Albuminuria or “protein in the urine” is the same term as “proteinuria.” Apparently, equality is due to the fact that albumin accounts for 80% of the protein composition of blood. This suggests that it is the transition of this fraction into urine that causes losses and disruption of body functions.
A healthy person's urine test may show "trace protein" or 0.033 g/L. This conclusion does not cause concern, but requires observation. There are physiological causes of proteinuria. It is known that protein molecules are large in size, so they normally do not pass through the membrane of the glomerular apparatus of the kidneys. Finding out the cause of albuminuria helps to identify the affected organ and promptly prescribe treatment.
How does protein get into the urine of a healthy person?
It has been established that the maximum amount of protein in the urine of a healthy person per day is up to 50 mg. It may not be present in each portion. More precisely, a tiny amount is not determined by conventional methods. For children, the norm is calculated per m2 of body surface: for babies up to a month, the figure should not exceed 240 mg, older - 60 mg per day.
In addition, proteins are contained in cellular elements (leukocytes, erythrocytes, tubular epithelium). When urine is excessively alkalized by eating a large meal, the cells partially disintegrate and the protein they contain passes into the urine. This is facilitated by an increase in pressure in the adductor arteries, accelerating the filtration process.
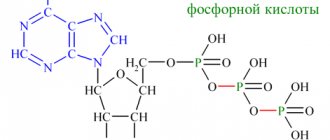
Violation of the permeability of the renal membrane concerns specifically the albumin fraction of proteins, since they have the smallest molecular sizes and in case of overload
filtration are able to penetrate through the pores
Microalbumin in urine
Leave a comment 5,100
A test for microalbumin in urine is prescribed by the attending physician to diagnose the urinary tract and for preventive monitoring of the patient’s health.
- Microalbumin in urine
- What it is?
- Research indicators: norm and pathology
- Causes of microalbuminuria
- Symptoms of albumin in urine
- Clinical manifestations
- Physiological manifestations
- How to get tested?
- How to collect analysis?
- Treatment of microalbuminuria
- Microalbumin in urine
- Microalbumin tests
- Interpretation of analyzes
- Rules for taking the analysis
- Microalbuminuria and rules of conduct when it is detected
- Albumin (in urine)
- Indications for analysis
- How to prepare for research
- Interpretation of research results
- Terms of use
- High levels of microalbumin in urine are an early indicator of nephropathy
- Microalbuminuria - what is it?
- Microalbumin norm indicators
- Decoding analysis data
- Causes of high albumin levels
- How to prepare for a daily UIA
- How to take the test correctly
- What does albumin mean in urine and what are the causes of microalbuminuria
- Albumin in urine
- Tests for microalbuminuria
- Appointments
- Preparing for the study
- Carrying out analysis
- Reference values
- Deviations from the norm
- What disorders does microalbumin in urine indicate? How to get tested for microalbuminuria?
- General information
- Urine testing for proteins
- How to properly collect urine?
- Reasons for the appearance of albumin in urine
- Protein in urine in diabetes mellitus
- Classification of stages of nephropathy progression
- Urine analysis for albumin - norm and ratio
- Diagnostic features
- Indications for analysis
- Reasons for increased albumin
- Symptoms
- Features of treatment
Classification of albuminuria
Albuminuria is classified into two types:
- False albuminuria.
- True albuminuria.
False albuminuria is accompanied by a large number of leukocytes and red blood cells in the urine when protein enters there. True albuminuria occurs in the process of disintegration of inflamed glomeruli and their replacement with connective tissue.
In medicine, there are 3 main stages of disease development:
- Normoalbuminuria - albumin in the urine is usually no more than 17 milligrams per liter.
- Microalbuminuria - in this case, this number ranges from 17 to 173.
- Macroalbuminuria - levels increase to more than 174 milligrams per liter.
Treatment
The specialist prescribes therapy based on the cause of the disease. For example, if albuminuria began as a result of some kind of inflammation, antibiotics are prescribed, if diabetic nephropathy - ACE inhibitors, etc. In this case, restorative medications are also required.
Also, at the discretion of the doctor, blood purification procedures - plasmapheresis or hemodesis - can be performed.
As the patient gets rid of the underlying disease, the level of protein in the urine will gradually decrease.
Diagnostics
In order to prescribe the correct treatment, the doctor needs to find out the reason for the appearance of protein in urine. Since, if this is, for example, a physiological increase in protein levels, then there is no need to prescribe a course of medications. Typically, a specialist recommends refraining from fatty, spicy, salty foods, reducing stress and just resting. Therefore, it is so important to find out the root cause of the disease, which is why diagnosis is needed.
First, the patient's morning urine is taken for analysis (since it is more concentrated) and examined using electrophoresis or a special test. In this way, the protein level and type of albuminuria are determined. For the correct result, urine is re-examined, and if the disease is confirmed, clarifying tests are prescribed: urine testing using the Nechiporenko and Zimnitsky methods, general and biochemical blood tests.
Since albuminuria occurs as a result of some more serious disease, a detailed diagnosis is carried out to identify the root cause of the disease (diabetes mellitus, kidney or heart disease, etc.). However, it is carried out in a hospital setting, where everything is monitored by a doctor and the necessary equipment is available for this.
Albumin norm
In the urine of a healthy body, signs of protein or its minimum levels may be detected, not exceeding 0.033 g/l. This conclusion is not dangerous, but requires control.
To be more precise, its scanty content cannot be determined by known research methods. For a child’s body, the norm is considered to be protein per square meter of body surface: for newborns, this norm should not exceed 240 mg; for older children, this value is 60 mg per day.
For women during pregnancy, this figure is no more than thirty milligrams per day.
Temporary physiological albuminuria
This phenomenon may be temporary and refer to manifestations of a transient nature. It can be identified:
- After the body has undergone significant physical stress. As a rule, this happens to athletes during competitions.
- From a rich diet, which is based on meat, eggs, and whole milk.
- In infants, when their mothers overfeed them.
- In women who are pregnant.
In such cases, the protein level reaches one gram, but then everything disappears on its own, without being accompanied by symptoms of kidney damage, the formation of casts or hematuria.
When protein levels are between thirty and three hundred milligrams, microalbuminuria is diagnosed, and in the case of higher levels, macroalbuminuria is diagnosed.
When studying albuminuria in pregnant women, one should be more careful, since exceeding the value is a symptom of preeclampsia.
Albuminuria in pathology?
This condition corresponds to two mechanisms of deviations:
- Glomerular. It appears to be an enhanced version of the permeability of basement membranes. Through the widened passages formed during diseases, small and large protein molecules enter the primary urine.
- Tubular. It occurs when the basement membrane is in a normal state. As a result, few proteins penetrate into the primary biological fluid. Once in the tubular apparatus, they accumulate because the reabsorption process is not ensured.
There are so many albumin molecules that the channel does not have time to reverse absorption so that they return to the blood again.
These mechanisms are included in the pathogenesis of various kidney diseases. The most important importance in diagnosing proteinuria is given to the choice of treatment method for developed renal failure.
Causes and types of pathological albuminuria
This condition is characterized by an increased protein content in the daily urine norm, the presence of leukocyte and erythrocyte cells, casts, dangerous microorganisms, salt deposits, and epithelial cells contained in the sediment. Albuminuria is classified into extrarenal and renal.
In the first condition, protein appears in the urine for the following reasons:
- in the form of impurities of inflammatory processes occurring in the organs of the digestive tract;
- from blood cells destroyed during anemia;
- with massive burns of the skin;
- from injuries that damage or tear muscle tissue;
- with hypothermia and frostbite.
In urology, most observations occur in situations with hematuria of various origins. True proteinuria is constantly accompanied by inflammatory processes and the breakdown of renal tissue, affecting the basement membranes, increasing their permeability to protein molecules.
This mechanism often occurs during glomerulonephritis, renal amyloidosis, nephrotic sclerosis, nephropathy in women during pregnancy, abnormalities in blood circulation in the kidneys, toxic effects of poisons and certain medications.
Content in urine in arterial renal hypertension
Arterial renal hypertension can also be a consequence of diabetes mellitus, in particular, diabetic nephropathy that arises against its background. Other causes of high blood pressure include:
- Spasm, atherosclerotic damage to the renal arteries or their thrombosis;
- Impaired filtration function of the kidney;
- Activation of the renin-angiotensin-aldosterone system.
As a result of these disorders, the permeability of the renal filter increases and albumins penetrate into the urine in large quantities.
There are no differences in the clinical picture of arterial hypertension of renal origin from essential hypertension. Symptoms will also include discomfort in the heart area, headache, dizziness, palpitations, and shortness of breath. For differential diagnosis, it is necessary to collect a thorough medical history (find out the presence of concomitant diseases, duration of symptoms), conduct a 24-hour urine test for albumin, and a general blood and urine test. In case of renal arterial hypertension, kidney pathologies are detected during the examination.
Treatment begins with relief of the underlying disease. The difference between renal hypertension and essential hypertension is its rapid malignant course. Therefore, surgical treatment of this hypertension is preferred:
- Balloon angioplasty to expand the lumen of the renal artery;
- Placement of a microprosthesis on the affected vessel;
- In case of prolonged progression, when operations are ineffective, it is advisable to remove the affected kidney.
Medications include captopril (an angiotensin II blocker) and propanolol, as it reduces renin production.
How to take a daily protein test
In order for the results of the study to be reliable, the following rules must be observed before submitting the analysis:
- One day before the expected urine collection, stop taking anticoagulants and diuretics (consult your doctor).
- Eliminate alcohol, coffee, tea from your diet. Limit meat consumption to 200–300 g per day.
- It is advisable to buy a special container at the pharmacy for collecting urine or prepare a container yourself (for example, a three-liter jar);
Urine collection algorithm:
- Before urinating for the first time in the morning, thoroughly wash the external genitalia.
- The first portion of urine is not collected, but the time of urination is recorded.
- Subsequent portions of urine are collected in a special container, including at night.
- It is advisable to store collected urine in a cool place.
- After collecting the last portion, it is necessary to mix all the liquid and seal the vessel.
- Take the vessel to the laboratory. If indicated, pour the indicated volume into a smaller vessel.
- All liquid you drink should also be recorded.
If all points were completed correctly, the analysis will show a reliable result. It is worth remembering that if hygiene rules are not followed, external pollutants can enter the urine - vaginal secretions, sperm residues.
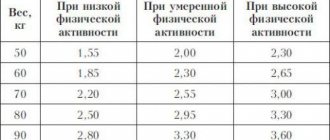
Daily protein standards for people of different ages
Depending on age, the normal amount of protein in urine may vary:
- In adult men and women - up to 0.05 g/day.
- Children under 14 years old - up to 0.07 g/day.
- Pregnant women - up to 0.5 g/day.
In any case, the detection of protein in the urine is a reason to prescribe other studies - ultrasound of the kidneys, general blood test.
Video about proteinuria in pregnant women from the Union of Pediatricians of Russia
Reasons for appearance
- Various kidney pathologies (amyloidosis, obstructive uropathy, pyelonephritis, etc.),
- High blood pressure.
- Metabolic syndrome (a set of disorders of the body, as a result of which the mass of fat increases, and there is a risk of cardiovascular diseases),
- Diabetes.
- Nephropathy in pregnant women (kidney damage in late pregnancy, including edema, immunity disorders, etc.)
- Heart failure.
- Renal circulatory disorders.
- Poisoning with toxic substances or drugs.
- Myeloma (cancer of the bone marrow).
Symptoms
The danger of the pathology lies in the absence of a clinical picture at the initial stage. A person does not have any complaints with albuminuria up to 30 milligrams per day. Symptoms of the disease occur in the prenephrotic stage. The patient may feel an increase in blood pressure above 140 to 90. Sometimes a person complains of pain in the head and in the heart area. The prenephrotic stage is accompanied by episodic attacks of arterial hypertension. The nephrotic stage of the pathology leads to changes in the renal glomeruli. Some of them are replaced by connective tissue, so they allow larger molecules - creatinine, red blood cells - to pass through. The described stage is accompanied by a constant increase in blood pressure numbers. Sometimes patients notice slight swelling on the face in the morning.
The final stage of uremia is characterized by gross disturbances in the structure of the kidneys. The patient loses several grams of protein per day, and red blood cells also enter the urine. At the last stage of the disease, massive swelling develops that does not go away in the evening. They are localized on the upper and lower extremities, face, and body cavities. Arterial hypotension reaches 180/100 or more, it is difficult to treat. Anemia occurs due to loss of red blood cells. The patient's skin becomes pale, he complains of dizziness and weakness. This stage requires hemodialysis, otherwise the person will fall into a coma.
Main symptoms
A mild form of albuminuria hardly manifests itself at all, but with a significant presence of protein, multiple edema . If this happens for a long time, the following signs appear, signaling the disease:
- Nausea, possible vomiting.
- Dizziness.
- Constant weakness and fatigue.
- Pain in joints and bones.
- Chills.
- Pain in the lower abdomen.
- Fever.
- Headache.
- The urine becomes cloudy or has a red tint due to the passage of red blood cells.
- Feverish condition.
- Reluctance to consume food.
If albuminuria occurs due to heart disease, the patient may feel shortness of breath when moving or at rest, arrhythmia appears, pain radiating to the left, in the shoulder blades, and an increase in blood pressure is observed.
Symptoms of albuminuria
It is necessary to focus on the fact that such a problem is not isolated as an independent disease. It serves as a symptom of changes that are functional or pathological in nature. With a disease of a paired organ, there is a likelihood of certain manifestations:
When albuminuria occurs as a result of heart disease, a person begins to experience:
- retrosternal pain radiating to the left shoulder blade;
- arrhythmia;
- increased blood pressure associated with pain in the head;
- shortness of breath when moving and even at rest.
There is no special treatment for this problem. The pathology is treated taking into account pathogenetic pathogenic phenomena. The disappearance or decrease in protein present in the biological fluid is considered an indicator of a successful treatment course.
For various inflammations of the paired organ, use:
- a restrictive diet that reduces the amount of irritating foods, salt, protein or fatty foods;
- bed rest is mandatory, hospitalization for acute forms of the disease;
- taking antibiotics that do not have nephrotoxic effects;
- getting rid of intoxication by administering Hemodez;
- introducing an alkaline composition that helps remove high levels of acidity;
- Reopolyglucon and Vasodilator, which help correct bleeding in the paired organ;
- cytostatic if there is an autoimmune mechanism;
- ACE inhibitor drugs;
- angiotensin blockers of the second group.
During the treatment course of chronic failure of a paired organ, machine, plasmapheresis or peritoneal hemodialysis is performed. The most effective treatment method is paired organ transplantation.
This disease is treated quite conservatively. The doctor attributes the intake of medications that affect blood microcirculation, improving the process. In addition, therapy is prescribed to relieve symptoms.
What is proteinuria
Proteinuria is a condition in which the amount of protein in the urine is higher than normal. Typically, an insignificant amount of protein is released - approximately 0.05 g per day. In various diseases and some physiological conditions, this figure increases to 3 g per day or more. Physiological proteinuria is normal and does not indicate any pathology. Pathological proteinuria can be a symptom of many diseases that relate to:
- renal apparatus - glomerulonephritis, tubular necrosis, pyelonephritis, various types of nephropathies, nephrosclerosis, renal tuberculosis;
- urinary tract - cystitis, urethritis, prostatitis, vulvovaginitis;
- hematopoietic system - myeloma, monocytic leukemia;
- muscular and skeletal system - bone injuries, muscle necrosis (rhabdomyolysis), myopathies of various origins.
Albuminuria is a narrower concept that involves the excretion of only albumin proteins in the urine. Proteinuria includes various types of proteins, including albumins, globulins, and pathological proteins (for example, in multiple myeloma).
Classification
Proteinuria is divided into pathological and physiological. The first appears during illness and serves as a signal that a malfunction has occurred in the body. The second appears as a result of normal metabolic processes in the body or in conditions that do not pose a threat to health. Proteins are also excreted in the urine in some diseases, but in such cases their detection has no diagnostic value. The level of protein in urine, as a rule, does not exceed 1 g/day. Types of physiological proteinuria:
- nutritional - after eating a large amount of protein foods - meat, beans, eggs;
- emotional - occurs under strong emotional stress, stress, mental overload;
- working - after physical activity, hard work;
- solar - with prolonged exposure to the sun;
- orthostatic - after a long stay in an upright position (walking, running);
- palpation - a small amount of protein is present in the urine after vigorous massage of the kidneys and abdomen;
- congestive - with heart failure;
- centrogenic - for skull injuries, epilepsy, concussion;
When describing diseases, the Greek equivalent of the word “kidney” is used - nephros (nephros). If we are talking about anatomical structures or localization, then the Latin is ren (ren). And Latin is also used when talking about glomeruli - glomerulus (glomerulus) and tubes - tubulus (tubulus).
Newborns may experience transient proteinuria in the first few weeks, which disappears after a few weeks without any consequences.
Pathological proteinuria has a more complex classification. It happens:
- Renal: Glomerular - occurs when the renal filter is damaged. The damaging factor can be toxins and substances that are released during inflammation. But the filter also suffers from the distribution of blood flow and the lack of specific proteins. Similar conditions can occur with hypertension, kidney congestion, glomerulonephritis and glomerulosclerosis (overgrowth of connective tissue in the glomeruli). In turn, renal glomerular proteinuria is divided into 2 more types: selective - in this case, proteins with low molecular weight - albumins, some transport proteins (for example, iron transporters) pass through the filter. Most often occurs with minor disorders, such changes are most often reversible;
- non-selective - observed in severe forms of glomerulonephritis, high molecular weight globulins and other types of proteins appear in the urine.
- Prerenal - the source of free proteins is located somewhere in the body. In this case, the function of the renal apparatus is usually not impaired, but there are too many proteins and they are excreted from the body. As a rule, these are pathological proteins or those that are formed as a result of tissue necrosis and inflammation. This type of proteinuria is observed in myeloma, myopathies, muscle necrosis, incompatible blood transfusion, and diabetes mellitus.
The doctor should always pay attention to the type of protein and its amount in the urine - this helps in making the correct diagnosis.
Traditional medicine against albuminuria
You can get rid of this problem on your own, using alternative medicine. The most popular are a variety of herbs and plants - black currant, butcher's broom, lingonberry leaf, cranberry, bearberry, rowan, propolis and fir, birch buds, etc. Fruit drinks and decoctions are prepared from all this. Most often, patients use the following recipes:
- The cranberries are washed, then the syrup is squeezed out. The remaining squeeze is boiled for fifteen minutes in five hundred milliliters of liquid. The resulting broth is mixed with the squeezed juice and cooled. You can add sugar for taste. It is recommended to drink this drink several times a day.
- Two tablespoons of birch buds are poured with boiling water (one glass) and infused for an hour and a half. Then the mixture must be filtered and drunk three times a day, fifty grams each.
- A couple of tablespoons of parsley seeds or its greens are ground into a homogeneous mass and poured with a glass of boiling water. The infusion must be kept for a couple of hours, then taken in small quantities.
- To prepare a healing herbal mixture, you will need to mix plantain, rose hips, and string (twenty grams each). Then add fifteen grams of yarrow and horsetail foliage, twenty-five grams of calendula inflorescences. Everything is mixed and ground. To brew, take two spoons of the mixture per half liter of water. The infusion is filtered and taken three times a day;
- Four tablespoons of corn grains are poured with water (500 ml). Cook until the corn becomes soft. The decoction is cooled, filtered and taken three times a day.
To keep the protein in urine at a normal level, you should drink more fluid. It is also recommended to eat fruits and vegetables that have a diuretic effect.
Why is kidney failure dangerous?
Kidney failure is a direct path to hemodialysis or organ transplantation:
- Life expectancy even after a successful operation leaves much to be desired;
- Finding a suitable donor and a surgeon willing to perform the operation is difficult, especially in small towns;
- Purely financially, until recently not everyone could even afford hemodialysis;
- The condition of patients without adequate therapy inevitably worsens.
That is why you need to treat your “filters” with care. The most painful and unpleasant situations arise precisely with them, with incorrect or untimely treatment.
Any hypothermia or injury can end sadly not only for the urinary system, but also for the person himself.
Of course, if the heart or lungs fail, minutes count, but you shouldn’t relax with your kidneys either—days count.
The doctor is not obliged to take care of your health and well-being, these are only your problems . Of course, health workers will try to do everything possible to ease the suffering. But quite often we are really talking only about relief, when it is no longer possible to help, no matter how much you want.
Content in urine during pregnancy
Women during pregnancy should regularly undergo a urine test in order to detect albumin in the urine and prevent the development of late gestosis.
Late gestosis, or late toxicosis of pregnancy, is a complication of a normal pregnancy. Preeclampsia most often occurs in women who have some pathology in the body, but in healthy pregnant women this complication can also occur.
Albumin enters the urine during gestosis due to disruption of the cardiovascular system:
- Spasm of blood vessels;
- Decrease in the volume of circulating blood in the body;
- Violation of microcirculation;
- Cardiac dysfunction;
- Reduced blood supply to tissues, which can result in ischemia and necrosis.
The appearance of albumin in the urine of pregnant women is one of the three symptoms of late gestosis. The other two are swelling and increased blood pressure. Therefore, to prevent the development of this complication, along with a urine test, regular blood pressure measurements are carried out for all pregnant women.
Late toxicosis of pregnancy leads to preeclampsia and eclampsia. These conditions are dangerous for the woman and the fetus, as they can cause:
- Placental abruption;
- Fetal hypoxia;
- Uterine bleeding;
- Convulsions;
- Development of coma.
If the woman is not helped in time, a stroke (cerebral hemorrhage) will occur, which will lead to the woman’s disability or death. There is also a high risk of fetal death. Only regular urine testing for albumin will help to avoid such developments.
If a woman develops preeclampsia or eclampsia, doctors recommend immediate delivery. After the birth of the child, the woman’s condition returns to normal.
What is the normal protein content in urine for adults and children?
Despite the fact that the norm is an extremely low concentration of protein in the urine or its absence, a positive test result does not always indicate kidney disease and, by and large, in rare cases such a study is enough to make the correct diagnosis.
Why can't there be protein in the urine of a healthy person?
The large size of protein molecules does not allow them to penetrate into the urine through the glomeruli. In this regard, a general urine test should normally show the complete absence of protein or the presence of a small amount (“traces”) in a concentration not exceeding 0.033 g/liter.
Even in the presence of an inflammatory process, due to the presence of blood and pus in the urine, the protein level rarely exceeds a concentration of 1 g/liter. Only in extremely severe stages of inflammation and a large amount of blood and pus in the urine can the protein content reach 20 g/liter.
Albuminuria and its types
The presence of proteins in the urine is called albuminuria and there are several types of this phenomenon. The most common is false albuminuria, in which protein appears due to inflammatory processes. Sources of such protein can be foci of purulent and catarrhal processes, both in the pelvis itself and in the bladder or ureters. True albuminuria has several types.
Physiological albuminuria
This is one of the types of true albuminuria, in which the appearance of protein is not associated with disease. Physiological albuminuria is almost always episodic and short-term. Protein in the urine with physiological albuminuria appears due to:
- hypothermia,
- physical activity,
- strong emotions
- consumption of foods containing undenatured proteins (raw eggs, raw milk, etc.).
In patients suffering from epilepsy, the protein content in the urine may increase after an attack.
Functional albuminuria
With functional albuminuria, the presence of protein indicates disturbances in the functioning of the body, however, in this case they are not associated with kidney disease.
Functional disorders of the body can cause orthostatic or cyclic albuminuria (in most cases characteristic of children and adolescents aged 7 to 14 years), allergic albuminuria and the appearance of protein in the urine associated with nervous or mental illnesses.
Congestive processes in the kidneys caused by cardiac decompensation can also cause the appearance of protein in the urine. This phenomenon is also referred to as the functional type of albuminuria.
Pathological albuminuria
This type of disease is also called renal albuminuria, since in this case the appearance of protein in the urine is associated with pathology of the kidney itself.
The pattern of protein excretion in the urine can indicate which disorder is present in each particular case. Thus, a constant, but not too high protein content (up to 5%) is characteristic of acute glomerulonephritis.
With this disease, along with protein in the urine, the concentration of red blood cells may increase.
A slight increase in protein can also be observed in chronic forms of nephritis, however, albuminuria in this case is not a characterizing factor, since regardless of the severity of the disease, the protein content may be insignificant or absent altogether.
A high concentration of protein in the urine is a characteristic sign of nephrosis. This symptom is especially striking in lipoid, sublimate and syphilitic nephrosis. In acute nephrosis, the protein concentration in the urine is higher than in chronic forms of the disease.
Please note that chronic nephrosis causes the presence of protein in the urine for a long time, sometimes for several months. In this case, the protein concentration can fluctuate, changing the value regardless of the course of the disease.
Protein in urine in women
When conducting a study of protein concentration in the urine of women, it is necessary to take into account the physiological state of the patient. Thus, an increase in protein concentration during menstruation and pregnancy may not be associated with any disease.
In the latter case, additional research will be required to determine the type of albuminuria, since the appearance of protein may not be dangerous (associated with changes in the body in the first trimester or with overload in the second or third trimester) or indicate nephropathy of the pregnant woman, which poses a threat not only to health, but also life of a woman and fetus.
Urinary proteins and their characteristic features
By determining the type of urinary protein, one can judge the type of albuminuria.
Acetic protein body in urine
The presence of this substance in urine does not accurately characterize albuminuria. It is obtained by combining protein with chondroitinsulfuric acid and most often appears simultaneously with regular protein.
The acetic-protein body is most often formed when blood circulation in the kidneys is impaired or when the renal epithelium is damaged.
With albuminuria associated with overload, the first to appear is the acetic-protein body (even with normal physical stress), then (if the load norms are exceeded) globulin and albumin can be seen in the urine.
Bence Jones protein body in urine
The appearance of this type of kidney protein is very characteristic. It accompanies osteosarcomas, endotheliomas, lymphatic leukemia, Rustitsky-Kahler disease (multiple myeloma).
Albumosis in urine
Albumoses occur with both false and true albuminuria - with pyelonephritis and paranephritis, cellular decay outside the urinary system (for example, with gangrene or lung abscess), with disorders in the gastrointestinal tract (gastric ulcer, impaired absorption process, etc.), as well as for other pathologies.
False urine protein results
The results of determining the concentration of protein in the urine may not always give the true picture. The results of the analysis can be influenced by external factors and physiological characteristics of the body.
False positive result when determining protein in urine
A urine test can determine the presence of protein based on the following factors:
- taking medications (penicillin, aspirin, sulfonamides, etc.),
- increased number of leukocytes and erythrocytes (leukocyturia, gross hematuria),
- contamination of the sample with secretions (vaginal, urethral, sperm, etc.).
False negative result when determining protein in urine
The presence of protein may not be detected during a general urine test in the following cases:
- urine has a relative density below 1.015,
- Urine pH is above 7.5,
- urease-positive microflora is present in the urine,
- the protein is represented by specific species (for example, myoglobin or Bence-Jones protein).
Source: https://yrolog.com/analizy/kakaya-norma-soderzhanie-belka-v-moche-u-vzroslyh-i-detej.html
Prevention
The basis for the prevention of microalbuminuria is the prevention of vascular pathologies. It is recommended to stop smoking, drinking alcoholic beverages, and eating foods with large amounts of animal fats. To prevent vascular diseases, you should lead an active lifestyle and engage in physical activity. If diabetes mellitus is detected, the patient should constantly monitor glucose levels and prevent its increase. If there are renal pathologies, a person is not recommended to self-medicate, but to follow all the doctor’s recommendations. Most often, the development of chronic nephropathies is associated with late seeking medical help.