Ureterohydronephrosis of the kidney is a condition manifested in the form of an increase in the volume of the renal pelvis and calyx and the ureteric canal.
These changes are accompanied by a decrease in the performance of the organ and atrophy of its functional cells. The physiological consequences of megaureter are poor patency of the ureter in the pelvis.
The reasons for the development of megaureter are multiple, determined both by congenital predispositions and defects, and by the influence of the environment and human lifestyle. What most often influences the occurrence of this pathology?
Hydronephrosis of the kidneys in adults: what is the diagnosis, how to treat and what is the outcome of the disease?
When the kidneys become enlarged due to the accumulation of a large amount of fluid in them, the patient is diagnosed with “kidney hydronephrosis”: what it is, the outcome of the disease, how to treat the pathology - these are the most common questions that face a person with hydronephrosis.
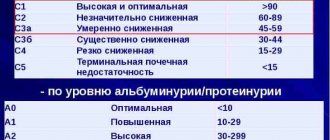
Hydronephrosis of the kidneys (ICD-10 code - N 13) is a pathological disease from the section of urology, in which an increased fluid content forms in one or both kidneys (left and right).
https://www.youtube.com/watch?v=QsDmlPcpB18
Hydronephrosis can be congenital or acquired. In the first case, the pathology manifests itself in the child immediately after birth. The acquired type of disease may have less obvious symptoms and most often occurs against the background of other kidney damage.
Ureteral obstruction occurs as a result of obstruction of the normal flow of urine. The simplest and most common form, which is characterized by discomfort in the kidney area, the functions of which are impaired.
- Double sided.
Usually one of the kidneys is affected - the right or left, but the disease can spread to two organs at once, and the parenchyma most often becomes thinner and inflamed.The cause of such damage is excessive accumulation of fluid, as a result of which irreversible pathological processes develop in the renal pelvis.
The disease occurs in a latent form, the symptoms are not obvious.
- Terminal.
It is characterized by complete atrophy of the parenchyma, resulting in the development of renal failure and, as a result of such irreversible processes, in most cases the disease leads to death.Hydronephrosis is also classified by severity:
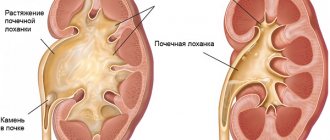
- The 1st degree is characterized by stretching of the renal pelvis, which is subject to excessive pressure from a full bladder. The kidneys, although they increase in size, function normally in the first stage.
At grade 2, the pelvis stretches even more, and the renal calyces also undergo stretching. This leads to compression of the parenchyma, in which atrophic processes develop, and kidney function is impaired.
- Hydronephrosis of the 3rd degree leads to irreversible atrophic processes of the kidney tissue, as a result of which the organ itself begins to die.
- cysts of various origins;
- urinary tract dyskinesia;
- narrowed lumen of the ureter;
- abnormal or abnormal location of the ureter and renal arteries;
- inflammatory processes in the genitourinary system;
- formation of scar tissue in the post-traumatic period;
- reflex disorders leading to difficulty in the outflow of urine as a result of damage to the spinal cord;
- severe pain from the kidney affected by hydronephrosis;
- dull pain in the lower back in any position of the body;
- increased blood pressure;
- constant bloating;
- with urolithiasis - the presence of blood in the urine.
- Ultrasound (to assess the condition of the tissues of the renal apparatus);
- cystoscopy of the bladder;
Preventing the disease from progressing to the terminal stage is possible only with timely diagnosis and adequate treatment.
Any therapeutic and surgical methods at the terminal stage are useless.
In men and women, the causes of this disease may be different. Among male patients, this disease is most often observed with prostate cancer, which blocks the urinary tract, increasing in size due to inflammatory processes.
Also, an increase in this organ can occur due to the formation of a benign prostate tumor.
In women, this disorder is often diagnosed during pregnancy, when pressure on the ureters is exerted by the enlarged uterus. Pathology also develops against the background of ovarian or cervical cancer.
All categories of patients are also characterized by non-pathological causes - this is compression of the ureters during cold-related inflammatory processes affecting organs located in the genitourinary tract.
As the pathology develops, patients may experience the following symptoms:
In some cases, an associated infection may develop during the disease - in such situations, the patient’s body temperature rises significantly.
The examination begins with a physical diagnosis, during which the specialist palpates the kidney area and evaluates the patient's response. After this, general urine and blood tests are prescribed, the results of which can determine the presence of inflammation in the kidney area.
What happens in the body during hydronephrosis
Hydronephrosis is a disorder of the kidney, which manifests itself in an enlargement of the pelvis and calyces due to improper drainage and retention of urine, which is accompanied by an increase in pressure of a hydrostatic nature. Pathological enlargement of the kidney leads to atrophy of the kidney tissue and a gradual deterioration in kidney function.
Typically, when urinary fluid forms in the kidney tissue, urine accumulates in the calyces and pelvis, after which it enters the urinary tract. The fluid then passes through the ureter into the bladder, where it is excreted from the body. Therefore, any violation of this fluid drainage system and its stagnation in the tissues is accompanied by the development of genitourinary diseases, including hydronephrosis.
Home Hydronephrosis congenital urolithiasis
N13 Obstructive uropathy and reflux uropathy
Kidneys
In accordance with the International Classification of Diseases, 10th revision, this disease is designated by several codes:
- 13.0 - hydronephrosis, in which the connections of the pelvis and urinary tract are disrupted;
- 13.1 - hydronephrosis, in which the urinary tract is narrowed;
- 13.2 - hydronephrosis with obstruction of the kidney and ureter by a stone;
- 13.3 - other forms of disease of unspecified origin.
Prevention
You can notice the development of renal hydronephrosis in time and prevent it by following the following preventive recommendations:
- people aged 35 years and older are recommended to visit a urologist and nephrologist 1-2 times a year;
- if you are predisposed to kidney disease, hypothermia must be avoided;
- all infectious lesions of the urinary tract and kidneys should be treated in a timely manner to avoid complications.
a healthy diet and giving up bad habits such as alcohol abuse and smoking can also reduce the risk of developing such pathologies
Types of disease according to the nature of localization
Removal of an organ or resection of its part occurs in two available ways:
- open (laparotomy) nephrectomy;
- closed (laparoscopic) nephrectomy.
Each of these approaches has its own advantages and disadvantages, and the preference in choosing each of them depends on the underlying disease, the severity of the patient’s condition and the extent of the process.
If we are talking about emergency surgical intervention, then patients are unconditionally referred to open surgery, thanks to which the doctor can assess the extent of the problem as much as possible and conduct a complete inspection of the lesion.
Based on the nature of localization, they are distinguished:
- unilateral;
- bilateral ureterohydronephrosis.
Unilateral ureterohydronephrosis is diagnosed most often. The bilateral form of the disease is observed in only 5% of the total number of patients. Also, this form of damage to the renal system is very rarely observed in children.
Depending on the damage to the kidney, ureterohydronephrosis on the right or ureterohydronephrosis on the left may develop. In view of this, abdominal pain can be supplemented by pain in the right or left hypochondrium.
Also in official medicine, the disease is distinguished by the degree of obstruction:
- refluxing - expansion of the ureter along the entire length;
- obstructive – expansion of the ureter only in the upper section;
- combined - simultaneous narrowing of the ureter and cystic reflux.
Classification
Doctors divide the disease according to various criteria. As hydronephrosis appears, it is divided into congenital and acquired; depending on the number of affected organs, unilateral and bilateral hydronephrotic transformation is distinguished.
Based on how the disease progresses, there are three stages of the disease. In the first stage, pyeelectasis increases slightly without disrupting the functioning of the body. In the second stage of the disorder, the kidney grows by an average of 20% by expanding the renal calyces and disrupting the normal flow of urine. At the third stage, the kidney increases in size up to 2 times and can completely atrophy.
Possible complications
Chronic hydronephrosis often contributes to the occurrence of urolithiasis and pyelonephritis, hypertension, which further aggravate the clinical picture of hydronephrotic transformation of the kidney. Sepsis sometimes develops against the background of infected hydronephrosis. The course of hydronephrosis may be complicated by the development of renal failure.
In this case, especially with bilateral hydronephrosis, the patient’s death occurs from intoxication with nitrogen metabolism products and disturbances in water-electrolyte balance. A life-threatening complication of hydronephrosis can be spontaneous rupture of the hydronephrotic sac, resulting in urine leakage into the retroperitoneal space.
What are the typical symptoms?
In the initial stages, hydronephrosis does not manifest itself and is asymptomatic, but some indirect signs may appear that are characteristic of the pathologies that caused hydronephrosis (for example, with urolithiasis, which results in blockage of the ureters, the patient experiences lower back pain).
As the pathology develops, patients may experience the following symptoms:
- severe pain from the kidney affected by hydronephrosis;
- dull pain in the lower back in any position of the body;
- increased blood pressure;
- the pain syndrome may transfer to the right side of the abdominal cavity;
- constant bloating;
- nausea and vomiting;
- with urolithiasis - the presence of blood in the urine.
In some cases, an associated infection may develop during the disease - in such situations, the patient’s body temperature rises significantly.
Surgery
As a rule, medications are not able to cope with ureterohydronephrosis, but only relieve the patient of pain and some complications. Therefore, surgery is necessary to restore kidney function. Infants are also prescribed this method of treatment, since most often the disease is caused by abnormalities in the structure of the organs of the urinary system.
Surgical treatment involves removing obstacles to the outflow of urine. For this purpose, an operation is performed to install a catheter or stent. Vascular resection is performed when there is an abnormal structure of the renal vascular system. If the lumen of the ureter is narrowed, the abnormal section is resected and replaced with the small intestine.
Treatment
Unfortunately, with a disease such as ureterohydronephrosis, treatment most often consists of surgical intervention, because medications are usually not effective enough and often cannot stop the development of pathoprocesses. To minimize the impact, minimally invasive surgery methods are used.
A small percentage of patients can be cured with medication, and in some, especially rare cases, ureterohydronephrosis is stopped due to natural processes occurring in the body - age-related changes, serious and long-term fluctuations in hormonal levels, etc.
In most cases, the specialist recommends surgery. Usually, such manipulations as the introduction of a special expansion catheter, surgical correction of defects, excision of the narrowing site, and ureterostomy are carried out promptly. In the most difficult cases, the functions of the ureter are assigned to the small intestine.
Surgical intervention is a rather complex process, and it is impossible to replace it with any other measures. At the same time, the process of preparation for invasive intervention and the course of the recovery process are of great importance. Both medications prescribed by a doctor and traditional methods can help with this.
If megaurethria is suspected, in addition to a hepatologist, it is imperative to consult a specialist in gastroenterology.
Signs, diagnostic methods and treatment of hydronephrosis
The goal of treatment for megaureter is to reduce the diameter and length of the ureter and restore the passage of urine through it into the bladder; elimination of PMR and complications arising from the disease. Treatment of megaureter involves surgical intervention (the exception is the bladder-dependent form); It is possible to use various minimally invasive techniques and conservative therapy.
Treatment tactics depend on the nature of the course and severity of megaureter, the age and general condition of the child, the presence of pyelonephritis, and the degree of renal dysfunction. In pediatric practice, in most cases of megaureter (about 70%), there is a tendency to reduce manifestations or resolve independently during the first 2 years of the child’s life due to maturation (ripening) and improved function of the ureters and kidneys.
Surgical treatment is performed for severe forms of megaureter that negatively affect kidney function. Surgical intervention for megaureter may include reimplantation of the ureter, formation of ureterocystoanastomosis (including Boari surgery) and antireflux correction. In extremely severe cases of megaureter, the preparatory step is implantation of the ureter into the skin (ureterostomy) for possible restoration of kidney function;
as well as reconstruction of the ureter, including its transverse and longitudinal oblique resection, and then suturing along the side wall to a suitable diameter or intestinal plastic surgery. In case of irreversible destructive changes in the kidney, a significant decrease in its function and the presence of another healthy kidney, nephroureterectomy is performed.
Minimally invasive methods (endoscopic dissection, bougienage, balloon dilatation of the ureter, installation of a ureteral stent for obstructive megaureter) are used in weakened patients; with serious concomitant diseases and other contraindications to surgery.
Treatment of this disease with folk recipes is prohibited and completely useless.
The postoperative period is the only option in which folk remedies can be used in combination with medications. Can be used:
- Decoctions and infusions of birch buds.
- A decoction of chamomile and burdock.
- Oatmeal infusions.
Analyzes
Procalcitonin
Total blood protein
General urine analysis
Blood urea
Blood creatinine
Blood biochemistry (assessment of kidney function)
Diagnostics
Endosonography (endosonography)
| any Endosonography of the pancreas – 28 clinics Endosonography of the stomach – 38 clinics Endosonography of the esophagus – 35 clinics Endosonography of the duodenum – 29 clinics Endosonography of the biliary tract – 21 clinics Intravascular ultrasound (IVUS) – 10 clinics |
Excretory urography for a child
Cystography for a child
Ultrasound of a child's kidneys
Kidney ultrasound
| any adrenal glands – 531 clinics kidneys only – 845 clinics duplex renal arteries – 344 clinics renal vascular constriction – 210 bladder clinics – 54 renal artery constriction clinics – 164 clinics |
Ultrasound of the ureters
Ultrasound of the child's bladder
Static nephroscintigraphy
Dynamic nephroscintigraphy
Eye biometrics
| any Exophthalmometry – 153 clinics Strabismus angle measurement – 193 clinics Computer keratometry – 87 clinics Pachymetry – 66 clinics Computer keratotopography – 40 clinics |
Codes: A02.07.004
Codes without services: A20.30.025 Herbal medicine
A02.07.004 Anthropometric studies
Ureterohydronephrosis is treated both conservatively, in the early stages, and surgically. Moreover, in most cases, the latter method is the only choice that saves a person’s life. Conservative therapy can only in rare cases relieve this pathology.
Measures prescribed for conservative treatment:
- Antispasmodic therapy. Drugs that reduce the tone of the urinary system are used (No-shpa, Papaverine, Baralgetas, Riabal, Spazmolgon, Magnesia 25%, Eufillin). Often this therapy saves urolithiasis and helps the latter leave the ureter and exit the body with urine. Thanks to this, relief comes in a matter of minutes. These drugs are also used for other reasons that cause ureterohydronephrosis.
- Treatment of pain syndrome. For these purposes, narcotic and non-narcotic analgesics are used (Omnopon, Butorphanol, Promedol, Tramadol, Ketanov, Ibuprofen, Dexalgin, Fanigan).
- Improving the functioning of the microvasculature located in the kidneys. Such patients are prescribed the drugs Trental and Petoxifylline both in the early and late stages.
- Treatment and prevention of infectious complications. Both antibiotics with a wide spectrum of effects on microorganisms and specific uroseptics are used. In the first case, 2nd and 3rd generation cephalosporins (Cefuroxime, Ceftriaxone, Cefazolin), fluoroquinolone series (Levofloxacin, Norfloxacin, Ciprofloxacin), macrolides (Sumamed, Erythromycin, Clarithromycin) are used. In the second, the well-known Nitroxoline and Palin.
- Treatment of inflammation in the kidney parenchyma. It is performed using Urolesan in tablets or drops, as well as Canephron in capsules. These drugs have a pronounced anti-inflammatory effect, are antispasmodics and antiseptics.
Surgical treatment
Surgical intervention in many cases is the only choice for providing care to patients with ureterohydronephrosis. At the moment, two types of operations are used in urology: palliative (alleviating the patient’s condition) and radical, that is, completely eliminating the problem. Palliative interventions are performed for inoperable tumors that grow into neighboring organs or when it is impossible to remove the entire kidney. Radical operations permanently relieve the patient of suffering and the problem that caused ureterohydronephrosis.
Hydronephrosis of the kidneys is treated with medication and surgery. The first method is relevant in the early stages of the disease and if the lesions are still reversible.
Treatment is performed only in a hospital setting and involves the use of the following groups of medications:
- hormonal agents (when diagnosing fibrosis in the retroperitoneal region);
- antibiotic drugs (to prevent and eliminate bacterial infections);
- painkillers and anti-inflammatory drugs;
- drugs that lower blood pressure;
- the use of drugs containing alkali (to dissolve stones in urolithiasis).
In the later stages, such conservative therapy is ineffective, and the patient undergoes surgery to install a nephrostomy.
A nephrostomy is an artificial urinary canal, which is a catheter and is installed during a surgical operation.
The nephrostomy is installed directly into the renal pelvis and, passing through the tissues of these organs, comes out, draining urinary fluid into a urinal. The procedure for installing a nephrostomy tube (nephrostomy) can be performed in one of three ways:
- open surgery;
- laparoscopy;
- puncture.
The type of operation is determined based on
tissues and general condition of the patient.
In general, any of these operations involves making punctures or incisions in the kidney area and inserting a catheter, which is subsequently connected to an external urine bag.
Treatment prognosis can be favorable only if treatment is started in the early stages of hydronephrosis.
In the case of bilateral damage, the prospects are not so good: most likely, the person will have to undergo hemodialysis for life, and sometimes a transplant of the affected organs may be necessary.
Urinary tract infection in children
Get advice on medical tourism×
Treatment abroad
Application for medical tourism
What is the best way to contact you?
Enter your phone number or email addressSubmit an application for medical tourismMedical tourism
Diagnosis of the disease
Proper study of the disease allows you to quickly and effectively identify and cure the disease. Hydronephrosis is diagnosed using several procedures.
- Examination by a doctor . The first and simplest diagnostic method. During the examination, the doctor conducts a dialogue with the patient, studies the medical history, and probes the site of the suspected disease. The examination is important for further prescribing procedures and diagnostics.
- Laboratory research . This stage may include a urine test, a complete blood count, and blood taken to study electrolytes and creatinine.
- Research carried out using special equipment . Computed tomography and ultrasound are used to diagnose hydronephrosis. Tomography allows you to illuminate the patient’s abdominal cavity and see the whole picture at once. Using ultrasound, the suspected affected organs are listened to and their structure and functioning are studied. Ultrasound is preferable for pregnant women and newborns and is completely harmless.
Reasons for the development of kidney hydronephrosis
The International 10th Revision of All Diseases is a generally accepted structure that codes specific diseases and their types. This is a medical classification confirmed by the World Health Organization. Specialists who assigned codes to various diseases identified the main causes of hydronephrosis:
- incorrect location of the ureter;
- renal artery pathology;
- obstruction of the lower urinary tract;
- stones in the kidneys;
- inflammatory processes in the genitourinary system;
- gynecological or urological tumors;
- dysfunction of the spinal cord, etc.
According to ICD-10, hydronephrosis can be congenital or acquired. In both cases, if not treated in a timely manner, the disease can lead to disability and even death. Urine accumulates in the pelvis and calyces, which is not excreted and poisons the body. As a result, the kidneys begin to deteriorate.
In the international 10th revision of diseases, such renal pathology is listed as obstructive uropathy and reflux uropathy. Code N13 does not include congenital renal obstructions, kidney or ureteral stones, or pyelonephritis. These are separate pathologies that have nothing to do with hydronephrosis.
We recommend
What is hematuria: classification according to ICD-10
Regardless of the reason for which ureterohydronephrosis began to develop, the ureter goes through the same stages of changes.
Initially, under the pressure of urine, which does not leave completely, the tone of the ureter decreases. This causes the pelvic part of the tube to expand.
Then the kidneys are involved in the process, their excretory function is disrupted. This is the 2nd stage of the process: during it, the tone of the renal pelvis and calyces decreases, which leads to disruption of the secretory-excretory function of the kidneys.
The last stage is the death of kidney cells with the formation of acute renal failure. If the disease is detected at stages 1–3, the prognosis is favorable, but the result of therapy largely depends on concomitant pathologies, the condition of the body, and compliance with therapeutic measures.
Ureterohydronephrosis can develop for various reasons. A congenital disease appears, as a rule, as a result of pathological processes in the prenatal period and in the first year of life.
Uretherohydronephrosis in children (congenital) occurs due to:
- narrowing of the urinary tract;
- retrocaval location of the ureter or underdevelopment of its lumen in the fetus;
- defect of the valve (a flap of mucous membrane covering the lumen of the ureter).
The causes of acquired ureterohydronephrosis in adults are:
- development of inflammatory diseases of the genitourinary system;
- injury to a paired organ of the urinary system (ureter);
- kidney displacement;
- obstruction by a blood clot resulting from blood or kidney diseases;
- the presence of neoplasms (both benign and malignant), localization - uterus, ovaries, rectum, etc.;
- injury to the spinal cord or spine (the nervous regulation of the urinary system is disrupted).
Also contribute to the development of this pathological process: excessive consumption of alcoholic beverages, uncontrolled use of certain medications (analgesics), radiation exposure.
The manifestation of ureterohydronephrosis in women during pregnancy is also a common occurrence. It develops as a result of displacement of organs (compression of the ureter) due to the growth of the uterus. In such cases, the right kidney most often suffers, and pain occurs on the right side.
Provoking factors can also be other, no less dangerous pathological conditions, including diabetes mellitus, anemia, polycystic ovary syndrome, and urolithiasis. Therefore, it is very important to know how this disease manifests itself and why it is necessary to seek medical help in a timely manner.
According to the common classification of this disease, it can be congenital and acquired. The congenital form occurs when:
- anomalies in the development of the renal vessels and their branches, when the arteries compress the underlying ureter and block its lumen;
- urinary tract dyskinesia;
- congenital obstructive defects of the ureter and urethra (strictures, the appearance of valves, etc.);
- abnormal location of the urinary tract (most often you can find the ureter located behind the inferior vena cava).
Hydronephrotic transformation of the kidney in adults occurs as a result of the progression of any urological diseases, but the root cause remains the same - disruption of the normal passage of urine. Most often, kidney hydronephrosis is caused by urolithiasis (KD), various infectious and inflammatory diseases of the urinary organs, oncological pathology (tumors of the kidneys and abdominal organs), traumatic damage to the ureter with narrowing and cicatricial deformation of its lumen, disruption of the innervation of the pelvic organs, as a result of which persistent spasm of smooth muscles occurs.
Hydronephrosis of the kidney does not develop quickly enough, so it is within the patient’s power to immediately begin treating all of the above-described pathologies, avoiding such a dangerous complication. This dangerous disease is in class XIV of the International Classification of Diseases (ICD-10). As a rule, it leads to the rapid development of renal failure with subsequent disability of the patient.
Mechanical compression of the renal vessels also occurs, which leads to ischemia of the organ, the occurrence of focal necrosis and sclerosis of the stroma. ICD-10 even identifies separate nosologies and consequences of renal hydronephrosis, which indicates the severity and seriousness of this pathology.
Depending on the level at which the obstruction to the outflow of urine occurred, hydronephrotic transformation of the kidneys may occur due to obstructions at the level of the bladder or urethra; obstructions at the level of the ureter that are not in its lumen (often these are tumors of the pelvic organs); obstructions that arise in the lumen of the ureter (stones, cicatricial narrowings and strictures); obstructions at the point where the ureter enters the kidney.
Even ICD-10 provides several separate codes characterizing these levels (Nos. 13.0, 13.1 and 13.2). Code No. 13, which refers to obstructive uropathy, includes subsections for renal obstruction, ureteral stricture, and ureteropelvic junction obstruction.
Diet
The consequence of certain dietary recommendations is also very important. Proper nutrition significantly enhances the effect of medications and alleviates the manifestation of the disease.
The basic rule of nutrition for this disease is to avoid any foods that burden the kidneys and urinary system.
You should completely stop eating pickles and generally significantly limit your intake of salt and acidic foods. It is also not recommended to eat spicy food - it can provoke inflammation.
Prohibited are fatty meats and broths, legumes, confectionery, carbonated drinks and any seasonings in the form of sauces and ketchups, especially factory-made ones. The patient's diet should be based on eating light foods, and the amount of protein should not be too high - this creates a load on the kidney.
The basis of the diet should be porridge, all kinds of vegetable dishes, dairy products, poultry and beef liver, as well as boiled potatoes.
It is allowed and even necessary to consume a lot of fruits and natural juices and fruit drinks, especially from fresh grapes, cherries, blueberries, cranberries, raspberries, cherries, citrus fruits and watermelons. It is allowed, in the absence of contraindications such as diabetes, the use of all kinds of dried fruits.
Meat consumption should be seriously limited. It is best to choose dishes from lean fish and lean white meat, observing their consumption in moderation. Alcohol and any flavoring additives, canned food, and dyes are absolutely excluded.
Eating foods that contain significant amounts of protein is undesirable. However, with certain indicators of the body, products can be introduced into the diet on the recommendation of a specialist.
Symptoms
Such a disease from the urinary system can be completely asymptomatic, up to the development of pyelonephritis (inflammatory damage to the kidney), the clinical signs of which are:
- a sharp increase in temperature indicators;
- change in the shade and transparency of urine - it becomes darker and cloudier;
- pain localized in the lumbar region.
Against the background of such symptoms, the main clinical picture of the disease develops, which is presented:
- spread of pain to the left or right side;
- false urges to visit the toilet to empty the bladder;
- urinary incontinence;
- unpleasant odor coming from urine;
- the presence of pathological impurities in urine;
- increased urge to urinate;
- fever;
- attacks of renal colic;
- complete disruption of the outflow of urine - most often this symptom is observed in females or in children.
Etiology
A cystic tumor of the distal bladder most often acts as a congenital anomaly that develops against the background of:
- narrowing of the mouth of the ureter, which occurred even at the stage of intrauterine development of the fetus;
- lengthening of the intramural section of this organ;
- lack of muscle fibers in the distal segment of the ureter;
- disruption of the innervation process in the bladder and nearby tissues.
In the vast majority of situations, such changes develop in children whose mother suffered serious illnesses during the intrauterine development of the fetus. Such pathologies include:
In addition, often abnormalities in the ureter develop against the background of the expectant mother’s addiction to bad habits, drug overdose, radiation and poor nutrition.
Acquired ureterocele in women and men in all situations is a consequence of strangulation of a bladder calculus in the intramural segment of the ureter, i.e. at its mouth.
The pathogenesis of this disease has several characteristics and consists of:
- disruption of the process of urine outflow from the ureter;
- increase in hydrostatic tone;
- overstretching of the wall of the ureter, its bulging into the cavity of the bladder;
- stagnation of urine in the renal pelvis, which is also called hydronephrosis.
The above changes and complete lack of treatment for ureterocele can lead to the development of irreparable complications.