19 years of experience
12 urologists
273,016 patients
5 branches
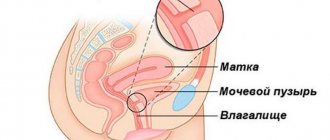
A vesicovaginal fistula is an abnormal duct that is located between the bladder and vagina. This pathology can occur after gynecological surgery; it is classified as a type of genitourinary fistula. Most often, the disease is provoked by various mechanical injuries to the bladder during surgery or after a difficult birth.
Symptoms and diagnosis
The main symptom of a fistula, which indicates the formation of a canal between hollow organs, is the release of urine, but not from the urethra, but from the vagina. This may be indicated by previous heavy vaginal discharge or blood in the urine.
In the future, the patient may feel pain in the lower abdomen, which has varying intensity, radiating to the hip or lower back. These symptoms are combined with purulent vaginal discharge, discharge mixed with urine and high fever. Sometimes menstrual discharge gets into the urine, pain in the kidney area and gastrointestinal disorders are also observed.
The intensity of symptoms depends on the extent of the inflammatory process, its location and the degree of damage to the pelvis.
Genitourinary fistulas can be diagnosed
several methods.
First, the doctor examines the vagina to establish the location of the fistula and its size, direction, connection with the uterus, urethra, their condition and degree of inflammation. The patient is also prescribed:
- general blood analysis;
- general urine analysis;
- Ultrasound of the pelvic organs;
- Ultrasound of the kidneys;
- cystoscopy;
- chromoscopy;
- hysteroscopy;
- renography and excretory urography;
- if necessary, CT and MRI of the pelvic organs.
Quite rarely, the disease is treated with conservative methods such as:
- rinsing the bladder with antibacterial agents;
- taking antibiotics, uroantiseptics;
- ointment tampons in the vagina.
If conservative treatment fails, a decision is made to undergo surgery.
Symptoms of genitourinary fistulas
Clinical manifestations of genitourinary fistulas depend on their location. The most typical symptoms of the pathological process are constant discharge of urine from the vagina, inflammation of the mucous membrane, and urinary dermatosis (skin irritation).
With a ureterovaginal fistula, due to impaired urine outflow, obstructive pyelonephritis may develop, accompanied by severe pain. In this situation, spontaneous closure of the pathological canal most often indicates a complete disruption (loss) of the functioning of the kidney. This condition requires immediate surgical attention.
Preparing for surgery
You should prepare comprehensively for the operation. First of all, it is necessary to weaken the inflammatory process and get rid of various infections. Preoperative preparation includes the following activities:
- taking antibiotics;
- hormone therapy for women undergoing menopause and for those who have had a hysterectomy;
- removal of ligature stones;
- preparation of the vaginal cavity and bladder with antiseptic and anti-inflammatory agents.
Before surgery, the patient should stop taking medications that affect blood clotting. Next, disinfection is carried out. The specialist determines which type of anesthesia is most suitable for the patient.
Causes of genitourinary fistulas
The main cause of fistulas is damage to the urinary tract during gynecological operations (removal of the uterus, incorrect choice of surgical delivery, plastic surgery of the anterior vaginal wall, etc.).
In addition, a prerequisite for fistula formation may be:
- radiation therapy for malignant tumors of the pelvic organs (so-called post-radiation MPS);
- burns during laparoscopic interventions;
- installation of synthetic materials in the treatment of pelvic organ prolapse and urinary incontinence;
- obstetric injuries;
- introduction of foreign bodies during masturbation.
Carrying out the operation
The manipulation is carried out under general anesthesia. The specialist can use two methods to access the lesion:
- through the patient’s vagina (transvaginal route);
- through the abdominal cavity (by opening the bladder - abdominal access).
Sometimes a specialist needs to perform an operation combining two types of access.
Transvaginal surgery
This technique is considered preferable if the patient has small fistulas, without serious complications and with well-movable vaginal walls.
The first stage of the operation is:
- insertion of a Foley catheter;
- performing trocar cystostomy;
- catheterization of the ureteric orifices.
After this, a rear speculum is inserted into the vagina and a self-retaining tetractor is placed.
The second stage of the operation includes full recognition of the fistula and its suturing in a circle. Next, the fistula is excised. The bladder in the damaged area is closed with a special material.
If the fistula reaches a large size, then specialists use the Martius method, when a fragment of the labia majora of the operated patient acts as the material for plastic surgery.
At the end of the operation, the doctor places a tampon with betadine into the patient's vagina.
Transvaginal surgery is the most successful method for eliminating fistulas, since the doctor has good visibility and sufficient space for manipulation.
Types and causes of fistula formation
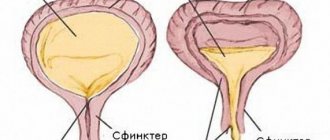
A bladder fistula is a defective painful passage that combines the organs of the abdominal cavity and groin, or the skin with the bladder.
The hole has the shape of a narrow channel lined with epithelium or granulation tissue, through which urine flows from the bladder to nearby organs, skin and through them to the outside. A fistula is formed as a result of a pathological process in the internal organs, damage to them as a result of invasive intervention and provokes continuous infection of the genitourinary organs. Casanova set from 850 rub.
Lovelace set from 850 rub.
Family set from 1200 rub.
Generics for increasing potency
Types and classification of genitourinary fistulas
Bladder fistulas can be:
| Natural. | Formed during intrauterine development, as a result of partial overgrowth of the urinary duct of the embryo |
| Found. | Formed during a person’s life during a previous illness, which is accompanied by the removal of pathological areas of the bladder or the forced removal of urine from it |
Depending on the location of fistulas in the genitourinary tract in women, it can be in the following areas of the body:
- bladder, vagina, rectum;
- the bladder, ureter, and vagina maintain communication through the fistula canal;
- the bladder, urethra, and vagina have commonalities with each other and transmit urine;
- the bladder and part of the uterus have one pathological canal;
- between the bladder and vagina.
In men, there are other types of fistula:
- vesicointestinal;
- urethro-prostate-perineal;
- urethro-prostate-rectal.
The name of the type of fistula is determined by the involvement of nearby organs and the formation of a canal opening between them.
Pathology can occur due to many reasons
The main causes of a fistula in the bladder
The origin of a fistula in the bladder is different in men and women , since the structure of the body and genitourinary organs is different.
But they are united by the root causes of pathological formation:
- Injury to organs. Operational events, accidents, shocks and other reasons that violate the integrity of tissues contribute to the formation of a hole in the bladder;
- Inflammatory diseases. The pathological condition is accompanied by the release of pus from the body, which can rupture the intercellular partitions and provoke a pathological fistula channel;
- Malignant formations. An oncological tumor has the ability to change the structure and volume of organs, rupture walls, and transfer cancer cells to neighboring areas;
- Radiation exposure. The appearance of a fistula is a complicated condition after irradiation.
The common factor in the appearance of a fistula in men and women is intestinal diseases, when the integrity of the wall of a hypertrophied and painful organ is disrupted and it communicates with the bladder.
Complications
Basically the operation is quite successful. Possible complications include relapse. When it occurs, the operation is performed again, but using the Martius method.
Quite rarely noted:
- vesicoureteral reflux;
- overactive bladder.
In these cases, the patient is prescribed antimuscarinics.
Contact the URO-PRO clinic for competent help. Do not self-medicate, this will help avoid complications in the future.
Make an appointment now by filling out the online form on our website.
Don't delay treatment - make an appointment. It's anonymous!
Call
8 (861) 217-70-99
or sign up online
Sign up online
Participated in the preparation of the article
Diagnostic minimum
Symptoms of a bladder rupture
Diagnosis begins with detailed questioning and examination. The doctor collects anamnesis regarding the onset of the disease and the patient’s complaints.
He is interested in what operations the patient has undergone and studies the history of his illness. He also examines it, and an external fistula and leaking urine can be detected.
A gynecologist has the ability to diagnose a vesicovaginal fistula; it is visible when examined using a speculum. The doctor also takes a sample of vaginal discharge to determine whether it is urine or not. If, according to the results of laboratory tests, the concentration of creatinine in this fluid exceeds that in the blood, then this is urine.
In addition, for women, a cystoscopic technique is provided, which is performed after the vagina is closed with tamponade. Cystoscopy makes it possible to understand where the tract is localized, what its size is, and how violently the inflammation proceeds.
More accurate, in terms of determining the size and location of the pathology, are vaginographic examination, chromocystoscopy, cystography, and retrograde urethropyelography. Undoubtedly, the doctor prescribes routine tests (general blood and urine tests, blood biochemistry, bacteriology of urinary fluid and vaginal discharge).
To understand how the kidneys work, monitoring the level of creatinine, urea, and electrolyte composition is prescribed. The course of the fistula is determined by fistulography. But a fistula between the bladder and the intestines can be identified by sigmoidoscopy and finger examination. If cancer is suspected, a biopsy is used.
Treatment and rehabilitation period
Traditional treatment involves surgical suturing. If the diameter is small, it is removed by electrocoagulation, which is carried out on the epithelium. A special catheter in the form of a balloon is inserted into the bladder for 10-14 days. If the gap is large, it sometimes becomes necessary to use artificial materials and other fabrics. In most cases, the large or small intestine or part of the omentum is used for this purpose.
Return to contents
Traditional methods
A small bladder fistula can be cured with St. John's wort. You need to take 3 tablespoons of the crushed mixture, add 200 grams of water and boil for 5 minutes. A mixture of boiled St. John's wort on cellophane is applied to the site of the fistula. This procedure must be applied continuously until the pus leaves the affected area. After this, you need to repeat the procedures several more times for prevention.
In the early stages, damage to the bladder can be healed with decoctions of St. John's wort.
To get rid of a fistula, use aloe leaves, which are mashed into a paste and infused with honey (10 leaves per 1 liter of honey) for 5-7 days. This mixture should be taken 1 teaspoon per day 3 times. During the course, the fistula is washed with a weak solution of furatsilin or an ointment is used: lard, toadflax inflorescences, oak bark, peppermint are crushed in the ratio of 2 parts lard to 1 part herbal collection. The ingredients are placed in a bowl and placed in the oven for 9 hours.
The resulting ointment should be applied to the fistula using cotton swabs. The compress is changed every 12 hours. You can relieve inflammation with herbal infusions of calendula, hawthorn, and peppermint. It should be remembered that self-treatment with folk remedies requires a responsible approach. If the means used are ineffective, you should seek help from a doctor.
Return to contents
Why does a fistula form?
A bladder fistula is formed due to trauma, when organs and tissues are damaged during surgery, especially if the intervention is performed unprofessionally. Congenital anomalies in a child inside the womb cause the development of congenital fistulas. This most often happens when the ureters and canals are poorly fused during the formation of the embryo.
All causes of fistula formation can be traumatic, inflammatory, cancer or radiation. The vesicogenital variety occurs quite often, accounting for more than 50% of all anomalies. Their etiology is usually in difficult labor and unsuccessful abortions. Inflammation provokes a breakthrough in the tissues of the bladder, and an abscess occurs in the prostate gland. Pus accumulates in the pelvic cavity, which leads to complications.
Possible complications and consequences
Lack of therapy or late contact with a doctor can lead to complications in the form of inflammation and abscesses. Cystitis, colpitis are concomitant pathologies. Kidney inflammation develops due to impaired urine flow. Stagnation of urine in the canals with an external fistula causes suppuration in the tissues. The menstrual cycle is disrupted or completely absent. When urine enters the organs, an inflammatory process occurs; in the worst cases, purulent processes begin. Self-medication often leads to negative results, so it is advisable to use folk remedies under the supervision of a doctor.
Return to contents
Consequences, prevention
The consequences of fistulas are always inflammation of the urinary reservoir and neighboring organs, as a result of which they cannot cope with their functions, intoxication of the body, kidney damage, even acute renal failure. With timely and adequate treatment, urinary fistulas close without disturbing the patient.
Preventive measures - timely treatment of diseases of the genitourinary system , regular preventive examinations. It is important that medical staff responsibly carry out surgical procedures, including during the delivery process. Attention is paid to pregnant women with a narrow pelvis and transverse placement of the fetus.
Treatment
Treatment of fistula of the urinary reservoir is conservative
and
operational
. The first method is used if the size of the fistula is less than 3 mm. Therapy involves inserting a Foley catheter into the bladder for 30 days and washing the latter. Then antibacterial and uroseptic drugs are prescribed.
If after 2 months the pathological tract does not close, and also if the initial size of the fistula is more than 3 mm, resort to fistuloplasty
. It involves excision of the affected tissue, separation of the bladder from the affected neighboring organ, and suturing the hole. During the operation, the access above the pubis is used for women, and the perineal area for men. After suturing the hole between the urinary reservoir and the vagina, an epicystoma is installed, and when suturing the enterovesical fistula, a colostomy is installed.
The operation is always preceded by taking antibiotics and uroseptic agents, the task of which is to reduce inflammation. The use of traditional methods is permissible only at the stage of recovery after treatment. Traditional medicine cannot act as the only method of treating fistulas.
Prevention
To exclude the occurrence of the disease, preventive measures should mainly come from doctors who perform surgical interventions. Attentiveness and professionalism during childbirth, special attention should be paid to women who have a narrow pelvic passage. Laparoscopic and abdominal operations should be performed with an increased level of safety. Increased attention must be paid when examining injuries to the abdominal cavity and genitourinary organs for the timely diagnosis of a fistula.
Bladder fistula: why it occurs and how to treat it
Bladder fistulas are a serious complication of various bladder diseases, as well as pathologies of the intestines and genital organs.
According to the classification, urinary and genitourinary fistulas are distinguished. The latter usually occur in women and are a consequence of obstetric or gynecological surgical interventions. Pathological communication between the urinary tract and the intestinal lumen is more often detected in males. In urological practice, such patients constitute one of the most severe groups of patients. The severity of their condition, on the one hand, is determined by the course of the underlying disease, which led to the formation of a fistula, and on the other hand, by the flow of intestinal contents into the urinary tract and urine into the intestinal lumen, and sometimes urine and feces into the surrounding tissue, which leads to the development purulent-septic complications.
Classification of the disease
Urethral fistulas can be divided according to the place of formation:
- urethrogluteal;
- urethrovaginal, such fistulas are formed in the vaginal mucosa, with urine leaking into this organ, which ultimately leads to an inflammatory process;
- urethro-perineal fistulas form in the perineal area, with urine leaking out;
- urethro-scrotal - these are formations extending into the scrotum;
- urethro-rectal fistulas open into the rectum, while infectious diseases that develop as a result of such a fistula can only be eliminated surgically;
- urethropenial, the opening from the urethra opens onto the penis.
There are also combined genitourinary fistulas. Moreover, several parts of the genitourinary system are involved in this process. More often you can find ureterovesical-vaginal fistulas; in rare cases, the intestines are involved in this process.
Diagnostics
Cystography plays an important role in the diagnosis of bladder fistulas.
Identifying bladder fistulas is usually not difficult. It is more difficult to determine the cause of the disease and assess the degree of existing disorders. This takes into account:
- patient complaints;
- history of his illness (presence of injuries to the genitourinary system, operations, radiation, etc.);
- objective examination data (in case of genitourinary fistulas, the size and location of the fistula can be determined by vaginal examination).
To clarify the diagnosis, additional diagnostic methods are used:
- plain radiography of the urinary tract (detects shadows of stones or gas in the bladder);
- excretory urography (allows you to evaluate the function of the bladder, its condition and determine the penetration of contrast into the intestines);
- cystography (detects fistula);
- cystoscopy (makes it possible to examine the walls of the bladder from the inside, visually determines the presence of a fistula tract and, if necessary, allows for a biopsy of a suspicious area of tissue);
- computed tomography with contrast (one of the most reliable methods for visualizing vesico-intestinal fistulas).
What types of fistulas are there?
- External - connection of the bladder with the skin. In this case, a specific hole is formed in the thickness of the skin. More often, the course is tortuous, which is dangerous due to the development of depressions into which urine gets in and provokes an inflammatory process.
- Internal - creating a communication between a bladder and hollow organs.
There is also a piece fistula of the bladder, which is specially created by surgeons during surgical interventions. A piece connection is made during severe operations for the purpose of removing urine, when the body is not able to remove urine naturally. This type of urinary fistula is classified as external because it is the optimal and safe way to remove urine.
Why do they arise?
Fistulas often arise as complications of surgical interventions.
The reasons for the formation of urinary fistulas can be different:
- congenital anomalies (fistula between the rectum and the bladder triangle in combination with atresia, that is, fusion of the anus);
- traumatic injuries (due to wounds, surgery);
- intestinal diseases (diverticulosis, Crohn's disease, appendicitis);
- malignant neoplasms of the intestine or bladder;
- perforation by foreign bodies;
- consequences of radiation therapy.
Among genitourinary fistulas, vesicovaginal fistulas are more common, and pathological communications between the bladder and the cavity or cervix are less common. They may be a consequence of:
- tissue damage during gynecological surgery, childbirth;
- unqualified provision of obstetric care;
- protracted labor in women with weak labor (prolonged compression of the bladder between the fetal head and the pelvic bones);
- violent trauma;
- spontaneous perforation of an abscess of the pelvic cavity into a hollow organ;
- tumor disintegration;
- diseases of the pelvic organs of inflammatory nature.
Post-radiation fistulas have a particularly severe course. Their formation is facilitated by:
- excess radiation dose;
- non-compliance with intervals between sessions;
- increased individual sensitivity to ionizing radiation.
Complications and consequences
If effective therapy is not carried out and the patient misses the time to seek help, complications begin - abscesses and inflammation. Colpitis and cystitis are frequent companions of fistula. An inflammatory process develops in the kidneys as a consequence of a violation of the outflow of urine, and inflammation is also present in the tissues.
The menstrual cycle is disrupted or stops completely. When urine enters the organs, inflammation and accumulation of pus occurs. In such cases, self-medication can be fatal, as can the incorrect use of traditional medicine. Any herbs or medications taken should be discussed with your doctor.