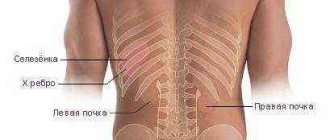
Kidney structure
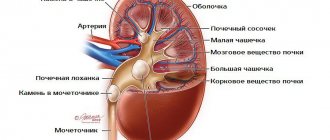
In order to understand how the human urinary system works, you need to know the structure of the kidney filter and its functions. The kidneys are paired organs consisting of parenchyma, externally covered with a connecting capsule. The so-called septa extend from the capsule, dividing each kidney into lobules. The kidney contains:
- the medulla, which is represented by collecting ducts and straight tubules of nephrons;
- the cortex is represented by renal corpuscles and a system of convoluted tubules of nephrons.
The medulla and cortex of the kidney form the parenchyma of the organ. And thin layers of loose connective tissue with numerous lymphatic and blood vessels and nerves form the stroma of the kidney.
The role of the kidneys in the human body
The role of the kidneys is unique; they are vital organs, the dysfunction of which can have very disastrous consequences for the health and functioning of the human body. The kidneys perform a number of functions:
- Regulate the level of Potassium and Sodium ions in the human body;
- Maintain acid-base balance in the blood;
- Remove excess fluid, excess microelements that help retain fluid inside the body, thereby regulating the volume of circulating blood;
- They have an endocrine function, producing special biologically active substances that affect the processes of blood clotting and the formation of red blood cells;
- Maintain blood pressure levels;
- Participate in protein, lipid and carbohydrate metabolic processes in the body;
- Perform an excretory function, removing breakdown products of various substances after digestion of food, medicines, toxic and harmful substances, as well as excess water;
- Perform a protective function against the effects of harmful substances on the human body.
What are nephrons?
Nephrons are the main functional and structural units of the organ. They are a system of tubes, blind on one side (at the beginning), which are lined with epithelial cells in one layer. These cells are called nephrocytes, and their morphological features and height in different parts of the nephrons are different.
There are about 2 million nephrons in the human kidney, the length of one nephron is approximately 30-50 mm, so their total length can be up to 100 km, and their surface area is about 6 square meters. There are two types of nephrons:
- cortical, their system of tubules is located mainly in the cortex;
- juxtamedullary, or peri-cerebral, their system of tubules is located mainly in the medulla of the kidney.
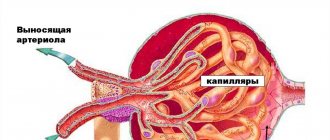
At the blind end of the nephron there is a capsule that encloses the glomerulus of the vessel; together with it, the capsule forms the renal corpuscle. A convoluted tubule (proximal) departs from this capsule; this tubule goes into the straight, ascending and descending thin sections of the nephron. These sections, in turn, form a loop that passes first into the straight distal tubule of the nephron, and then into the distal convoluted tubule of the nephron. The distal convoluted tubules are collected in the intercalary sections into tubes, which are the initial sections of the urinary tract.
Nephron capsule
The nephron capsule is a bowl-shaped cavity with two bounding leaves:
- External, consisting of flat-shaped nephrocytes;
- Internal, consisting of padocyte cells.
Padocyte cells have cytotrabeculae (large cytoplasmic processes), from which cytopodia (small cytoplasmic processes) extend. Podocytes, with their cytoplasmic processes, are adjacent to a three-layer basement membrane, on the opposite side of which there are endotheltocytes of the capillaries of the blood vessel of the renal glomerulus.
A nephron is a collection of cells that form a capsule and a glomerulus with channels extending from it, designed to filter blood plasma and drain urine. This is the elementary functional unit of the kidney, responsible for urination. The nephron consists of a glomerulus that has its own capsule. The afferent arteriole, a blood vessel through which blood enters the glomerulus, flows into it. From the afferent arteriole, many small arterioles depart, which form a glomerulus and gather into a larger one, the efferent arteriole.
The latter is much smaller in diameter than the bringing one, which is necessary to maintain high pressure (about 120 mm Hg) at the inlet. Due to this, the hydrostatic pressure in the glomerulus increases, and therefore almost all the fluid is filtered and not carried into the efferent arteriole. Only thanks to hydrostatic pressure, approximately equal to 120 mmHg, does such a process as renal filtration exist. At the same time, in the kidneys, blood filtration occurs in the nephron glomerulus, and its speed is almost 120 ml per minute.
How to improve filtering
It is extremely necessary to restore kidney filtration, especially if there is persistent hypertension. Along with urine, excess electrolytes and fluids are washed out of the body. It is their delay that causes an increase in blood pressure.
To improve renal activity, in particular glomerular filtration, specialists may prescribe medications such as:
- Theobromine is a weak diuretic that, by increasing renal blood flow, increases filtration activity;
- Euphylline is also a diuretic containing theophylline (an alkaloid) and ethylene diamide.
In addition to taking medications, it is necessary to normalize the patient’s general well-being, restore immunity, normalize blood pressure, etc.
To restore kidney function, you also need to eat a balanced diet and follow a daily routine. Only an integrated approach will help normalize the filtration activity of the kidneys.
Folk methods such as the watermelon diet, rosehip infusion, diuretic infusions and herbal infusions, teas, etc. also help a lot in increasing renal activity. But before doing anything, you need to consult a nephrologist.
The body is an amazing collection of organs and tissues that work harmoniously to maintain human life. And the main process that maintains life is metabolism. As a result of the breakdown of substances, the energy necessary for the occurrence of basic biological processes is synthesized. However, along with energy, potentially harmful metabolic products are also formed. They must be removed from the cell, intercellular fluid and blood by the kidneys. In the kidneys, filtration occurs in the glomerular apparatus, a special structure of the active nephron into which the afferent arteriole flows.
Hepatic encephalopathy
Hepatic encephalopathy usually ends in hepatic coma. Chemical agents that cause its development can be ammonia, fatty acids, mercaptans and other false neurotransmitters. The prodromal stage of hepatic encephalopathy is characterized by euphoria, which over time gives way to depression, slow speech, and sleep disturbances. As the disease progresses, signs of depression, drowsiness, and tremors increase.
Factors that aggravate encephalopathy are a consequence of liver failure: gastrointestinal bleeding, alkalosis and hypokalemia, renal failure, pathology of the central nervous system (atherosclerosis, alcoholism, drug addiction, previous stroke, mental illness).
The main clinical manifestations of hepatargia are predominantly mental and neurological disorders, “liver” odor from the mouth, increasing jaundice, and ascites.
Stages of encephalopathy (according to U. Steiniger et al., 1996):
- Neurasthenic syndrome.
- Doubt.
- Sopor.
- Coma.
- Deep terminal coma.
The basic principles of treatment of encephalopathy include conservative (detoxification, enterosorption, normalization of rheological properties of blood) and special invasive methods (plasmapheresis and amino acid dialysis).
1) vasogenic (caused by disruption of the permeability of the blood-brain barrier and the movement of protein-enriched fluid into the brain tissue with a subsequent increase in intracranial pressure);
2) cytotoxic (in which toxins damage neurons, causing intracellular edema, as well as increased intracranial pressure).
Death with edema can occur suddenly as a result of herniation of the medulla oblongata into the foramen of the occipital bone. The use of corticosteroids and controlled hyperventilation does not provide a positive effect, and the administration of a 20% mannitol solution at a dose of 1 g/kg provides a short-term reduction in edema and does not increase the likelihood of a positive treatment outcome.
Cascade blood filtration
Unlike therapeutic plasmapheresis, when plasma with autoimmune factors is removed from the body and disposed of, the plasma obtained by the cascade plasmapheresis device is sent to a secondary filter. At this stage, unlike conventional plasmapheresis, only harmful components are selectively removed from the plasma. The purified plasma is returned to the person.
The main purpose of using cascade plasmapheresis is to combat atherosclerosis, which causes myocardial infarction, stroke and other severe cardiovascular diseases. Cascade filtration of plasma is also the basis of other methods of efferent therapy. With the help of cascade plasma filtration, some specific treatment methods are carried out, in particular LDL apheresis, or the removal of low-density lipoproteins using filtration technology. In this case, at the second stage, the plasma obtained as a result of filtration of the first stage is passed through columns with sorbents.
Human blood is of great importance for the normal functioning of the body, therefore the condition of the entire body depends on its purity. Under the influence of negative external influences, changes associated with age, bad habits and poor nutrition, gradual contamination of the blood occurs with toxins, toxic and other substances that have a negative effect on it.
You can help your body become healthier and stronger if you periodically do blood cleansing procedures. This is precisely why the plasmapheresis procedure is performed.
You need to know that this method of healing cannot be carried out independently. All procedures must be performed only in a medical facility and only by highly qualified specialists. And also, before deciding on such treatment, you can consult with a doctor who has already performed such “operations” more than once.
Special functions of the renal tubules
The first phase of blood plasma filtration occurs with the participation of the renal filter in the cavity of the nephron capsule. This filter is capable of retaining blood plasma proteins (fibrinogen, antibodies) and blood cells, as well as macromolecules with a negative charge. This is how primary urine is formed.
Cubic or prismatic cells in the proximal nephron have a brush-like border at their apical pole. And the basal labyrinth is the basal part of the plasmalemma, which has “pits” in which mitochondria are located. In this part of the nephron, absorption back into the blood occurs:
- Water;
- Glucose (up to 100%);
- Amino acids (about 98%);
- Electrolytes;
- Uric acid (about 77%);
- Urea (about 60%).
The ascending part of the nephron loop and the distal convoluted section are formed by cubic-shaped nephrocytes (the same as in the proximal section, but without “pits” and a bristly border), and the thin section of the loop is lined with flat-shaped cells. In these sections, water and electrolytes are reabsorbed into the bloodstream.
Next, the nephrons are collected into tubes, which are lined with epithelium of tall cylindrical light and dark cells. It is assumed that light cells are responsible for the reabsorption of electrolytes and water into the bloodstream and produce prostaglandins, while dark cells produce hydrochloric acid.
To maintain optimal conditions for the formation of urine by the kidneys, a process of self-regulation occurs:
- When blood pressure in the afferent vessel increases, the muscle fibers contract and the volume of blood flow decreases, thereby reducing the pressure;
- When blood pressure decreases, the walls of the afferent vessel expand, thereby increasing blood flow.
In a state of stress or shock, blood flow and pressure in the glomeruli decreases; in other cases, as a rule, the pressure in them is maintained at the same level.
Glomerular filtration rate is one of the indicators by which the functional state of the kidneys is determined. The second indicator is reabsorption, which is normally almost 99%. This means that almost all of the primary urine that enters the convoluted tubule from the glomerulus of the nephron after passing through the descending tubule, loop of Henle and ascending tubule is absorbed back into the blood along with nutrients.
Blood flow to the kidneys is carried out through the arteries, which normally consume a quarter of the total minute volume of blood circulation, and the filtered amount is discharged through the veins. This means that if the systolic output of the left ventricle of the heart is 80 ml, then 20 ml of blood will be captured by the kidneys, and another 20 ml by the brain. The remaining 50% of the total systolic volume supplies the needs of the remaining organs and tissues of the body.
The kidneys are organs that take up a huge portion of the blood circulation, but they need blood not so much for metabolism as for filtration. This is a very fast and active process, the speed of which can be easily tracked using the example of intravenous dyes and radiocontrast agents. After their intravenous administration in the kidneys, blood filtration occurs in the glomerular apparatus of the cortex. And within 5-7 minutes after entry it can be seen in the renal pelvis.
In reality, the contrast travels from the venous bed to the lung, then to the heart and then to the renal artery in 20-30 seconds. In another minute, it enters the renal glomerulus, and after a minute, through the collecting ducts located in the pyramids of the kidneys, it is collected in the renal calyces and released into the pelvis.
That is, the filtration of drugs, poisons or metabolic products actively takes place after only 2.5 minutes in the blood. This is a very fast process, which is possible due to the special structure of the nephron. In the kidneys, blood filtration occurs in these structures, the glomeruli of which are located in the cortex. The renal medulla contains only nephron tubules. Therefore, it is correct to say that filtration occurs in the cortical layer of organs.
Many people are mistaken when they claim that in the kidneys, blood filtration occurs in the pyramids. This is a mistake, since they contain mainly only the collecting ducts of the nephron, convoluted, descending and ascending tubules, as well as the loop of Henle. This means that in the pyramids the main process is the reabsorption and concentration of urine, after which it is collected and released into the renal pelvis. The filtration itself takes place in the cortical layer of the kidney, which is richly supplied with blood.
In the kidneys, blood filtration occurs in the nephron capsules, more precisely, in the glomerular apparatus. Here primary urine is formed, which is blood plasma without the main high-molecular proteins. The epithelium that lines the inside of the kidney tubules has special functions. Firstly, it is able to absorb water and electrolytes, returning it to the vascular bed.
Secondly, epithelial cells can absorb low molecular weight proteins, which will also be transferred into the blood without destroying their structure. Thirdly, the nephron tubule epithelium is capable of independently synthesizing amino acids by transamination and glucose by gluconeogenesis from amino acid residues. But this process is not chaotic, but is regulated by the body.
This means that epithelial cells have a number of receptors that receive a signal from mediator molecules, activating either the process of amino acid or glucose synthesis. The fourth feature of the epithelial lining of the renal glomeruli is the ability to absorb monosaccharides in the form of glucose-6-phosphate.
To understand the mechanism of blood purification and urine formation, you need to have an understanding of the structure of the kidney. This paired organ consists of a huge number of nephrons, in which urine formation occurs.
The main renal functions are:
- Urination;
- Blood purification, removal of drugs, metabolites, etc.;
- Regulation of electrolyte metabolism;
- Control of blood pressure and volume;
- Maintaining acid-base balance.
Each bud is bean-shaped. Each kidney has a kind of depression, which is also called a gate. They lead into a fat-filled space or sinus. The pyelocaliceal system, nerve fibers and vascular system are also located there. The vein and artery of the kidney, as well as the ureter, emerge from the same portal.
Each kidney consists of many nephrons, which are a complex of tubules and a glomerulus. Blood filtration occurs directly in the renal corpuscle or glomerulus. It is there that urine is filtered from the blood and goes into the bladder. The video shows the structure of the kidneys
Filtration in the glomeruli of the kidneys occurs according to a simple principle:
- First, fluid is squeezed out/filtered from the glomerular membranes under hydrostatic pressure (≈125 ml/min);
- The filtered fluid then passes through the nephrons, most of it in the form of water and necessary elements is returned to the blood, and the rest is formed into urine;
- The average rate of urine formation is about 1 ml/min.
The glomerulus of the kidney filters the blood, clearing it of various proteins. During the filtration process, primary urine is formed.
The glomerular filtration rate is the volume of primary urine produced in the renal structures per minute. The normal filtration rate is 110 ml/min in women and 125 ml/min in men. These indicators act as a kind of guidelines, which are subject to correction in accordance with the weight, age and other indicators of the patient.[/alert]
Glomerular filtration circuit
Nephrons filter up to 180 liters of primary urine per day. All the blood in the body can be cleansed by the kidneys 60 times per day.
But some factors can provoke disruption of the filtration process:
- Reduced pressure;
- Urinary outflow disorders;
- Narrowing of the kidney artery;
- Trauma or damage to the membrane that performs filtering functions;
- Increased oncotic pressure;
- Reducing the number of “working” glomeruli.
Such conditions most often cause filtration disorders.
How to determine a violation
Violation of filtration activity is determined by calculating its speed. You can determine how limited filtration is in the kidneys using various formulas. In general, the process of determining the rate comes down to comparing the level of a certain control substance in the patient’s urine and blood.
The more inulin in urine in relation to its level in the blood, the greater the volume of filtered blood. This indicator is also called inulin clearance and is considered as a value of purified blood. But how to calculate the filtration rate?
= GFR (ml/min),
where Min is the amount of inulin in the urine, Pin is the content of inulin in plasma, Vurine is the volume of final urine, and GFR is the glomerular filtration rate.
When measuring filtration in women, the result obtained must be multiplied by 0.85.
Quite often in clinical settings, creatinine clearance is used to measure GFR. Such a study is also called the Rehberg test. In the early morning, the patient drinks 0.5 liters of water and immediately empties the bladder. After this, you need to urinate every hour, collecting urine in different containers and noting the duration of each urination.
How is blood purified?
This procedure is one of the most popular methods of blood purification. Medical personnel perform this “operation” in six stages.
- First, blood is drawn.
- After this, the blood is separated into its constituent elements.
- Next, the substances obtained as a result of processing are reintroduced into the bloodstream.
- The missing amount of plasma is replaced with a special physiological solution.
- Plasma that has been processed or that was taken from the patient is added to it.
- The fluid obtained as a result of this entire process is reintroduced into the body.
Additional plasma treatment services are also provided. However, this can only be done in cases of an individual approach.
The process is performed only if there are special devices and apparatus in medical clinics. The patient must lie down during each procedure.
Blood fluid is removed from the body using one or two needles. The devices used for this procedure must be large, much larger than the needles that are inserted into the veins when connecting the IV.
- Fractions are separated by three methods.
- Filtration or membrane.
- Centrifugal or gravity.
- Cascade.
First method
The blood fluid that was taken from the patient is filtered in devices created for this procedure. When the entire stage is completed, the resulting substances are introduced into the patient’s blood, but the plasma substances are destroyed or further filtered. The same applies to cells that have not undergone treatment.
Second method
The collected blood is placed in bags, which are then sent to a centrifuge. The formed element settles in the apparatus. The blood is divided into cell masses and plasma. The plasma is subsequently removed from the bag and the resulting elements are reintroduced into the bloodstream.
Third method
The collected plasma is filtered in a special device. During the filtration process, the plasma passes through an additional filter insert, which allows only low molecular weight proteins to pass through.
Violation of the acid-base state and water-electrolyte balance.
Respiratory alkalosis of central origin, metabolic alkalosis as a result of nausea, vomiting and hypokalemia may occur. Metabolic acidosis develops due to cell hypoxia and accumulation of lactate in the blood. Lactic acidosis is a negative prognostic sign. A variety of electrolyte disturbances are observed: hyponatremia, hypokalemia, hypocalcemia and hypomagnesemia.
= GFR (ml/min),
Fi = (U1/p) x V1,
where Fi is glomerular filtration, U1 is the content of the control component, p is the level of creatinine in the blood, and V1 is the duration of the test urination. Using this formula, a calculation is made every hour throughout the day.
Symptoms
Signs of impaired glomerular filtration are usually reduced to changes of a quantitative (increase or decrease in filtration) and qualitative (proteinuria) nature.
Additional signs include:
- Decreased pressure;
- Renal congestion;
- Hyperswelling, especially in the area of the limbs and face;
- Urinary disorders such as decreased or increased urge, the appearance of uncharacteristic sediment or color changes;
- Pain in the lumbar area
- Accumulation of various kinds of metabolites in the blood, etc.
A drop in pressure usually occurs during shock or myocardial failure.
Symptoms of glomerular filtration disorder in the kidneys
Infusion-drip detoxification
In addition to hardware methods, infusion-drop therapy is quite widely used in medicine, especially in the case of alcohol intoxication.
Droppers for blood purification are included in the treatment of withdrawal symptoms, as they facilitate the functioning of the kidneys, liver and cardiovascular system. Thanks to infusion-drop therapy, blood pressure is normalized, tremors and convulsions go away, anxiety is reduced, and intoxication symptoms such as vomiting, nausea, headache and dizziness disappear. Due to sedative components, aggression is reduced, sleep and the patient’s overall well-being are normalized.
Blood supply to the kidneys
In the human body, the kidneys have the largest blood flow volume compared to other organs. The renal arteries, which supply nutrition to the kidneys, are short and begin from the abdominal aorta. In the kidney, the arteries are divided into arterioles (smaller vessels), which are located in the interpyramidal space.
The arcuate artery passes between the medulla and the renal cortex. From it, smaller arteries, passing in the interlobular space, branch off, feeding the cortex. Next, the interlobular arteries become intralobular, and then branch into the arterioles of the renal glomerulus.
These afferent arterioles from the proximal part go to the renal corpuscles of the intermediate and interstitial nephrons. Next, the arterioles from the distal sections go to the so-called juxtamedullary nephrons of the kidneys. Thus, two types of blood circulation are formed in the kidney:
- Cortical circulation, which is located in the area of the Malpighian tubules;
- Juxtaglomerular circulation, located at the border of the medulla and cortex, in the area of large renal glomeruli.
The efferent and afferent arterioles of the juxtamedullary glomeruli are the same in size. They slow the blood flow and filter the blood, with a small amount of urine being released. In this case, the efferent arteriole does not form a network, does not branch, but descends into the medulla, providing it with nutrition. Already inside the medulla, it branches into capillaries, which collect into venules, and these, in turn, into venous vessels, which connect into the renal veins. The renal veins are collected and drained into the inferior vena cava system.
Where does it happen?
The kidney is, as it were, placed in a capsule, under which there is a granular layer called the cortex, and below it is the medulla. The medulla folds into renal pyramids, between which there are columns that expand towards the renal sinuses. At the tops of these pyramids there are papillae, which empty the pyramids, removing their contents into small calyxes, then into large ones.
The number of calyces may vary in each person, although in general 2-3 large calyces branch into 4-5 small calyces, with one small calyx necessarily surrounding the pyramidal papilla. From the small calyx, urine enters the large calyx, and then into the ureter and bladder structures.
Blood is supplied to the kidneys through the renal artery, which branches into smaller vessels, then the blood enters the arterioles, which divide into 5-8 capillaries. This is how the blood enters the glomerular system, where the filtration process takes place.
Renal filtration scheme
Coagulopathies and bleeding.
Impaired liver function in maintaining hemostasis leads to gastrointestinal bleeding, which in the fulminant form of liver failure can cause death. Violation of the synthesis of coagulation factors, as well as antithrombin III, proteins C, B and thrombocytopenia predetermine the development of disseminated intravascular coagulation syndrome.
Gastrointestinal bleeding, developing against the background of liver failure, increases coagulopathy. To replace blood coagulation factors, fresh frozen blood plasma is used at a dose of 10-20 ml/kg. Hemostatic therapy involves the administration of a 12.5% solution of ethamsylate (dicinone) at a dose of 5 mg/kg, a 1% solution of vikasol (menadione sodium bisulfite) - 1 ml.
For thrombocytopenia (platelet count