neonatal adrenal hemorrhage (cross).
An important role of the radiologist is to be able to provide some imaging criteria that help distinguish idiopathic neonatal hemorrhage from congenital neuroblastoma (which can also bleed). The absence of flow on the Doppler image characterizes bleeding over the mass (Fig. 21), as do serial ultrasound studies that demonstrate a decrease in the size of the adrenal mass. This reduction in size usually continues until complete regression occurs between 20 and 165 days of life.
Rice. 21. Neonatal hemorrhage into the adrenal glands. The absence of color Doppler flow is shown.
TRAUMATIC BLEEDING
Adrenal hemorrhage can occur due to either accidental or provoked trauma. In accidental trauma, this occurs in approximately 3% of cases and is associated with other ipsilateral thoracic and intra-abdominal injuries. The picture of provoked blunt abdominal trauma may have signs of hemorrhage into the adrenal glands. Abused children with similar findings also have ipsilateral rib and visceral injuries. Sonographic features are similar to neonatal idiopathic hemorrhage (Fig. 22).
Rice. 22. Traumatic hemorrhage into the adrenal glands in an 8-year-old boy
Causes of neuroblastoma
Until now, scientists have not come to a consensus on what contributes to the formation of neuroblastoma. This disease mainly manifests itself in children under two years of age, so there are several theories about the occurrence of this pathology.
Pathology can be a manifestation of heredity, and it reaches its peak of development before the baby reaches one year of age. It can develop in several areas at once: in the adrenal glands, lumbar and cervicothoracic regions.
The pathological process can occur at an early stage of maturation of nerve cells, in which they reside for the first three months of a baby’s life. A mutation that occurs at the cellular level leads to incomplete maturation of uneven cells; with their constant division, malignant tumors develop
Gene mutations that may be associated with external and internal psychogenic phenomena cannot be excluded.
Statistics for children and adults
Neuroblastoma is considered the most common malignant neoplasm in children. It is found in approximately 14% of cancer cases. It can be congenital or appears before the age of 5 years, with the peak incidence occurring at two years of age.
A third of all tumors are located in the adrenal medulla. Usually has unilateral localization. Neoplasms can also be found in the space behind the peritoneum, in the chest, neck and pelvic area.
After 15 years, the detection of neuroblastomas is an extremely rare case, but development options have been described even in old age. With congenital pathology, it is often combined with other developmental anomalies.
Features of adrenal neuroblastoma
The cells from which this tumor develops are the precursors of neurons of the sympathetic nervous system. They are germinal tissue and are called neuroblasts. The neoplasm is considered malignant and undifferentiated, that is, the most aggressive in its course.
Neuroblastoma gives early and distant metastases, spreading through the blood and lymphatic vessels. In most patients, at the time of detection, the lymph nodes, bones and bone marrow are already affected. Less common is the transition of cells to the liver, kidneys and brain tissue.
However, this tumor has a unique feature - under the influence of unknown factors, it can become differentiated. In this case, neuroblastoma transforms into a benign neoplasm, acquiring the features of a ganglioneuroma. It can also have a mixed structure.
Some patients are able to completely get rid of neuroblastoma without treatment or with low doses of chemotherapy, even in the presence of metastasis. This is how a tumor differs from all other neoplasms of the human body.
We recommend reading the article about adrenal androsterome. From it you will learn about the cause of the tumor, symptoms in women and men, as well as the diagnosis and treatment of adrenal androsteroma. And here is more information about the hormone dopamine.
Sources used:
- https://onkologia.ru/onkoendokrinologiya/neyroblastoma-nadpochechnika/
- https://m.baby.ru/wiki/nejroblastoma-u-detej-priciny-vozniknovenia-i-podhody-k-terapii/
- https://etopochki.ru/nadpochechniki/nejroblastoma-nadpochechnika-u-detej.html
- https://uran.help/diseases/nejroblastoma-nadpochechnika.html
- https://endokrinolog.online/nejroblastoma-nadpochechnika/
- https://www.syl.ru/article/307137/neyroblastomyi-u-rebenka-simptomyi-prognoz-lechenie
The unpredictable nature of neuroblastoma in a child
Neuroblastoma is a malignant neoplasm, and its course is rapid and quite difficult for a child. In 85% of cases it occurs in the retroperitoneal space, in 15-18% of cases it affects the adrenal glands. According to statistics, this disease occurs in one out of one hundred thousand children.
The malignancy of the tumor is explained by the uncontrolled division of cells produced by the patient’s own body, which cannot be treated with antibiotics or other drugs without a similar effect on other cells. As is the case with cancer, neuroblastoma cells have the ability to separate from the general mass and, through the flow of blood or lymph, metastasize throughout the baby’s body.
The unpredictability of neuroblastoma lies in its ability to self-destruct. No one can explain how or why this happens, but neuroblasts incredibly transform into neurons and stop dividing. Neuroblastoma transforms into ganglioneuroma, a benign tumor that can be easily removed surgically.
"Important! The process of tumor degeneration is observed only in cases where the tumor is small in size.”
Neuroblastoma can metastasize to any place in the body, but most often to the adrenal glands, bone marrow, lymph nodes, and bone marrow. Extremely rarely - into the liver, skin and other organs. Tumor cells behave like healthy ones and tend to form organs of the nervous system. They are actively directed towards the brain, but neuroblastoma affects the brain extremely rarely.
With treatment in the early stages, you can achieve good results and even complete recovery. Inexplicably, even with a large number of metastases, the neuroblast can mature, degenerate, and complete recovery occurs.
How to recognize neuroblastoma?...
To establish a diagnosis, we first turn to the possibilities of clinical laboratory diagnostics, which include:
- Determination of catecholamines, their precursors and metabolites in the urine of a child. Increased excretion of substances produced by the tumor in exorbitant quantities will be reflected in the analysis.
- Excessive release of a neuronal glycolytic enzyme into the blood, called neuron-specific enolase (NSE), may indicate the development of a tumor process and, by the way, not only neuroblastoma. An increase in the level of NSE is typical for other tumors: lymphoma, nephroblastoma, Ewing's sarcoma, so this tumor marker can hardly be suitable for differential diagnosis, but it has proven itself well in prognostic terms: the lower the level of the marker, the more favorable the prognosis. For example, with neuroblastoma stage. IVS of nonspecific enolase is always less than with a similar stage 4 tumor.
- An important tumor marker for neuroblastoma is ferritin, which is actively produced, but iron is not used (anemia), but enters the blood. A change in the amount of this marker is observed mainly in stages 3-4 of the disease, while in the initial stages (stages 1-2) its level is slightly increased or generally remains within normal limits. During the treatment period, the indicator tends to decrease, and during remission it returns to normal.
- A high level of membrane-bound glycolipids - gangliosides - can be detected in the blood serum of most patients with neuroblastoma, and rapidly growing neoplasia increases the indicator by 50 times or more, but active therapy contributes to a significant drop in the marker content, while relapse, on the contrary, is noticeable increases.
Other methods for diagnosing neuroblastoma include:
neuroblastoma on a diagnostic image
- Bone marrow aspiration biopsy and/or trephine biopsy of the sternum and iliac wing, biopsy of lesions suspicious for metastases - the resulting material is sent for cytological, immunological, histological, immunohistochemical analysis (depending on the capabilities of the medical institution);
- Ultrasound diagnostics, because ultrasound quickly and painlessly finds a tumor in the abdominal cavity and pelvic organs;
- Chest X-ray, which can find a tumor localized there;
- CT, MRI and other methods.
Suspicion of distant metastasis poses the task of immediate and particularly careful examination of not only the bone marrow, but also the skeletal bones. For this purpose, I use methods such as R-graphy, radioisotope scintigraphy, trephine and aspiration biopsy, CT and MRI.
Peculiarities
When a mother gives birth to her baby, the following changes occur to the baby:
- A large amount of hormones from the mother's body is retained.
- The processes of synthesis of adrenocorticotropic hormones are suppressed, which leads to a decrease in the production of own hormones. This condition is often accompanied by signs of renal failure.
- Such clinical manifestations persist until 10-15 days of life.
- Gradually, the newborn experiences a change in hormonal levels due to the stabilization of the production of corticosteroids.
In the first 90 days of development, the baby's glands decrease by almost half. This is due to the thinning and reformation of the cortical layer. A year later, the mass of the adrenal glands increases again. By 12 months, the fetal tissue part is absorbed, and glomeruli, fascicles and mesh tissue are already present in the cortical zone. At three years, the process of separation of cells and the cortical layer of the glands is completed, but the formation of structures continues for another 10 years.
The final determination of adrenal gland mass occurs at 18-20 years of age. By this time, the glands function as in an adult.
Before 12 months, cortisol production is not established. Increased levels of the hormone are observed in the morning.
Causes
Like other cancers, neuroblastoma occurs due to genetic changes. However, it is not completely known why such mutations occur. Some experts believe that the causes of neuroblastoma are directly related to exposure to carcinogenic factors. This can be either chemicals or radioactive exposure.
As a result of mutations, cancer cells are formed, which have the ability to quickly divide and spread to other organ tissues. Most of the patients with this diagnosis are infants. This is because the development of neuroblastoma occurs in the womb or immediately after birth.
When a child is born, most neuroblasts are already fully formed, some of them remain in an underdeveloped state. During the normal course of the process, they disappear, and if mutations occur, they are transformed into a cancerous tumor.
The risk of developing the disease is complicated by hereditary predisposition. However, this probability is minimal, occurring in no more than 2% of cases.
Neuroblastoma of the retroperitoneal space, as a rule, is detected in the womb during ultrasound. The cause of the appearance is also mutations of embryogenesis. In pediatric patients, the malignant tumor may disappear on its own. Cancer cells mature in a timely manner, and then remission is observed.
The disease is divided into the following stages:
- Stage I – localized neuroblastoma, operable;
- Stage IIA – removal of a tumor fragment is possible;
- Stage IIB – neoplasm only on one side, partially operable;
- Stage III – development of metastases to nearby organs and lymph nodes;
- Stage IV – metastases also develop in distant organs. With stage IV neuroblastoma, the formation becomes practically inoperable.
Regardless of the cause of neuroblastoma, treatment must begin as early as possible. At the initial stage of formation, the disease is completely eliminated.
Acute failure
Acute adrenal insufficiency in newborns is a very severe form of pathology. The causes of this condition are usually severe hemorrhage in these organs, which is due to:
- birth trauma;
- asphyxia;
- hemorrhagic syndrome in infectious diseases.
Somewhat less frequently, ONN may occur as a result of congenital hypoplasia, which is transmitted in an autosomal recessive manner or has X-linked inheritance. Such a pathology in a newborn can be detected during genetic testing.
Signs of an acute condition
In the case when the adrenal glands practically do not work, the symptoms of the disease in children manifest themselves as follows:
- The baby practically does not move, his blood pressure and muscle tone drop sharply.
- The pulse is frequent, shortness of breath develops, and the volume of urine excreted decreases.
- There is vomiting, diarrhea, and pain in the intestinal area that varies in intensity and location. As a result of fluid loss, dehydration can quickly occur, which is a very dangerous condition in a newborn baby.
- The temperature decreases, the skin becomes pale or bluish, sometimes a marbled pattern and hemorrhages are noted.
- In the last stage, a collaptoid state develops, caused by vascular insufficiency. A decrease in potassium levels in the blood causes the heart muscle to stop working.
The rate at which symptoms develop in newborns depends on the cause of the deficiency. With sudden damage to the adrenal glands as a result of hemorrhage or discontinuation of glucocorticoids, the clinical picture of the disease develops in a matter of hours. If acute deficiency becomes the result of a chronic process, then the onset of its onset may last for several days or months.
Treatment of acute adrenal insufficiency
This condition can quickly lead to the death of a newborn baby, so treatment is carried out only in an intensive care unit. When providing assistance, parenteral administration of hormones (glucocorticoids and mineralocorticoids) begins immediately. This replacement therapy, if started on time, immediately has an effect and causes an improvement in the condition of the little patient.
If necessary, anti-shock measures and symptomatic treatment are carried out.
Disease Prevention
It is impossible to prevent the development of serious pathologies of the adrenal glands, since many of them are the result of autoimmune, hereditary and nervous pathologies. The child must be provided with a balanced diet, taught a healthy lifestyle, and stress must be minimized. The best prevention would be scheduled visits to doctors and timely diagnosis of all diseases.
You can also learn from this video about dyslexia, what its main causes are and how to treat this disease.