Kidney diseases are common. Ultrasound, magnetic resonance imaging and kidney urography are used to diagnose them. This allows you to find out what external disturbances have occurred to the organ, as well as what changes there are in its structure. Urography is most often used in the diagnosis of urolithiasis. It is necessary in order to make the correct diagnosis and, accordingly, prescribe the correct treatment. How is the procedure performed and what are the features of diagnosis in children?
About terminology
Urography is any X-ray examination of the urinary organs with mandatory confirmation of visual changes by photographs (x-rays), including the structures of the kidneys, ureters, bladder, and urethra.
Some authors consider the term “pyeloureterography” to be more acceptable. It actually includes x-ray monitoring of the entire urinary tract and specifies the scope of the procedure. Others stop at “renal urography” if we are talking only about an isolated study of renal structures.
When prescribing a “tomography”, the doctor relies on layer-by-layer images of an organ to clarify the location and size of organ damage using different depths of penetration of X-rays. A series of images allows you to select the optimal image.
Patients don’t have to pay attention to this, but when paying for diagnostics in a private clinic, the cost will vary, you need to be prepared for this and check in advance. In addition, you should pay attention to what type of urography is intended to be used. Currently used:
- overview;
- excretory urography (infusion).
Each method has its own indications and negative sides.
Optimal research methodology
However, conventional intravenous pyelography does not always accurately depict damaged structures. While the contrast passes through the urinary tract, an additional series of images can be taken, which will be called ureterography, but the images are often not clear enough, and part of the tract may be spasmed and it will not be possible to get a complete picture.
Therefore, to obtain better images, a retrograde injection of contrast agent is performed through the external opening of the urethra. This study is called retrograde ureteropyelography.
It can be used to diagnose obstructive urethral diseases:
- strictures;
- tumors;
- diverticula;
- traumatic injuries of the urinary canals.
Using pyelography, you can evaluate not only the anatomical features of the organs of the excretory system, but also their function
The value of survey urography
An overview image of the kidneys actually includes the bone structures of the spine, partly the abdominal organs, and soft tissues. This is a standard examination method that allows you to obtain a minimum of information about:
- the location of both kidneys;
- large concretions (stones);
- gross changes in structure, contours, dimensions.
The renal collecting apparatus of the kidneys is not visible during survey urography
This type of examination is usually used in primary diagnosis. It does not require the introduction of contrast.
Excretory urography
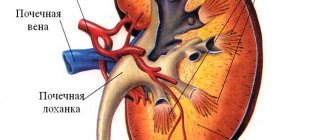
The method is carried out with the obligatory use of a radiopaque substance. The essence of the method: a medical drug is administered intravenously (stream or drip), which is clearly visible under the influence of x-rays. It quickly accumulates in the urinary system. As it is processed and excreted by the kidneys, the calyces and pelvis are completely filled, then the substance passes into the ureters, bladder and urethra.
By controlling the isolation process over time, it is possible to take optimal pictures of these structures, from which much more information is obtained than with survey urography. Using the established standards for the start of contrast flow, it is possible to register a delay in one of the kidneys, and, therefore, judge its functional ability.
results
When assessing the results of urography, the doctor analyzes the location and shape of the kidneys, and also notes the rate of removal of the radiocontrast substance. Parenchymal structures, the pyelocaliceal system and its functionality are assessed. Obstacles to normal urinary flow, insufficient filling of the pelvis with urine, etc. are identified.
Renal stones are also detected during urography, but only closer to the final images do they become visualized, since at the beginning of the diagnosis the stones are darkened by contrast. If during the diagnostic process there is no progress of contrast through the kidneys, then it is possible that the kidney is missing, underdeveloped or blocked by a stone. Sometimes a similar picture occurs with severe hydronephrosis.
Neither children nor adults should be afraid of urographic examination, since identifying kidney pathology at an early stage maximizes the chances of a successful recovery.
Contrast requirements
The quality of the resulting image and the reliability of information about pathological changes depend on the choice of contrast agent. The required drug should not:
- “go away” and accumulate in tissues;
- participate in general metabolism;
- have toxic properties.
Ready-made preparations are used that have maximum radiopacity with minimal allergenic properties.
Products containing iodine are more often used. A day or two before the test, the patient is supposed to do a test to identify individual sensitivity. If a rash, skin itching, or swelling occurs, administration of the drug is strictly contraindicated.
In practice we use:
- Cardiotrust,
- Triyombrust,
- Visipack,
- Urografin.
Drugs are injected into a vein slowly or in a dropper
Indications
The retrograde ureteropyelography procedure is indicated for identifying pathological processes in renal tissues such as:
- Pyelonephritis;
- Hydronephrosis;
- Renal tuberculosis;
- Congenital anomalies in the renal structure;
- Glomerulonephritis;
- Salt stones;
- Hypertension;
- Neoplasms of various types;
- Hematuria;
- All kinds of infectious diseases;
- Structural abnormalities in tissues;
- Postoperative monitoring of organic structures.
In the presence of urate-type nephrolithiasis, stones are not visible on X-ray examination, therefore, when conducting a retrograde ureteropyelographic study, gas is used, which visualizes urate stones.
How is preparation for urography carried out?
A prerequisite for the patient’s readiness for urography is thorough cleansing of the intestines from gases and feces.
To do this, preparation for urography includes tips:
- 3 days in advance, stop eating carbohydrate foods, foods that cause increased gas formation and fermentation in the intestines (brown bread, carbonated water, do not eat vegetables and fruits, kefir, cottage cheese);
- take a laxative the day before;
- do an enema in the evening and 3 hours before the examination;
- take Carbolen or activated carbon, chamomile infusion.
The difficulty lies in the fact that the possibility of complete cleansing depends not only on the nature of the diet, but also on the individual characteristics of the intestines, liver, and age of the patient.
- For young people, diet is important, for older people with intestinal atony - enemas.
- Weakened bedridden patients swallow a large volume of air, so they are advised to walk more around the house, in the hospital room.
- Outpatients are usually better prepared because they are able to move around a lot.
- It must be taken into account that the use of iodine-containing substances impairs the liver’s ability to absorb intestinal gases.
Who is indicated for infusion urography?
Excretory urography of the kidneys and lower urinary organs is prescribed to patients to identify and exclude:
- congenital anomalies of the urinary system;
- chronic inflammatory diseases;
- tumor processes;
- functional bladder changes in children;
- urolithiasis with attacks of renal colic;
- kidney prolapse;
- hydronephrosis;
- traumatic injury.
The study is carried out when the patient detects such unclear symptoms as:
- hematuria;
- partial or complete blockage of the ureter;
- unusual kidney mobility.
Contrast urography is necessary in preparation for surgery and for monitoring after surgery.
When and how many pictures to take is determined by the radiologist. They are usually carried out from the first minute, first at intervals of 5-7 minutes, then 12-25 minutes over the course of an hour.
If the drug is administered slowly by drip, then radiographs are taken after 45 minutes or an hour.
When a contrast agent is administered, patients may feel fever, a moderate burning sensation in the vein, and less commonly, nausea or dizziness. Unpleasant symptoms disappear within a few minutes.
Advantages and disadvantages of the method
Intravenous urography has the following capabilities:
- Allows you to study in detail the pathological processes that occur in the cups and collectors for collecting urine, as well as in other structures of clinical nephrology.
- When the contrast agent accumulates in sufficient quantities, it becomes possible to assess the functionality of organs in infectious and inflammatory diseases of the kidneys and other pathologies.
- Allows a detailed examination of pathological foci, stones, and foreign bodies.
- It is convenient to use in pediatrics because it is a less unpleasant and less painful procedure.
- Low cost and non-invasive.
At the same time, intravenous urography has a number of disadvantages:
- Quite limited information is available about the structure of functionally active epithelial cells of the kidneys and the spaces surrounding the kidneys.
- It is impossible to obtain data on functional parameters of urination.
- The procedure is not performed in case of renal failure and allergy to iodine, and it is also contraindicated in case of heart and liver failure.
- During the study, iodine preparations and radiation exposure are used.
The method of intravenous renal urography has been used in medical practice since 1929. Over time, the diagnostic value of this procedure only began to gain momentum and now it can be performed in almost any clinic.
What are the contraindications?
Contraindications are associated with a possible reaction to the contrast agent and exacerbation of certain diseases. Similar conditions are possible under:
- an allergic reaction to the drug identified before using contrast;
- pregnancy in any trimester;
- unclear internal bleeding;
- identifying reduced blood clotting;
- •renal failure with impaired excretory function;
- acute stage of glomerulonephritis;
- thyrotoxicosis;
- pheochromocytoma (adrenal tumors).
Particular attention is paid to the examination of patients with diabetes mellitus taking the drug Glucophage from the biguanide group. It contains the substance metformin, which, when combined with iodine contrast, can cause a sharp increase in the level of lactic acid in the patient’s blood and lead to acidosis.
Glucophage should be discontinued in agreement with the endocrinologist two days before the x-ray examination
For patients with diabetes, it is especially important to ensure that the excretory function of the kidneys is sufficiently preserved so that the contrast is removed from the body in a timely manner.
Competitive survey methods
During magnetic resonance imaging, the organ is exposed to a magnetic field and radio frequency waves. The computer allows you to obtain the required image at different depths.
MRI urography helps diagnose:
- kidney size, thickness of the cortex and medulla;
- anatomical structure of the vascular bundle, calyces and pelvis;
- tissue structure density;
- cystic changes;
- tumors;
- dynamics of cyst or tumor growth;
- functional ability of the kidney;
- damage to the urinary tract.
Diagnosis can be carried out both without contrast and with the introduction of a contrast agent. It is believed that the second option improves diagnosis by 15%.
CT scans typically have a superior view with an optimal “cut” at the level of the kidneys
For MRI contrast, agents containing gadolinium salts are used. It is a soft metal with highly soluble salts. Considered to be slightly toxic. It has the ability to penetrate cells and enhance the magnetic signal. Possible application:
- Premovista,
- Magnevista,
- Dotarema,
- Omniscan.
There is no cross-reaction to iodine. Just as with excretory urography, a skin test is first performed to identify allergies.
The technique has been widely used in the early diagnosis of tumors in recent years. But if there are contraindications to urography, you can trust its results.
Vaccination cystography is chosen by the doctor if a thorough examination of the bladder is necessary. The method involves installing a catheter through the urethra into the ureter and injecting a radiopaque substance into the bladder.
Modern devices allow you to monitor the picture during voiding cystoscopy on the monitor
The first photograph is taken against the background of a filled bladder. The patient is then asked to urinate and a second radiograph is taken along the way.
The method is intended to detect vesicoureteral reflux. During urination, the detrusor muscle tenses and intravesical pressure increases. If the ureteral sphincters are weak and cannot cope with containment, then the contrast rises into the ureters. They are visible in the second photo.
If necessary, only a specialist can choose a method for replacing excretory urography. MRI does not have a radioactive effect on the patient, so it can be used with great indications for examining a child.
Types of urography
To study the patency of the urinary tract, including the ureters, antegrade (descending) and retrograde (ascending) pyeloureterography are used.
Retrograde urography is performed on one side only. Using a cystoscope, a catheter of the required size is inserted into the ureter (taking into account the degree of narrowing). Through it, the pelvis and ureter are carefully filled with a contrast agent. Usually about 5 ml of solution is administered to an adult.
Practice has shown that bilateral catheterization is poorly tolerated by patients due to spasm of the pelvis and calyces. To prevent pain, the solution is preheated to body temperature and administered very slowly.
The images are taken with the patient in a horizontal position on his stomach and back, as well as in a vertical position. This is necessary to completely fill the calyces in all parts of the kidneys.
An hour after contrast administration, it is recommended to repeat the image in order to assess the evacuation capacity of the pelvis and ureters.
Complications
During the diagnostic study, the following undesirable manifestations may develop:
- renal pelvic reflux;
- distension of the pelvis;
- lower back pain;
- allergies up to the development of anaphylactic shock.
Diagnosis is often complicated by the appearance of hematomas and blood clots at the puncture site. If the ureter is damaged, contrast may enter beyond it or into the kidney tissue, which subsequently causes an increase in body temperature. If sterility is not maintained, infectious infection often occurs, and the administration of contrast can provoke the development of renal colic.
Features of antegrade pyelography
Antegrade pyelography allows you to examine the upper urinary tract. There are 2 options depending on the method of contrast administration:
Survey urography of the kidneys
- percutaneous;
- using pyelo-(nephro)stomy.
The percutaneous method is indicated when other methods have failed to identify kidney and upper urinary tract disease. For example, if during excretory urography there is no release of a contrast agent due to impaired renal function or if it is impossible to perform retrograde urography due to:
- reduced bladder size;
- stone in the ureter;
- sharp narrowing;
- compression of the outflow tract by the tumor.
Percutaneous puncture antegrade pyelography is performed mainly when hydronephrosis is suspected, when other diagnostic methods do not provide confidence in the detected pathology. This method allows not only to identify hydronephrosis, but also to detect its cause (stone, scar narrowing, tumor).
Usually, before antegrade urography, survey films and excretory venous urography are performed. They are needed to select the site of puncture of the pelvis.
Video on the topic
How does it feel during and after intravenous urography? Feedback from one of the patients before you:
Urography is performed to study the condition of the kidneys: the patient is injected with contrast and X-rays are taken. For this reason, a similar method of studying the condition of the kidneys is called contrast urography. The method is based on the ability of the injected contrast to block X-rays: first, the dye accumulates in the kidneys, then it is released by the organs of the genitourinary system, and this makes it possible to assess their condition.
Urography is prescribed to patients with suspected kidney stones, genitourinary tract infection, in the presence of blood in the urine, which can signal acute inflammation or cancer, and in cases of damage to the urinary tract.
There are survey, intravenous, excretory urography.
How is the antegrade urography procedure performed?
The patient is placed on his stomach on an x-ray table. An anesthetic is injected locally into the skin and muscles. Then a puncture needle is made at the projection point of the renal pelvis. To control the position of the needle in difficult cases, an x-ray is necessary.
Another guideline is to obtain colored urine from a syringe when administering a blue indigo carmine solution intravenously 10 minutes before puncture.
Urine is completely removed from the pelvis (it is sent for testing to the laboratory), and a contrast agent in a volume of 10 to 20 ml is injected into the kidney with a syringe.
Images are then taken with the patient lying on his stomach, side and upright.
After that, the entire contents of the pelvis are removed with a syringe and the needle is removed from the body.
After the operation, an artificial nephrostomy is left for the first days for flushing the kidney, introducing antimicrobial drugs into the pelvis and control urography
The introduction of contrast through pyelo-nephrostomy drainage is used mainly in the postoperative period, when the drainage is specifically left in the pelvis for this purpose. The end of the tube is treated with alcohol and secured with a clamp.
Contrast can be administered no earlier than 14 days after surgery. Usually 6–8 ml of solution is sufficient. A larger amount can cause overstretching of the pelvis.
If the tone of the ureters is preserved, then after a minute the contrast agent moves into the lower sections. Delay indicates decreased motor function.
Medical reviews from operating urologists speak about the accumulated experience of performing antegrade percutaneous urography in the diagnosis of polycystic kidney disease and hydronephrosis in children.
The authors describe an interesting diagnostic phenomenon: against the background of antegrade pyelography, doctors observe the excretion of a contrast agent by the opposite kidney after 15–20 minutes. This is explained by the entry of part of the drug into the general circulation and confirms the fairly good excretory function of the other kidney.