Chronic kidney disease ICD code 10. Chronic kidney disease ICD
CKD stage 4, kidney damage with a pronounced decrease in GFR (15-29 ml/min)
CKD stage 5, chronic uremia, end-stage kidney disease (including cases of RRT (dialysis and transplantation)
* - appropriate disease codes should be used to indicate the etiology of CKD
** - code N18.9 indicates cases of CKD with an unspecified stage
The need to identify CKD at an early stage in children
Children have their own list of diseases that lead to the development of CKD:
1. Family history of polycystic kidney disease or other genetic kidney diseases. 2. Low birth weight. 3. Acute renal failure as a result of perinatal hypoxemia or other acute kidney injury. 4. Renal dysplasia or hypoplasia. 5. Urological abnormalities, especially obstructive uropathy. 6. Vesicoureteral reflux associated with recurrent urinary tract infections and kidney scarring. 7. History of acute nephritis or nephrotic syndrome. 8. History of hemolytic-uremic syndrome. 9. History of Schonlein-Henoch disease. 10. Diabetes mellitus. 11. Systemic lupus erythematosus. 12. History of hypertension, in particular as a result of thrombosis of the renal artery or renal vein in the perinatal period.
Children with retarded physical development (growth retardation, low body weight), rickets-like skeletal deformities, metabolic acidosis, early-onset anemia, polyuria, polydipsia, proteinuria, hypertension, impaired renal concentration function represent a risk group for the development of CKD, which requires a thorough examination of these patients, prescribing corrective and replacement therapy to prevent or slow down the progression of CKD.
Congenital, hereditary and acquired kidney diseases in children potentially carry the risk of developing unfavorable outcomes - the formation of chronic kidney disease (CKD) and chronic kidney disease.
The need to identify CKD in children at an early stage is a socially significant task - the sooner we begin to prevent the identification of risk factors for the development of CKD in children, the more people will remain healthy and able to work, while the risk of developing concomitant diseases in them will be significantly reduced.
Nephrosclerosis
Nephrosclerosis
is a pathological condition caused by the death of nephrons, their replacement by connective tissue with an increase in renal failure. It manifests itself as polyuria, nocturia, hypertension, swelling, discomfort in the lower back, and in the later stages - oliguria, hematuria, intoxication.
Diagnosed using laboratory tests, ultrasound, CT, MSCT of the kidneys, nephroscintigraphy, angiography of the renal vessels, urography, biopsy.
For treatment, etiopathogenetic therapy of the underlying disease, anticoagulants, antiplatelet agents, antianemic, detoxification, vitamin and mineral agents, replacement therapy, and kidney allotransplantation are used.
Nephrosclerosis is a secondary clinical and anatomical condition, manifested by compaction, wrinkling of the kidneys and a decrease in their functional capacity due to the replacement of parenchyma with fibers and interstitial substance of connective tissue. The shriveled kidney was first described in 1914 by the German clinician F. Volhard and pathologist K.T. Farom.
Typically, nephrosclerosis complicates the course of urological and other somatic pathologies.
In the twentieth century, its leading cause was considered to be glomerulonephritis, at present it is arterial hypertension and diabetes mellitus (more than 60% of all diagnosed cases).
The prevalence of nephrosclerosis in European countries is 0.06%. At the same time, 10-20% of patients require regular hemodialysis, and mortality from chronic renal failure reaches 22%.
Nephrosclerosis
Kidney shrinkage is a polyetiological process that complicates various vascular disorders and urological diseases.
Depending on the type of nephrosclerosis, experts in the field of urology and nephrology identify two groups of causes that cause primary or secondary replacement of the renal parenchyma with fibrous structural elements of connective tissue.
A primarily wrinkled kidney is formed against the background of damage to the renal vessels caused by diseases such as:
- Arterial hypertension
. In patients with essential hypertension and symptomatic hypertensive conditions, the renal vessels persistently spasm and narrow, and the nutrition of the parenchyma is disrupted. Connective tissue compaction of the vascular wall or death of arterioles and glomerular capillaries ends, respectively, with the formation of slowly progressive arteriosclerotic nephrosclerosis or malignant arteriolenecrotic glomerulosclerosis of Farah. - Atherosclerosis of the renal arteries
. The deposition of atherosclerotic plaques on the inner lining makes the vascular wall less elastic and narrows the lumen of the vessels feeding the renal parenchyma. A decrease in tissue perfusion provokes the destruction of nephrons and tissue hypoxia, which promotes excessive formation of connective tissue. As a result, as a result of atherosclerosis, the cortical substance becomes thinner, the cells of the urinary tubules atrophy, which reduces the functional capacity of the kidney. - Chronic venous congestion
. Against the background of stagnation caused by nephroptosis, narrowing or chronic thrombosis of the renal veins, parenchymal vessels dilate paretically, the flow of oxygenated arterial blood decreases, and ischemia increases in the tissues. The situation is aggravated by compaction of the vascular walls, which further disrupts tissue metabolism. Under hypoxic conditions, partial cell death occurs, and nephrosclerosis occurs within 10-15 years.
In some patients, angiogenic renal destruction occurs acutely with partial or complete thromboembolism of the renal artery. A sharp disruption of blood circulation causes a kidney infarction—massive death of nephrons as a result of acute ischemia. Subsequently, the necrotic area is gradually replaced by connective tissue, and nephrosclerosis develops.
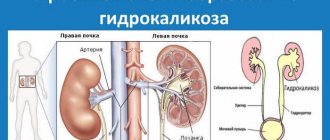
A secondarily wrinkled kidney is spoken of in cases where the patient initially suffers from a urological disease, in which the renal parenchyma is destroyed under the influence of infectious agents, autoimmune complexes, mechanical factors (stretching, trauma by stones), etc. The main causes of secondary (nephrogenic) nephrosclerosis are:
- Kidney diseases
. Hardening of the parenchyma can result in pyelonephritis, kidney tuberculosis, glomerulonephritis, urolithiasis, and polycystic disease. A separate group of causes of nephrosclerosis consists of secondary nephropathies, which complicate the course of other pathological processes - diabetes mellitus, systemic lupus erythematosus, malignant neoplasia, preeclampsia. - Diseases of the lower urinary tract
. Nephrosclerosis can develop against the background of hydronephrosis, caused by obstructive stagnation of urine during sclerosis of the bladder neck, the formation of uretero-vaginal fistulas, and compression by pelvic tumors. Atrophic processes are observed in 30-60% of patients suffering from vesicoureteral reflux.
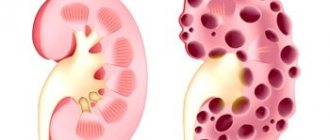
Despite the variety of causes that cause nephrosclerosis, the mechanism of development of the disease as a whole is common.
Initially, under the influence of various damaging factors (hypoxia, inflammatory and dystrophic processes caused by pathogenic factors of microorganisms, autoimmune complexes, direct traumatic effects, etc.
) destruction of the glomerular and tubular epithelium occurs with the exclusion of some nephrons from the general blood supply.
Since kidney cells are not capable of regeneration, after phagocytosis of destroyed cellular elements, nephrosclerosis begins - the damaged area is replaced by connective fibers, and the kidneys themselves become denser.
In the remaining glomeruli, blood circulation and filtration increase, resulting in an increase in the volume of urine excreted and a decrease in its relative density.
Against the background of blood flow disturbances, the synthesis of renin, which regulates glomerular filtration, increases, which contributes to the occurrence or worsening of arterial hypertension.
Due to the high compensatory capabilities of the renal tissue, clinical signs of renal failure appear only with severe nephrosclerosis with the loss of 70% of the nephrons of both kidneys or 85% of one. When 5% of cells or less are retained, functional failure of the organ occurs, requiring replacement therapy.
CT urography. Pronounced asymmetry in the size of the kidneys, a significant decrease in the size of the right kidney.
The clinical picture of the disease at an early stage is characterized by an increase in the amount of daily urine (more than 2 liters), increased frequency of urination at night (more than 3 times per night), constant nagging pain in the lumbar region, and an increase in blood pressure. As nephrosclerosis progresses, swelling appears: first on the face, then it spreads evenly throughout the body. Swelling is most pronounced in the morning.
At a later stage, the symptoms worsen: the volume of daily urine decreases to 0.5–0.8 l, an admixture of blood may appear in the urine, the patient is bothered by dry mouth and constant thirst. General symptoms of intoxication arise and increase: headache, nausea and vomiting, weakness, muscle pain.
Serious disturbances in the processes of filtration and reabsorption, which occur with the destruction of more than 70-75% of the initial number of nephrons, lead to the formation of chronic renal failure.
Because the shriveled kidney stops producing erythropoietin, which is necessary for the maturation of red blood cells in the bone marrow, iron deficiency anemia often develops. Patients with nephrosclerosis have an increased risk of nephrogenic arterial hypertension due to excess renin production.
When vitamin D metabolism is disrupted, osteoporosis occurs with increased bone fragility and a tendency to form pathological fractures.
Patients with suspected nephrosclerosis are prescribed a comprehensive examination to determine the features of the morphological structure of the kidneys, identify signs of parenchymal atrophy, and assess the functional viability of the organ. The most informative laboratory and instrumental methods for diagnosing a wrinkled kidney are:
- General urine analysis
. For nephrosclerosis, a significant decrease in the relative density of urine (up to 1.005-1.015 g/l) is indicative. With increasing signs of chronic renal failure, erythrocyturia (up to 2-3 red blood cells in the field of view), cylindruria, proteinuria (up to 0.033 g/l) are possible. - General blood analysis
. In patients with a shriveled kidney, the content of hemoglobin and red blood cells decreases, moderate thrombocytopenia, and an increase in the duration of bleeding and blood clotting time are noted. Slight leukocytosis often occurs. - Biochemistry of blood
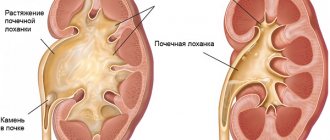
. Assessment of functional capacity using biochemical parameters reveals renal failure. With nephrosclerosis, the content of uric acid, creatinine, urea, magnesium, phosphorus, and sodium may be increased. The level of protein and potassium decreases. - Sonography
. Characteristic echographic signs of nephrosclerosis are a decrease in the size of the affected organ, thinning of the parenchyma, atrophy of the cortex, and its unclear differentiation with the medulla. Often, kidney ultrasound reveals nephrocalcinosis. - X-ray methods
. With survey and excretory urography, the size of the kidneys and the cortical layer are reduced, and calcifications are detected in the parenchyma. Impaired filling of the pyelocaliceal system with a contrast agent may indicate the development of chronic renal failure. - Angiography
. On renal angiograms, the arteries are usually narrowed and deformed. In some patients, the fine arterial pattern may be absent (the “burnt wood” symptom). The cortex is thinned. Irregularity of the outer contour of the kidneys is typical. - Dynamic nephroscintigraphy
. When the kidney shrinks, it accumulates and excretes nephrotropic radionuclide more slowly. The study is complemented by static nephroscintigraphy, which reveals parenchymal defects by the uneven distribution of the radiopharmaceutical. - Tomography of the kidneys
. Three-dimensional models and layer-by-layer images obtained during CT and MSCT reveal thinning of the cortical layer and a decrease in the size of the organ. Signs of nephrosclerosis are narrowing and deformation of small arterial vessels. - Needle biopsy of the kidneys.
Histological analysis of a kidney biopsy reveals a significant decrease in the number of nephrons and a large number of connective tissue fibers. During the study, the condition of arterioles and capillaries is assessed.
Differential diagnosis of nephrosclerosis is carried out with diabetes mellitus and diabetes insipidus, acute renal failure, rapidly progressive glomerulonephritis, hepatorenal syndrome, hypochloremic azotemia. If necessary, the patient, in addition to a nephrologist and urologist, is consulted by a therapist, cardiologist, phthisiatrician, rheumatologist, endocrinologist, oncologist, and oncohematologist.
CT urography. Nephrosclerosis on the right.
Conservative therapy for the initial stages of kidney shrinkage is aimed at correcting the underlying disease that provoked the sclerotic process and increasing renal failure.
Taking into account the pathology that caused nephrosclerosis, the patient is prescribed antibiotics, antihypertensive drugs, statins, glucocorticosteroids, antiglycemic, diuretic, non-steroidal anti-inflammatory and other etiopathogenetic drugs.
To relieve disorders caused by functional renal failure, the following can be used:
- Anticoagulants and antiplatelet agents
. By influencing the rheological properties of blood, they improve blood flow in the renal arterioles and capillaries and, by restoring tissue perfusion, they slow down nephrosclerosis. Prescribed with caution when chronic renal failure increases. - Vitamin and mineral complexes
. To correct changes in the biochemical composition of the blood caused by impaired filtration, potassium, calcium, vitamin D, multivitamin formulations, and bisphosphonates are used. Taking them improves metabolism and prevents osteoporosis. - Antianemic drugs
. If anemia is detected, erythropoietin preparations are prescribed, which stimulate the formation of red blood cells, and iron, necessary for the synthesis of hemoglobin. Reducing hemic hypoxia makes it possible to slow down sclerotic processes in the kidney tissues. - Detoxification therapy
. To speed up the elimination of toxic metabolites that accumulate in the body during nephrosclerosis, enterosorbents are used, which bind metabolic products in the intestines. Herbal remedies based on artichoke can be prescribed to reduce urea levels.
If kidney shrinkage is combined with stage III-IV chronic renal failure, renal replacement therapy is indicated - peritoneal dialysis, hemodialysis, hemodiafiltration, hemofiltration. A radical treatment method recommended for nephrosclerosis with a decrease in the number of viable nephrons to 5% or less is kidney transplantation after abdominal or laparoscopic nephrectomy.
With timely detection of the disease, the prognosis is relatively favorable; the appointment of adequate therapy allows one to achieve a long-term state of compensation for nephrosclerosis. Over time, the functioning of the nephrons deteriorates, and chronic renal failure develops: such patients require an organ transplant or regular hemodialysis.
To prevent nephrosclerosis, it is necessary to follow the recommendations of a specialist in the treatment of nephrological diseases (especially of an inflammatory nature), monitor the level of blood pressure, blood glucose, avoid hypothermia, and do not abuse salt and meat foods. An important role in preventing the development of a wrinkled kidney is played by regular visits to a family doctor for early detection and correction of somatic pathology.
Source: https://www.KrasotaiMedicina.ru/diseases/zabolevanija_urology/nephrosclerosis
Pyelonephritis according to ICD 10 - classification of the disease
Pyelonephritis is an inflammatory disease of the kidneys. The pelvis and tissue (mainly interstitial) are directly affected. People of all ages are affected, but in women, due to structural features, the pathology occurs more often than in men.
According to the International Classification of Diseases, Tenth Revision (ICD-10), the condition is classified in class XIV “Diseases of the genitourinary system”. The class is divided into 11 blocks. The designation of each block begins with the letter N. Each disease has a three-digit or four-digit designation. Inflammatory kidney diseases belong to the headings (N10-N16) and (N20-N23).
Urinary tract infection - treatment and symptoms
Urinary tract infection often accompanies young people. But in modern society, all generations can suffer from this disease: from infants to the elderly.
What to do if such a disease appears? In our article we will describe detailed instructions for recognizing the disease. We will also tell you how the pathology is treated.
Point one: what types of infections are there?
Urine is formed in the kidneys by filtration, then it passes through the ureters and enters the bladder. From there, the fluid is pushed into the urethra and comes out.
Significant differences are observed in the urinary system of men and women. The urethra in women is straight and short, which causes a high prevalence of infections in the urine among the female population.
What can be surprising about this well-functioning system?
When an infectious agent enters any part of the tract, inflammation occurs. The International Classification of Diseases (ICD 10) lists the following nosologies:
- urethritis (the microbe multiplies in the initial part of the tract);
- cystitis (bladder infection);
- pyelonephritis (inflammation of the renal pelvis);
- kidney abscess (the kidney tissue itself is affected).
Urinary tract infections of unknown etiology are also isolated in urinary tract when the source of inflammation is not identified.
Point two: what causes the disease?
A urinary tract infection (UTI) can be caused by any agent, be it bacteria, virus or fungus. But we will focus on the most common pathogens. These are Escherichia coli, Proteus, Staphylococcus (fecal, aureus, saprophytic). Less common are Klebsiella, Candida (fungi) and Pseudomonas.
It is worth noting that modern flora is very resistant to antibacterial drugs. Therefore, treatment of the urinary tract requires a competent choice of antibacterial drug.
In infants, an infection in the urine is caused by the same flora. In the first months of life, boys get sick more often than girls.
Point three: what does the disease look like?
What symptoms can be found in a person with an infection in the urine?
- Painful sensations. The pain syndrome depends on the localization of the process. With pyelonephritis, the kidneys hurt (the lower back ache under the ribs, the symptoms of “effleurage” are positive). A bladder infection is accompanied by pain in the suprapubic region. When the urethra becomes inflamed, pain radiates to the external genitalia.
Symptoms of “effleurage” or Pasternatsky are characterized by pain when the patient taps in the area of the affected kidney and the short-term appearance of blood in the urine. These symptoms are accompanying kidney stones. With pyelonephritis, only pain appears.
- There is a frequent urge to urinate. Symptoms appear not only during the day, but also at night. In this case, urine is either not excreted at all or is excreted in small quantities.
- The clarity and color of urine changes. These symptoms are associated with the appearance of cells (leukocytes), mucus (desquamated epithelium), and bacterial particles in the secretions. As a result, the urine becomes cloudy, dark yellow, and flakes settle at the bottom. When bacteria actively multiply, an unpleasant, foul odor appears. Normal urine is straw-yellow and transparent.
- Dysuria. This intense burning or pain during urination. Symptoms of dysuria are characteristic of damage to the urethra, less often of inflammation of the bladder.
In addition to urethritis, ICD distinguishes urethral syndrome. During this pathology, a woman experiences painful urination and a false urge to go to the toilet. In this case, bacteria are not detected in the urine.
- The appearance of blood in the urine.
- Fever, chills, intoxication.
Point four: how to identify the disease?
Infection in urine is not easy to identify. First, a general analysis is carried out. Its result allows us to do a more specific study:
- determine the number of leukocytes in the urine;
- determine the number of bacterial particles;
- conduct cultures for sensitivity to antibiotics.
When there is an infection in the urine, the sensitivity of the bacteria is very important. The number of resistant forms increases year by year. This knowledge helps optimize treatment.
Additional methods include:
- scraping from the urethra to identify sexually transmitted infections;
- general blood analysis;
- Ultrasound of the kidneys.
The diagnosis is made based on a combination of three factors:
- a clear clinical picture (dysuria, false urges, pain above the pubis, fever, lower back pain);
- the presence of leukocytes in the urine (more than 104 in 1 ml of urine);
- bacteriuria (infection in the urine) – more than 104 units per 1 ml.
Point five: how to recover?
First of all, treatment should begin with getting rid of the infectious agent in the urine. This requires antibiotics. They are prescribed for a period of 10 to 14 days with mandatory monitoring of urine sterility after the course of therapy. If symptoms disappear, but the pathogen is isolated, the drug is changed and treatment is resumed.
The drug is selected only by the doctor, taking into account the sensitivity of the pathogen, experience of previous therapy and the individual characteristics of the patient. First-line antibiotics for cystitis and urethritis - Amoxiclav, Fosfomycin, Cefuroxime, Nitrofurantoin, Co-trimaxazole, Fluoroquinolones (Norfloxacin, Ofloxacin). They are prescribed in tablet form. A bladder infection does not disappear quickly; visible results will be obtained only after 12-14 days. For pyelonephritis and other infectious diseases of the kidneys, these drugs are prescribed intravenously.
Pyelonephritis is a reason for hospitalization of the patient.
Treating an infection in the urine is sometimes a very difficult task. To do this, it is recommended to use additional agents that suppress inflammation and ensure sterility of the discharge. Herbal preparations and medicinal mixtures are the best choice, which will complement the treatment and ensure a quick recovery.
Canephron. Contains rosehip, lovage and rosemary herbs. Canephron drops and tablets are good at relieving spasms that accompany a bladder infection. Treatment with this drug accompanies the use of antibiotics. It enhances the effect on bacteria and helps relieve inflammation. In addition, plant components have diuretic properties. Frequent emptying of the bladder promotes rapid evacuation of bacteria and speeds up treatment.
Leros urological collection contains birch leaves, parsley root, nettle, elderberry and other herbs. It is taken daily. Relieves inflammation, relieves pain and has an additional diuretic effect. Treatment lasts 2 weeks. In some cases, the course can last 1 month.
infekc.ru
Why is the disease dangerous?
The first symptoms are not immediately associated with kidney disease:
- Increased blood pressure.
- Itching appears.
- Swelling of the limbs.
- Feeling of fatigue inappropriate to the load.
Treatment of symptoms without consultation with specialists, at home, leads to a worsening of the condition.
The disease can be triggered by any factors surrounding a modern person: stress, hypothermia, overwork, weakened immunity, unhealthy lifestyle.
The disease is dangerous because it can become chronic . During exacerbation, the pathological process spreads to healthy areas. As a result of this, the parenchyma dies and the organ gradually shrinks. Its functioning is reduced.
The disease can lead to the formation of kidney failure and the need to connect an “artificial kidney” device. A kidney transplant may be required in the future.
The consequences are especially dangerous - the addition of a purulent infection, necrotization of the organ.
ICD-10 indicates:
Chronic pyelonephritis. Code N11
Usually develops due to non-compliance with the therapeutic regimen of an acute condition. As a rule, the patient knows about his illness, but sometimes it can be latent. Symptoms expressed during an exacerbation gradually subside. And it seems that the disease has receded.
In most cases, pathology is detected during clinical examination, during urine analysis in connection with other complaints (for example, high blood pressure) or diseases (for example, urolithiasis).
When collecting anamnesis in these patients, symptoms of previous cystitis and other inflammatory diseases of the urinary tract are sometimes revealed. During exacerbations, patients complain of pain in the lumbar region, low temperature, sweating, exhaustion, loss of strength, decreased appetite, dyspepsia, dry skin, increased blood pressure, pain when urinating, and decreased amount of urine.
Non-obstructive chronic pyelonephritis associated with reflux. Code N11.0 .
Reflux is the backflow (in this context) of urine from the bladder into the ureters and above. Main reasons:
- Bladder fullness.
- Bladder stones.
- Hypertonicity of the bladder.
- Prostatitis.
Chronic obstructive pyelonephritis. Code N11.1
Inflammation develops against the background of obstruction of the urinary tract due to congenital or acquired anomalies in the development of the urinary system. According to statistics, the obstructive form is diagnosed in 80% of cases.
Non-obstructive chronic pyelonephritis NOS N11.8
With this pathology, the ureters are not blocked by stones or microorganisms. Patency of the urinary tract is preserved, urination is not impaired either qualitatively or quantitatively.
Classification and diagnosis
A urinary tract infection is an infection that occurs anywhere in the urinary system, from the perinephric fascia to the external opening of the urethra. (Carolin P., Cacho MD 2001).
Urinary tract infection (UTI) is classified as follows (EAU, 2008):
1. Type of pathogen (bacterial, fungal, mycobacterial);
2. Localization in the urinary tract:
a) diseases of the lower urinary tract (urethritis, cystitis)
b) diseases of the upper urinary tract (acute and chronic pyelonephritis)
3. Presence of complications, localization of UTI and combinations:
a) uncomplicated lower urinary tract infection (cystitis)
b) uncomplicated pyelonephritis
c) complicated UTI with or without pyelonephritis
d) urosepsis
e) urethritis
e) special forms (prostatitis, orchitis, epididymitis)
It is necessary to take into account age (elderly patients), the presence of concomitant diseases (including diabetes mellitus, etc.), the state of immunity (immune-compromised patients)
Uncomplicated UTIs usually respond successfully to appropriate antibiotic therapy.
Complicated UTIs are more difficult to respond to antimicrobial therapy and, in some cases, require the intervention of a urologist, since they can lead to severe purulent-septic complications.
Classification ICD 10
N 10 – acute tubulointerstitial nephritis (includes acute pyelonephritis)
N 11.0 – chronic tubulointerstitial nephritis (includes non-obstructive chronic pyelonephritis, reflux-associated)
N 11.1 – chronic obstructive pyelonephritis
N 11.8 – other chronic tubulointerstitial nephritis (includes non-obstructive pyelonephritis)
N 11.9 – chronic tubulointerstitial nephritis, unspecified (includes unspecified pyelonephritis)
N 12 – tubulointerstitial nephritis not defined as acute or chronic (includes pyelonephritis)
N 15.9 – tubulointerstitial kidney disease, unspecified (includes kidney infection, unspecified)
N 20.9 – urinary stones, unspecified (calculous pyelonephritis)
N 30.0 – acute cystitis
N 30.1 – interstitial cystitis (chronic)
N 30.8 – other cystitis
N 30.9 – unspecified cystitis
N 39.0 – urinary tract infection without established localization
Formulation of diagnosis
When formulating a diagnosis, the International Classification of Diseases, 10th revision, is used, indicating in chronic forms the nature of the course (recurrent, latent), phase of the disease (remission, exacerbation) and kidney function (stage of chronic kidney disease).
Taking into account the generally accepted international terminology, as well as the fact of the often occurring widespread ascending infection and the difficulties of clearly determining the localization of inflammation, it is advisable to use the term “urinary tract infection (UTI)” before the intended localization of the pathological process.
Here are examples of diagnosis formulations and the corresponding ICD-10 codes:
- Main Ds: UTI, chronic pyelonephritis, recurrent, exacerbation, CKD stage 1. (N 11.8)
Main Ds: UTI, acute right-sided pyelonephritis. (N 10) Complication: Paranephritis on the right.
Main Ds: UTI, acute cystitis. (N 30.0)
Epidemiology
Urinary infection remains one of the important causes of illness in various age groups. UTI is quite widespread; about 7 million outpatient visits and more than 1 million hospitalizations for UTI are registered annually in the United States. The economic cost is more than one billion dollars. 20-50% of women experience a UTI at least once in their lifetime. Women are more at risk of UTI, but the risk of UTI and its complications increases with age in both women and men (IDSA. 2001). In Russia, the most common urinary tract disease is acute cystitis (AC) - 26-36 million cases per year, with only 68 episodes per 10,000 in men aged 21-50 years. Acute pyelonephritis (AP) is also more common in women, and in all age groups. The incidence of AP is significantly higher than OC and ranges from 0.9 to 1.3 million cases annually. In women, the risk of UTI is 30 times higher than in men, including 4-10% due to pregnancy. In postmenopausal women, UTI develops in 20% of patients. The incidence of urinary tract diseases in the population of Irkutsk in 2007 was 6022 per 100,000 adults,
and mortality is 8 per 100,000 resident population
Currently, the main risk groups, clinical forms, diagnostic criteria for UTI have been identified, and effective ways to manage the infection in complicated and uncomplicated cases, including in risk groups, have been developed.
studfiles.net
Calculous pyelonephritis. Code N20.9
Develops against the background of kidney stones. If you identify the presence of stones in time and begin treatment, you can avoid chronicity of the disease.
Stones may not make themselves felt for years, making their diagnosis difficult. The appearance of severe pain in the lumbar region means only one thing - it’s time to contact a qualified specialist. It is sad that most patients are reluctant to consult a doctor at the first symptoms of the disease.
From the above it follows that this disease is a real chameleon among other pathologies. Insidious in its love to take the guise of other diseases, it can end sadly. Listen to your body. Do not drown out pain and other symptoms with self-medication. Seek help promptly.
Diagnostic principles
Diagnosing nephrosclerosis before it begins to manifest clinically is quite difficult, but possible. First of all, standard research methods are carried out: general and biochemical blood and urine tests. Rehberg's kidney test and Zimnitsky's urine test will also be indicative. Among the instrumental diagnostic methods, organ radiography and ultrasound are most often used.
Timely diagnosis is vital. After all, the sooner treatment is started, the greater the likelihood of avoiding a huge number of threatening pathological conditions.
N25—N29 Other diseases of the kidney and ureter
N25 Disorders resulting from renal tubular dysfunction
- N25.0
Renal osteodystrophy - N25.1
Nephrogenic diabetes insipidus - N25.8
Other disorders due to renal tubular dysfunction - N25.9
Renal tubular dysfunction, specified
N26 Shriveled kidney, unspecified
N27 Small kidney for unknown reason
- N27.0
Small kidney, unilateral - N27.1
Small kidney bilateral - N27.9
Small kidney, unspecified
N28 Other diseases of the kidney and ureter, not elsewhere classified
- N28.0
Renal ischemia and infarction - N28.1
Acquired kidney cyst - N28.8
Other specified diseases of the kidneys and ureter - N28.9
Diseases of the kidney and ureter, unspecified
N29* Other lesions of the kidney and ureter in diseases classified elsewhere
- N29.0*
Late syphilis of the kidney A52.7 - N29.1*
Other lesions of the kidney and ureter in infectious and parasitic diseases classified elsewhere - N29.8*
Other lesions of the kidneys and ureters in other diseases classified elsewhere
Add a comment Cancel reply
List of classes
- Class I. A00-B99. Some infectious and parasitic diseases
Excluded: autoimmune disease (systemic) NOS (M35.9)
disease caused by the human immunodeficiency virus HIV (B20 - B24) congenital anomalies (malformations), deformations and chromosomal disorders (Q00 - Q99) neoplasms (C00 - D48) complications of pregnancy, childbirth and the postpartum period (O00 - O99) certain conditions arising in the perinatal period (P00 - P96) symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere (R00 - R99) trauma, poisoning and some other consequences of external causes (S00 - T98) endocrine diseases, nutritional disorders and metabolic disorders (E00 - E90).
Note. All neoplasms (both functionally active and inactive) are included in class II. The corresponding codes in this class (for example, E05.8, E07.0, E16-E31, E34.-) can, if necessary, be used as additional codes to identify functionally active neoplasms and ectopic endocrine tissue, as well as hyperfunction and hypofunction of the endocrine glands, associated with neoplasms and other disorders classified elsewhere. Excluded: certain conditions arising in the perinatal period (P00 - P96), some infectious and parasitic diseases (A00 - B99), complications of pregnancy, childbirth and the puerperium (O00 - O99), congenital anomalies, deformities and chromosomal disorders (Q00 - Q99 ), diseases of the endocrine system, nutritional disorders and metabolic disorders (E00 - E90), injuries, poisoning and some other consequences of external causes (S00 - T98), neoplasms (C00 - D48), symptoms, signs and deviations from the norm identified in clinical and laboratory studies, not classified elsewhere (R00 - R99).
General information about the disease
Chronic pyelonephritis is a nonspecific inflammation of kidney tissue.
As a result of the spread of the pathological process, destruction of the vessels of the organ and pelvis is noted. The chronic form develops against the background of previously suffered acute pyelonephritis, in which treatment was carried out incorrectly or was completely absent. In some cases, the pathology may be asymptomatic and many patients do not even notice the presence of the disease. Pyelonephritis can become chronic for several reasons:
- urine reflux;
- inadequate treatment of the acute form;
- impaired excretion of urine as a result of narrowing of the urinary tract;
- chronic intoxication.
Chronic pyelonephritis according to ICD-10 has code N11 and is divided into several forms depending on various symptoms.
Statistical data
According to statistics, chronic pyelonephritis occurs in 60% of cases of genitourinary system disease with the development of an inflammatory process. In 20%, the pathology develops against the background of an acute course.
The chronic course differs from the acute course in that the pathological process affects both kidneys, while the organs are not affected equally. This form most often occurs latently, and remissions are replaced by exacerbations.
Nephrosclerosis of the kidneys
11.09.2017
Hypertensive nephrosclerosis, nephrosclerosis (shrinked kidney), hypertensive kidney disease, hypertensive disease, hypertensive nephropathy are synonyms of the same disease. Let's figure it out, kidney nephrosclerosis, what is it?
Characteristics of the disease
What is nephrosclerosis? The term hypertensive nephrosclerosis has traditionally been used to describe a clinical syndrome characterized by long-term hypertension, hypertensive retinopathy, left ventricular hypertrophy, minimal proteinuria, and progressive renal failure.
So, what is kidney nephrosclerosis, a health condition associated with kidney damage due to chronic high blood pressure, in which tissue is replaced by connective tissue and the kidney itself shrinks in size (“shrinks”). This leads to malfunctions up to the complete cessation of the functioning of the organ.
The disease can be divided into two types: benign and malignant. Benign nephrosclerosis is common in people over 60 years of age. The malignant form is rare and affects 1-5% of people with high blood pressure (diastolic blood pressure above 130 mm/Hg).
Hypertensive disease must be distinguished from renovascular hypertension, which is a form of secondary hypertension.
It is customary to distinguish two forms of this disease:
- primary wrinkled kidney—develops as a result of damage to the kidney vessels;
- Secondary wrinkled kidney - damage to the kidney tissue (parenchyma) in various diseases.
ICD code -10 –I12.
Nephrosclerosis symptoms and risk group
It cannot be said that the disease is asymptomatic; it’s just that not everyone seeks medical help on time, attributing all the symptoms to fatigue, a cold, overeating, etc.
Classic symptoms of chronic kidney disease:
- loss of appetite;
- urinary disorders;
- decrease in urine volume;
- the presence of constant pulling pain in the lower back;
- nausea;
- vomit;
- high blood pressure;
- itching;
- drowsiness or confusion;
- change in the appearance of urine (bloody, dark, strong-smelling, foamy);
- weight loss and bad taste in the mouth.
Symptoms may appear mild, but develop over time and become a chronic condition of the body. The risk group includes people with:
- poorly controlled moderate to high blood pressure;
- elderly age;
- other kidney diseases.
Cause of nephrosclerosis
Nephrosclerosis is not an independent disease. The term "hypertension" is used to refer to high blood pressure, and "nephropathy" refers to kidney damage.
It follows that the disease is caused by chronic high blood pressure, which causes damage to kidney tissue, including small blood vessels, glomeruli, renal tubules and interstitial tissues. The tissue hardens and thickens.
Constriction of blood vessels means that less blood flows into the tissue, which reduces the supply of oxygen, leading to tissue death (ischemia).
Mechanism of occurrence
As a result of benign arterial hypertension in the kidneys, hyaline (pink, amorphous, homogeneous material) accumulates in the walls of small arteries and arterioles, causing thickening of their walls and narrowing of the arterial openings, that is, a process known as atherosclerosis occurs. The resulting impaired blood flow causes tubular atrophy, interstitial fibrosis, glomerular changes, and scarring around the glomeruli. Additional complications often associated with hypertensive nephropathy include damage to the glomeruli, leading to protein and blood in the urine. Hypertensive nephropathy refers to kidney failure that can be attributed to a history of hypertension. However, despite the known association between hypertension and chronic kidney disease, the underlying mechanism remains unclear.
Glomerular ischemia, hypertension and hyperfiltration
High blood pressure can damage the endothelium, commonly known as the lining of a blood vessel, in the long term. This leads to the accumulation of plaques that settle in the renal arteries, causing stenosis and coronary kidney disease.
In this situation, the organ supplied by the narrowed artery suffers from inadequate blood flow, which in turn reduces its size. An alternative mechanism for hypertensive nephropathy is prolonged glomerular hypertension and hence glomerular hyperfiltration.
They can occur simultaneously, but do not have to. The idea is that hypertension leads to glomerular sclerosis, which ultimately means decreased kidney function.
As a compensatory mechanism, unaffected nephrons relax to increase blood flow to the kidney perfusion and increase glomerular filtration through the intact glomeruli.
Diagnostics
A doctor can make a diagnosis only based on medical history and biochemical studies. Chronic hypertension with progressive kidney disease results in increased concentrations of albumin in the urine (albuminuria).
Protein excretion in the urine usually does not cause symptoms, but can indicate many diseases of the genitourinary system. The most indicative is a 24-hour urine collection. The doctor recommends ultrasound diagnostics, and in some cases histology.
Etiology of the disease
Pyelonephritis develops as a result of the activation and spread of pathogenic microbes under the influence of various factors.
Most often this is infection with E. coli, streptococci, enterococci and other microorganisms. Additional causes of inflammation in the kidneys are:
- improper treatment of the acute form of the disease;
- urolithiasis, prostate adenoma, urine reflux and other diseases of the genitourinary system that were not promptly diagnosed and treated;
- proliferation of bacteria that remain in the kidney tissues for a long time;
- decreased immunity as a result of prolonged infectious diseases or immunodeficiency states;
- chronic pyelonephritis can be a complication after ARVI, tonsillitis, measles, pneumonia or scarlet fever (children are most susceptible);
- chronic pathologies such as diabetes, tonsillitis, obesity or bowel dysfunction;
- in women, pyelonephritis develops during pregnancy, after childbirth or during the onset of sexual activity;
- unidentified congenital diseases of the genitourinary system.
Hypothermia and the presence of autoimmune reactions can trigger the development of the pathological process.
Consequences of urolithiasis
If a person has kidney MCD, and what it is, how the condition manifests itself, he does not know, the disease may not be detected in time. This will lead to the development of complications: acute nephropathy, urolithiasis, problems in the functioning of the gastrointestinal tract system, as well as the risk of developing uric acid infarction.
With advanced renal pathology, all organ systems suffer, especially the central nervous system, which is responsible for a person’s psychological health. The positive thing is that all consequences are eliminated without surgical treatment.
Clinical picture
The chronic form of pyelonephritis can be asymptomatic. Signs do not appear during remission. They become pronounced during the acute stage. The main clinical manifestations of pyelonephritis include:
- Intoxication of the body . It is characterized by the presence of general weakness, nausea, vomiting, malaise, decreased appetite, fever and headaches and chills. When diagnosed, pale skin and tachycardia are noted.
- Painful sensations . Localized mainly in the lumbar region.
- Unpleasant urine odor can especially occur early in the morning, after sleep.
- Pain when urinating , frequent urge to go to the toilet.
Classification of the disease
Based on ICD-10, the types and forms of chronic pyelonephritis are determined by various factors. Highlight:
- Primary chronic form . Pathology develops on a healthy organ, the pathological process affects both kidneys.
- Secondary chronic form . It is a complication of another pathology. At first it is unilateral in nature, then the inflammation affects the second kidney.
A certain group of scientists prefers to divide pyelonephritis into a community-acquired form and a hospital-acquired form, when the patient requires hospitalization. Depending on the location of the pathological process, the following are distinguished:
According to the severity of the disease, the disease can be divided into:
- Complicated when other pathologies are associated.
- Uncomplicated, occurring without concomitant diseases.
A separate group includes pyelonephritis, which occurs with renal failure. Most often, complicated forms are diagnosed in male patients.
Treatment options
Diagnosis and therapy are complicated by the fact that in the remission stage the disease does not show symptoms.
Each patient with chronic pyelonephritis requires an individual approach and comprehensive treatment. First of all, to relieve symptoms during the exacerbation stage, medications are prescribed to relieve symptoms and destroy pathological microorganisms. When a chronic form of pyelonephritis is established, the following groups of drugs are prescribed:
- Cephalosporins. "Kefzol", "Cefepime" or "Tseporin";
- Semi-synthetic penicillins. “Amoxiclav”, “Ampicillin” or “Oxacillin” are broad-spectrum antibiotics that help destroy microorganisms that cause the development of the disease;
- “Negram”, the drug belongs to the group of nilidixic acids;
- in severe cases, Tobramycin, Gentamicin or Kanamycin are prescribed.
Ascorbic acid, Selenium, and Tocopherol are used as antioxidants. Antibiotics for chronic pyelonephritis are prescribed for up to eight weeks. In cases of severe exacerbation, antibacterial drugs are administered intravenously, which helps to achieve greater effectiveness and faster results. “5-NOK” is considered one of the most modern remedies for pyelonephritis. It helps relieve symptoms and relieve inflammation in a short time.
The patient should limit the consumption of fatty foods, salty and spicy foods, and also follow the drinking regime prescribed by the doctor.
Traditional methods
Treatment of the pathology can occur at home after stopping the exacerbation stage and only after consultation with the attending physician. The most effective are the following recipes:
- White acacia tea . Brew like regular tea. Drink half a glass for 10 days.
- Bean broth . Chop a glass of beans, pour a liter of boiling water, put on fire and bring to a boil. Take daily for 7 days in a row.
- Heather infusion . Pour two tablespoons of dried herbs into two glasses of boiling water and leave for an hour. Then strain and drink in large sips.
For pyelonephritis, baths with the addition of tincture of pine branches are also useful. The water temperature should not be less than 35 degrees. The duration of the bath is no more than 15 minutes. The course of treatment is 15 procedures.
Disease Prevention
To avoid the development of inflammation in the kidney tissues, a number of preventive measures should be followed. Experts recommend:
- avoid hypothermia;
- Healthy food;
- strengthen immunity;
- promptly treat infectious diseases.
The chronic form is dangerous because it may not manifest itself for a long time. The disease is diagnosed through the diagnosis of other pathologies. If symptoms occur, you should consult a doctor, since the acute form always develops into a chronic form, which is difficult to treat.