Kidney surgery in a child will help cope with kidney failure and other serious diseases. Impacts on the organ can vary: from internal examination to transplantation or removal. Carrying out procedures using specially designed instruments will help the child recover faster and return to his normal lifestyle.
Kidney removal
A nephrectomy is an operation in which one of the kidneys is removed.
Do not panic if the doctor recommends removal of the kidney: the postoperative period in most cases proceeds without complications. Life with one kidney can be quite fulfilling, with minor limitations. Nephrectomy is indicated for:
some developmental anomalies,
polycystic kidney disease and other diseases, when the kidney no longer performs its functions and causes infections and complications.
The operation to remove the kidney is performed in a urology hospital. After a nephrectomy, the patient remains in the hospital for 1-3 weeks. The duration of the recovery period depends on the previous condition and the type of access: open or laparoscopic.
After surgery, kidney removal, the consequences depend on the patient’s concomitant diseases, the experience of the specialists and preoperative preparation. In the postoperative period, nonspecific complications mainly occur due to general anesthesia and prolonged immobility.
These include:
pulmonary embolism,
The listed complications are observed quite rarely. To prevent them, proper preoperative preparation of the patient and early activation after surgery are important.
Early postoperative period
1. Physical activity
Immediately after the intervention, the patient should lie on his back and not make sudden movements to avoid complications in the form of sutures slipping off the renal pedicle. By the end of the first day, with the help of medical staff, you can carefully turn onto your side. If there are no complications, you can sit up in bed on the 2-3rd day, and get up on the 4th day. During the early postoperative period, it is necessary to activate the operated patient within reasonable limits:
turns to the side.
2. Nutrition after nephrectomy
A few hours after the operation, the patient is allowed to drink some water or rinse his mouth. You can eat food the next day. Sometimes the postoperative period after kidney removal is complicated by intestinal paresis. Sluggish peristalsis may be due to irritation of the peritoneum during surgery and is manifested by bloating, delayed passage of gas and stool. In these cases, a gas tube is used, an enema is given, and drugs are prescribed that enhance intestinal motility.
Rehabilitation after nephrectomy
For people who have had a kidney removed, rehabilitation can take about 1-1.5 years. During this period, the remaining kidney begins to perform more work and can fully compensate for the absence of the second kidney. During the adaptation process, the kidney increases in size (hypertrophies), so for a year, those operated on are bothered by a mild dull pain in the area of the remaining kidney. This symptom is not dangerous and disappears on its own over time. After discharge from the hospital, excessive physical activity should be avoided.
walking in the morning and evening,
hardening water procedures (wiping with a wet towel, then shower).
It is known that the skin, along with the kidneys, performs an excretory function, so it is necessary to ensure its cleanliness.
Nutrition in the absence of one kidney involves taking easily digestible food. The diet should be sufficiently high in calories. Protein intake should be limited.
The basis of nutrition is:
dishes from vegetables and fruits,
fermented milk products (in small quantities),
lean meat and fish (200-300 g per week).
All dishes are steamed, boiled or stewed. Fried, smoked and canned foods are excluded.
You should not sharply limit the amount of liquid and salt, as this can only cause harm. You can drink clean water without gas, fruit juices diluted with water, weak tea, lingonberry and cranberry juice. The exact diet can be drawn up by your doctor or nutritionist.
Rehabilitation after kidney removal includes measures to preserve the second kidney in a healthy state. To do this you need:
avoid various infections (genitourinary, food, respiratory);
timely treat chronic and acute inflammatory diseases (tonsillitis, otitis, caries, sinusitis, sore throat, etc.);
regularly visit a urologist to assess the functional state of the second kidney.
Important: if you get sick, do not self-medicate, but consult a doctor. Untreated infectious diseases can cause pyelonephritis or glomerulonephritis of the second kidney and lead to loss of its function.
Life after kidney removal is not much different from the life of other people. With adequate physical activity, good nutrition and proper work and rest schedule, the life expectancy of people with one kidney is almost the same as that of healthy people. Many young women with one kidney can give birth to a child, although this issue is decided individually in each case.
after kidney removal
In the absence of complications and good adaptation of the body, working capacity is restored 1.5-2 months after nephrectomy.
Advice: if your profession involves heavy physical labor or constant intoxication, then you should change your place of work. Don't forget about additional good rest.
Many people are concerned about the question of whether kidney removal will result in disability after surgery. Nephrectomy in itself is not grounds for recognizing a person as disabled. The issue of ability to work is decided by a medical and social commission. The decision depends on the compensatory capabilities of the remaining kidney and concomitant diseases.
For some kidney diseases, characterized by a long and severe course and the development of dangerous complications, surgical treatment remains the only option to preserve the patient’s health, and often life. Nephrectomy is performed if there is significant damage to the kidney tissue or a tumor is detected. Patients should not panic, since the intervention itself, the postoperative period and the recovery process do not cause complications. With one kidney, people are able to live a full life with only minor limitations.
Video: Contact lithotripsy of a ureteral calculus of a single kidney
Decreased glomerular filtration rate (GFR).
Glomerular filtration rate (GFR) measures how efficiently your kidneys remove waste from your blood. People with a solitary kidney have a decreased glomerular filtration rate.
In the nephron, tiny blood vessels intertwine with urine-collecting tubes. Each kidney contains approximately 1 million nephrons.
You can have high blood pressure, proteinuria, and decreased GFR and still feel fine. As long as these conditions are under control, they probably do not threaten your health or life. Visit your doctor regularly to monitor these changes.
How can you protect your kidneys?
Doctor's supervision
Your doctor monitors your kidney function by measuring your blood pressure and ordering blood and urine tests once a year.
Normal blood pressure is 120/80 mmHg. or lower. You have high blood pressure if, when measured, it is above 140/90 mmHg. Patients with kidney disease or a solitary kidney should keep their blood pressure below 130/80 mmHg. Controlling your blood pressure is very important because high blood pressure can damage your kidneys.
To detect protein in your urine, your doctor may use a strip of special paper that is placed in a small cup of your urine. The color of the test strip indicates the presence or absence of protein in the urine. A more sensitive test for protein in the urine (proteinuria) is done in a laboratory and the protein to creatinine ratio is calculated. A high protein to creatinine ratio in the urine (above 30 milligrams of albumin per gram of creatinine) indicates that protein is being lost that should remain in the blood.
Previously, measuring GFR required contrast material to be injected into the bloodstream, followed by a 24-hour urine collection (24-hour urinalysis) to measure how much contrast material the kidneys filtered during that time. Currently, GFR is measured in another way, which is based on calculating the amount of creatinine in a small amount of blood. The new method of calculating GFR uses a special formula that takes into account the patient's creatinine level, weight, age, sex and race. Some laboratories calculate GFR at the same time as testing blood creatinine levels. If your glomerular filtration rate is below 60, you have chronic kidney disease.
Blood pressure control
If your blood pressure is higher than normal, you should work with your doctor to find treatment to keep your blood pressure no higher than 130/80 mmHg. For patients with a single kidney, it is necessary to carefully select medications that lower blood pressure. Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers are two classes of blood pressure-lowering medications that protect the kidney and reduce proteinuria. However, with renal artery stenosis, that is, with a narrowing of the artery supplying the kidney, these medications are contraindicated. Diuretics can also lower blood pressure by reducing blood volume. Treatment of high blood pressure may require a combination of two or more medications, in addition to changes in diet and lifestyle.
Kidney removal surgery
Nephrectomy is a method of radical kidney removal used for certain medical reasons. During the operation, not only the organ itself is subject to excision, but also the adrenal gland, surrounding adipose tissue, and regional lymph nodes. Such interventions are carried out in order to save the patient's life and are performed in various ways. In ICD-10, nephrectomy is located in the “Convalescent Status” section and is coded Z54.
Reasons for appointment and essence of the procedure
Doctors identify a number of reasons leading to the removal of the filtering organ, and if a doctor prescribes the procedure, then it is impossible to avoid it. Indications for nephrectomy are as follows:
- Cancerous tumors affecting one kidney.
- Injuries or wounds to an organ (including gunshot wounds), accompanied by damage to the kidney tissue.
- Urolithiasis with gradual death of structures due to the inflammatory process.
- Polycystic kidney disease, which develops against the background of chronic renal failure.
- Congenital or acquired in childhood anomalies of organ development.
- Hydronephrosis caused by impaired urine outflow. The kidney increases in size, and its tissues gradually atrophy.
Operations are also carried out in cases where a person, becoming a donor, donates his healthy organ in order to save the life of a sick patient.
Ban on holding
Nephrectomy, like any operation, is accompanied by certain risks, and the unpredictability of the development of complications can occur both in an elderly patient and in persons with a history of the following disorders:
- diabetes;
- pathologies of the heart and blood vessels;
- blood diseases, including poor clotting;
- arterial hypertension
- dysfunction of the second kidney;
- the presence of only one filter organ.
What is partial nephrectomy and how is it performed?
Our readers successfully use Intoxic to get rid of parasites.
Seeing how popular this product is, we decided to bring it to your attention. Read more here... Partial removal of organ tissue is called resection. It is performed on the kidneys for a number of diseases. Doctors may not offer this treatment method due to contraindications. The risk of complications leads to the need for preparatory procedures and observation after the intervention. In modern surgery, kidney resection is performed using two methods: abdominal and laparoscopic. The rehabilitation course includes restoring the functioning of the operated organ. Kidney resection is practiced when the organ is incompletely damaged. Incomplete kidney damage is typical for polycystic disease, tuberculosis, the occurrence of tumors, closed and open wounds. Most often, intervention is carried out according to indications:
- the size of the neoplasm does not exceed 4 centimeters;
- high risk of kidney cancer;
- closed organ wound
- rapid progression of a benign tumor, suspicion of its malignancy;
- bilateral kidney oncology;
- polycystic disease;
- echinococcosis;
- risk of developing chronic renal failure;
- urolithiasis with a stone in the lower expanded cup;
- kidney injury leading to damage to its segment;
- tuberculosis affecting an organ;
- hydronephrosis in segmental form.
Nephrectomy cost
Taking care of the health of its citizens, the state annually allocates a certain amount of funds for operations. Of course, the number of people in need of surgical treatment is much larger, so it is carried out on a first-come, first-served basis, with patients from certain groups first on the list: the socially disadvantaged (pensioners, disabled people), as well as those who need this intervention for health reasons. Quotas are distributed in special institutions after the issuance of a conclusion by the medical commission.
Routine kidney removal is also carried out in non-governmental medical centers. In private clinics, the average cost of surgery is the following:
- from 15,000 rubles for open nephrectomy;
- from 30,000 rub. - for laparoscopy.
According to statistics, poor citizens wait patiently for their turn, while wealthy patients prefer minimally invasive interventions. Open kidney removal operations are performed free of charge in a public hospital.
Life expectancy: forecasts and statistics
There is no clear answer to the question of how long people with one kidney live after removal of the affected organ. The operation is performed due to the presence of a certain disease. If it was possible to completely cure, then the person’s life activity will differ little from the previous one - pre-operative. A proper diet and healthy lifestyle will help reduce the load on the remaining organ, as a result of which it will increase its functionality. In this case, a person can live another 20-30 years.
In some cases, kidney failure may develop over a ten-year period after nephrectomy. In this case, to avoid complications, it is recommended to undergo examination at least once a year.
The mortality rate in patients with cancer after intervention is within 3%. After 5 years, if the carcinoma is removed, survival is observed in more than 30% of patients. Operated organ tuberculosis has a mortality rate of about 25-28% over 10 years.
Stages of development and symptoms
The pathology develops gradually.
The following stages of chronic renal failure are distinguished:
- Latent. At this stage, a person experiences swelling, and its severity depends on how much liquid he has consumed per day. This stage is also characterized by periodic changes in pressure and pain in the lumbar region. The patient also experiences constant fatigue, insomnia, and loss of appetite. These symptoms cannot be called specific, so the diagnosis must be differential. Frequent urination at night indicates kidney failure. Over time, the signs of this stage of pathology development become brighter. At this stage, changes in the kidneys can still be stopped, and the progression of the disease can be stopped.
- Azethomic. It occurs if therapy for the disease at the previous stage was unsuccessful (or did not exist at all). This stage passes more quickly. The patient's blood pressure changes more often, discomfort appears in the heart area, he sharply loses weight, because the person often can no longer eat normally. The patient develops anemia, general weakness, and limbs go numb.
- Intermittent. It is characterized by an intensification of all symptoms.
- Terminal. At this stage of pathology development, changes in the kidneys are irreversible. Therapy for chronic renal failure involves only eliminating symptoms and maintaining the patient’s life through regular hemodialysis. If possible, the patient undergoes surgery to remove the organ and replace it with a donor one. As for the symptoms, the system stops producing urine, all toxins remain in the body. Not only the patient’s body swells, but also his internal organs. A person may experience bleeding from the gums and nose, bruises appear on the skin, and neurological and mental disorders develop. Stabilizing blood pressure is difficult even when using strong drugs.
The last stage is characterized by the fact that a person’s life expectancy is reduced to several months or even hours. In the chronic form of insufficiency, the patient receives disability (the group depends on the stage of the disease).
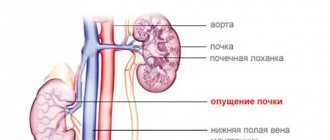
Hydronephrosis of the kidney is a condition in which the kidney is stretched under the influence of urine, as a result of difficulty in its outflow. Normally, urine flows out at low pressure, but if the outflow is obstructed, the urine returns to the collecting ducts of the kidney and the renal pelvis.
Symptoms of hydronephrosis depend on the duration of the urinary tract blockage
The symptoms of hydronephrosis depend on the duration of the urinary tract blockage. If the blockage occurs quickly, then the patient suffers from paroxysmal pain in the right side, if the patient has hydronephrosis of the right kidney, or in the left side, if the patient has hydronephrosis of the left kidney. If the blockage occurs slowly, the patient may not be bothered by any symptoms or may experience aching pain and discomfort in the side on the affected side.
The calyces and pelvis of the kidneys are surrounded by capillaries and nerve fibers, parenchyma. It contains nephrons, whose function is to filter the blood and cleanse it of metabolic products. Due to disruption of normal urinary outflow, the parenchyma becomes inflamed, atrophy occurs and kidney function deteriorates.
The final fluid, that is, urine, must pass freely through the kidneys to the urethra. When physical obstacles arise in its path, fluid gradually accumulates in the kidneys, their collecting system expands, and hydronephrosis develops.
If left untreated, nephrons die and kidney failure develops. As a result of hydronephrotic transformation of the kidneys, the entire body is poisoned with its own metabolic products.
Unilateral hydronephrosis is more often diagnosed. In 35-40% of cases, the right kidney is affected. A bilateral process occurs in 5% of cases.
The main provoking factor of hydronephrosis is a reduction in the outflow of urine due to a decrease in passage in any part of the urinary tract. It can be caused by various pathological and physiological conditions. All factors for the development of hydronephrosis can be congenital or acquired.
- violations of the structure of the ureters (kink, incorrect localization);
- narrowing of the urethra;
- anomaly in the structure of the renal vascular system.
- urolithiasis - the formation of stones can cause blockage of the urinary tract and inhibition of the outflow of urine;
- tumor formations and kidney cysts;
- BPH;
- inflammation of the urinary system;
- pregnancy - the growing uterus puts pressure on the ureter, disrupting the flow of urine.
- 1st degree - urine accumulates in the renal pelvis in an insignificant volume, their walls expand slightly, kidney function is normal.
- a feeling of incomplete emptying of the bladder after urination.
- the painful syndrome is localized mainly on the side of the affected organ;
- arterial hypertension;
- increased flatulence;
- swelling;
- sudden increases in pressure;
- a significant decrease in urine output;
- vomiting and nausea.
- general blood and urine analysis;
- antibiotics;
- blood pressure lowering agents;
- NSAIDs and others.
- Bougienage is the introduction of bougies into the ureter, with the help of which it expands. The operation is performed using an endoscope.
- Balloon dilatation - a special labeled balloon is inserted into the ureter. The narrowed area is expanded by applying pressure.
- fresh fruits and vegetables;
How to take Furosemide and why is the drug prescribed? Read the answer at this address.
At the early stage of hydronephrosis, its symptoms are determined by causative factors. For example, with urolithiasis, renal colic may develop.
Localization of the pathology in the left or right kidney has its own characteristics.
Usually occurs as a complication of urolithiasis. Renal pressure increases. The first signs of a left-sided destructive process are acute pain in the side of the abdomen, radiating to the left leg. The outflow of urine is impaired and diuresis decreases. The color of urine may be cloudy with a pink tint (if the urinary tract mucosa is injured by a calculus). Back pain appears, radiating to the shoulder blades and groin.
The goal in the treatment of kidney hydronephrosis is to remove the cause of the pathology, reduce the load on the kidneys by removing accumulated urine, and prevent irreversible deformation of the organ. The doctor can offer a solution to the problem in several ways: medication or surgery.
The role and possibilities of conservative treatment for hydronephrosis are very limited. In most cases, the use of medications is indicated before surgery. Taking medications is aimed at eliminating the symptoms of hydronephrosis (sanitizing foci of infection, stimulating urination, suppressing pain).
If the dynamics of the kidney changes for the worse, then surgery is necessary. The goal of such therapy is to eliminate mechanical obstacles to urine excretion, which have become a factor in the development of hydronephrosis. During the intervention, an additional path for urine excretion can be created or the calyces and pelvis of the kidneys may be narrowed.
View a selection of effective and safe methods for treating gestational pyelonephritis during pregnancy.
Memo to people with one kidney: how to live longer
In the recent past, removing a kidney was considered a death sentence for the patient. Today there is an opportunity to live a full life, engage in normal activities and even have offspring. To feel normal, you just need to lead a healthy lifestyle and remember the recommendations of your doctor, which include:
- special therapeutic nutrition;
- rational daily routine;
- daily walks;
- stay in the fresh air for a sufficient period of time;
- compliance with hygienic standards of the genitourinary system;
- strengthening the body's defenses and increasing immunity;
- prevention of hypothermia, colds, chronicity of existing diseases;
- Regular visits to doctors for preventive examinations.
You should also change the type of main work activity if it is associated with increased stress or harmful toxic substances.
Indications for kidney removal surgery
Indications for nephrectomy (removal of the left or right kidney) include a group of pathological manifestations affecting the organ:
- tumors of a malignant nature, if one kidney is not affected or functions partially;
- traumatic damage to the kidney, in which the organ stops working normally and it is impossible to restore its functions;
- kidney stones, which provoked suppuration of the kidney tissues and their death;
- polycystic kidney disease, developing against the background of renal failure (nephrectomy is used if drug therapy does not help);
- pathologies of kidney development in childhood;
- problems with urine excretion from the kidney (hydronephrosis), which provoke tissue atrophy.
Return to contents
Polycystic kidney disease in children
The disease is diagnosed by ultrasound, CT, excretory urography, scintigraphy and renal angiography.
Occurs with variable frequency: 1:250-1200 newborns. But due to the latent nature of the disease in childhood, such a diagnosis is made much less frequently. Polycystic disease can manifest itself (depending on the degree of kidney damage and clinical form) both in infancy and in adolescence and adulthood (30-40 years).
PKD (polycystic kidney disease) is the subject of study by urologists and geneticists, as it is one of the hereditary diseases.
As a result, the renal cortex becomes covered with large cysts, which leads to a significant increase in kidney size. Also, one of the factors that accelerates the process of cyst formation is increased proliferation (proliferation of organ tissue due to accelerated cellular growth) and impaired differentiation of one of the epithelial (filtering) layers of nephrons. This is what causes cysts to replace healthy kidney tubules. As a result, neighboring nephrons are severely compressed, and the overall performance of the kidney sharply decreases, leading to significant renal failure in the patient.
With the development of the pathological process at a later age (in early childhood and childhood), a significant decrease in the number of cysts and their size is observed. The liver is very often involved in the cyst formation process, and when studying its structure, an increase in the lumen of the intrahepatic bile ducts, as well as general periportal fibrosis, is determined.
The course of PPD largely depends on the age of the child at which the first symptoms of the disease were detected. According to this characteristic, 4 groups (clinical forms) are distinguished: from perinatal (in newborns) to juvenile (puberty of a teenager). Its symptoms and further prognosis depend on the group of the disease.
Thus, with the perinatal and neonatal forms of the disease, up to 90% of the kidney tissues are replaced by cysts, which inevitably leads to significant growth of the kidneys and, as a consequence, an increase in the entire abdomen. Children experience severe and rapidly increasing renal failure (RF). However, a common cause of death is not PN, but pneumothorax and pulmonary hypoplasia with resulting distress syndrome.
If the disease develops later (during the period from early childhood to juvenile age), then the number of detected cysts will be much smaller, but signs of liver changes will become more frequent. The result of a clinical examination may be the detection of some enlargement of the liver and kidneys, and sometimes hepatosplenomegaly (when the spleen also enlarges along with the liver).
Symptoms that especially clearly characterize polycystic kidney disease in children are:
- sustained increase in blood pressure;
- urinary tract infection.
There is a gradual increase in renal failure with the manifestation of impaired depuration function of the kidneys (consists in their ability to excrete urea).
It is possible to develop anemia with osteodystrophy and, as a result, a noticeable slowdown in the child’s growth. At the same time, signs of liver fibrosis may be detected, complicated by bleeding in the gastrointestinal tract and frequent manifestations of increased pressure in the portal vein. If PBP develops in children in early childhood (3-5 years), the disease progresses much milder than in newborns, and the prognosis is much better.
Death in newborns with this disease can occur after 2-15 years from the onset of cyst formation. This is if you do not undertake radical treatment methods.
Scientific research in this area has shown that patients undergoing active systematic treatment and surviving the first 6 years of life have a good chance of living more than 15 years. The main cause of death in childhood polycystic disease remains renal failure and its complications.
To date, no way has been found to stop the process of cyst formation. Therefore, all treatment and therapy methods are lifelong and are aimed mainly at preventing complications of renal failure and maintaining kidney functionality. Patients are forced to maintain a constant dietary and drinking regime, as well as undergo repeated courses of drug therapy.
If the course of the disease is accompanied by an inflammatory process in the kidneys in newborns (and not only), a course of treatment of pyelonephritis with antibiotics and uroseptics is prescribed. For arterial hypertension, antihypertensive drugs are used. In case of exacerbation of PN against the background of polycystic kidney disease, hemodialysis is performed, and the need for kidney transplantation is also considered (in some cases, together with the liver).
You can also counteract the rapid increase in volume of cysts with the help of surgical intervention. To do this, percutaneous puncture aspiration of cysts is performed (with monitoring of the process on ultrasound), as well as laparoscopic excision.
Preparing for a nephrectomy
Before performing a nephrectomy, you need to do a thorough examination of the patient. The doctor must find out why the organ stopped working, that is, identify the reasons for removing the kidney, and find out everything about the condition of both kidneys. In addition, the importance of the examination is due to the fact that the operation is performed under general anesthesia, which poses some danger for a patient in serious condition.
Diagnostics
Diagnostic measures include:
- Assessing the patient's respiratory function - nothing should interfere with the functioning of the lungs, since respiratory depression occurs during general anesthesia.
- X-ray examination of the organs of the genitourinary system - the condition and possible additional damage to the organs are determined.
- Taking a blood test for creatinine - indicates kidney failure if the indicator is elevated.
- Computer (CT) and magnetic resonance imaging (MRI) of the affected kidney.
- Ultrasound, CT or MRI of the peritoneal vessels reveals the presence of venous thrombosis.
If clarification of information about the patient’s condition is required, additional urine and blood tests are taken to identify infections, and fluorography is performed. Before the kidney is removed, the patient must spend about 3 weeks in the urology department. During this period, the entire diagnostic range of studies and careful monitoring of the patient are carried out.
Preoperative preparation
The day before surgery, final preparations are carried out. The patient is given an enema to cleanse the intestines and the hair is shaved in the place where further manipulations by the surgeon are expected. It is forbidden to eat for the whole day before the nephrectomy. You should drink a minimum amount of water, and if possible, avoid liquids altogether.
Abdominal surgery (open)
How do they do it?
Patients are placed on the operating table and secured with elastic bandages so that they do not make involuntary movements. Next, they are put under anesthesia, and the operation to remove the kidney begins. There are several options for making the incision: in the front in the area of the lower border of the ribs or on the side between the 10th and 11th ribs. The second technique of nephrectomy is considered less traumatic, since the doctor has direct access to the kidney.
The operation to remove a kidney using the open method lasts about three hours.
After making the incision, it is necessary to install a dilator and fix the pancreas and duodenum so that when working with the kidney they do not harm them and prevent displacement. The connective and fatty membranes are separated from the kidney to be removed. If there are blood vessels in the tissues, they are blocked with clamps. The veins approaching the kidney are sealed, disrupting the original structure of the kidney protein.
The ureter is compressed on both sides. An incision is made between the installed clamps. Next, the organ is sutured with absorbable threads. If cancer has metastasized from the kidney to the ureter, it is removed along its entire length. Before removing the kidney, the surgeon sutures the renal pedicle. Through it, arteries, veins and the ureter enter the kidney. To prevent the development of bleeding, the vessels are sutured. The separated kidney is removed from the peritoneum.
Possible problems
The most common complications after abdominal surgery are:
- Bleeding caused by an undetected blood vessel or insufficient occlusion of large veins or arteries.
- Intestinal obstruction.
- Heart failure caused by patient predisposition or taking the wrong dose of anesthetics.
- Thrombosis of large vessels.
- Problems with the blood supply to the brain, usually caused by bleeding or a blood clot.
- Respiratory failure caused by anesthesia. If breathing problems go away over time, the patient’s life and health are not in danger.
Anatomy of the kidney in newborns
In the lumbar region, the kidney is separated from the skin by a layer of soft tissue, sometimes not exceeding 5 mm, so lumbotomy should be performed strictly layer by layer and with great care.
The renal hilum, which is a slit measuring 6-10×4-8 mm, can be deployed ventrally or dorsally.
The adrenal gland of a newborn sometimes corresponds in size to ½ of the kidney and can cover its surface from the upper pole to ⅓ and even ⅔, sometimes overlapping the vessels of the renal pedicle or even reaching the lower edge of the kidney (see figure).
Various relationships between the kidney and adrenal gland in newborns: a - the adrenal gland covers the upper pole of the kidney and blood vessels; b - the adrenal gland covers only the upper pole.
The left kidney is separated from the tail of the pancreas by the edge of the left adrenal gland. Sometimes the kidney can come into contact with the spleen, being separated from it only by the peritoneum and tissue. The latter circumstance must be taken into account in cases of difficult kidney release. Only careful preparation can avoid injury to the spleen or tail of the pancreas.
The renal pelvis in newborns is located predominantly intrarenally and reaches almost half the height of the newborn’s body in length. The pre- and retro-ureteric fascia are delicate and thin, so the organs are easily displaced and protruded to great depths.
One should remember about the frequent scattered division of the renal artery at the hilum of the kidney, as well as the possibility of additional (parallel to the aorta) vessels, which occur in ⅓ of cases. The vessels to the poles of the kidney can arise both from the renal artery itself and from the adrenal and phrenic arteries (see figure).
Not only the adrenal vessels, but sometimes also the testicular artery can depart from the trunk of the renal artery, so ligation of the main trunk of the left renal artery near the aorta during nephrectomy can lead to disruption of the blood supply to the adrenal gland or left testicle. This implies the need for careful, sequential suturing and ligation of vascular trunks in the immediate vicinity of the gates and poles of each kidney.
In cases where the renal hilum is directed posteriorly, the renal vessels are intimately connected to the posterior abdominal wall. Accessory arteries often cross the ureter or pelvis, having an ascending or descending direction. The renal vein can vary in length and number of veins, usually entering it intrarenally. Accessory renal veins, as a rule, correspond to accessory arteries and are located next to them.
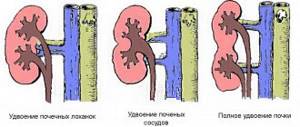
When assessing the vessels in the area of the renal pedicle during nephrectomy, it is necessary to keep in mind that with one of the most common kidney anomalies in children - duplication - an atypically located vessel may not go to the adrenal gland, but to the doubled part of the kidney located above.
Laparoscopic surgery
Progress of the operation
The patient lies on his back. A bean-shaped cushion is placed under the legs to make it easier for doctors to turn the patient over. The body of the person being operated on is fixed with elastic bandages. As in the previous case, laparoscopic nephrectomy is performed under general anesthesia. A surgical instrument called a trocar is inserted near the navel. It is represented by a tube with a stylet at the end, which is used to pierce tissue. A camera is attached to it, with the help of which the surgeon can control the insertion of the remaining trocars, providing access to the organ from all sides. After all the necessary preparations have been made, the patient is turned on his side, deflating the pillow under his feet. The body is fixed again.
The vessels approaching the kidney and the ureter are clamped with staples of a laparoscopic stapler. They cannot be sutured until the kidney is removed from the body. The damaged organ is removed with the largest trocar, measuring 11 millimeters, after the patient is turned onto his back again. The edges of a plastic bag and a laparoscope are placed in the middle of the instrument, which is used to directly trunce the organ. Next, the trocars are removed from the patient’s peritoneum. The wound and damaged tissues are sutured with self-absorbing thread. The excised kidney is examined histologically.
Possible problems
Laparoscopic nephrectomy is considered a gentle method of kidney removal, so the risk of complications after it does not exceed 16%. The most common problems:
- A hematoma that develops during surgery is a collection of blood of limited size, which will resolve on its own after some time.
- Obstruction of the gastrointestinal tract. Problems with intestinal motility occur due to drugs that relax the muscles or accidental squeezing of the intestine during a nephrectomy.
- Postoperative hernia at the site where the trocar enters most often occurs in overweight people who have had their kidneys removed urgently.
- The development of an inflammatory process in the lungs, unrelated to an infectious infection, is the reaction of the immune system to a surgical procedure.
- Blockage of the pulmonary artery by a blood clot or gas. Occurs if an artery is damaged during surgery.
- Paralysis of the brachial nerve if it was touched by the surgeon. Given the severity of the lesion, the patient may feel a tingling sensation in the arm, and in some cases, be unable to move it.
Return to contents
Caring for the patient after surgery
After surgery, patients experience severe discomfort in the incision area. Also, patients who have undergone nephrectomy complain of impaired sensitivity due to dissection of the nerves in the area of the surgical wound.
During the postoperative period, patients are advised to take strong painkillers, and, if necessary, throughout the recovery period. To prevent the formation of pneumonia, it is necessary to organize breathing exercises, despite the fact that they can cause pain due to the proximity of the surgical incision to the diaphragm.
Possible complications of surgery may be the following: infection, postoperative pneumonia, excessive bleeding. There is also a risk of kidney failure in people with poor functioning or damage to the remaining kidney.
Kidney malformations requiring nephrectomy: a - giant hydronephrosis (photograph during surgery); b — multicystic (photo of the specimen)
Much less often, a kidney has to be removed if it ruptures as a result of a birth injury.
Postoperative complications and consequences
The consequences of kidney removal directly depend on the quality of preparation for surgery, the actions of the surgeon during nephrectomy, how successful the operation was, and the presence of additional diseases in the patient. Removal of an organ is associated with the risk of developing nonspecific complications. Most often, such problems are caused by anesthesia and the fact that the patient lay motionless for a long time (kidney removal lasts 2-4 hours). These include:
- congestive pneumonia - secondary inflammation of the lungs, provoked by problems with ventilation or hemodynamic disorders;
- stroke - a violation of blood circulation in the brain;
- infarction - ischemic necrosis of a portion of the myocardium;
- thrombophlebitis - thrombosis that develops against the background of inflammation of the vein wall.
If a person’s fever does not go away for a long time after surgery, this indicates the presence of an inflammatory process. The consequences of nephrectomy are usually associated with the development of renal failure. The cause of the pathology may be compression of the contralateral vein if the patient had a thrombus consisting of pathological cells in the kidney with a tumor. Since the patient has only one working organ left, he needs to take on the entire load. After some time, normal functioning is restored, but sometimes it is necessary to carry out extrarenal blood purification.
Early postoperative period
Immediately after surgery to remove a kidney, the person undergoing surgery is placed in the intensive care unit for constant monitoring of the condition. For the first and next few days, the operated patient has a catheter to remove urine. The patient is allowed to drink and eat not immediately, but only after the doctor confirms the presence of intestinal motility. Water is consumed in small quantities, and food is ground.
Among the unpleasant symptoms, pain occurs after removal when taking a deep breath or coughing. It also hurts when moving the body. Despite this, breathing exercises are recommended to speed up recovery and prevent pneumonia. Under the supervision of a doctor, the patient needs to gradually increase physical activity. From the 2-3rd day it is allowed to roll over to one side and stand up. There is no need to make sudden movements so that the seams do not come apart. Physical activity prevents problems with the intestines and blood circulation from developing.
Rehabilitation upon returning home
The main rehabilitation after kidney removal begins at home, since the patient is now responsible for his own condition. People with a removed kidney need at least 1.5 years to recover after surgery. Over time, the kidney gets used to the stress and works on a compensatory principle. It is more difficult for older people to recover.
Nutrition rules
The rehabilitation period for people who now live with one kidney begins with a change in diet. The main condition for selecting dishes is the easy digestibility of the food consumed. The diet includes foods with moderate calorie content and low protein concentration. The daily menu must include:
- bread based on rye flour;
- vegetable and fruit salads;
- cereal porridges and pasta;
- dairy products.
Meat is included in the diet with caution. You can eat no more than 100 g of boiled veal, chicken or rabbit per day. It is allowed to eat low-fat fish and chicken eggs in the form of an omelet. It is forbidden to consume milk in large quantities because of the calcium it contains, which provokes stone formation. It is not recommended to eat legumes, as they increase gas formation in the intestines.
The diet is divided into 5-6 small meals. The amount of water per day is agreed upon with the attending physician, taking into account the consumption of liquid from soups, diluted juices, vegetables and fruits. All dishes are steamed, boiled or baked. The dose of salt per day is 5 g, and bread - no more than 400 g. The diet developed by the doctor must be adhered to in full.
Physical activity
A physically active life with one kidney means little stress on the body for the first 2-3 months. Those undergoing surgery are required to walk for about half an hour in the mornings and evenings. Over time, you can walk up to 3 hours every day. Heavy lifting is excluded. You are allowed to lift no more than 3 kilograms. The back is fixed with a special bandage. Once a week, the kidneys are unloaded - bath procedures are performed.
Prevention of complications and lifestyle precautions
Restoring a normal lifestyle in the postoperative period is associated with maintaining the health of the remaining one kidney. Necessary:
- prevent the development of infection;
- if inflammation occurs in any organ, do not hesitate to start treatment;
- Have your kidney examined regularly.
Life after kidney removal is closely related to being attentive to your own health. Those who have undergone nephrectomy should not overexert themselves and allow the body to become hypothermic. If you have any suspicions or symptoms of the disease, you should immediately consult a doctor. If before the operation the patient’s work was associated with harmful or toxic production or severe physical activity, the field of activity should be changed.
Rehabilitation and disability
If the patient has no complications after nephrectomy and the body quickly adapts to the new lifestyle, working capacity is fully restored in 1.5-2 months. Sick leave will be required for this period. But the question often arises whether a person with one kidney becomes disabled. Nephrectomy is not considered as a basis for assigning disability. Disability after kidney removal is determined by the only authority - the medical and social commission. The commission members are authorized to find out how much the remaining kidney is able to compensate for the absence of the second and take into account the presence of concomitant diseases to make a decision.
Etiological factors of renal agenesis
The pathological formation of an organ during the development of the fetus in the womb, when the baby has only a single kidney, is called renal agenesis. At the same time, other renal structures may remain unformed. Most often this concerns the ureter, which may be completely absent. In newborn girls, along with this defect, pathology of the genital organs is often observed.
Modern studies have not been able to prove that agenesis is a genetic pathology that is inherited. If a child is born with one kidney, this indicates damage to the development of organs in the early stages of pregnancy. Statistics show that mothers with diabetes are much more likely to have a child with a solitary kidney.
But still, teratogenic factors play a predominant role. A pregnant woman is very vulnerable to external factors. The same applies to the embryo.
The following etiological factors may have a decisive influence:
- severe viral illnesses during pregnancy;
- intense influence of toxic materials on the embryo;
- active influence of radiation;
- abuse of bad habits (alcohol, smoking, drugs) during pregnancy;
- infection of the genitourinary system;
- taking medications in large doses often leads to abnormal development of the fetus.
Even a severe form of influenza in the mother can have consequences on the development of fetal organs. As for sexually transmitted diseases, syphilis has the most negative impact. Hormonal contraceptives can have a great influence on the structure of fetal development.
The most dangerous period for the occurrence of anomalies is the first and second months of pregnancy. The shorter the period, the stronger the pathogenic effect on the unborn baby. If, for example, already in the first month the embryo has experienced a detrimental effect, then upon examination agenesis will likely be detected. Therefore, it is extremely important to undergo ultrasound and examinations by a specialist on time.
Statistics say that boys with one kidney are born more often than the opposite sex. The absence of the right kidney is most often observed in medicine. Its size is usually smaller than the left one, and it is more prone to complications.
The left kidney usually performs the work of the missing organ quite efficiently, and the child can live for a long time without experiencing discomfort. But agenesis of the left kidney is much more difficult for the body. One right organ does not carry the load for two. True, this pathology is much less common.