Causes
Before considering the symptoms of hypercortisolism, we need to briefly talk about the pathology itself. There are only two reasons why this may occur:
- Long-term treatment with glucocorticoids.
- Increased secretion of cortisol by the adrenal cortex.
In simpler terms, the reason always lies in a hormonal imbalance. Cortisol itself, synthesized by the pituitary gland, is vital for the body, because it is a regulator of carbohydrate metabolism, as well as a direct participant in the development of stress reactions.
Some people, due to their profession, have constantly elevated levels of this hormone. Athletes are usually susceptible to this. Cortisol is also actively produced in the bodies of women carrying a fetus. In pregnant women, the level of this hormone increases significantly in the last months of pregnancy.
Cortisol is also produced in large quantities by alcoholics, heavy smokers and drug addicts. Also at risk are people suffering from any mental disorders.
What role do adrenal hormones play?
A prolonged increase in the circulatory system of hormones produced by the adrenal glands causes the occurrence of hypercortisolism syndrome. This disease is characterized by the failure of all metabolic processes and disruption of the functioning of important body systems. The factors that led to hormonal imbalance are mass formations of the adrenal glands, pituitary gland and other organs, as well as the use of medications that contain glucocorticoids. To eliminate the manifestation of the disease, various medications are prescribed, and the neoplasm can be affected by radiation or it can be removed from the body surgically.
The adrenal cortex produces steroid-type hormones—mineralcorcortinoids, androgens, and glucocorticoids. Their synthesis is controlled by adrenocorticotropic hormone, for example, corticotropic hormone or ACTH. Its production is regulated by the reeling hormone, vasopressin of the hypothalamus. Cholesterol is a common source for the production of steroids.
Symptoms of hypercortisolism
The most active glucocorticoid is cortisol. An increase in its amount leads to a stop in the synthesis of corticotropin due to feedback. Thanks to this, hormonal balance is maintained. The production of the main mineralocorticoid hormone, that is, aldosterone, is less dependent on ACTH. The main corrective mechanism of its synthesis is the renin-antiotensin system, which responds to changes in the volume of circulating blood. Diagnosis of hypercortisolism is based on passing the necessary tests; after receiving the result, the attending physician prescribes appropriate treatment.
They are produced in large quantities in the glands of the reproductive system. Glucocorticoids affect all types of metabolic processes. They increase glucose levels in the circulatory system, promote the breakdown of protein and the redistribution of adipose tissue. Hormones have an anti-inflammatory and calming effect, promote sodium retention in the body and increase blood pressure.
Predisposing factors
Symptoms of hypercortisolism can be expected in the event of one of the following circumstances:
- The presence of a hereditary predisposition (problems with the endocrine system in relatives).
- Completion of a long therapeutic course, which involved taking glucocorticoid hormones. The risk is especially high when using dexamethasone and prednisolone.
- The presence of inflammatory processes or tumor formations occurring in the pituitary gland. It is important to note that this predisposing factor is more characteristic of the female body.
- Thyroid or lung cancer.
- Adrenal adenomas (benign tumors).
Forms of the syndrome
Pathology can manifest itself at any age in any gender.
The syndrome differs from the disease in that in the second case, hypercortisolism occurs secondary, and the pathology of the pituitary gland is primary.
In medicine, there are three types of hypercortisolism, which are based on the difference in the causes of the pathology:
- exogenous;
- endogenous;
- pseudo-syndrome.
In medical practice, there are also cases of juvenile hypercortisolism syndrome. Juvenile hypercortisolism is also identified as a separate type and is caused by age-related hormonal changes in the body of a teenager.
Exogenous
Under the influence of external causes, such as the use of drugs containing glucocorticoids for treatment, iatrogenic or exogenous hypercortisolism may develop.
Basically, it goes away after stopping the drug that provokes the pathology.
Endogenous
Factors in the development of endogenous hypercortisolism may be the following reasons:
- pituitary tumors (pituitary microadenoma);
- bronchial tumors;
- testicular tumors;
- ovarian tumors;
- tumor or hyperplasia of the adrenal cortex.
The provoking tumor of the bronchi or gonads is most often ectopic corticotropinoma. It is this that causes increased secretion of corticosteroid hormone.
Pseudo-Cushing syndrome
False hypercortisolism occurs for the following reasons:
- alcoholism;
- pregnancy;
- taking oral contraceptives;
- obesity;
- stress or prolonged depression.
The most common cause of pseudo-syndrome is severe alcohol poisoning. In this case, any tumors are absent.
Classification
She should pay a little attention before talking about the symptoms and diagnosis of hypercortisolism. This pathology comes in three types:
- Endogenous. The disease occurs due to internal disorders occurring in the body. In approximately 70% of cases, the cause is Cushing's disease. This is not a syndrome of the same name. The names are similar, but the pathologies themselves are not similar. Cushing's disease is characterized by increased production of adrenocorticotropic hormone by the pituitary gland. By the way, it stimulates the release of cortisol from the adrenal glands.
- Exogenous. Symptoms characterized by Cushingoid syndrome are most characteristic of this type of hypercortisolism. This is the most common type of pathology. The reason for the formation is long-term treatment with steroids. Typically, glucocorticoids are used to treat rheumatoid arthritis, asthma, or immunosuppression.
- Pseudo-syndrome. Sometimes certain symptoms and manifestations give the impression that a person suffers from hypercortisolism. This may even be indicated by the results of a general diagnosis (which is why it is important to also carry out a differentiated one). Specific symptoms do not always indicate that the patient has true hypercortisolism. And common causes of the development of pseudosyndrome are obesity, pregnancy, alcohol intoxication, depression and stress. Less commonly, taking oral contraceptives containing progesterone and estrogens. Even an infant can experience pseudosyndrome, since substances that are present in the mother’s body and cause this disease enter into his body along with mother’s milk.
Be that as it may, a diagnosis will need to be made and treatment will be prescribed. But which one exactly will be decided by the endocrinologist, taking into account the results of the examination and the specifics of the patient’s body.
results
Somatic mutations and hereditary duplication in cortisol-producing foci
- Genome sequencing was performed on samples from 10 patients with unilateral cortisol-producing adenoma and overt Cushing's syndrome. A low level of somatic mutations was detected in the adenoma.
- Within this small sample of genetic lesions, somatic variation PRKACA, encoding the Cα subunit of PKA, was found in 8 of 10 tumors (c.617A→C, p.Leu206Arg in 7 andc.595_596insCAC, Leu199_Cys200insTrp in 1).
- The affected amino acids were highly conserved across species.
- Complete coding sequences were found in 33 of these samples
- In one case, the defect was inherited: mother and son, both carrying the same PRKACA duplication, suffered from bilateral macronodular hyperplasia.
PRKACA mutation and regulation by the catalytic subunit of the regulatory subunit
- Analysis of the structure of the full-length tetrameric mouse holoenzyme RIIβ(2):Cα(2) revealed that the mutation is located in a highly conserved basis of interaction between the regulatory and catalytic subunits of PKA, data that confirm the functional significance of the Leu206Arg variant.
- Leu206 is the part of the active site cleaved from the catalytic subunit, the inhibitory sequence of which is attached to the regulatory subunit, mimicking the substrate of the catalytic subunit.
- This interaction maintains the catalytic subunit inactivated in the absence of cAMP.
- Exchange of Leu206 with the bulky and positively charged amino acid Arg between the side chains of the mutated Arg206 in the Cα subunit of Val115 and Tyr228 in the RIIβ subunit.
- The functional manifestations of the two identified variants (Leu206Arg and Leu199_Cys200insTrp) were detected in intact cells by FRET microscopy using a protein kinase activity sensor (AKAR4-NES).
- Protein kinase activity in cells transfected only with the same non-mutant Cα or its variants was high and was also not stimulated by cAMP analogues, indicating retention of catalytic activity in the mutant cells.
- However, after retransfection with excess non-mutant RIIβ, basal cellular PKA activity was reduced in cells transfected with non-mutant Cα and rendered susceptible to cAMP analogues.
- And protein kinase activity in the cell transfected with mutant genes remained high and unresponsive to cAMP analogues.
- These data indicate that the mutations render the catalytic subunit resistant to physiological inhibition by the regulatory subunit.
- The lack of suppression persisted when an equal amount of nonmutant Cα was cotransfected, indicating a dominant effect of these mutations.
- Similarly, transfection of the mutant Leu206Arg caused a significant increase in protein kinase activity above basal characteristics, such that protein kinase activity was at the same level as in those cells that were transfected with non-mutant Cα and stimulated with cAMP, in the absence of suppression by cotransfection with RIIβ, which also indicates a deficiency suppression of a mutant catalytic subunit by a regulatory subunit.
Association of PRKACA germline duplication with increased protein levels and protein kinase activity
- When compared with tumor tissue samples from patients without any genetic defects, tumor tissue samples with PRKACA duplications have elevated PKA Cα, messenger RNA, and protein levels.
- Immunohistochemical analyzes confirmed increased expression of the PKA Cα subunit in adrenal tissue from these patients.
- Increased expression of the PKA Cα subunit is associated with increased basal and cAMP-stimulated activity. Clinical phenotype and PRKACA mutation status.
- 22 of 59 patients with overt Cushing's syndrome with unilateral adenomas contained a PRKACA mutation, but this disorder was not present in any adenomas associated with: subclinical Cushing's syndrome (40 patients)
- in inactivated adrenal adenomas (20)
- aldosterone-producing adrenal adenomas (20 patients)
- adrenocortical carcinomas (42 patients)
- in adrenal tissue (10 patients) or lymphatic DNA (35 patients) from patients with ACTH-independent adrenal hyperplasia (35 patients).
Signs of pathology
Now you should pay attention to the symptoms of hypercortisolism. The most characteristic symptom is obesity. It is observed in more than 90% of patients with this diagnosis. Moreover, fat deposits are very uneven. They are localized on the back, stomach, chest, neck, face. The limbs may be relatively thin.
Another symptom of hypercortisolism observed in men and women is a moon-shaped red-purple face with a cyanotic tint. This is also called “matronism”. In addition to this sign, a “menopausal” hump is also noticeable. It occurs due to fat deposition in the area of the VII cervical vertebra.
Changes in the structure of the skin are also observed. It thins out and becomes almost transparent. This is especially noticeable on the back of the hands.
How does this disease manifest itself?
The main symptoms most often appear:
- Obesity;
- Increased blood pressure;
- Muscle weakness;
- Sexual dysfunction;
- Pigment spots may appear on the skin;
- Women grow hair on their chest and face.
Obesity in such patients has a peculiar appearance, that is, subcutaneous fatty tissue accumulates to a greater extent in the supraclavicular region, shoulders and cervical vertebrae, and the abdomen also increases. As a result of the redistribution of fatty tissue, the arms and legs become thin and the muscles atrophy. The face takes on a “moon-shaped” shape, the skin becomes dry and flaky, ulcers appear that are difficult to treat, the cheeks have a purple-red color. Other symptoms include stretch marks on the chest, hips, and abdomen, which are red or purple in color.
The most dangerous manifestation of hypercortisolism is disruption of the heart and blood vessels, which causes arterial hypertension syndrome. As pressure increases, headaches and “fly spots” appear before the eyes. Due to metabolic failure, diabetes mellitus and osteoporosis can develop, which is very severe.
Hypercortisolism leads to a significant decrease in immunity, which serves as a catalyst for the appearance of ulcers, pustules, pyelonephritis, fungal infections of the nails and skin. Symptoms also include nervous system disorders, sleep disturbances, bad mood, and psychosis.
In girls, after the start of the menstrual cycle, amenorrhea (a condition where there are no periods) may occur. Growth and sexual development are delayed, and the voice becomes rough.
Disorders in the muscular system
Continuing to study the symptoms of hypercortisolism (Itsenko-Cushing syndrome), it is also necessary to make a reservation that with this disease, muscle tone and strength decrease, and muscles atrophy. All these changes manifest themselves as signs of myopathy.
Patients also experience “sloping buttocks.” What is this? This is the name of the syndrome in which the volume of the gluteal and thigh muscles decreases. A “frog belly” also appears, manifested by malnutrition.
A hernia of the linea alba is often formed. Preperitoneal tissue and the hernial sac simply “bulge out” through the slit-like spaces of the aponeurosis. This pathology is manifested by abdominal pain, flatulence, constipation, vomiting and nausea. However, its development can be recognized by the presence of a tumor-like protrusion: it is visible to the naked eye.
Symptoms of hypercortisolism
The list of symptoms of hypercortisolism is very extensive and is as follows:
- Weakness that increases over time;
- Permanent fatigue;
- Sleep problems;
- Fatigue;
- Reduced blood pressure;
- Mental asthenia;
- Nausea and vomiting;
- Poor appetite (or lack thereof);
- Stomach ache;
- Constipation alternating with diarrhea;
- Weight loss.
The most pronounced symptoms of Addison's disease include: ever-increasing muscle weakness, deterioration of skeletal and smooth muscles, and melanosis (excessive pigmentation of the skin and mucous membranes).
The first places where melanosis appears are skin folds and grooves. Subsequently, the pigmentation becomes diffuse. Pigmentation occurs in conditions of decreased production of aldosterone and cortisol and an increase in the amount of melanoform hormone secreted by the pituitary gland.
A lack of glucocorticosteroids provokes the development of hypotension and hypoglycemia, weight loss, lack of appetite, as well as the appearance of disturbances in the activity of the cardiovascular system. An absolute decrease in heart size is also quite likely.
In the event of stress reactions to such factors as infections, mental trauma, pregnancy or surgery, rapid dehydration and a significant decrease in blood pressure occur - an Addisonian crisis.
Its clinical manifestations are the following symptoms:
- A fall in the level of chlorine, cholesterol and sodium simultaneously with an increase in the level of nitrogen and glucose (found in the blood);
- Increase in chlorine and sodium levels (detected in urine).
Skin changes
Continuing the story about the causes and symptoms of hypercortisolism, it should be noted that the integument of people suffering from this disease has a characteristic “marble” tint. The skin has an obvious vascular pattern; it is prone to dryness and flaking, in some places interspersed with isolated areas of sweating.
If you pay attention to the skin of the thighs, buttocks, abdomen, mammary glands and shoulder girdle, you can notice stretch marks. These are stretch marks of cyanotic or purple color, the length of which starts from a couple of millimeters and sometimes reaches 8 cm. Their width is frightening: stretch marks can reach 2 cm.
Patients also suffer from acne, spider veins, subcutaneous hemorrhages, and hyperpigmentation in some areas.
Epidemiology of ectopic ACTH syndrome
This disease was first described in 1928 in a patient with lung cancer who had symptoms of hypercortisolism. An autopsy revealed enlarged adrenal glands.
Tumors have also been described that synthesize not only ACTH, but also other hormones. For example, high levels of prolactin, parathyroid hormone, calcitonin. But the most common is ectopic ACTH syndrome .
Most often, ectopic ACTH production is found in lung cancer (50% of all cases), lung carcinoid (10%), and pancreatic tumors (10%).
This syndrome also occurs in medullary thyroid cancer, pheochromocytoma, ovarian, testicular, prostate, esophageal, stomach, and colon cancer. Ectopic ACTH syndrome accounts for 15% of all cases of hypercortisolism. Most often found in men, especially smokers.
Read what the unclear term “pheochromocytoma” means in the article “Everything you need to know about pheochromocytoma.”
Bone problems
Their appearance is also a symptom of hypercortisolism in women and men. In the presence of this disease, bone tissue is damaged and thinned, which leads to the development of osteoporosis. Its signs are severe pain, bone deformation (fractures are also possible), scoliosis and kyphoscoliosis. The thoracic and lumbar regions are especially affected.
Due to compression of the vertebrae, people seem to lose height and become stooped. If Itsenko-Cushing syndrome is diagnosed in a child, then he lags behind in physical development. The reason is a slowdown in the development of epiphyseal cartilage.
HYPERCORTICISM (Cushing's disease and syndrome)
Read:- E Epileptic syndrome
- E. Sjögren's syndrome
- F50-F59 Behavioral syndromes associated with physiological disorders and physical factors
- F59 Unspecified behavioral syndromes associated with physiological disturbances and physical factors.
- I I. COMMON NEUROLOGICAL SYNDROMES.
- I. Acute reflex vertebral syndromes
- I. Syndrome of vegetative (vegetative-vascular) dystonia.
- II. Alcohol withdrawal syndrome
- II. Edema syndrome.
- II. PROLIFERATIVE SYNDROMES IN HEMOBLASTOSES
Hypercorticismus is the general name for a group of syndromes caused by excess levels of corticosteroids in the blood.
Prevalence. A relatively rare disease. Hypercortisolism occurs more often in women aged 20-40 years.
Etiology. There are primary hypercortisolism (Cushing's syndrome) and secondary hypercortisolism (Cushing's disease). Primary hypercorticism (approximately 15% of cases) develops with adenoma (corticosteroma) or adenocarcinoma of the adrenal cortex. Secondary hypercortisolism (about 85% of cases) occurs with infectious and traumatic lesions of the hypothalamus and pituitary adenomas.
Pathogenesis. The pathogenesis of the disease is associated with a violation of the regulatory mechanisms that control the function of the hypothalamic-pituitary-adrenal system. In Itsenko-Cushing's disease, excessive secretion of ACTH occurs, which is the main pathogenetic factor of the disease. Overproduction of ACTH mainly enhances the function of the zona fasciculata and zona reticularis of the adrenal cortex. In Itsenko-Cushing's disease, the sensitivity of the hypothalamic-pituitary system to corticosteroids decreases, resulting in a simultaneous increase in the secretion of ACTH and cortisol.
Increased production of cortisol in Cushing's disease and syndrome leads to arterial hypertension, osteoporosis, obesity, decreased resistance to infections, impaired carbohydrate metabolism and even the development of diabetes mellitus. Strengthening the function of the zona reticularis of the adrenal cortex leads to overproduction of steroids with androgenic properties.
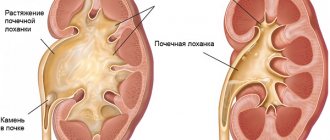
Pathological picture. In a morphological study of the pituitary gland in Itsenko-Cushing's disease, an adenoma of cells secreting ACTH (chromophobe or basophilic adenoma) can be noted; Less common is adenocarcinoma of the anterior pituitary gland. In patients with Itsenko-Cushing syndrome, a corticosteroma is detected, consisting of mixed light and dark cells (adenocortical adenoma). Osteoporosis with spontaneous bone fractures, hypertrichosis and hirsutism are also noted. Histological examination of the skin reveals stretching and death of elastic and collagen fibers, thinning of the epidermis. Nephrolithiasis and chronic pyelonephritis are often found.
Clinical picture. Patients complain of headaches, pain along the spine and in the lower back, increased fatigue, general weakness, sexual disorders (in men - impotence, in women - decreased libido, disrupted menstrual cycle, sometimes amenorrhea), apathy and poor intelligence.
A general examination reveals characteristic features - the so-called Cushingoid appearance. Patients have a rounded, moon-shaped face with a crimson-red blush on the cheeks (matronism), a kind of obesity (sometimes without weight gain) with an increase in the size of the abdomen (“frog belly”), fat deposition in the neck, above the collarbone and in the area of the VII cervical vertebra (“bull scruff”) with significant emaciation of the arms and legs. The skin is thin, dry, flaky, with a purple-marbled pattern. On the skin of the abdomen, shoulders, mammary glands, inner thighs and other parts of the body, wide dystrophic stretch marks of a reddish-violet color (striae) are observed. There are boils and acne on the skin. Women experience male pattern hair growth (hirsutism) with hair loss on the scalp. The growth of vellus hair predominates on the face. Men may experience some feminization, decreased facial hair growth, and hair loss on the body.
In severe cases, there are changes in the skeletal system - osteoporotic changes in the skeleton with compression of the bodies of the thoracic and lumbar vertebrae, displacement of the vertebrae and compression of the spinal cord and nerve roots, fracture of the bones of the spine, collarbone and ribs. Due to a decrease in the body's reactivity, bronchitis, pneumonia, and tuberculosis often occur.
When examining the cardiovascular system, there is an expansion of the border of the heart to the left, an accent of the second tone over the aorta, and a systolic murmur at the apex. Blood pressure is increased.
In some cases, gastroduodenal ulcers (“steroid ulcer”) are found; sometimes they are complicated by gastric bleeding. Many liver functions are impaired. Many patients develop pyelonephritis, characterized by a chronic, latent course, and urolithiasis. With prolonged arterial hypertension, nephrosclerosis develops, which in advanced cases is complicated by renal failure up to the development of uremia.
When examining peripheral blood, an increase in the number of erythrocytes and leukocytes, lymphopenia and eosinopenia are observed. In the active stage of the disease, an increase in fibrinogen levels and a decrease in fibrinolytic activity of the blood are noted. The content of albumin and potassium in the blood is reduced and the level of globulins, sodium and chlorine is increased. Hypophosphatemia is noted, and the activity of alkaline phosphatase is reduced - one of the factors in the development of osteoporosis. Reduced tolerance to carbohydrates, hyperglycemia, and glycosuria are often recorded. With Itsenko-Cushing's disease, the levels of ACTH and cortisol in the blood are increased, and with Itsenko-Cushing's syndrome - only the level of cortisol. The urinary excretion of 17-OX, 17-KS, and cortisol increases.
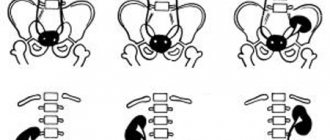
In the topical diagnosis of adrenal lesions, X-ray examination with retropneumoperitoneum or arteriography can be used. Scanning of the adrenal glands using cholesterol labeled with radioactive iodine is also used. Tumors of the pituitary gland (adenomas) may appear on X-ray images as an increase in the size of the sella turcica or its destruction. Computed tomography is used.
Flow. The disease usually develops slowly but progresses steadily.
In terms of severity, hypercortisolism can be mild, moderate, or severe. In mild cases, the symptoms of the disease are moderate. The menstrual cycle is sometimes preserved. Osteoporosis may be absent. Moderate severity is characterized by the severity of all symptoms of the disease without complications. In severe cases, along with a clear picture of the disease, there are complications.
Complications: erysipelas, sepsis, cellulitis, pneumonia, cerebral hemorrhage, renal failure, cardiovascular failure, hypertension, diabetes mellitus, osteoporosis with subsequent bone fractures.
Treatment. The diet should include a limited amount of fat, carbohydrates and fluids with sufficient protein. vegetable are prescribed once a week
For hypothalamic-pituitary forms of hypercortisolism of mild and moderate severity, radiotherapy is used. Drug therapy aimed at blocking pituitary function (parlodel, cyproheptadine or reserpine) can be used. If radiotherapy is ineffective and the disease is severe, a bilateral total adrenalectomy is performed, followed by maintenance therapy with prednisolone in a daily dose of 5-10 mg.
The main treatment for adrenal tumors (Cushing's syndrome) is surgical removal of the tumor. For inoperable tumors, corticosteroid synthesis inhibitors are indicated. For this purpose, chloditan, metopyrone, aminoglutethimide, trilostane are prescribed.
At the same time, prevention and treatment of various complications of hypercortisolism is carried out.
The prognosis of the disease without treatment is unfavorable. Severe forms of the disease lead to early disability and often end in death due to the occurrence of various complications.
7.10. PHEOCHROMOCYTOMA
Pheochromocytoma (phaeochromocytoma) is a hormonally active tumor arising from mature cells of the chromaffin tissue of the adrenal medulla, paraganglia or sympathetic ganglia.
Prevalence. The disease is relatively rare and averages 1-3 cases per 10,000 patients. Pheochromocytoma can occur at any age, but most often occurs between 20 and 50 years in people of both sexes.
Etiology. The cause of the disease is unknown. There is evidence of a genetic predisposition to the development of pheochromocytoma. The literature indicates the possible role of hormonal imbalance in the origin of pheochromocytoma.
Pathogenesis. The pathogenesis of pheochromocytoma is caused by excessive production of catecholamines (adrenaline, norepinephrine, dopamine) by tumor chromaffin cells. Depending on the predominance of adrenaline or norepinephrine, the manifestations of the disease may be somewhat different in accordance with the characteristics of the biological action of these substances. When adrenaline predominates, agitation, tremors, dilated pupils, tachycardia, and hyperglycemia occur. With the predominance of norepinephrine, sweating, bradycardia, increased blood pressure, and an increase in basal metabolism are observed. With excess production of catecholamines, stimulation of the renin-angiotensin system and increased secretion of aldosterone occurs. Due to an excess of catecholamines, the early development of atherosclerosis of the coronary arteries occurs. The concentration of sodium inside the cell increases, and potassium decreases. As a result, necrosis can occur even with unchanged coronary vessels. Prolonged catecholaminemia causes disturbances in carbohydrate metabolism, leading to the development of diabetes mellitus.
Pathological picture. The most common location of pheochromocytoma is the medulla of one of the adrenal glands. Much less often (in 10-15% of cases) the tumor has an extra-adrenal (extra-adrenal) localization (sympathetic paraganglia along the abdominal aorta and at the site of its bifurcation, less often in the mediastinum and other places). In approximately 10% of cases, pheochromocytomas are bilateral or multiple. Pheochromocytomas are benign (90%) and malignant (10%).
The size of pheochromocytoma ranges from 1 to 12 cm, and its weight is from 5 to 200 g or more. In larger tumors, cysts and hemorrhages are usually found; small tumors are grayish bodies of dense consistency. Pheochromocytoma tissue contains 20 times more adrenaline and 200 times more norepinephrine than the adrenal glands of healthy people.
Clinical picture. According to the clinical course, there are 3 forms of pheochromocytoma: adrenalosympathetic, permanent and asymptomatic.
Adrenal losympathetic (paroxysmal) form - occurs in 25-30% patients and is characterized by attacks of hypertensive crises. The occurrence of crises is facilitated by emotional stress, rich food, and palpation of the tumor, which leads to a sudden increase in the release of catecholamines from the tumor into the blood. The attack often occurs suddenly. Patients develop a feeling of fear, anxiety, trembling, chills, pale skin, and headache. At the same time, blood pressure increases, pain appears behind the sternum, in the heart area, and palpitations. Spastic abdominal pain, nausea, and vomiting are often disturbing. Body temperature, as a rule, is raised to 40°C and even higher.
During a general examination, one may note pallor of the skin, increased sweating, and the patient is agitated. At the height of the crisis, epileptic convulsions are possible. Swelling of the neck veins is observed. The pupils are dilated. Objective symptoms of shortness of breath and acrocyanosis are noted. Heart sounds are rapid, sometimes arrhythmic, less often - bradycardia. Blood pressure is significantly increased, often reaching 250-300 mm Hg. Art.
The duration of the crisis is from several minutes to several hours, rarely longer. In the stage of reverse development of the attack, vascular spasms stop, the patient’s skin turns pink, becomes warm, profuse sweat is noted, and sometimes there is the release of copious amounts of light-colored urine. The crisis can be complicated by retinal hemorrhage and cerebrovascular accident. During an attack, the patient may die from coronary insufficiency, ventricular fibrillation, pulmonary edema or shock.
At the beginning of the disease, hypertensive crises occur relatively rarely, at intervals of months and even years. As the disease progresses, crises become frequent and can occur several times a day.
The permanent form of pheochromocytoma is characterized by a stable increase in blood pressure without crises. With a long course, significant changes occur in the kidneys, myocardial dystrophy, persistent tachycardia, early development of atherosclerosis with damage to the coronary vessels and peripheral arteries. Changes in the fundus of the eye manifest themselves in the form of swelling of the optic nerve nipple, vasoconstriction, exudates, and hemorrhage. Orthostatic hypotension is characteristic. Increased excitability, fatigue, headaches, weakened memory, mood lability, and sometimes depression are noted. 10% of patients develop diabetes mellitus.
B e s ymptomatic form occurs without pronounced clinical manifestations. However, patients are often bothered by weakness, headaches and pain in the lumbar region. Some patients develop shock or acute adrenal insufficiency in a stressful situation.
Laboratory data. During attacks of the disease, an increase in the number of leukocytes, lymphocytosis, and eosinophilia are observed in the blood. There may be erythrocytosis and increased ESR, hyperglycemia, an increase in the concentration of non-esterified fatty acids, increased fibrinolytic activity of the blood and its coagulability. The level of adrenaline, norepinephrine and their metabolites (vanillylmandelic acid, metanephrine, normetanephrine) is determined in the urine. If more than 50 mcg of adrenaline, 100 mcg of norepinephrine and 6 mg of vanillylmandelic acid are excreted in urine per day, we can confidently say that patients have pheochromocytoma.
Great importance in the diagnosis of pheochromocytoma is attached to the adrenolytic test: with the introduction of the adrenolytic 5 mg of regetin intravenously or intramuscularly, blood pressure quickly decreases.
In determining the location of the tumor, an important role belongs to radiological (retropneumoperitoneum or suprarenography) and echographic examination of the adrenal glands.
The electrocardiogram reveals tachycardia, rhythm disturbances (extrasystoles, His bundle block, ventricular fibrillation, Adams-Stokes syndrome) and transient myocardial ischemia.
Flow. Pheochromocytoma has a gradually progressive course. The attacks gradually become more frequent and more severe, leading to disability in patients.
Complications: stroke, myocardial infarction, pulmonary edema, collapse, extensive hemorrhages into the tumor followed by bleeding or peritonitis, gastrointestinal bleeding, malignant degeneration of the tumor. These complications can lead to death of the patient.
Treatment. Recovery of patients can occur only after surgical removal of the tumor.
Conservative treatment with adrenolytics (regitine, tropafen ) mostly gives only a short-term effect and is usually used more often for preoperative preparation of patients. It should be remembered that the use of adrenolytic drugs is sometimes accompanied by orthostatic collapse.
If the pulse rate is 120 beats per minute, often with rhythm disturbances, beta-blockers (obzidan, inderal) are used intravenously or orally with caution.
Date added: 2014-12-12 | Views: 1672 | Copyright infringement
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | 100 | 101 | 102 | 103 | 104 | 105 | 106 | 107 | 108 | 109 | 110 | 111 | 112 | 113 | 114 | 115 | 116 | 117 | 118 | 119 | 120 | 121 | 122 | 123 | 124 | 125 | 126 | 127 | 128 | 129 | 130 | 131 | 132 | 133 | 134 | 135 | 136 | 137 | 138 | 139 | 140 | 141 | 142 | 143 | 144 | 145 | 146 | 147 | 148 | 149 | 150 | 151 | 152 | 153 | 154 | 155 | 156 | 157 | 158 | 159 | 160 | 161 |
Other changes
In addition to the listed signs, there are many other symptoms of hypercortisolism, which are also consequences of this disease.
On the part of the heart, for example, cardiomyopathy often occurs, accompanied by manifestations of failure and arterial hypertension. Many patients begin to suffer from extrasystole and atrial fibrillation.
The nervous system also suffers greatly. This is expressed in depression, lethargy, and steroid psychosis. Some patients experience euphoria, others experience suicide attempts.
Another 10-20% of people suffering from hypercortisolism develop so-called steroid diabetes mellitus, which is in no way associated with pancreatic disease. The disease is relatively easy: it can be quickly compensated for by taking medications that reduce sugar, as well as following an individual diet.
Considering the symptoms of hypercortisolism in men and women, it should also be noted that this disease often causes the development of poly- and nocturia and edema (peripheral).
How can the syndrome occur?
The pathology can be hidden, with a slight increase in hormone synthesis, or pronounced. Doctors distinguish three forms of manifestation of the disease:
- Subclinical hypercorticism, occurs at an early stage or in small forms of tumors, is manifested by increased blood pressure and dysfunction of the gonads.
- Iatrogenic occurs due to exposure to a drug for the treatment of rheumatic diseases, blood. During organ transplantation it is detected in 75% of cases.
- Functional or endogenous hypercortisolism is detected in serious pathologies of the pituitary gland and in diabetes mellitus. Patients with juvenile Itsenko-Cushing syndrome require special monitoring.
Up to 65% of cases are due to iatrogenic hypercortisolism.
Manifestations of the disease depending on gender
The signs of this disease are the same in all patients. However, in addition to all of the above, men and women are faced with purely individual changes in their bodies. This is logical, because hormonal levels have gender specificity.
Women with this pathology often experience infertility, amenorrhea, hypertrichosis, hirsutism and virilization. The menstrual cycle is also disrupted.
And in men, obvious signs of feminization appear. The testicles may atrophy, libido and potency often decrease, and gynecomastia occurs.
Diagnostics
Much has been said above about the symptoms of hypercortisolism in men and women. Treatment will be discussed later, but now a little attention needs to be paid to the issue of diagnosis.
The basis for suspicion of the pathology in question is physical and amnestic data. As part of the diagnosis, the first step is to determine the reason why hypercortisolism occurred. For these purposes, screening tests are carried out. Namely:
- Examination of 24-hour urine for the presence of cortisol excretion. If the level is 3-4 times higher than normal, then hypercortisolism is diagnosed.
- Small dexamethasone test. If a person is healthy, then taking this drug will reduce the level of the hormone by at least half. This does not happen with hypercortisolism.
An increased level of 11-OX in the urine and a low level of 17-KS are also detected. Hypokalemia and increased levels of cholesterol and red blood cells are observed.
In order to determine what exactly became the source of the pathology, a CT or MRI is performed, as well as scintigraphy of the adrenal glands. If the doctor considers it necessary, he prescribes a biochemical blood test. Typically, this study reveals the notorious steroid diabetes mellitus and electrolyte disturbances.
Material and research methods
We performed a retrospective analysis of archival data of medical histories of patients with various forms of hypercorticism aged from 9 to 21 years from three departments (children's department, endocrine surgery department and neuroendocrinology department) of the Russian Scientific and Practical Medical Center of Endocrinology of the Ministry of Health of the Republic of Uzbekistan for the period from 1999 to 2011. In total for this During the period, 39 patients were hospitalized with various forms of hypercortisolism, of which 19 (48.7%) were boys and 20 (51.3%) were girls. The average age of boys was 16.05 years, and girls - 16.15 years.
All patients underwent a range of studies, including the study of endocrine status, general clinical, biochemical, hormonal (ACTH, growth hormone, cortisol, rhythm of cortisol secretion, prolactin, small and large tests with dexamethasone, free cortisol in urine, etc.), radiological (CT/ MRI of the sella turcica and adrenal glands, chest x-ray) and other studies.
Therapy
And this nuance needs to be given a little attention, since we are talking about the causes and symptoms of hypercortisolism. Treatment of the pathology depends on the cause of its occurrence.
If, for example, a medicinal (iatrogenic) form of the disease is diagnosed, then the path to healing lies through the abolition of glucocorticoids, as well as their further replacement with some other immunosuppressants. When a person has a pathology of an endogenous nature, he is prescribed drugs that suppress steroidogenesis.
In some cases, tumor lesions of the adrenal glands, lungs or pituitary gland are detected. Then surgery becomes the solution. Because in such cases, tumors can only be removed through surgery.
However, sometimes intervention is unrealistic for one reason or another. Then the patient is prescribed an adrenalectomy, during which the entire adrenal gland is amputated. An alternative is radiation therapy to the hypothalamic-pituitary region. Although it is often combined with drug or surgical treatment. This approach helps to strengthen and consolidate the effect of therapy.
But that's not all you need to know about eliminating symptoms and treating hypercortisolism. The diagnosis is serious, and therefore cannot be avoided without drug therapy, even if surgery is indicated. The patient is prescribed a number of medications, including:
- Antidepressants.
- Antihypertensive drugs.
- Diuretics.
- Biostimulants.
- Medicines that lower blood sugar.
- Cardiac glycosides.
- Immunomodulators.
- Sedatives.
- Vitamins.
If the patient has developed osteoporosis, then symptomatic treatment will be indicated. Compensation for carbohydrate, mineral and protein metabolism is also required.
But the most responsible and important thing is postoperative treatment. If the patient has undergone adrenalectomy, he will have to constantly adhere to hormone replacement therapy. Without this, his body will not be able to function normally.
What determines the effectiveness of treatment?
Hypercortisolism can develop rapidly, that is, all symptoms appear within 6-12 months, and the clinical picture can develop gradually over 3-10 years. Treatment will depend on correct diagnosis, the severity of the disease and the speed of development of symptoms. Treatment should be aimed at eliminating clinical manifestations and normalizing cortisol levels.
For moderate and mild severity, medications are used that will prevent the body from producing excess amounts of adrenal hormones or radiation therapy is prescribed, which reduces the activity of the pituitary gland. If all this does not give the desired effect, then surgical treatment is used. During this procedure, the pituitary tumor is removed. Or an adrenalectomy is performed, that is, the removal of one of the adrenal glands, but after such an operation constant replacement therapy is necessary.
Forecast
When studying the specifics of such a serious disease, it is necessary to answer a very important question: what are the chances of recovery for this pathology? What's the prognosis? The symptoms of hypercortisolism and its manifestations are severe, this could be seen based on the above. And, unfortunately, if the pathology is ignored, the risk of death is extremely high. Mortality reaches 40-50%.
The prognosis is satisfactory if the cause of the pathology is a benign corticosteroma. But again, healthy adrenal function is restored in only 80% of patients.
If malignant corticosteroma has been diagnosed, the 5-year survival rate will be approximately 20-25%. This is about 14 months on average.
In all cases, the prognosis is determined by how timely treatment was started. Therefore, diagnosis should not be delayed under any circumstances. The more advanced the case, the more serious the complications, the shorter the patient’s life will be. That is why it is strongly recommended to undergo a general examination at least once a year to ensure your good health. And if a problem is discovered, then at least it can be brought under medical control in time.
What types of hypercortisolism exist and what are their features?
Adrenal Cushing's syndrome is divided into the following types:
- functional;
- exogenous;
- endogenous.
Functional type of disease and its features
The functional type of the disease can be present in diabetics.
This type of hypercortisolism develops in people with large body weight, with diagnosed diabetes mellitus, depression and liver dysfunction. Often this disease is registered in children of puberty and adolescence (juvenile dyspituitarism), during pregnancy and in people who drink alcohol in large quantities.
Exogenous type of disease
This form of the disease develops as a result of long-term use of medications containing corticosteroids. This type is caused by drug therapy, so it is also called iatrogenic. And also exogenous hypercorticism often develops after transplantation, with bronchial asthma, systemic diseases and inflammation of the joints.
Endogenous type of disease
Endogenous hypercortisolism develops with concomitant disorders in the body. This can be hyperplasia, malignant and benign neoplasms in the adrenal cortex, as well as tumors in organs such as:
- pituitary;
- ovaries;
- testicles;
- pancreas and thyroid gland;
- lungs;
- thymus;
- bronchi.