Indications for the procedure
If it is impossible to restore the functional activity of the ureter using medications, plastic surgery is prescribed. The main indications for their implementation are:
- hydronephrosis;
- hydroureteronephrosis against the background of the development of strictures (organic narrowing of the ureter);
- previous damage to the urinary duct as a result of injuries and gynecological operations in women;
- postpartum and pathological obstructions (disorders that prevent the normal outflow of urine).
At the same time, such procedures are not prescribed for the following indications:
- serious disturbances in the activity of the cardiovascular system;
- acute infectious diseases;
- chronic pathologies accompanied by inflammatory processes in the ureter;
- problems with blood clotting;
- diabetes;
- period of bearing a child.
To determine the presence of contraindications, immediately before surgery, the patient must undergo a diagnostic examination, which allows identifying such violations.
Hydronephrosis of the kidney
This is a condition that occurs when the ureter is obstructed at its junction with the pelvis. In this case, the outflow of urine is disrupted, which leads to expansion of the collecting system.
It begins to compress the parenchyma, the blood vessels and nerve endings located in it. If this process is not stopped, then atrophy and necrosis of the renal tissue gradually develops.
Hydronephrosis
In clinical practice, there are two types of this disease. Congenital hydronephrosis is caused by hypoplasia or aplasia of the ureteropelvic orifice, embryonic adhesions and kinks of the ureter.
Acquired develops with urolithiasis, oncological processes in the pelvis or ureter, traumatic damage to the urinary tract.
During endoscopic or open operations on the kidney or ureter without plastic surgery, there is a high risk of scar formation, which also leads to a narrowing of the lumen of the urinary canal.
At the very beginning of the disease, the pelvis, to some extent, can compensate for the growing intrarenal pressure. However, the process of urine formation occurs continuously, so the pressure inside the organ continues to increase.
In severe cases, the parenchyma and the nephrons located in it are completely replaced by connective tissue. This condition is a direct indication for kidney removal.
The danger of this pathological process may lie in the fact that it can be asymptomatic for a long time. Occasionally, intermittent pain may occur in the lumbar region.
Symptoms
It is often attributed to radiculitis or lumbar osteochondrosis. This picture is especially characteristic of congenital anomalies of the ureter, its compression by a tumor or narrowing of the lumen due to scar formation.
If hydronephrosis occurs against the background of urolithiasis, then renal colic may develop.
The cause of the pain syndrome is a gradual increase in intrarenal pressure and impaired blood circulation in the parenchyma.
Temperature increase
Very often this condition is complicated by the addition of a bacterial infection. In such cases, a strong increase in temperature is observed.
Bilateral hydronephrosis may be accompanied by chronic renal failure. Violation of the filtration function of the kidneys negatively affects the functioning of all organs and systems of the body.
With the development of chronic renal failure, an increase in blood pressure, general weakness, decreased performance, swelling in the face and ankles, shortness of breath, arrhythmia, and digestive disorders are observed.
How does ureteroplasty differ from other operations?
In addition to ureteroplasty, other operations are used that also solve problems of the functionality of the urinary system, but differ in technical terms.
One type of such intervention is bougienage , which is used for pathological narrowing of the urethra. This disorder can occur against the background of autoimmune reactions, the activity of pathogenic microorganisms and due to hypothermia.
Bougie is the physical expansion of the urethra using a bougie - a special catheter with a thickening of different shapes at the end.
This procedure can be performed not only to expand the canal, but also as a diagnostic procedure, during which a specialist can identify the degree of fusion of the walls of the urinary canal and determine the presence of various formations and scars on its walls.
Another type of surgical intervention is reimplantation , which is done for a pathology called “megaureter”.
This disease, unlike fusion, is a congenital dilatation of the ureter, as a result of which patients experience urinary incontinence and problems with the regularity and nature of urination in general.
During this operation, a resection of the ureter is performed in a certain area from the bladder (for this, an area located above the narrowed area is selected).
Next, an anastomosis - a new connection in which there are no obstacles to urine output and at the same time, the width of the channel prevents reflux (reflux of urine back into the kidney).
During the operation, a special catheter is inserted into the patient's ureter, in the presence of which the anastomoses are not irritated and healing takes place over the next two weeks, while urine does not leak through the sutures during emptying of the bladder.
Read our article on how to do bladder catheterization.
an endoscopic type of operation : no incisions are required in the abdominal cavity, and the entire procedure is carried out by accessing and inserting special surgical instruments through punctures.
Diagnostics
Basic methods for diagnosing ureteral cancer:
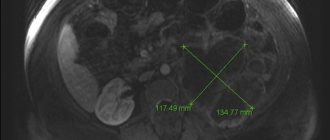
- computed tomography or magnetic resonance imaging - detects even small tumors;
- Ultrasound of the retroperitoneal organs - may reveal some larger tumors;
- Ureteroscopy is an endoscopic examination used to confirm the diagnosis.
The most accurate method is ureteroscopy. This is an endoscopic examination. The doctor inserts a thin tube into the urethra, from there into the bladder, and then into the ureter. If a tumor is detected, the doctor takes a piece of tissue for histological examination. The laboratory determines the degree of malignancy of the tumor, which is important for choosing treatment tactics.
Our doctors will help you
Leave your phone number
Types of surgeries on the ureter
Intestinal plastic
There are several types of such operations, one of which is directly plastic.
During the procedure, an isolated section of the small intestine located close to the urinary tract is used, from the tissue of which a new artificial urinary canal is formed. It then connects to the renal collecting system and the bladder.
Such plastic surgery can be partial or complete . In the first case, intestinal tissue is used to replace only a certain section of the ureter, and in the second, the entire canal is replaced after removal of pathological tissue.
During the operation, the patient is given a catheter for external urination, which is maintained during the postoperative period.
The operation is indicated not only for the removal of entire fragments of the ureter, in which irreversible dystrophic processes lead to the impossibility of the organ performing its functions in the future. The procedure allows you to eliminate the formation of adhesions and various formations on the inner and upper surface of the organ.
When performing the operation, endotracheal anesthesia (the narcotic drug is administered through the trachea). During the excision of pathological tissues, the circulatory system is not affected.
Boari method
Another option for plastic surgery is the Boari method , which is used to restore the integrity of the tissues of the ureters by forming new segments from the tissues of the bladder stem.
A plastic catheter in the form of a tube is first inserted into the ureter and fixed to the walls of the canal. Sections of healthy tissue are excised from the walls of the bladder and sewn into the affected areas of the ureter.
Upon completion of the operation, the catheter, which temporarily serves to drain urine during surgery, is removed through the urethra.
Endoplasty
For vesicoureteral reflux, patients are prescribed endoplasty, which is characterized by minimal trauma to the tissue of healthy organs. The operation itself is quick and virtually devoid of pathological complications. The procedure is performed in the following sequence:
- A needle is inserted into the orifice of the ureter, through which a gel is injected through a syringe to dilate the orifice of the ureter.
- The gel is injected under the mucous membrane of the ureter to a depth of seven millimeters.
- The needle is removed.
- Over the next 12 hours, a catheter is maintained in the ureter, in the presence of which a normal channel structure is formed.
Uretero-ureteroanastomosis
In case of damage to the lower part of the ureter, the operation uretero-ureteroanastomosis is used (as the name implies, two parts of the ureter are sutured together according to the “end to end” principle).
Sometimes, if the end of the ureter from the bladder side is too small, an anastomosis is performed directly to the bladder, and this operation is already called urethrocystoanastomy.
Sometimes the ureters are transplanted into the bladder (ureterocystoneostomy) . The operation is performed when there is a violation of the patency of the pelvic ureter. In this case, the end of the ureter is sutured into the apex of the bladder.
Uretero-ureteroanastomosis is performed with preliminary insertion of a Foley catheter into the ureter.
This is a latex instrument that first serves as a support for more comfortable stitching, and in subsequent days or weeks (depending on the length of the rehabilitation period, which can last from a week to a month) it is used to drain urine.
Plastic surgery with a pelvic flap (Calpa de Vnrda operation)
A stay suture is placed on the ureter in the area of its exit from the pelvis. The ureter is crossed in an oblique direction, then longitudinally dissected along the lateral or anterior wall (in the avascular zone) over a length equal to the length of the intended V-shaped flap. A more precise incision can be made after cutting out a flap from the renal pelvis.
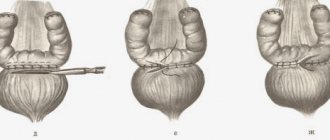
Resection of the pelvis and upper third of the ureter begins with a short incision with a scalpel with a hook-shaped blade No. 11 along one of the previously marked lines. The resection is continued by cutting the pelvis with scissors between the stay sutures. The altered LMS, the pelvic ureter and the altered part of the pelvis are removed (Fig. 4.1).
A vinyl chloride tube of a suitable size is inserted into the ureter to protect its posterior wall from being caught in the suture during anastomosis. A suture is applied with a 4/0-6/0 synthetic absorbable thread, stitching the top of the V-shaped flap from the outside to the inside, then the corner of the ureter incision from the inside to the outside. The second suture is placed at a distance of 0.2 cm from the first. Both seams are tied with 4-5 knots, the ends of the threads are cut off. A stay suture is left on the ureter to facilitate manipulation.
Do not grab tissue with tweezers. With an alternative method, a mattress suture is applied with a thread with a double needle and after tying the suture, the posterior wall of the anastomosis is sutured from the lumen side with one needle, and the anterior wall from the outside with the other. Stitches should be made through the muscular layer and adventitia, trying to capture less mucous membrane in the seam.
A continuous suture of the posterior line of the anastomosis is continued to the apex of the ureter, overlapping at every 4-5th stitch. The anterior line of the anastomosis is sutured in the same way, while blood clots are washed out of the collecting-pelvic system (PSS), which is especially important with an anterior approach.
Figure 4.1. Diagram of the stages of the Andersen-Hines operation
Both threads are tied at the apex of the ureter, one of them is cut off, and the remaining defect of the renal pelvis is sutured with the other. If it is necessary to use a pyeloureterostomy (vinyl chloride tube), then its end is brought out through the renal parenchyma. If necessary, a nephrostomy tube is installed before suturing the renal pelvis.
The wall of the pelvis is pierced with a thin needle and an isotonic sodium chloride solution is injected to check the tightness of the sutures and the patency of the anastomosis. If the thin vinyl chloride tube inserted into the pelvis at the beginning of the operation has not yet been removed, it is connected to a syringe and, raising it 100 mm, is filled with a gravity-fed CLS solution.
A rubber or vinyl chloride drainage is installed and fixed next to the anastomosis so that the tube does not touch the suture line and the ureter below the anastomosis. This can be achieved by fixing with a long suture. As an alternative, a drainage system for active suction can be used. It is important to install the drainage tube correctly.
If the kidney is mobilized, then it is pulled back to its previous position and fixed with sutures; otherwise, the lower pole of the kidney will move anteriorly and compress the ureter. The posterior and anterior edges of Gerota's fascia are sutured, isolating the kidney and the plastic zone from the abdominal wall. The wound is sutured in layers. The drainage tube is brought out from the side so that the patient does not squeeze it while lying down.
A postoperative drainage system is being set up. In the case of non-drainage plastic surgery, drainage of the bladder should be longer in order to reduce urine pressure in the plastic surgery area.
A spiral flap is cut out from the dilated pelvis in an oblique direction, after which the incision is extended down the ureter to a distance equal to the length of the flap. A stay suture is placed on the flap and folded downwards. The posterior edge of the flap is sutured to the lateral edge of the ureter with a running 4/0 or 5/0 synthetic absorbable suture (Fig. 4.3).
Figure 4.3. Diagram of the stages of Operation Calpa de Virda
The anterior edge of the flap and the renal pelvis are sutured in the same way. When modifying Scardino-Prince, not a spiral-shaped, but a vertical flap of the renal pelvis is cut out (Fig. 4.4).
Figure 4.4. Diagram of the stages of the Calpa de Virda operation as modified by Scardino-Prince
Drainage, as in previous operations, is performed by ureteropyelostomy, nephrostomy or stenting of the upper bladder.
Many years of clinical experience show that effective surgery leads to improved kidney function and a decrease in the degree of dilatation of the renal joint in the next 1-1.5 years, with subsequent stabilization of the effect. The high efficiency of resection of the pelvis, the upper third of the ureter according to Andersen-Hines (97.82%) emphasizes its pathogenetic validity.
All operations aimed at expanding the diameter of the sclerotic ureteropelvic segment - operations such as Foley and Calpa de Virda - have a significant drawback: scar tissue remains in the anastomosis.
According to V.A. Grigoryan (1998), reconstructive operations for stenosis of the LMJ and GN lead to improvement in 10.5% of operated patients, to complete restoration of urodynamics within 3-12 months - in 82.3%. The positive results obtained are maintained throughout the entire long-term observation period, excluding isolated cases.
During operations involving the removal of a narrowed LMS, the question almost always arises of which part of the altered pelvis should be resected. Usually they try to remove as much of the dilated pelvis as possible to bring its size back to normal. According to some authors, part of the dilated pelvis must be excised, since the atonic wall leads to the formation of pockets and discoordination of contractile function.
A study by J. Harish (2003) found that during the Andersen-Hines operation it is necessary to increase the area of ureter resection by an average of 0.8 cm due to the predominance of the size of the area with impaired innervation over the area of visible narrowing. At the same time, the problem of expanding resection of the pelvis must be solved purely individually, depending on the functional state of the pyelocalyceal system.
The feasibility of open operations for so-called functional hydronephrosis without removal of the UJJ is questionable. Considering the insufficiently satisfactory results of plastic surgery on the ureteropelvic segment without its excision, a number of authors classify these operations as palliative, giving generally only a short-term effect in only 18-20% of patients. As a rule, patients who have undergone organ-sparing operations without excision of the LMS are re-operated, and nephrectomy is performed in 41% of them.
A comprehensive study of the PUJ and the pelvic ureter casts doubt on the term “functional GN.” With intraoperative electropyeloureteromyography, the patent segment in all cases shows low bioelectrical activity or is completely “silent”.
Histological examination of the patent segment, which is considered characteristic of functional GN, reveals a deficiency of muscle fibers throughout the entire circumference extending to the pelvic ureter (hypoplasia). The intercellular spaces are thickened, muscle cells are separated, the main composition is connective tissue and collagen fibers. Thus, significant morphological changes in the LMS explain the pathogenesis of GN.
The irreversibility of structural changes justifies the expediency of resection of the pelvis and upper third of the ureter with removal of the altered LMS and creation of a morphofunctionally complete ureteropelvic anastomosis.
The practical significance of intraoperative electropyeloureteromyography is emphasized by many researchers. Some authors consider it the only method that determines the zone of akinesia of the ureteropelvic segment with dynamic (functional) obstruction in patients with hydronephrosis, when there are no mechanical obstacles to the outflow of urine. Violation of the urodynamics of the urinary tract is caused by a disorder in the coordinated activity of the pelvis, urinary tract and ureter.
Such physiological studies during surgery encounter certain difficulties, since they require technical support and the participation of specialists in functional diagnostics. According to Yu.A. Pytel (1997), a much more informative method is the indigo carmine test, which consists of filling the pelvis with an indigo carmine solution until a threshold pressure is reached in it and observing the waves of contraction of the pelvis and ureter.
The most important condition is preliminary emptying of the CLS, which allows one to get a true picture of the topographic relationships between the pelvis, ureter and renal vessels. In addition, if the tone of the pelvis is sufficient, then after emptying it decreases significantly and takes on its real shape and size.
According to Yu.G. Alyaeva, V.A. Grigoryan et al. (2008), extended resection of the pelvis is indicated in late stages of GN with pronounced structural and functional changes in the urinary tract. In patients with giant CL, for early and complete restoration of urodynamics, it is advisable to remove the entire afunctional area of the pelvis.
If necessary, it is possible to use an indigo carmine test. It will allow you to determine not only the area of the stricture, but also the afunctional area (usually 0.1-0.3 cm in length), distal to which waves of contraction of the ureter are clearly visible. This zone is optimal for removal, and the intersection of the urinary tract is performed 0.5-0.6 cm distal and proximal to the afunctional area.
Preparation
The main requirement for the patient before operations of this nature is the preliminary elimination of any infectious, colds and inflammatory diseases in the urinary system.
Often, with obstructive disorders, which are an indication for ureteroplasty, the patient develops pyelonephritis, and before surgery it is necessary to first cure the disease.
Approximately two weeks before plastic surgery, the patient is transferred to a diet that involves a complete restriction of fiber intake.
These days it is necessary to perform daily bowel cleansing with the help of an enema. To prevent the development of pathogenic microflora in the intestines, a prophylactic course of weak antibiotics is prescribed.
Two to three days before surgery, natural methods of eating are stopped and the patient is transferred to parenteral nutrition. It involves the introduction of nutrients without the participation of the gastrointestinal tract, through intravenous infusions of nutrient solutions.
Hydroureteronephrosis
Unlike hydronephrosis, this disease, in addition to the renal collecting system, also affects the ureter. This process occurs when it is compressed or blocked, which is caused by many factors.
Causes of pathology
Moreover, the lower the ureteral obstruction is localized, the larger the area of its damage.
The most common causes of hydroureteronephrosis are:
- scars that form after surgical interventions;
- damage to the ureter as a result of medical error during operations on the abdominal organs;
- compression of the ureter by tumors of nearby organs, such as the uterus, ovary, rectum;
- narrowing of the lumen of the ureter due to various inflammatory and infectious diseases;
- congenital abnormalities of the structure or location of the urinary tract;
- radiation therapy for cancer.
The mechanism of development of this disease is the same as with hydronephrosis, with the only difference being that the ureter is also involved in the pathological process.
Hydroureteronephrosis is manifested by pain in the lumbar region on the side of the affected kidney. In most cases, the disease affects only one ureter; a bilateral process can be observed as a complication of radiation therapy.
Recovery period
Specialists always guarantee an almost 100% favorable outcome and rapid recovery after ureteroplasty, subject to three conditions:
- The operation was performed in the absence of contraindications.
- The surgeons did not make mistakes that could lead to complications.
- During the rehabilitation period, the patient strictly follows the doctors' recommendations regarding restrictions on physical activity and nutrition.
For about three months, the patient should not lift anything weighing more than 3-5 kilograms, and should also avoid sports, long walks and other activities that may slow down the fusion of internal sutures.
During this period, you must regularly visit your doctor according to the schedule he has drawn up for routine examinations. If such examinations show the presence of disorders or complications, additional drug treatment may be prescribed.
The catheter is usually removed during the first week after surgery, but the amount and color of urine must be monitored : they should get closer to normal every day.
In recent years, such operations have been performed using laparoscopy (several punctures are made to access the pelvic ureter, into which surgical instruments are inserted).
Such punctures heal quickly, and the patient can be discharged after a few days. But in some cases, abdominal surgery is required, in which the patient must remain in the hospital for up to three weeks until the abdominal incision heals.
Ureteral fistulas
Another indication for plastic surgery on the ureter is its injury during strip operations.
Myoma
This often happens during gynecological operations for tumor lesions of the body or cervix, during removal of fibroids.
There is also a risk of damage to the ureter during extremely difficult labor and a cesarean section. In addition, injury is possible during laparoscopic procedures.
That is, in the vast majority of cases, such injuries are typical for women.
The main symptom of a ureteral fistula is the release of urine from the vagina in small quantities, regardless of controlled urination.
And if in the case of hydronephrosis or hydroureteronephrosis, the outflow of urine can be temporarily restored by inserting a catheter directly into the renal pelvis, then in the case of a ureteral fistula, plastic surgery must be done immediately.
Depending on the degree and location of urinary tract damage, there are several types of ureteroplasty:
- plastic surgery on the ureteropelvic segment;
- ureteroureteroanastomosis;
- ureterocystoanastomosis (ureterocystoanastomy);
- plastic surgery using the Boari method;
- intestinal plastic surgery.