Proteinuria - the presence of protein in the urine - is detected as a result of laboratory urine testing. Clinically, it does not manifest itself; protein in the urine can only be determined through laboratory diagnostics. Many people mistakenly believe that proteinuria is a disease.
In fact, proteinuria is a symptom, a sign of kidney dysfunction. Large loss of protein in the urine is usually considered the main symptom of nephrotic syndrome. People suffering from diabetes have to become closely acquainted with it. As such, proteinuria indicates kidney pathology or damage to the urinary tract.
The formation of proteinuria in the human body
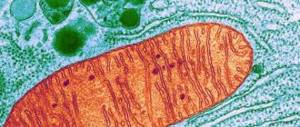
As part of their primary function, the kidneys filter small amounts of protein from the bloodstream.
This is how it appears in primary urine. Next, the mechanism of protein reabsorption in the renal tubules is triggered. The result of the functioning of healthy kidneys and the absence of excess proteins in the blood plasma is the presence of a small amount of protein in secondary urine (the fluid that is excreted from the body).
A laboratory test of urine does not detect proteins at this concentration, or gives a result of 0.033 g/l.
Exceeding this value is called proteinuria - the content of protein in urine in large quantities. This condition is a reason for further diagnosis in order to identify the causes of the disorder.
Causes
The kidneys perform the function of preventing the removal of necessary proteins from the human body. They have a filter consisting of many small vessels, and when it is damaged due to some factors, the membranes of the vessels increase.
Due to inflammatory processes in the kidneys or in the presence of cardiovascular diseases, blood flow is disrupted, which is why this condition occurs. The pores in the filter increase, allowing the protein to pass freely into the urine.
The reasons may also be related to the functioning of the nervous system. When a person experiences stress or other negative emotions, blood vessels constrict.
The phenomenon can also occur in extreme heat due to excessive sweating after taking a cold shower. A false positive test for protein in women can occur immediately after the end of menstruation.
Forms
Based on the content of certain proteins in plasma and urine, the following types of proteinuria are conventionally distinguished:
- selective;
- non-selective.
By localization:
- glomerular;
- tubular.
By etiology:
- “overflow” proteinuria;
- functional proteinuria: orthostatic;
- idiopathic;
- tension proteinuria;
- febrile proteinuria.
[18], [19], [20], [21], [22], [23], [24], [25], [26]
When is the test ordered?
Daily proteinuria (testing must be done periodically during pregnancy and diagnosed renal dysfunction) is carried out to assess the effectiveness of glomerular filtration, as a result of which primary urine is formed.
In pathological conditions of the organ, the semi-permeable membrane membranes are damaged and their subsequent deformation occurs. This leads to the appearance of foci of inflammation. As a result, large elemental conglomerates do not penetrate through the biological filter.
Their content in daily urinary secretions makes it possible to assess the degree of damage and judge the course of the pathological process.
This laboratory test is prescribed for:
- exacerbation of autoimmune diseases;
- acute and chronic glomerulonephritis of infectious-inflammatory etiology, characterized by damage to the glomerular filtration mechanism;
- malignant hyperplasia of any localization;
- diabetes mellitus;
- hypertension;
- multiple myeloma;
- macroglobulinemia;
The suspended content of protein fragments in daily urinary secretions acts as a marker of oncological pathologies, endocrine disorders, and difficult pregnancy. Such an examination is prescribed during the period of remission of chronic diseases to monitor the patient’s condition.
Types of proteinuria
Proteinuria is divided into a number of classifications:
- secretory proteinuria;
- tubular proteinuria;
- albuminuria;
- isolated;
- postrenal;
- marching;
- transient;
- massive;
- glomerular proteinuria.
In connection with diseases, proteinuria is divided into the following types:
- functional;
- pathological
Based on its composition, proteinuria is divided into selective and non-selective.
Secretory proteinuria
Secretory proteinuria is also called Tamm-Horsfall proteinuria. Tamm-Horsfall protein (THP) is produced exclusively by renal tubular cells of the distal loop of Henle.
Secretory proteinuria:
- It is the most abundant bladder protein in mammals.
- The physiological function of TNP remained unexplored for more than half a century. However, new lines of research are positioning it as a central antimicrobial molecule. This molecule fights urinary tract infection (UTI).
- With secretory proteinuria, the highest level of release of Tamm-Horsfall protein is observed, produced by the surface of the distal tubules.
Tubular proteinuria
Features of the disease:
- Quantitative determination of protein in urine by colorimetric method with pyrogallol red
- with tubular proteinuria, low molecular weight proteins are released;
- albumin content in urine is low;
- the analysis reveals the presence of globulins α2 and β2;
- quantitatively, tubular proteinuria is usually insignificant;
- proximal tubules lose their ability to absorb fluids from the body cavities, including low molecular weight plasma proteins.
Glomerular proteinuria
Features of the disease:
- glomerular proteinuria is the most common type of this disease;
- the disease is caused by glomerular pathology and abnormal capillary permeability;
- correlates with disease progression and development of EPR.
Currently, therapy is aimed at reducing proteinuria. This is done to reduce further damage to the filter and as a marker of remission.
Other proteinuria
Physiological proteinuria can be caused by a number of temporary conditions:
- late pregnancy;
- intense running;
- long hikes;
The following types are also observed:
- emotional – for nervous breakdowns, severe emotional states, conflicts;
- palpation – occurs with long-term palpation of the lower abdomen and kidney area;
- nutritional – causes the appearance of excessive amounts of protein in the patient’s diet;
- centrogenic – associated with brain damage;
- febrile - provoked by elevated temperature.
Symptoms and signs of proteinuria
There are functional and pathological proteinuria. The first occurs under the influence of some external factors, the second may be caused by the development of pathological processes in other organs.
Types of functional proteinuria:
- transient proteinuria - occurs during heavy physical exertion, when eating large amounts of protein foods (alimentary proteinuria), after suffering stress, during hypothermia. The appearance of protein in the urine in these cases is associated with the physiological characteristics of the kidneys. Does not require treatment;
- orthostatic proteinuria - in young people, protein appears in the urine when standing for a long time or when walking for a long time. In the supine position, proteinuria disappears and does not require treatment. Pathological proteinuria is a sign of dysfunction of the urinary system.
Types of pathological proteinuria:
- prerenal proteinuria - detected during the breakdown of tissue protein, for example, during burn disease, during a tumor process, hemolysis of erythrocytes, etc.;
- renal - proteinuria associated with kidney damage. It is divided into glomerular, tubular and mixed proteinuria, in which both the tubules and the renal glomeruli are involved in the pathological process;
- Postrenal proteinuria occurs with cystitis, urethritis and inflammatory processes of the genital organs.
In the postrenal form of proteinuria, a large number of leukocytes and gross hematuria are determined in the urine.
In the renal form of proteinuria with damage to the glomerular filter, the permeability of the walls of the glomerular epithelium is impaired, and protein reabsorption is impaired. If the filtration of low molecular weight proteins is impaired, selective proteinuria develops.
Selective proteinuria is detected with minor damage to the glomerular apparatus and is reversible. Nephrotic syndrome is minimally expressed and, with proper treatment, is reversible.
Nonselective proteinuria is characteristic of deeper damage to the glomerular apparatus and is manifested by the loss of high molecular weight proteins. It appears in chronic and acute forms of glomerulonephritis, diabetic nephropathy, renal amyloidosis, autoimmune and systemic diseases.
Tubular proteinuria is associated with damage to the proximal tubules, which lose the ability to reabsorb protein filtered in the glomeruli. Appears with pyelonephritis, congenital pathologies with damage to the tubular filter. If more than 3 grams of protein is excreted from the body in the urine during the day, nephrotic syndrome develops with severe edema and chronic renal failure.
Transient proteinuria
- Excretion of protein in urine is possible due to fever, inflammatory diseases (for example, urinary tract infections) or physical exertion. Typically, no more than 1 g of protein is excreted per day. In patients with epidemic nephropathy, the level of proteinuria at the onset of the disease can be up to 10 g/day, but it decreases over the next few days. A month after the illness, proteinuria may completely stop.
- Resolution of proteinuria should always be confirmed by repeated rapid urine tests. If the rapid test results are twice negative, further studies are not indicated.
Which doctors should you contact if you have proteinuria?
Test systems are used to determine proteinuria. These are standard strips and protein precipitation with acids - sulfasalicylic or trichloroacetic. Subsequently, the protein concentration is determined using nephelometry or refractometry methods.
The biuret method and the Kjeldahl method are recognized as more accurate. They detect the amount of protein in tissues and fluids using the azotometric method. These methods of protein chemistry and radioimmunoassays make it possible to detect various low-molecular and high-molecular proteins in urine. The following are presented for analysis:
- prealbumin,
- albumin acid glycoprotein,
- beta2-microglobulin,
- alpha 1-antitrypsin,
- alpha lipoprotein,
- siderophyllin,
- ceruloplasmin,
- haptoglobin,
- transferrin,
- a2-macroglobulin,
- gamma globulin.
Prevention
Unfortunately, there are no specific recommendations for the prevention of proteinuria. The only thing that can be said with certainty is that you need to see a specialist. Prompt assessment, diagnosis, treatment and long-term monitoring of patients' health can significantly prevent potential progression of the underlying disease process.
Limiting protein intake is often required. However, patients should receive adequate daily protein intake depending on their age. A positive response to proteinuria is an indicator of a good prognosis. This reaction is also a predictor of high survival, stabilization of renal function, as well as subsequent changes in glomerular filtration rate.
Familiar to many phrases, “They found protein in a urine test,” in medical language it sounds briefly: proteinuria. This is what is called the increased concentration of polypeptide amino acid compounds, proteins, in the composition of urine excreted from the body.
Most often, a patient who has laboratory-diagnosed proteinuria first thinks about something like a urogenital infection or kidney inflammation - and indeed, in many cases the reason lies precisely in this. However, the most well-known existing classifications of proteinuria (according to Bergstein, Robson, etc.) number over twenty different types and types, divided into several large groups. There is also a separate nosological code in the International Classification of Diseases: N06, “Isolated proteinuria with specified morphological lesion,” which, in turn, suggests a number of subtypes.
An increased protein content in the urine may be a physiological, natural reaction of the body to certain conditions - a transient reaction, not associated with any pathology of the urinary system and leaving no consequences. However, in most cases, this is still a symptom, a sign of nephrological trouble, which (even in the absence of other symptoms, or, more accurately, especially in this case) requires further research and clarification.
- Daily proteinuria how to test
Our clinic has specialized specialists on this issue.
(17 specialists)
What to do?
Protein in the urine during pregnancy is a serious symptom that requires medical supervision. It is necessary to find the cause of proteinuria as early as possible in order to prevent the development of severe gestosis and its complications. The combination of proteinuria and the following symptoms deserves special attention:
- swelling of the lower extremities, arms or face;
- increased blood pressure;
- headache;
- severe weakness;
- pain in the lumbar region;
- the appearance of pus or blood in the urine.
If any of these symptoms appear, you should definitely consult a doctor. After determining the cause of proteinuria, the detected pathology is treated and the accompanying complications of pregnancy are corrected.
How to prepare for the test
No special measures are required, but some nuances are worth considering:
- You must notify your doctor about taking any medications on an ongoing basis and, if necessary, agree with him on the advisability of their use on the day of the test;
- do not change the drinking regime, both before and during urine collection;
- do not eat unusual foods, follow your usual diet;
- exclude alcoholic drinks;
- the day before the test, you should stop taking diuretics and vitamin C;
- avoid physical and nervous overload;
- If possible, provide the body with adequate sleep.
Treatment of proteinuria with traditional methods
Treatment of proteinuria may require a sufficient amount of time, and conservative therapy prescribed by a doctor is used in courses. Together with medications or in between them, the use of folk remedies is allowed, which you should definitely notify your doctor about. Discuss with him which of the following recipes is suitable in your particular case:
- parsley seeds - 1 tsp. grind the seeds in a coffee grinder or mortar until a powder forms, add a glass of boiling water and leave for several hours; take small sips throughout the day;
- birch buds - 2 tbsp. place the kidneys in a thermos and brew with a glass of boiling water; after 1.5 hours, strain; drink 50 ml three times a day;
- corn - 4 tbsp. pour 500 ml of boiling water over corn grains and simmer over low heat until the grains soften; Strain the broth and drink throughout the day, prepare a new one the next morning;
- oats - 5 tbsp. pour oat grains (not flakes!) into a liter of water and boil until softened; drink small portions throughout the day;
- lingonberries - pour 20 grams of crushed lingonberry leaves with a glass of boiling water, leave for 20-30 minutes, strain; take 1 tbsp. three times a day;
- bearberry – 1 tbsp. Grind the bearberry, brew in three glasses of water and simmer over low heat until the broth has reduced by three times; strain; drink small portions throughout the day.
Non-plasma (tissue) uroproteins
In addition to blood plasma proteins, there may be non-plasma (tissue) proteins in the urine. According to Buxbaum and Franklin (1970), non-plasma proteins account for approximately 2/3 of all urine biocolloids and a significant part of uroproteins in pathological proteinuria. Tissue proteins enter the urine directly from the kidneys or organs anatomically associated with the urinary tract, or enter the blood from other organs and tissues, and from it through the basement membranes of the glomeruli of the kidney into the urine. In the latter case, excretion of tissue proteins into the urine occurs similarly to the excretion of plasma proteins of various molecular weights. The composition of non-plasma uroproteins is extremely diverse. Among them are glycoproteins, hormones, antigens, enzymes. Tissue proteins in urine are detected using conventional methods of protein chemistry (ultracentrifugation, gel chromatography, various types of electrophoresis), specific reactions to enzymes and hormones, and immunological methods. The latter also make it possible to determine the concentration of non-plasma uroprotein in the urine and, in some cases, to determine the tissue structures that became the source of its appearance. The main method for detecting non-plasma protein in urine is immunodiffusion analysis with antiserum obtained by immunizing experimental animals with human urine and subsequently depleted (adsorbed) by blood plasma proteins.
Diagnostics
All laboratory methods for detecting protein fractions in urine are divided into quantitative, semi-quantitative and qualitative. Quantitative laboratory methods for determining proteinuria are divided into colorimetric and turbidimetric. Semi-quantitative methods for identifying this condition include the following research options:
- Determination of protein fractions in urine using special diagnostic test strips.
- Brandberg-Roberts-Stolnikov technique.
To qualitatively determine proteinuria, the following laboratory methods are used:
- Boiling test.
- Heller ring test.
Detected proteinuria during pregnancy can be normal only if its value does not exceed 30 mg. If this indicator is from 30 to 300 mg, then we are talking about the development of microalbuminuria. When the value of protein fractions increases above 300 mg, microalbuminuria is diagnosed in pregnant women. This condition indicates the development of preeclampsia.
Medium molecules of blood and urine
Medium molecules (MM), otherwise called protein toxins, are substances with a molecular weight of 500-5000 daltons. Their physical structure is unknown. The composition of SM includes at least 30 peptides: oxytocin, vasopressin, angiotensin, glucagon, adrenocorticotropic hormone (ACTH), etc. Excessive accumulation of SM is observed with a decrease in kidney function and a large amount of deformed proteins and their metabolites in the blood. They have a diverse biological effect and are neurotoxic, cause secondary immunosuppression, secondary anemia, inhibit protein biosynthesis and erythropoiesis, inhibit the activity of many enzymes, and disrupt the phases of the inflammatory process. The level of SM in blood and urine is determined by a screening test, as well as by spectrophotometry in the ultraviolet zone at wavelengths of 254 and 280 mm on a DI-8B spectrophotometer, as well as dynamic spectrophotometry with computer processing in the wavelength range 220-335 nm on the same spectrometer from Beckman . The content of SM in the blood is taken as the norm equal to 0.24 ± 0.02 arb. units, and in urine - 0.312 ± 0.09 arb. units Being normal waste products of the body, they are normally removed from it at night by glomerular filtration by 0.5%; 5% of them are disposed of in other ways. All SM fractions undergo tubular reabsorption.
What does the analysis for daily proteinuria show?
A laboratory test can determine the amount of protein passing through the urinary system. The formation of urine for removal from the body occurs by filtration of the plasma fraction of blood circulating through the glomerular filtration apparatus of the tubules.
The following are released into the urine:
- enzymatic substances;
- epithelial cells exfoliated due to inflammation;
- organic substances;
- metabolites of pharmacological compounds when taking medications;
- excess trace elements and minerals entering the body with food;
- non-digestible elements;
- protein proteins.
In the subsequent phase of the filtration process, secondary absorption of nutrients occurs, including proteins and glucose. Such urine contains products of material metabolism and protein breakdown.
In cases of renal function disorders, the physiological mechanism fails. Substances in higher than normal concentrations are released into the urine. Such an analysis gives the urologist the opportunity to differentiate the etiological factors of deviations in laboratory parameters.
Etiology
The reasons for the progression of proteinuria in patients are quite varied. But it is worth noting the fact that they are the same in both adults and children. As a rule, the main cause of proteinuria is pathologies of the kidneys and the urinary system as a whole.
Proteinuria progresses against the background of such ailments:
- – one of the most common causes of proteinuria;
- myeloma;
- tubular proteinuria;
- renal vessels;
- glomerular proteinuria;
- acute tubular necrosis;
- diabetic glomerulosclerosis;
- potassium kidney;
- congestive kidney;
- myoglobinuria;
- hemoglobinuria.
Proteinuria can also be caused by. Often it appears in the background. The reasons for the increase in protein concentration in urine in children and adults include the presence of malignant damage to vital organs (heart, brain, lungs, etc.).
Folk remedies
At home, it is allowed to carry out treatment with folk remedies, but only with the consent of the attending physician. One of these is cranberry, which helps reduce the percentage of protein in urine. Some recipes:
- the berries are washed, the juice is squeezed out, and the cake is boiled for 20 minutes, then the broth is cooled, filtered, poured with juice and consumed internally instead of tea throughout the day (you can add honey or sugar to taste);
- Mash the berries with a fork, pour 200 ml of boiling water, leave for 30 minutes, and consume orally throughout the day.
Cranberry is useful for proteinuria.
Infusions prepared from the following ingredients are effective in the treatment of proteinuria: parsley: plant seeds in a volume of 1 tbsp. l. grind
- until it becomes a powder, pour 200 ml of hot water, leave for 2 hours, then filter, take 10 ml orally three times a day;
- birch buds: a few tablespoons of dried buds are poured into 200 ml of hot water, infused for an hour and a half, consumed orally, half a glass three times a day;
- linden, lemon: 1 lemon is crushed, mixed with crushed linden leaves in a volume of 20 g, poured with hot water (200 ml), infused for 24 hours, taken orally 1 tsp. three times a day before meals.
The main causes of increased urine protein
The following etiological forms of proteinuria are distinguished:
- Proteinuria is a symptom that can tell you a lot about your body.
- Cardiac (congestive) develops with heart failure;
- Renal (true) appears when there is a change in glomerular permeability;
- False is characterized by an increase in urine protein directly in the urinary tract in the presence of inflammation;
- Lordotic (orthostatic) is provoked by lumbar lordosis, causing venous stagnation of the pelvis;
- Paroxysmal (epileptic) accompanies an attack of the disease;
- Palpation is formed by feeling the lower back with your fingers;
- Sports – for people engaged in active physical labor;
- Transient (muscular) proteinuria is observed with strong muscle loads.
There are a number of dangerous diseases in which pathological protein appears in urine: hemolytic anemia, paraproteins, liver disease.
How long to wait for research results
Analysis of daily diuresis does not require specific equipment and the use of time-consuming technology. During the study, the laboratory assistant evaluates the volume of urinary fluid excreted within 24 hours and the ratio of the conditionally daily portion to the night portion.
A healthy adult produces 3 times more urine during the waking phase than during sleep. The total amount of urine is 75-80% of the fluid consumed during the control period.
The analysis result is ready 1-2 hours after the start of processing of the biological material. If the laboratory has a waiting list of patients, they usually ask to pick up the printout the next day after delivery.
Proteinuria severity
Depending on the severity, mild, moderate and severe proteinuria are distinguished.
Mild proteinuria
Mild proteinuria (from 300 mg to 1 g/day) can be observed with acute urinary tract infection, obstructive uropathy and vesicoureteral reflux, tubulopathies, urolithiasis, chronic interstitial nephritis, kidney tumors, polycystic disease.
Moderate proteinuria
Moderate proteinuria (from 1 to 3 g/day) is observed in acute tubular necrosis, hepatorenal syndrome, primary and secondary glomerulonephritis (without nephrotic syndrome), and the proteinuric stage of amyloidosis.
Severe (pronounced) proteinuria
Severe or severe proteinuria is defined as a loss of protein in the urine exceeding 3.0 g per day or 0.1 g or more per kilogram of body weight in 24 hours. Such proteinuria is almost always associated with dysfunction of the glomerular filtration barrier in terms of protein size or charge and is observed in nephrotic syndrome.
Detection and quantitative assessment of proteinuria are important both for diagnosis and for assessing the course of the pathological process and the effectiveness of treatment. In conclusion, it should be noted that the diagnostic significance of proteinuria is assessed in conjunction with other changes in the urine.
Development factors
If a person’s urine analysis reveals severe proteinuria, the reasons may be hidden behind the following conditions:
- Congenital diseases (Fabry disease).
- The presence of benign and malignant neoplasms.
- Glomerulonephritis.
- Idiopathic nephrotic syndrome.
- Lowe's syndrome.
- Proximal renal tubular acidosis.
- Wilson-Konovalov disease.
- Intoxication with salts of heavy metals.
- Hypervitaminosis of vitamin D.
- Hypokalemia.
- Taking medications with antibacterial activity (sulfonamides, penicillins).
- Presence of cysts in the kidney area.
- Acute form of tubular necrosis.