What is a rectovaginal fistula?
A rectovaginal fistula is an unnatural connection between the vagina and rectum through a fistulous tract (canal). The fistula tract can be short, straight or tortuous. Most fistulas are acquired diseases. Congenital malformations are usually corrected during childhood.
A fistula forms within a few days. The reasons for its formation may be:
- complications during childbirth;
- radiation therapy (irradiation for cancer treatment) in the pelvic area, rectum;
- injuries to the walls of the vagina or rectum;
- paraproctitis - purulent inflammation of the tissue around the rectum leads to perforation (formation of a hole) in the vaginal wall and a rectovaginal fistula is formed;
- complications of Crohn's disease, colon diverticulosis;
- complicated operations on the rectum;
- complicated gynecological operations.
The posterior wall of the vagina and the anterior wall of the rectum are located very close, therefore, when exposed to damaging factors, the intestinal mucosa falls through the opening into the vagina. The rectal wall is practically pressed into the vaginal wall, since the intraluminal pressure is higher in the rectal ampulla. Such a pathological connection of the walls is always accompanied by inflammation, so the tissues grow together. And in just a few days, an abnormal communication of organs with each other is formed - a rectovaginal fistula. It does not heal itself and becomes a chronic “problem” for the patient.
Prognosis and prevention of vaginal fistulas
Serious postoperative complications of vaginal fistulas are failure of intestinal sutures and recurrence of the fistula, requiring repeated radical surgery. The prognosis for ability to work and quality of life after elimination of vaginal fistulas is relatively favorable. After closure of vaginal fistulas, women are recommended to deliver their next pregnancy by cesarean section no earlier than 2-3 years after the operation.
Prevention of vaginal fistulas consists of preventing obstetric injuries, qualified management of obstetric and gynecological operations, and timely treatment of genital inflammation.
Symptoms of the disease
- Pathological vaginal discharge - pus or mucus with an unpleasant (fecal) odor.
- When the hole size is 1 cm or more in diameter, patients note fecal discharge from the vagina.
- The passage of intestinal gases from the vagina.
- Pain in the perineal area.
- Frequent inflammatory diseases of the female genital organs are vaginitis (colpitis), cervicitis.
- Ascending urinary tract infections - urethritis, cystitis, chronic pyelonephritis.
- Violations in intimate life.
- Hygiene problems.
- Itching and maceration of the skin of the perineum.
Why should you contact our clinic?
- Availability of experienced highly specialized urologists and gynecologists
- Use of gentle surgical approaches
- Use of innovative technologies such as da Vinci robotic surgery
- Multidisciplinary approach to patient care
- Providing a personal case manager to coordinate the treatment process
Contact our consultants to find out about the possibility of treating genitourinary fistulas in one of the best clinics in Israel.
- 5
- 4
- 3
- 2
- 1
(1 vote, average: 5 out of 5)
What examinations are necessary to clarify the diagnosis?
Diagnosis of a rectovaginal fistula includes a mandatory examination by a coloproctologist, gynecologist, and a number of standard studies - CBC, OAM, biochemical blood tests. Next, to establish the length of the fistula tract, the level of its location on the rectovaginal septum and the presence of purulent leaks, the following are carried out:
- Transvaginal ultrasound;
- Transanal ultrasound;
- Ultrasound of the pelvic organs and retroperitoneal space;
- Colposcopy;
- Sigmoidoscopy;
- Anoscopy;
- Probing and staining of the fistula tract (according to indications);
- Irrigoscopy (according to indications);
- CT or MRI of the pelvic organs (if indicated).
The identified location of the fistula—low, close to the anal sphincter or high, closer to the cervix—affects the choice of type of operation.
Diagnostics
Diagnosis of vaginal fistulas begins with a gynecological examination of the patient and collection of anamnestic data. With low-lying formations, a retracted scar (ostium) is visualized in the mirrors, from which urine or intestinal contents ooze. Determination of the direction and height of the fistula tract is carried out by probing with a button probe. To localize urovaginal fistulas, chromocystoscopy and urethrocystoscopy with indigo carmine are performed.
In the diagnosis of inflammatory fistulas, laboratory tests of urine and blood, ultrasound of the kidneys and pelvis are prescribed. For difficult to diagnose punctate and highly located urovaginal fistulas - retrograde and excretory urography, cystography, renography, vaginography. For rectogenital fistulas, a rectovaginal examination is performed to determine their consistency and size, the amount of scar damage to surrounding tissues, the presence of infiltrate, the degree of anal sphincter insufficiency, and the likelihood of developing an abscess.
It is mandatory to differentiate the diagnosis using colonoscopy and sigmoidoscopy. For complex fistulas, contrast radiographic studies are performed: fistulography and irrigoscopy.
Diagnosis of the disease may include histological or cytological analysis of affected tissues taken via CT scan or biopsy. The rectoanal reflex is assessed using instrumental methods - anorectal manometry, electromyography, sphincterometry.
Treatment
Treatment of rectovaginal fistulas after radiation therapy (irradiation) is still a controversial topic. The decision is made on a case-by-case basis, depending on the stage of cancer, the general condition of the patient and the condition of the tissue at the site of the intended operation. The degree of radiation damage to tissues is of great importance for the prognosis (they may recover poorly and regenerate after surgery).
Fistulas resulting from birth trauma or traumatic injury, in most cases, respond well to surgical treatment, because pathological processes in the underlying tissues are minimal, and the healing process is faster and easier than in other cases.
The causes of rectovaginal fistulas are radically different - from acute trauma to chronic inflammation, therefore the methods of intervention and tactics of patient management are strictly individual.
During the operation:
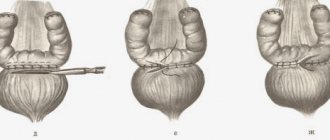
- excision and suturing of fistula openings from the rectum and vagina;
- mobilization of the rectovaginal septum (elimination of tissue tension in the fistula area);
- strengthening the tissues of the septum. The mucosa is reduced (plasty with a tissue flap) or the septum is duplicated with a mesh graft;
- excision of the fistula tract, search and elimination of purulent leaks, branches of the fistula tract, inflammatory infiltrates.
To access fistulas located close to the anal sphincter, perineal or transvaginal access is used. If the fistula tract is located in the middle or upper third of the rectovaginal septum, it is possible to use access through the anterior abdominal wall (incision on the abdomen).
If necessary, a temporary colostomy can be performed (the intestinal opening is exposed to the abdominal wall). In this case, feces are removed through the stoma and the operated area is cleansed and heals faster. Subsequently, the anatomical integrity of the large intestine is restored with repeated surgery (the colostomy is removed).
Diagnosis of ureterovaginal fistulas in Israel
Israeli clinics are constantly expanding their range of services.
Today, if you are not sure about the correctness of the diagnosis given to you or the treatment prescribed, you can seek a “second opinion” from independent Israeli experts. Also, now it is possible to get to them for a consultation without leaving your country, and, accordingly, without spending extra money on flights and rental housing. Use also entitles you to a free first in-person visit with a doctor. The diagnostic process at the Top Assuta clinic is clearly coordinated and takes no more than three days:
Day 1: consultation with a urologist and gynecologist
Specialized doctors will listen to your complaints, review existing medical documents, conduct a physical examination and prescribe additional laboratory and instrumental diagnostic tests.
Day 2: diagnostic procedures
To confirm the diagnosis, as well as collect detailed information necessary to choose the optimal therapeutic strategy, you may be prescribed the following medical tests:
- X-ray with dye . During the procedure, your doctor will fill your bladder with a solution containing an X-ray contrast agent. He will then ask you to cough or put pressure on your bladder. With a vaginal fistula, an x-ray will show the contents of the bladder leaking into the vagina.
- Cystoscopy . During this examination, the doctor will use a cystoscope, a hollow device with a camera used to visualize the inside of the bladder and urethra. A cystoscope can detect damage to these organs.
- Retrograde pyelogram . The test involves injecting dye through the bladder into the ureters, followed by an x-ray. An x-ray can help identify fluid leakage between the ureter and vagina.
- Fistulogram . This is an X-ray examination of the fistula. The test helps the doctor determine how many fistulas the patient has (sometimes there are several). The study also provides information about which pelvic organs are associated with the fistula.
- CT - urography. At the initial stage, the doctor injects a special dye into the patient’s vein. Then a computed tomography scan is performed. The test produces detailed images (slices) of the vagina and urinary tract.
- MRI. An MRI machine uses a magnetic field and radio waves to create detailed images of the body's internal structures. With this test, the doctor can determine the path of the ureterovaginal fistula.
Day 3: medical consultation
After the results of all the studies are ready, your attending physician will convene a medical council, which will be attended by doctors of various specialties. Together they will review the diagnostic results, make an accurate diagnosis and develop a therapeutic plan tailored to your specific needs and wishes.
Complications
Ureterovaginal fistulas are often complicated by ascending infection of the kidneys. As a result of the penetration of pathogenic or opportunistic microorganisms, patients develop pyelonephritis, which, in the absence of adequate therapy and impaired immunity, can lead to kidney destruction, peritonitis and urosepsis. Accumulation of urine in the area of the defect leads to the formation of paraureteral urinoma.
When the ureteral lumen narrows at the confluence with the vagina, the outflow of urine worsens, which is accompanied by the development of ureterohydronephrosis, and subsequently chronic renal failure. Constant vaginal urination reduces the quality of intimate life, irritates the mucous membranes, disrupts the normal reaction of vaginal secretions, and provokes the onset of inflammatory processes (colpitis, bacterial vaginosis, vulvitis, urethritis).
Due to the irritating effect of urine, activation of opportunistic flora or secondary infection, the urethrovaginal canals are often complicated by infectious and inflammatory processes - vaginosis, vulvovaginitis, exocervicitis, urethritis. Possible upward spread of infection with the development of endocervicitis, cervicitis, endometritis, salpingitis, oophoritis, adnexitis, cystitis, pyelonephritis. Constant leakage of urine from the vaginal cavity causes maceration of the skin of the external genitalia and can provoke neurotic excoriation.
The pathology interferes with the normal course of labor and significantly increases the risk of rupture of the soft birth canal. Like other types of genitourinary fistulas, urethro-vaginal communications significantly worsen the patient’s quality of life - they interfere with normal sexual life, contribute to the development of depression, hypochondria, and neuroses.
The effectiveness of surgical treatment for gynecological fistulas is 80-100%. The effectiveness of treatment of radiation fistulas is reduced to 50-60%.
Possible complications arising after surgery:
- lack of sexual desire;
- change in the quality and duration of sexual contact;
- psycho-emotional disorders;
- inflammation of the vaginal mucosa;
- bacterial kidney damage (pyelonephritis);
- inflammatory process on the walls of the vagina (vaginitis);
- narrowing of the vaginal walls (stenosis);
- infertility.