Presentation slides
Slide 2
Slide 3
Endoscopic methods continue to occupy an important place in the treatment of ureteral stones. At the same time, many researchers give preference to endoscopic methods of intervention over radiotherapy for stones located in the middle and tender third of the ureters. Kogan M.I., Romodanov D.A., Skorikov I.I., Kopylov V.V. Experience in endoscopic treatment of ureteral stones // In the book Urolithiasis. Edited by Perevezev A.S. - Kharkov, 1999. - pp. 185-186. Myagky V.M., Vovk V.M., Rudenko S.N. Experience in the use of contact ureterolithotripsy during exacerbation of pyelonephritis. // In the book Urolithiasis. Edited by Perevezev A.S. - Kharkov, 1999.-p.187-192
Slide 4
This is due to the fact that during occlusion, the stone damages the mucous and submucosal layers of the ureter, and the additional pathological effect in the area of urine damage further enhances the development of gross cicatricial processes, which, in the form of a sleeve, tightly envelop the stone and do not allow the passage of a ureteroscope to the stone and the implementation of contact lithotripsy or placing a loop above the stone for traction of the stone. 3. Kogan M.I., Romodanov D.A., Skorikov I.I., Kopylov V.V. Complications during endoscopic treatment of ureteral stones // In the book Urolithiasis. Edited by Perevezev A.S. - Kharkov, 1999. - pp. 186-187. 6. Tiktinsky O.L., Alexandrov V.P. Urolithiasis. SP b; 2000.
Slide 5
Slide 6
Slide 7
Computed tomography was also used to diagnose X-ray negative ureteral stones. The size of the stones ranged from 6 to 9 mm. The traditional drug therapy used in these patients to eliminate stones (antispasmodics, analgesics, antibacterial and diuretics) was not effective, and the patients abstained for a long time from the proposed methods of surgical treatment or extracorporeal lithotripsy and did not visit medical institutions. The duration of presence of stones in these areas ranged from 26 days to 3 months.
Slide 8
Balloon dilatation was performed using a Fogarty catheter. For this purpose, a Fogarty catheter No. 6 or No. 8 according to Frenth was inserted to the site of occlusion and the balloon was inflated with air in a dosed manner. To displace the stone from the occlusion zone to the part of the ureter dilated by the balloon, hemodilution was performed 30 minutes before the start of balloon dilatation, antispasmodics, α1-blockers and decongestants were prescribed.
Slide 10
For hemodilution, a 0.9% sodium chloride solution (400 ml), a 5% glucose solution (400 ml) and rheopolyglucin (200 ml) were used. Antispasmodics (No-spa 2 ml), diuretics (Lasix 2 ml) and decongestants (diclofenac sodium 3 ml) were administered intravenously along with solutions for hemodilution. Omnic (recently Omnic Ocas) 4 mg orally was used as an α1-blocker, which was prescribed to patients per os 2 hours before balloon dilatation. Immediately after balloon dilatation, a ureteroscope was inserted into the ureter and stone traction or contact lithotripsy was performed.
Slide 11
Slide 12
Preliminary pharmacodilation with Omnik (Omnik Okas) of the distal ureter significantly improved the conditions for carrying out a ureteroscope through the intramural and juxtavesical sections of the ureters. In this case, there is practically no need to bougienage the ureter, which significantly reduces the time for endoscopic manipulation. We also noted the advantages of preliminary pharmacodilation during catheterization and stenting of the ureter in previous studies Borisov O.V., Kostev F.I., Ukhal M.I., Borisov S.O. Victimization of pharmacodylation of the distal section of the duct during endourological surgery and conducting EUHL in patients with urolithiasis. -. Hospital surgery, 2001, No. 2. With. 101-102.
Slide 13
The stone moved to the dilatation zone in 15 of 18 patients (82.6%). This made it possible to place a conductor or loop above the stone for traction of the stone in all these patients. Contact lithotripsy was performed in all patients with stones exceeding 7 mm (11 people 73.3%). Stone traction was performed in 4 patients with stones from 6 to 7 mm.
Slide 15
Balloon dilatation made it possible to pass the ureteroscope into the distal zone of ureteral stenosis in all three cases, where it was not possible to displace the stone and conduct a session of contact lithotripsy. In two cases, we were able to fragment stones and eliminate fragments using special forceps. In one case, due to perforation of the ureter and the threat of urinary leakage, the patient underwent an open operation - ureterolithotomy with simultaneous excision of the ureter in the area of the scar process and the application of uretero-uretero anastomosis on the internal stent.
Coral stones are a special type of kidney stones
Coral kidney stones deserve special attention, the special form of which determines the clinical course of this type of urolithiasis. Coral stones are composed of ammonium, magnesium phosphate and calcium phosphate. Such stones are localized in the renal pelvis and calyces, and as they grow, they can spread to the entire calyceal system. Coral stones, like a cast, repeat the shape of the renal collecting system. In the process of growth of coral stones, three main stages are distinguished:
- In the first degree, the kidney stone is almost completely located in the renal pelvis, but has peculiar processes towards the renal cups.
- In the second degree, the processes of the coral stone fill all the large cups of the kidney.
- In the third degree, the coral stone completely fills the renal pelvis and calyces, forming branches at the level of the small calyces.
Tips for making a good presentation or project report
- Try to involve the audience in the story, set up interaction with the audience using leading questions, a game part, do not be afraid to joke and smile sincerely (where appropriate).
- Try to explain the slide in your own words, add additional interesting facts; you don’t just need to read the information from the slides, the audience can read it themselves.
- There is no need to overload the slides of your project with text blocks; more illustrations and a minimum of text will better convey information and attract attention. The slide should contain only key information; the rest is best told to the audience orally.
- The text must be well readable, otherwise the audience will not be able to see the information being presented, will be greatly distracted from the story, trying to at least make out something, or will completely lose all interest. To do this, you need to choose the right font, taking into account where and how the presentation will be broadcast, and also choose the right combination of background and text.
- It is important to rehearse your report, think about how you will greet the audience, what you will say first, and how you will end the presentation. All comes with experience.
- Choose the right outfit, because... The speaker's clothing also plays a big role in the perception of his speech.
- Try to speak confidently, smoothly and coherently.
- Try to enjoy the performance, then you will be more at ease and less nervous.
Counteract the disease first; It’s too late to think about medicine when the disease has taken root from a long delay.
Slide 2
The work was completed by: 8th grade student of the MB OU Pelya - Khovanskaya Secondary School Andrey Vilkov
Life is short, the path of art is long, opportunity is fleeting, experience is deceptive, judgment is difficult. Therefore, not only the doctor himself must use everything that is necessary, but also the patient, those around him, and all external circumstances must contribute to the doctor in his activities.
Hippocrates
Slide 3
Urolithiasis (UCD)
Urolithiasis (UCD) is a fairly common disease: 3-9 people out of 100 have this pathology. In young and middle-aged men, urolithiasis occurs 2-3 times more often, but women “catch up” with men during menopause, when the risk of stone formation increases significantly. The fact is that during the childbearing period, female sex hormones (estrogens) prevent the formation of stones in the urine.
Slide 4
The essence of urolithiasis is that crystallization and precipitation of salts occurs in the urine tract. Some crystals are layered on top of others, forming sand and stones. Moreover, more often this occurs in the renal pelvis, somewhat less often in the bladder. Attacks of pain, renal colic, complications in the form of secondary infection and bleeding from the urinary tract do not appear immediately. At first, the disease is usually asymptomatic. Small stones may pass on their own in 1-3 weeks, especially if their diameter is less than 5 mm. If the stones are larger (10 mm), then they pass away on their own in only 50% of cases. As long as the stone does not move, it does not make itself felt; pain occurs precisely when it moves.
Slide 5
It happens that stones in the renal pelvis are discovered during examination by chance, in the absence of any symptoms. The question arises what to do with them. This is decided by the urologist. You can live with a small stone, if it does not cause inflammation or renal colic and does not impair kidney function. Some stones are crushed (using shock wave lithotripsy), and if this is not possible, they are removed promptly. Our goal is to prevent the formation of stones. Let's talk about this.
Slide 6
Multi-colored rockfall
Urinary stones are distinguished by their composition, depending on the salts they contain. More often they are mixed - they contain both organic and inorganic parts, and there may be much more of some salts in them than others. This is very important to know, since this is what preventative measures depend on. The first information about the content of salt crystals and their composition can be obtained from the results of a clinical urine test.
Slide 7
What kind of stones form in the urinary tract?
Most often these are oxalates (from oxalic acid salts). They fall out in alkaline urine, are spiny, dense, and irregular in shape. They can easily injure the urinary tract, therefore they are considered the most dangerous. If oxalate crystals have ever been found in the urine, it is imperative to carry out prevention of KSD. ♦ Another type of stones is urate (from uric acid and its salts). They are round (often cluster-shaped), darker (in general, the color depends on pigment inclusions), and fall out in acidic urine. Urates can be combined with phosphates.
Slide 8
- Phosphates (from salts of phosphoric acid) have an irregular shape, they are rough, grayish or white. These stones are fragile and crumble easily. As a rule, they fall out in alkaline urine.
- Other types of stones are much less common - cysteine, protein, etc.
- Slide 9
Causes of the disease
Normally, salts in urine are only in a dissolved state; crystals begin to form only due to a violation of mineral metabolism. It is believed that this disorder is polyetiological, that is, the onset of crystallization is promoted not by one, but by several different factors, each of which can act as the main one. Who is more likely to get urolithiasis? What leads to the formation of stones?
- Slide 10
Presentation for urologists: urolithiasis. Urolithiasis disease. Presentation on the topic
URINOLOGICAL DISEASE URILOTHIC DISEASE Urolithiasis (urolithiasis) is one of the most common causes of surgery on the kidneys and ureters. Urolithiasis (urolithiasis) is one of the most common causes of surgery on the kidneys and ureters. Much is known about it, but all the reasons for the formation of stones have not yet been clarified. Even now, discussions continue regarding the problems of etiology, pathogenesis and prevention of both the disease itself and its relapses. Much is known about it, but all the reasons for the formation of stones have not yet been clarified. Even now, discussions continue regarding the problems of etiology, pathogenesis and prevention of both the disease itself and its relapses. Urolithiasis accounts for % of all urological diseases. Urolithiasis accounts for % of all urological diseases.
Etiology and pathogenesis Urolithiasis is a polyetiological disease. Urolithiasis is a polyetiological disease. It occurs as a result of congenital anomalies, climatic conditions, deficiency of vitamins and microelements, hormonal disorders, changes in urine pH, inflammatory processes, and the like. It occurs as a result of congenital anomalies, climatic conditions, deficiency of vitamins and microelements, hormonal disorders, changes in urine pH, inflammatory processes, and the like. Congenital tubulopathies (enzymopathies) create the background for subsequent stone formation. Congenital tubulopathies (enzymopathies) create the background for subsequent stone formation. They are a violation of metabolic processes in the body or the function of nephron tubules as a result of insufficiency or absence of any enzyme. In this case, a blockade of metabolic processes occurs. They are a violation of metabolic processes in the body or the function of nephron tubules as a result of insufficiency or absence of any enzyme. In this case, a blockade of metabolic processes occurs.
Etiology (according A. Pitel and I. Pogorelko) A). Disorders of urinary tract: A). Disorders of urinary tract: congenital abnormalities those favor to apostasies; congenital abnormalities those favor to apostasies; obstructive processes; obstructive processes; neurogenic duskiness of the urinary tract; neurogenic duskiness of the urinary tract; inflammative and parasitogenic damages; inflammative and parasitogenic damages; foreign bodies of urinary tract; foreign bodies of urinary tract; traumatic injuries. traumatic injuries. B) Liver and digestive tract disorders: B) Liver and digestive tract disorders: latent and manifested hepathopathy; latent and manifested hepathopathy; hepatogenic gastritis; hepatogenic gastritis; colitis, etc. colitis, etc. C) Endocrine diseases C) Endocrine diseases hyperparathyreoidism; hyperparathyroidism; hyperthyroidism; hyperthyroidism; hypopituitary diseases; hypopituitary diseases; D) Infect focuses on the urogenital system. D) Infect focuses on the urogenital system. E) Metabolism disorders. E) Metabolism disorders. essential hypercalciuria; essential hypercalciuria; disorders of membranes for colloid substances diffusion; disorders of membranes for colloid substances diffusion; renal rickets, etc renal rickets, etc F) Injuries those lead to continuous immobilization F) Injuries those lead to continuous immobilization fractures of the vertebral column and limbs fractures of the vertebral column and limbs osteomyelitis osteomyelitis diseases of the bones and joints diseases of the bones and joints chronic diseases of the visceral organs and nervous system. chronic diseases of the visceral organs and nervous system. G) Climate and geographical causes. G) Climate and geographical causes. dry and hot climate with a high vaporization dry and hot climate with a high vaporization decrease water supply decrease water supply iodine deficiency iodine deficiency H) Disorders of nutrition and vitamins balance: H) Disorders of nutrition and vitamins balance: retinole and oscorbine acid deficiency in food. retinole and oscorbine acid deficiency in food. excessive amount of the ergocalciferole in organism. excessive amount of the ergocalciferole in organism.
Risk factors Medication associated with stone formation: Medication associated with stone formation: calcium supplements calcium supplements vitamin D supplements vitamin D supplements acetazolamide - ascorbic acid in megadoses (> 4 g/day) acetazolamide - ascorbic acid in megadoses (> 4 g/day) sulphonamides - triamterene sulphonamides - triamterene Anatomical abnormalities associated with stone formation: Anatomical abnormalities associated with stone formation: tubular ectasia (medullary sponge kidney) tubular ectasia (medullary sponge kidney) pelvo-ureteral junction obstruction pelvo-ureteral junction obstruction calix diverticulum, calix cyst calix diverticulum, calix cyst ureteral stricture ureteral stricture vesico-ureteral reflux vesico-ureteral reflux horseshoe kidney horseshoe kidney ureterocele ureterocele 4 g/day) acetazol»> 4 g/day) acetazolamide — ascorbic acid in megadoses (> 4 g/day) sulphonamides — triamterene sulphonamides - triamterene Anatomical abnormalities associated with stone formation: Anatomical abnormalities associated with stone formation: tubular ectasia (medullary sponge kidney) tubular ectasia (medullary sponge kidney) pelvo-ureteral junction obstruction pelvo-ureteral junction obstruction calix diverticulum, calix cyst calix diverticulum, calix cyst ureteral stricture ureteral stricture vesico-ureteral reflux vesico-ureteral reflux horseshoe kidney horseshoe kidney ureterocele ureterocele"> 4 g/day) acetazol" title="Risk factors Medication associated with stone formation: Medication associated with stone formation: calcium supplements calcium supplements vitamin D supplements vitamin D supplements acetazolamide — ascorbic acid in megadoses (> 4 g/day) acetazol"> title="Risk factors Medication associated with stone formation: Medication associated with stone formation: calcium supplements calcium supplements vitamin D supplements vitamin D supplements acetazolamide — ascorbic acid in megadoses (> 4 g/day) acetazol»>
Coral stones It has been proven that in many cases hyperparathyroidism leads to kidney pathology: the formation of stones and nephrocalcinosis, when calcium salts accumulate (deposit) in the renal parenchyma, gradually predetermining its necrosis. It has been proven that in many cases, hyperparathyroidism leads to kidney pathology: the formation of stones and nephrocalcinosis, when calcium salts accumulate (deposit) in the renal parenchyma, gradually predetermining its necrosis. Since the process is bilateral, it leads to progression of kidney failure. Since the process is bilateral, it leads to progression of kidney failure.
Clinic The main symptoms of urolithiasis are pain in the lumbar region, hematuria, discharge of salts and stones in the urine. The main symptoms of urolithiasis are pain in the lumbar region, hematuria, and the passage of salts and stones in the urine. The intensity of pain and its irradiation depend on the location of the stone. The pain can be dull and sharp. The intensity of pain and its irradiation depend on the location of the stone. The pain can be dull and sharp. Dull pain is typical for inactive stones. It intensifies with movement and excessive fluid intake. Dull pain is typical for inactive stones. It intensifies with movement and excessive fluid intake. Acute pain is manifested by renal colic. It can be caused by a sudden cessation of urine flow due to blockage of the upper urinary tract by a stone. Acute pain is manifested by renal colic. It can be caused by a sudden cessation of urine flow due to blockage of the upper urinary tract by a stone.
Clinic The duration of renal colic varies. The duration of renal colic varies. It is accompanied by weakness, dry mouth, headache, chills, increased body temperature, dysuria, and motor agitation of the patient. It is accompanied by weakness, dry mouth, headache, chills, increased body temperature, dysuria, and motor agitation of the patient. The lower the stone descends along the ureter, the more pronounced the dysuric disorders. The lower the stone descends along the ureter, the more pronounced the dysuric disorders.
Clinic A complication of urolithiasis is hydronephrotic transformation, which may not manifest itself for a long time. A complication of urolithiasis is hydronephrotic transformation, which may not manifest itself for a long time. The addition of an infection aggravates the course of the disease. The addition of an infection aggravates the course of the disease. In the case of complete destruction of both kidneys as a result of pyelonephritis and hydronephrotic transformation, anuria can become the final stage of the disease. We are talking about the progress of chronic kidney failure, which leads to oliguria, and then to anuria. Anuria can also occur against the background of sufficient diuresis as a result of an attack of acute pyelonephritis. In the case of complete destruction of both kidneys as a result of pyelonephritis and hydronephrotic transformation, anuria can become the final stage of the disease. We are talking about the progress of chronic kidney failure, which leads to oliguria, and then to anuria. Anuria can also occur against the background of sufficient diuresis as a result of an attack of acute pyelonephritis.
Laboratory tests Stone analysis: In every patient one stone should Stone analysis: In every patient one stone should be analyzed. be analyzed. Blood analysis: Calcium Albumin Creatinine Urate Blood analysis: Calcium Albumin Creatinine Urate Urinalysis: Fasting morning spot urine sample Urinalysis: Fasting morning spot urine sample Dip-stick test: pH, Leucocytes/Bacteria Dip-stick test: pH, Leucocytes/Bacteria Cystine test , Ca, P, citrate, urate Cystine test, Ca, P, citrate, urate
Excretory urography Usually, excretory urograms reveal X-ray negative stones in the form of filling defects. Usually, excretory urograms reveal X-ray negative stones in the form of filling defects. If the image does not give a clear idea of the pathology, and the symptoms are characteristic of a stone, retrograde pneumography and pyelography are used. If the image does not give a clear idea of the pathology, and the symptoms are characteristic of a stone, retrograde pneumography and pyelography are used.
Endovesical methods Cystoscopia shows swallowing of the ureter orifice in lower location of the stone, it may also partially project out to the orifice. Cystoscopia shows swallowing of the ureter orifice in lower location of the stone, it may also partially project out to the orifice.
Treatment of pain Drugs aimed at relieving renal colic: Diclofenac sodium Diclofenac sodium Indomethacin Indomethacin Hydromorphone hydrochloride + atropine sulphate Hydromorphone hydrochloride + atropine sulphate Baralgin Baralgin No-spae + Analgine No-spae + Analgine Tramadol Tramadol
Renal colic At the beginning of an attack of renal colic, administration of an increased dose of cystenal (20 drops per lump of sugar) is effective. At the beginning of an attack of renal colic, administration of an increased dose of cystenal (20 drops per lump of sugar) is effective. If the pain does not disappear, a novocaine blockade of the spermatic cord is performed in men and the place of attachment of the round ligament of the uterus to the abdominal wall in women. Usually, a ml of 0.25% novocaine solution warmed to body temperature is sufficient for this. If the pain does not disappear, a novocaine blockade of the spermatic cord is performed in men and the place of attachment of the round ligament of the uterus to the abdominal wall in women. Usually, a ml of 0.25% novocaine solution warmed to body temperature is sufficient for this. Novocaine blockade provides not only a therapeutic effect. It also makes it possible to differentiate right-sided renal colic from acute appendicitis, in which the blockade does not eliminate pain. Novocaine blockade provides not only a therapeutic effect. It also makes it possible to differentiate right-sided renal colic from acute appendicitis, in which the blockade does not eliminate pain.
Catheterization In cases where the above methods are ineffective, catheterization of the ureter is prescribed. In cases where the above methods are ineffective, ureteral catheterization is prescribed. If you manage to get past the stone and eliminate urinary stasis, the pain immediately stops. The catheter is left in the ureter for several hours. If you manage to get past the stone and eliminate urinary stasis, the pain immediately stops. The catheter is left in the ureter for several hours. percutaneous nephrostomy
Stone passage Spontaneous stone passage can be expected in up to 80% of patients with stones not larger than 4 mm in diameter. For stones with a diameter exceeding 7 mm the chance of spontaneous passage is very low. Spontaneous stone passage can be expected in up to 80% of patients with stones not larger than 4 mm in diameter. For stones with a diameter exceeding 7 mm the chance of spontaneous passage is very low. The overall passage rate of ureteral stones is: Proximal ureteral stones: 25% Proximal ureteral stones: 25% Mid-ureteral stones: 45% Mid-ureteral stones: 45% Distal ureteral stones: 70% Distal ureteral stones: 70%
Indications for active tactics Stone removal is usually indicated for stones with a diameter exceeding 6-7 mm. Stone removal is usually indicated for stones with a diameter exceeding 6-7 mm. Active stone removal is strongly recommended in patients fulfilling the following criteria: Active stone removal is strongly recommended in patients fulfilling the following criteria: - persistent pain despite adequate medication; — persistent pain despite adequate medication; — persistent obstruction with risk of impaired renal function; — persistent obstruction with risk of impaired renal function; — stone with urinary tract infection; — stone with urinary tract infection; — risk of pyonephrosis or urosepsis; — risk of pyonephrosis or urosepsis; — bilateral obstruction; — bilateral obstruction; — obstructing calculus in a solitary functioning kidney. — obstructing calculus in a solitary functioning kidney.
Lithotripsy In patients with coagulation disorders the following treatments are contra-indicated: extracorporeal shock wave lithotripsy (ESWL), percutaneous nephrolithotomy with or without lithotripsy (PNL), ureteroscopy (URS) and open surgery. In patients with coagulation disorders the following treatments are contra-indicated: extracorporeal shock wave lithotripsy (ESWL), percutaneous nephrolithotomy with or without lithotripsy (PNL), ureteroscopy (URS) and open surgery. In pregnant women, ESWL, PNL and URS are contra-indicated. In expert hands URS has been successfully used to remove ureteral stones during pregnancy, but it must be emphasized that complications of this procedure might be difficult to manage. In pregnant women, ESWL, PNL and URS are contra-indicated. In expert hands URS has been successfully used to remove ureteral stones during pregnancy, but it must be emphasized that complications of this procedure might be difficult to manage. In such women, the preferred treatment is drainage, either with a percutanous nephrostomy catheter, a double — J stent or a ureteral catheter. In such women, the preferred treatment is drainage, either with a percutanous nephrostomy catheter, a double — J stent or a ureteral catheter. For patients with a pacemaker it is wise to consult a cardiologist before undertaking an ESWL treatment. For patients with a pacemaker it is wise to consult a cardiologist before undertaking an ESWL treatment.
Percutaneous nephrostomy. Percutaneous nephrostomy. Because of this technique, urologists can now perform operative procedures within the kidney without using the standard large flank incisions and mobilization of the kidney. Because of this technique, urologists can now perform operative procedures within the kidney without using the standard large flank incisions and mobilization of the kidney. This technique, along with refinements in endoscopic instruments and advances in fiberoptics, allows endoscopic manipulation in the upper urinary tract by the percutaneous approach. This technique, along with refinements in endoscopic instruments and advances in fiberoptics, allows endoscopic manipulation in the upper urinary tract by the percutaneous approach. Percutaneous nephrolithotomy with or without lithotripsy (PNL) Percutaneous nephrolithotomy with or without lithotripsy (PNL)
Stone extraction Cystoscopic technique Cystoscopic technique With the patient under anesthesia and with fluoroscopic control, stones in the distal ureter can sometimes be removed with a wire stone basket. With the patient under anesthesia and with fluoroscopic control, stones in the distal ureter can sometimes be removed with a wire stone basket. Ureteropyeloscopy Ureteropyeloscopy Manipulation of small ureteral stones under direct vision with a ureteroscope is a major advance in the management of ureteral calculi. With this technique, small stones can be easily trapped in a stone basket and safely extracted through the dilated ureter. Manipulation of small ureteral stones under direct vision with a ureteroscope is a major advance in the management of ureteral calculi. With this technique, small stones can be easily trapped in a stone basket and safely extracted through the dilated ureter.
Extracorporeal lithotripsy An extracorporeal noninvasive technique that uses shock waves to disintegrate urinary calculi while the patient is immersed in a water bath has been tested extensively and is now in clinical use. An extracorporeal noninvasive technique that uses shock waves to disintegrate urinary calculi while the patient is immersed in a water bath has been tested extensively and is now in clinical use. With this technique, calculi in the upper urinary tract are reduced to fragments, which pass spontaneously from the collecting system and bladder in most patients. With this technique, calculi in the upper urinary tract are reduced to fragments, which pass spontaneously from the collecting system and bladder in most patients. Size, location, and consistency of stone determine the number of shocks needed for fragmentation. In general, between 500 and 2,000 shocks arc necessary to fragment and pulverize an intrarenal calculus sufficiently for complete passage. Size, location, and consistency of stone determine the number of shocks needed for fragmentation. In general, between 500 and 2,000 shocks arc necessary to fragment and pulverize an intrarenal calculus sufficiently for complete passage.
Indications for surgical treatment Frequent attacks of the renal colic or persistent pain that disables the patient. Frequent attacks of the renal colic or persistent pain that disables the patient. Disorder of the urine outflow causing the hydronephrotic degeneration of the kidney. Disorder of the urine outflow causing the hydronephrotic degeneration of the kidney. Obturative anuria. Obturative anuria. Frequent attacks of the acute pyelonephritis, progress of the chronic pyelonephritis that causes renal insufficiency. Frequent attacks of the acute pyelonephritis, progress of the chronic pyelonephritis that causes renal insufficiency. Total hematuria. Total hematuria. Calculous pyonephrosis, apostematous pyelonephritis or carbuncle of the kidney. Calculous pyonephrosis, apostematous pyelonephritis or carbuncle of the kidney. Stone at the sole kidney that causes obstruction. Stone at the sole kidney that causes obstruction. Stone in the ureter of the sole kidney that wont pass away spontaneously. Stone in the ureter of the sole kidney that wont pass away spontaneously.
Open surgical treatment of Pyelolithotomy: Pyelolithotomy: Simple pyelolithotomy is used for removal of calculi confined to the renal pelvis. Simple pyelolithotomy is used for removal of calculi confined to the renal pelvis. Minimal dissection of the renal sinus is usually needed, and exposure of the entire kidney is not required. Minimal dissection of the renal sinus is usually needed, and exposure of the entire kidney is not required.
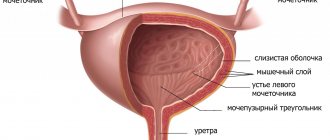
Open surgical treatment of Ureterolithotomy. Ureterolithotomy. There are retroperitoneal, transperitoneal and combined surgical accesses. It depends on stone location. There are retroperitoneal, transperitoneal and combined surgical accesses. It depends on stone location. To remove stone from the superior ureter the Fedorovs access is used, from medial ureter – Cuckulidzes or Derevyanko access is performed, the inferior ureter – Pyrogovs access is needed, the pelvic portion of ureter may be accessed through the suprapubic arcuate incision. To remove stone from the superior ureter the Fedorovs access is used, from medial ureter – Cuckulidzes or Derevyanko access is performed, the inferior ureter – Pyrogovs access is needed, the pelvic portion of ureter may be accessed through the suprapubic arcuate incision. Bladder stones Primary stones of the bladder are relatively rare in the USA but occur commonly in children in parts of India, Indonesia, the Middle East, and China. These stones usually occur in sterile urine. They are uncommon in girls. Primary stones of the bladder are relatively rare in the USA but occur commonly in children in parts of India, Indonesia, the Middle East, and China. These stones usually occur in sterile urine. They are uncommon in girls. Secondary vesical stones form as a result of other urologic conditions. Secondary vesical stones form as a result of other urologic conditions. They nearly always occur in men and are frequently associated with urinary stasis and chronic urinary tract infection. They nearly always occur in men and are frequently associated with urinary stasis and chronic urinary tract infection. Urinary obstruction may be due to prostatic hyperplasia or urethral stricture. Urinary obstruction may be due to prostatic hyperplasia or urethral stricture. Neurogenic vesical dysfunction may be a cause of chronic infection and urinary retention with eventual stone formation. Neurogenic vesical dysfunction may be a cause of chronic infection and urinary retention with eventual stone formation.
Clinic Patients with bladder stones frequently give a history of hesitancy, frequency, dysuria, hematuria, dribbling, or chronic urinary tract infection unresponsive to antimicrobial drug therapy. Patients with bladder stones frequently give a history of hesitancy, frequency, dysuria, hematuria, dribbling, or chronic urinary tract infection unresponsive to antimicrobial drug therapy. Sudden interruption of the urinary stream associated with the acute onset of pain radiating down and along the penis may occur when the stone intermittently obstructs the bladder neck. Sudden interruption of the urinary stream associated with the acute onset of pain radiating down and along the penis may occur when the stone intermittently obstructs the bladder neck.
Diagnostics Most vesical stones are radiopaque and apparent on a plain film of the pelvis. Most vesical stones are radiopaque and apparent on a plain film of the pelvis. Oblique films may be helpful in differentiating bladder stones from calcifications in ovaries, lymph nodes, or uterine fibroids. Oblique films may be helpful in differentiating bladder stones from calcifications in ovaries, lymph nodes, or uterine fibroids.
Treatment Small bladder stones may be removed by transurethral irrigation. Small bladder stones may be removed by transurethral irrigation. Larger stones may be crushed by one of a variety of different manual lithotrities and removed from the bladder by irrigation. Larger stones may be crushed by one of a variety of different manual lithotrities and removed from the bladder by irrigation. Ultrasonic and electrohydraulic lithotriptors are available to fragment large bladder calculi. Ultrasonic and electrohydraulic lithotriptors are available to fragment large bladder calculi.
Slide 1
Slide 2
Urolithiasis Types of stones Calcium stones X-ray positive More common in men The first stone is formed and detected at the age of 20-30 years. The second is formed over the next 10 years. After removing a stone, a new one will form within 2-3 years. Urate stones X-ray negative Half of the patients suffer from gout Half have a complicated hereditary history
Slide 3
Urolithiasis Types of stones Cystine stones X-ray positive Contain sulfur and are yellow in color. Tripelphosphate stones X-ray positive More often in women and patients with catheters - sources of bacteria that produce urease. The stones are large in size and act as pelvises and cups. Tipelphosphate, urate and cystine stones reach large sizes - coral stones - large sizes, acting as a collecting system, do not move.
Slide 4
Urolithiasis Calcium stones Grow on the renal papillae. Ultrasound or radiographic studies reveal multiple calcifications - nephrocalcinosis. Typically occur with severe hypercalciuria. Putty Cystine and uric acid in high concentrations precipitate as “putty.” May cause obstruction of the ureters. 1 g of uric acid and 400-800 mg of cysteine may fall out per day. Oxalates do not form putty
Slide 5
Urolithiasis Stones are considered as a constant source of infection Localized on the stone itself Impaired passage of urine
Slide 6
Urolithiasis To diagnose urolithiasis, ultrasound of the kidneys is performed. X-ray of the kidneys - excretory and survey urography. Determination of Calcium. Uric acid; pH of urine; Oxalates and citrates in urine; Electrolytes.
Slide 7
Urolithiasis General principles of treatment Always combined - therapist + surgeon Avoid dehydration The volume of drink is selected individually based on the volume of urine (≥ 2 l/day) Evaluate the dynamics of stone localization, volume, kidney function, presence of infection, formation of indications for surgery Removal by open access, endoscopically , with cystoscopy, extracorporeal lithotripsy.
Slide 8
Urolithiasis When verifying calcium stones The drug of choice is thiazide diuretics When verifying urate stones Increase in urine pH Reduction of uric acid excretion - goal less than 1 g/day Diet with a low purine content Alkaline solutions (drinking) Allopurinol 100 mg/day
Conservative treatment is not an alternative to stone removal using one of the modern methods of surgical treatment: percutaneous and endoscopic operations, radiation therapy, open surgical treatment. Conservative therapy, the duration of which is determined individually, is one of the stages in the complex treatment of the patient.
CONSERVATIVE THERAPY for urolithiasis A set of therapeutic measures aimed at correcting metabolic disorders of stone-forming substances in the body: 1. diet therapy (individual); 2. Maintaining adequate water balance; 3. Drug therapy; 4. Herbal medicine; 5. Physiotherapy and balneotherapy; 6. Physical therapy; 7. Sanatorium-resort treatment
DIET RECOMMENDATIONS FOR ICD Modern dietary recommendations: 1. The diet should be prescribed taking into account metabolic disorders, as well as individual eating habits; 2. Ca 2++ limitation should be avoided; 3. A balance of calcium and oxalates is necessary; 4. Maximum limitation of the volume of food, especially rich in stone-forming substances, its variety, consumption of animal protein and NaCl should be “adequate” or moderately limited; 5. K+ intake should be high; 6. Fluid intake should ensure the formation of at least 2 liters. urine per day (recommended cranberry juice, lingonberry, mineral water)
LIQUID CONSUMPTION Fluid intake has a target rel. urine density up to 1010 g/l; Is hard water (Ca ++ and Mg ++) dangerous for ICD? — the content of Ca++ in drinking water increases the excretion of Ca++, but the excretion of Ox (Ca++ binds Ox); — bicarbonate increases the excretion of citrate, and the content of Mg ++ in water has a beneficial effect on the excretion of citrate and Mg ++ (protective factors).
FLUID CONSUMPTION -Tea, coffee and white wine risk of ICD ability of caffeine and alcohol to inhibit antidiuretic hormone dilution of urine; — Drinking grapefruit juice risks the formation of stones (the effect remains unclear); — Orange and lemon juices are healthy because they have a high citrate content.
“WATER LOAD” If there is a tendency to urolithiasis (history) and severe crystalluria (CAM), it is recommended to resort to “water stress”: Simultaneous intake on an empty stomach of 0.5-1 low-mineralized mineral water, beer, compotes, tea, 1 watermelon, and contraindications (cardiovascular diseases, etc...) taking decoctions of diuretic herbs and diuretics (triampur) diuretic effect and flushing the kidneys 1 time every 7-10 days.
Diet therapy includes measures to maintain urine pH (normally 6.2-6.4). Fluctuations can be from 5.0 to 7.0 (sleep, eating) Reasons that cause changes in urine pH: pH values: - consumption of acids; - abundant consumption of fat and protein; - loss of gastric contents; - hunger, physical stress, diabetes, chronic renal failure, gout; pH values: - vegetarian diet; - urinary infection; - use of alkalis; - diarrhea, hypokalemia, PCA, respiratory alkalosis; REGULATION OF URINE pH
Calcium restriction should not be recommended for hypercalciuria! Previously, this was a popular recommendation 1. There is no clear distinction between calcium absorption and renal hypercalciuria; 2. There are no studies showing that calcium leads to a reduction in relapses of urolithiasis; 3. calcium leads to secondary hyperoxaluria; 4. dietary calcium predisposes to bone loss due to negative calcium balance; 5. Chronic calcium restriction can lead to disruption of Vit.D metabolism, which leads to more intense calcium absorption in the intestine and bone resorption. CALCIUM AND LAB
OXALATES AND LAB The main dietary recommendation is a joint restriction of Ca 2++ and oxalates!; Spinach, sorrel and rhubarb contain large amounts of bioavailable oxalates - RISK; Peanuts, tea, almonds, chocolate and nuts - RISK; 1 large milk chocolate bar – 95 g oxalates and 430 mg. Ca 2++ does not cause an increase in oxalate or Ca 2++ excretion; Consumption of oxalates is not accompanied by hyperoxaluria if Ca 2++ binds oxalate in the intestinal lumen: a 20-fold oxalate load should be accompanied by consumption of Ca 2++ (up to 4 g/day); Ca2++ limitation
PROTEIN AND LAB Consumption of protein leads to the excretion of stone-forming substances: - Hyperuricuria () due to purine overload; - Hyperoxaluria () due to the synthesis of oxalates; — Hypercalciuria () — Hypocitraturia () due to increased reabsorption of citrate; Reducing protein intake leads to the opposite changes.
When consuming K + (16 g/day): - with K + hypercalciuria occurs; - when Na+ in food is 100 mmol, Ca 2++ excretion in urine is 25 mg; — hypocitraturia () occurs both with K + and with NaCl consumption; Corresponding recommendations follow from this. POTASSIUM, SODIUM AND LAB
4 g/day), since 40% of exogenous ascorbic acid is metabolized into oxalic acid (during the analysis) Ox + Ca2 ++ (always available "title="VITAMIN "C" AND LAB Theory: Medication, the use of which may be associated with ICD is vitamin C (>4 g/day), since 40% of exogenous ascorbic acid is metabolized into oxalic acid (during the analysis) Ox + Ca2 ++ (always available "class="link_thumb"> 17
At what levels can kidney stones cause obstruction?
Kidney stones can be single or multiple, which is of fundamental importance for the choice of treatment tactics. During diagnosis, it is important to clarify the shape, size and location of stones, since the location in which stones can cause obstruction largely determines the clinical picture and subsequent course of the pathological process. There are three main risk areas where a stone can cause obstruction:
- ureteropelvic segment - in this area the wide pelvis narrows to 2-3 mm. and passes into the ureter, which has a diameter of up to 19 mm;
- the area where the ureter crosses the upper edge of the entrance to the pelvis - at the intersection with the iliac vessels, the diameter of the ureter narrows to 3-4 mm;
- vesicoureteral segment - the ureter in this area also narrows to 2-4 mm.
Share:
Causes of stone formation
Diseases of various kinds change environmental parameters. Mainly pH factor (5.5 – 6). Or variations in parameters become a prerequisite for dysfunction. As a result of inflammation, the body's own protein, including blood elements (erythrocytes, leukocytes, bacteria), enters inside. At the same time, the dynamics of urine output are disrupted. Similar consequences are provoked by injuries.
Changes in the pH factor are caused by a number of diseases:
- Catarrhal cystitis.
- Central nervous system disorders.
- Diathesis (oxaluria, uraturia, phosphaturia).
- Diseases of the gastrointestinal tract.
- Injuries and diseases of the musculoskeletal system.
- Viral infections, for example, malaria.
Acidification of the body leads to increased excretion of calcium. As a result, the concentration of salts in the urine increases, and the kidney is at risk. Pathologies of the parathyroid gland and pituitary gland affect calcium metabolism.