Concept and main functions of the kidney parenchyma
Parenchyma is the main tissue of an organ. Its components are the cells of the medulla (inner layer) and cortex (outer layer) of the substance. The structure of the tissue is smooth, in appearance it resembles a capsule in which the organ and elements of the urinary system are placed.
The main function of the parenchyma is to remove metabolic products from the body and, as a result, create conditions for preserving the natural internal state of the organ.
The thickness of the kidney tissue in a healthy person of the middle age group is from 15 to 23 millimeters. If the patient has ever suffered from infectious diseases, there are untreated inflammatory and chronic processes in the urinary system, this will lead to thinning of the tissue. However, the parenchyma has the ability to gradually recover.
Now you will not be frightened by the term kidney parenchyma; what it is and what its functions are, has become known.
Etiology and pathogenesis
Replacement of the renal parenchyma with connective tissue can be observed in advanced hypertension (see) and is most often associated with narrowing of the renal arteries - primary N. (angiogenic N.), primary wrinkled kidney. Due to insufficient blood supply and increasing hypoxia, dystrophic and atrophic changes in the renal parenchyma occur, followed by the proliferation of connective tissue. Depending on the nature of the process leading to narrowing of the renal arteries, N. is distinguished between hypertensive, or arteriolosclerotic, and atherosclerotic. In the pathogenesis of primary N., hron, venous plethora, is also important, in which the proliferation of connective tissue in the kidneys is associated with increased synthesis of tropocollagen in conditions of oxygen deficiency. Primary N. includes post-infarction N., which develops with scarring of multiple renal infarctions (see).
The growth of connective tissue in the kidneys can occur secondaryly, as a result of various diseases (secondary N., secondary wrinkled kidney). Secondary N. is the outcome of inflammatory and degenerative processes that occur in the kidneys during chronic, glomerulonephritis, pyelonephritis (pyelonephritic shrinkage of the kidneys, pyelonephritic shrinkage of the kidneys), kidney stones (calculous N.), tuberculosis (tuberculous N.), syphilis (syphilitic N.). ), rheumatism (rheumatic N.), systemic lupus erythematosus (lupus N.), amyloidosis (amyloid wrinkling of the kidneys, or amyloid-wrinkled kidneys), diabetes mellitus (diabetic N.).
Secondary N. can develop after such adverse effects as trauma (including after repeated kidney operations), exposure to ionizing radiation, as well as in severe forms of nephropathy in pregnant women - preeclampsia and eclampsia. Spasm of the arteries, inflammation of the renal glomeruli and degeneration of the tubules characteristic of nephropathy after delivery in some cases are transformed into hron, glomerulonephritis, which, slowly progressing, leads to wrinkling of the kidneys, the severity of the changes and the characteristics of the course distinguishes two forms - benign and malignant. The benign form is characterized by arteriolosclerosis (Fig. 1), often in combination with atherosclerosis of the renal artery and its large branches, atrophic changes in groups of nephrons with secondary hyalinosis of the glomeruli (Fig. 2), an increase in the connective tissue stroma, and hyalinosis of the papillae of the pyramids. Macroscopically, the surface of the kidneys is fine-grained, and when combined with atherosclerosis, it becomes coarsely lumpy. As arteriolosclerotic changes increase, combining
Such sharp information. diseases such as hemorrhagic nephrosonephritis, leptospirosis, typhoid and typhus, scarlet fever, measles, as well as sepsis, are accompanied by changes in the parenchyma, interstitium and vessels of the kidneys that vary in mechanism of injury and severity - from focal glomerulonephritis without impaired renal function to tubular necrosis and acute renal insufficiency. After these inflammatory and necrotic changes, N. develops of varying degrees of severity, which usually does not progress.
There is also involutive N., which is caused by age-related changes in the vessels of the kidneys, as well as atherosclerosis or hypertension, often observed in elderly and senile people.
Presence of heart problems and their symptoms
Erythremia, or polycythemia, is a tumor blood disease. The pathology is characterized by hyperplasia of hematopoietic sprouts located in the bone marrow and, as a consequence, excessive formation of red blood cells.
Platelets and white blood cells are produced in smaller, but still increased quantities. In addition, the level of hemoglobin increases and the volume of circulating blood increases. The disease is benign in nature, but in rare cases, erythremia becomes malignant.
Erythremia is a rare pathology - only 29 out of 100,000 people get sick per year. The main group of patients is people 60–79 years old. At a young age, the disease develops less frequently, but is more severe. Elderly men get sick slightly more often than women of their age (1.5:1.0).
At this time, medicine cannot accurately answer why erythremia develops. There are several hypotheses explaining the appearance of the disease:
- mutation of stem cells and transformation of genes that regulate the growth of blood cells;
- genetic predisposition - Down, Klinefelter, Bloom, Marfan syndromes;
- ionizing radiation, which causes blood diseases;
- benzene poisoning;
- side effects of some antibiotics (Chloramphenicol), cytostatics (Methotrexate, Azathioprine, Cyclophosphamide);
- in children - toxic dyspepsia, stress erythrocytosis.
Blood in the body is produced by red bone marrow, located in the bones of the pelvis, spine, skull, ribs, and tubular bones of the extremities. In the hematopoietic function, the main role is played by stem cells - unique units of bone marrow. By dividing, they form clones that are reborn into any blood cell.
Today, more and more people are complaining about poor heart condition. If emergency assistance is not provided in time, the consequences can be very sad. The most dangerous condition of our motor is acute myocardial infarction. What kind of disease is this, how to fight it and provide quality treatment?
- Description and causes of the disease
- Signs of the disease
- Classification of the disease
- Diagnosis of the disease
- What to do?
In Russia, tens of thousands of people die every year from myocardial infarction, 65,000 to be exact. Many others become disabled. This disease spares no one, neither the elderly nor the young. The whole point is the heart muscle, which is called the myocardium.
A blood clot blocks a coronary artery and heart cells begin to die
Blood flows through the coronary arteries to this muscle. A blood clot can block one of the arteries that supplies it. It turns out that this part of the heart remains without oxygen. In this state, myocardial cells can last about thirty minutes, after which they die.
This is the immediate cause of a heart attack - arrest of coronary circulation. However, it can be caused not only by a blood clot. In general, the reasons for this situation in the vessels can be described as follows:
- Atherosclerosis. In this case, a blood clot forms. If you do not interfere with its formation, it will grow very quickly and eventually block the artery. The above process occurs, which causes such a terrible disease;
- Embolism. As you know, this is a process in which the blood or lymph contains particles that should not be in a normal state. This leads to disruption of local blood supply. If embolism is the cause of acute myocardial infarction, then most often it is a fat embolism, in which droplets of fat enter the bloodstream. This happens with numerous bone fractures;
- Spasm of heart vessels. This means that the lumen of the coronary arteries narrows sharply and suddenly. Although this process is temporary, the consequences can be the most unpleasant;
- Surgical interventions, namely complete transverse dissection of the vessel or its ligation;
In addition, the factors that influence the above reasons, and accordingly, the occurrence of the acute course of the disease we are discussing, can be described as follows:
- Diabetes is a dangerous disease, so its treatment should not be left to chance;
- Smoking;
- Stress;
- Hypertension;
- Age (the most common occurrence of myocardial infarction occurs in women after 50 years and men after 40 years);
- Obesity;
- Hereditary predisposition;
- Low physical activity;
- Heart arythmy:
- Already suffered myocardial infarction;
- Cardiovascular diseases;
- Alcohol abuse;
- Increased amount of triglycerides in the blood.
You can help your heart even before the disease worsens; you just need to change your life.
Symptoms that are quite pronounced will help determine the occurrence of a heart attack. The main thing is to recognize them in time and take the necessary measures.
This disease has a clear sign that occurs very often - pain localized behind the sternum. However, for some, this feature may not be expressed strongly, and for those who have diabetes, it may not be present at all.
Clinical picture
The danger of a drying out kidney is the absence of a symptomatic picture at the initial stages of development of the pathological process. Exceptions include acute illnesses. As the disease progresses, the patient experiences pain in the lumbar region.
A wrinkled kidney is characterized by signs of diuresis disorder. There is a significant increase in the amount of urine excreted up to 3.5 liters per day with a low specific gravity (below 1010), which leads to its clarification.
The amount of protein in the urine increases. Proteinuria is not typical for nephrosclerosis against the background of vascular pathologies; in rare cases, laboratory tests can detect traces of protein. A wrinkled kidney due to disruption of the organ’s vascular system occurs with symptoms that are characteristic of hypertension, which significantly complicates the diagnostic process.
- increased blood pressure;
- rounding and protrusion of the left border of the heart, which is clearly visible on x-ray images;
- tachycardia;
- hypertrophy of the left and right ventricle.
In this case, the patient may be bothered by the following symptoms:
- dizziness;
- headache;
- sleep disturbance;
- feeling of anxiety;
- increased aggressiveness;
- weakness;
- fast fatiguability;
- dyspnea;
- pain in the area of the heart muscle;
- uremic asthma;
- pulmonary edema is manifested by wheezing and sputum production;
- swelling of the limbs, gradually increasing, affects the face and torso;
- disturbances in the functioning of the digestive tract, which is manifested by stool retention, diarrhea, nausea and vomiting;
- itching and peeling of the skin.
Diagnostics
It should be remembered that if unpleasant symptoms occur, you should consult a doctor as soon as possible. Based on data collection, a specialist will be able to make an accurate diagnosis and prescribe the correct treatment.
First, the doctor examines and interviews the patient.
The specialist may also refer the patient to donate blood and urine for laboratory analysis.
In addition, the doctor will definitely ask the patient about the medications he has taken previously.
After this, the specialist will examine the patient’s chart. This is necessary in order to identify what diseases the person has previously suffered from and whether he or she has an allergic reaction to the components of the drug.
Currently, citizens suffering from drug addiction are often sent to inpatient departments. Kidney infarction in this category of citizens occurs while taking drugs containing opium injected into the body. As a result, this patient develops specific endocarditis. The consequence of such a lesion is disruption of the tricuspid and other heart valves. This process develops rapidly against the background of reduced immunity in the patient.
In addition, additional diagnostic methods are used. These include:
- Conducting Doppler ultrasound of the ureters and kidneys, abdominal cavity and aorta. With its help, the general condition of the kidneys and the vessels in them is revealed. It is considered a non-invasive diagnostic method, which is currently available to every medical clinic.
- Use of computed tomography and magnetic resonance imaging. They will be especially effective when a special contrast agent is introduced. Using contrast, you can identify abnormalities and identify the problem area.
- Use of angiography.
Most patients do not know where to go to identify a kidney infarction. A nephrologist diagnoses and treats this disease.
Development of nephrosclerosis
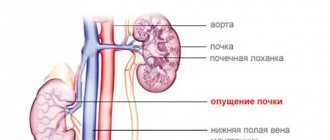
The human kidneys are a paired organ located retroperitoneally in the lumbar region. They are bean-shaped and consist of parenchymal tissue and the pyelocaliceal system. Wrinkling is the process of replacing functional parenchymal tissue with connective tissue. At the same time, the organ decreases in size. The functions of the organ decrease or completely disappear.
The kidneys perform the following important functions in the human body:
- excrete metabolic products, excess water, medications and various toxic substances into the urine;
- produce the hormone renin;
- provide a constant blood pH;
- regulate blood clotting;
- participate in phosphorus-calcium metabolism.
Wrinkling can be primary or secondary. Primary wrinkled kidney is a disease in which the blood supply to the organ is disrupted. The secondary form is caused by damage to parenchymal tissue against the background of another pathology. Nephrosclerosis is more often diagnosed in adults. Children are rarely affected.
Main etiological factors
The reasons for the development of nephrosclerosis are numerous. Primary kidney shrinkage is caused by the following factors:
- hypertension;
- thromboembolism or thrombosis of the renal artery;
- kidney infarction;
- the presence of atherosclerotic plaques in the vessels of the kidney;
- violation of venous outflow;
- thinning of the cortex;
- atrophy of renal tubular cells.
The most common cause is primary arterial hypertension. It is characterized by a persistent increase in blood pressure from 140/90 mm Hg. and higher. Hypertension occurs in benign or malignant forms. In the first case, the elasticity of the walls of the renal arteries decreases. The latter narrow, which leads to impaired blood flow. This is how benign nephrosclerosis develops.
This pathology develops gradually over about 10 years. The malignant form of primary renal scarring is characterized by a more rapid progression and necrosis of the small vessels of the glomeruli. This leads to atrophy of renal tubular cells. A common cause of primary nephrosclerosis is heart attack.
This is a condition characterized by the death of individual parts of the organ as a result of acute impairment of renal blood flow. It is possible when the lumen of the arteries is blocked by a thrombus or embolus. The more infarction zones and the larger their size, the higher the risk of organ shrinkage. A secondary wrinkled kidney most often develops against the background of severe diabetes mellitus, late toxicosis of pregnancy, chronic forms of pyelonephritis and glomerulonephritis, tuberculosis and nephrolithiasis (urolithiasis).
In diabetes mellitus, nephropathy develops due to vascular damage. This leads to slow blood flow and sclerosis. In such patients, not only the kidneys, but also other organs (eyes, heart, adrenal glands) suffer. Nephrosclerosis can be the result of severe toxicosis during pregnancy. This is due to a disruption in the functioning of blood vessels against the background of disruptions in the central nervous system.
Signs
The attending physician should know the possible symptoms of kidney shrinkage. Their severity depends on the size of the area of nephron necrosis. The most common signs of kidney shrinkage are:
- excessive urine output (polyuria);
- decrease in diuresis to 500-800 ml per day;
- predominance of nocturnal diuresis (nocturia);
- lack of urination (with the death of 90% of nephrons);
- swelling;
- increased blood pressure;
- visual impairment;
- various types of bleeding (uterine, nasal, gastrointestinal);
- pain in the heart area;
- signs of cardiac asthma (shortness of breath, cold sweat, asthma attacks);
- rapid pulse;
- headache;
- brittle nails;
- nausea;
- vomit;
- weakness.
Such individuals have reduced immunity, which is manifested by regular respiratory diseases. A common symptom is nagging pain in the lumbar region. Wrinkling occurs in 2 stages. At the first stage, symptoms characteristic of the underlying disease are observed. With hypertension, this means high blood pressure, headache, nausea, and weakness. Diabetes is associated with polyuria, thirst, sweating, weight loss, and frequent urination.
In the second period, symptoms of chronic renal failure appear. They are caused by an increase in nitrogen compounds in the blood and intoxication of the body. Azotemia is manifested by lack of appetite, weakness, fatigue, itching, nausea, and vomiting. Due to kidney failure, the heart suffers. This manifests itself as attacks of angina pectoris with chest pain and cardiac asthma. Possible consequences of nephrosclerosis include blurred vision, including retinal detachment and swelling of the optic nerve.
Primary wrinkled kidney, macroscopic specimen
Arteriosclerosis –
a group of diseases characterized by thickening of the walls of the arteries and loss of elasticity.
Nosological forms:
atherosclerosis, sclerosis (post-inflammatory, etc.), Mönckeberg mediacalcinosis, arteriosclerosis and hyalinosis (with arterial hypertension, diabetes mellitus, etc.).
Atherosclerosis
is a chronic progressive disease manifested in focal thickening of the intima of the aorta and arteries of the elastic and muscular-elastic types due to the accumulation of lipoproteins and other blood components and the reactive proliferation of connective tissue.
The main local manifestation is an atherosclerotic fibrous plaque (atheroma),
leading to a narrowing of the lumen of the arteries, the development of aneurysms, or thrombus formation, resulting in
absolute or relative insufficiency of blood supply to the organ.
Unstable (easily vulnerable) atherosclerotic plaque
– 1) with a progressive increase in the lipid core and thinning of the tegmentum, 2) with hemorrhage into the necrotic core of the plaque, 2) with a pronounced inflammatory infiltrate, an abundance of blood vessels. The result is a rupture or tear of the fibrous cap, thrombosis in the area of ulceration, obstruction of the arterial lumen, thromboembolism or embolism with atheromatous masses.
Clinical and morphological forms of atherosclerosis (groups of independent nosological forms):
atherosclerosis of the aorta, coronary arteries of the heart, arteries of the brain, lower extremities, mesenteric and renal arteries.
Arterial hypertension
is a group concept for several syndromes and diseases characterized by a systolic blood pressure level of 140 mmHg. Art. or more, and (or) a diastolic blood pressure level of 90 mmHg. Art. or more, in people who are not receiving antihypertensive drugs.
Types of arterial hypertension:
by development mechanism: primary (hypertension) and secondary (symptomatic).
Secondary arterial hypertension:
neurogenic, endocrine, hypoxic (“metabolic”), hemic and mixed.
Hypertonic disease
(essential hypertension, hypertensive disease) is a chronic disease, the main manifestation of which is an increase in blood pressure.
Clinical and morphological forms of hypertension:
cardiac, cerebral, renal.
Options:
benign and malignant.
Coronary heart disease (CHD,
coronary heart disease
)
is a group of diseases leading to acute or chronic dysfunction of the heart, resulting from a relative or absolute decrease in the supply of arterial blood to the myocardium;
these are cardiac forms of atherosclerosis and hypertension
. The pathogenetic basis of IHD is the narrowing or obstruction of the coronary arteries of the heart by atherosclerotic plaques.
Classification of IHD:
acute forms
- variants of angina pectoris (clinical concept), sudden (acute) coronary death, acute (primary), recurrent and repeated myocardial infarction;
chronic forms
- diffuse small-focal (atherosclerotic) cardiosclerosis, large-focal (post-infarction) cardiosclerosis, chronic cardiac aneurysm.
Acute coronary syndrome
– a group concept that combines unstable angina and myocardial infarction.
List of drugs studied during the lesson (marked with the icon:
)
macropreparations
- atherosclerosis of the aorta with a parietal thrombus, gangrene of the lower limb (see Fig. 1-25, 1-26), ischemic cerebral infarction (see Fig. 1-16, 5-44, 29-15, 29-16), myocardial hypertrophy (concentric and eccentric), arteriolosclerotic nephrosclerosis, atherosclerotic nephrosclerosis, nephrocirrhosis (primary shriveled kidneys), atherosclerosis of the coronary arteries of the heart, unstable (easily vulnerable) atherosclerotic plaques of the coronary arteries of the heart, myocardial infarction (primary and repeated, different stages), large lesion new (post-infarction) cardiosclerosis, chronic cardiac aneurysm, diffuse small-focal (atherosclerotic) cardiosclerosis;
microslides
– aortic lipoidosis (see Fig. 2-33), aortic atherosclerosis, myocardial hypertrophy, arteriolosclerotic nephrosclerosis, atherosclerosis of the coronary arteries of the heart, myocardial infarction (different stages),
electron diffraction patterns
- aortic lipoidosis, arteriole spasm during hypertensive crisis, myocardial ischemia.
Rice. 15-1. Electron diffraction pattern. Atherosclerosis, stage of lipoidosis (experiment).
Free-lying lipoproteins in the intima (L), xanthoma cells: macrophage (Mph) and smooth muscle cell (SMC), loaded with cholesterol (Chl). KlV – collagen fibers (from [2]).
a b
Rice. 15-2. Macropreparations (a, b). Atherosclerosis of the aorta with a parietal thrombus.
Intima of the aorta with lipid spots of yellow color, atherosclerotic fibrous plaques rising above the surface of the intima, dense consistency, yellowish-white color, complicated lesions - ulcerations, parietal thrombi with a characteristic corrugated surface (1), calcification (a - preparation I.N. Shestakova)
.
See also fig. 5-4
a b
Rice. 15-3. Microslides (a, b). Atherosclerosis of the aorta,
a - atherosclerotic plaque with a large lipid core with cholesterol crystals and foam cells (1), covered on top with a fibrous cap, lymphomacrophage infiltration of connective tissue growths (a), b - intracellular (in smooth muscle cells and macrophages - foam cells) and extracellular accumulation lipids in the thickened intima of the aorta (lipids are yellow-orange); b – Sudan III staining, x 100 (see also Fig. 2-32, 2-33).
Rice. 15-4. Microslide. Arteriosclerosis (mediacalcinosis) of Mönckeberg.
Idiopathic calcification (deposits of calcium salts of blue-violet color) and sclerosis of the middle shell (media) of the medium-sized artery of the anterior mediastinum (systemic mediacalcinosis of the walls of arteries of unknown etiology in the elderly). The lumen of the artery is not narrowed, x 60.
Rice. 15-5. Macropreparation. Concentric myocardial hypertrophy (stage of hypertrophy compensation).
The size and weight of the heart are increased, the wall is thickened, and the volume of the papillary and trabecular muscles of the left ventricle is increased. The cavity of the left ventricle is not dilated, the myocardium has a dense consistency, reddish-brown color (preparation by N.O. Kryukov). See. also Fig.9-1.
Rice. 15-6. Macropreparation. Eccentric myocardial hypertrophy (stage of decompensation of hypertrophy).
The size and weight of the heart are increased, the wall is thickened, and the volume of the papillary and trabecular muscles of the left ventricle is increased. The cavity of the left ventricle is expanded (dilated), the myocardium has a flabby consistency, clayey appearance, with signs of fatty degeneration (“tiger heart”), preparation by I.N. Shestakova (see also Fig. 9-2).
a b
Rice. 15-7. Microslides (a, b). Eccentric myocardial hypertrophy (stage of decompensation of hypertrophy),
a — cardiomyocytes and their nuclei are increased in size, the nuclei of some cells are hyperchromic, the stroma is moderately sclerotic; b – when stained with Sudan III, accumulations of orange lipids are visible in some cardiomyocytes; b – Sudan III staining, a – x 200, b – x 400 (see also Fig. 2-15, 9-3).
Rice. 15-8. Electron diffraction pattern. Arteriole spasm during hypertensive crisis.
The lumen of the vessel (Ps) is narrowed, endothelial cells (En) are pressed against each other, interendothelial spaces are not detected. The basement membrane (BM) is corrugated and split. The internal elastic membrane (IM) is fragmented. SMC – smooth muscle cell (from [2]).
a b
Rice. 15-9. Macropreparations (a, b). Arteriolosclerotic nephrosclerosis.
The kidneys are reduced in size, compacted, with a fine-grained surface, small cysts with transparent contents, on the section the cortex (especially) and the medulla are thinned, the volume of fatty tissue at the renal hilum is increased (see also Fig. 2-53).
a b
Rice. 15-10. Microslides (a, b). Arteriolosclerotic nephrosclerosis.
Nephrosclerosis in benign arterial hypertension: 1 - hyalinosis and sclerosis of arterioles, 2 - glomerular hyalinosis (preserved - compensatory enlarged), 3 - stromal sclerosis, 4 - protein degeneration and atrophy of the convoluted tubule epithelium; x 100. (See also Fig. 2-54).
a b
Rice. 15-11. Microslides (a, b). Hyperplastic arteriolosclerosis (a) and necrotizing arteriolitis (b) of the kidneys in malignant arterial hypertension;
a — sclerosis of the walls of arterioles (they look like onion peels), the lumen of the arteriole is significantly narrowed; b – eosinophilic foci of fibrinoid necrosis of the wall of a sclerotic and hyalinized arteriole—necrotizing arteriolitis; - x 200.
a b
Rice. 15-12. Macropreparations (a, b). Atherosclerotic nephrosclerosis.
The kidneys are reduced in size, compacted, with many rough, star-shaped scar retractions (post-infarction scars). On the section, the cortex (especially) and medulla are unevenly thinned, the volume of fatty tissue at the renal hilum is increased.
a b
Rice. 15-13. Macropreparations (a, b). Nephrocirrhosis (primarily shriveled kidneys).
The kidneys are significantly reduced in size, deformed and compacted, with a fine-grained surface and many coarse, star-shaped scar retractions, small cysts with transparent contents, on the section the cortex and medulla are sharply narrowed, the volume of fatty tissue of the renal hilum is increased (preparations by I.N. Shestakova ).
Rice. 15-14. Macropreparation. Stenosing atherosclerosis of the coronary arteries of the heart.
Atherosclerotic fibrous plaques of yellow color in a longitudinally dissected coronary artery (see also Fig. 5-50).
a b
Rice. 15-15. Macropreparations (a, b). Unstable (easily vulnerable) atherosclerotic plaques of the coronary arteries of the heart – 1;
a – atheromatosis of atherosclerotic plaques is expressed, fibrous caps are thinned; b – rupture of the cover of an unstable atherosclerotic plaque with release of atheromatous masses into the lumen of the coronary artery; b – preparation by N.O. Kryukov (see also Fig. 5-51).
a b
Rice. 15-16. Macropreparations (a, b). Unstable (easily vulnerable) atherosclerotic plaques of the coronary arteries of the heart – 2.
Hemorrhages into atherosclerotic plaques (a, b) with destruction of the fibrous cap (b). Preparations by N.O. Kryukov.
Rice. 15-17. Macropreparation. Obstruction of the coronary artery of the heart by atheromatous masses due to rupture of the cap of an unstable atherosclerotic plaque.
The lumen of the coronary artery is obstructed by loose yellow masses.
a b
Rice. 15-18. Macropreparations (a, b). Thrombosis of the coronary arteries of the heart.
Obstructive thrombi of the coronary arteries of the heart with their stenotic atherosclerosis. See. also fig. 5-10.
a b
Rice. 15-19. Microslides (a, b). Atherosclerosis of the coronary arteries of the heart.
Unstable atherosclerotic plaques with large lipid cores, foci of calcification (blue-violet color), necrosis and thinning of the fibrous cap; x 60 (b - preparation by N.O. Kryukov).
Rice. 15-20. Microslide. Lipids in atherosclerotic plaque of the coronary artery of the heart.
Intracellular (in smooth muscle cells and macrophages - foam cells) and extracellular accumulation of lipids in the atherosclerotic plaque, colored yellow-orange in vessels III; staining with Sudan III, x 140 (preparation by L.V. Kaktursky).
Rice. 15-21. Microslide. The head of the thrombus in the area of rupture of the fibrous cap of the atherosclerotic plaque of the coronary artery of the heart (1);
x 60 (preparation by N.O. Kryukov).
a b
Rice. 15-22. Macropreparations (a, b). Implanted stents in the coronary arteries of the heart with stenosing atherosclerosis.
Stents (arrows) restored the patency of the coronary arteries of the heart in places of their stenosis or occlusion by atherosclerotic plaques.
a b
Rice. 15-23. Macropreparations (a, b). Shunts of the coronary arteries of the heart for stenosing atherosclerosis,
a – aorto-coronary bypass, b – mammocoronary anastomosis and aorto-coronary bypass.
a b
Rice. 15-24. Macropreparations (a, b). Thrombosis of aorto-coronary bypass grafts.
Red occlusive thrombi of coronary artery bypass grafts (arrows).
Rice. 15-25. Macropreparation. Myocardial infarction less than 1 day old. Macroscopic test for myocardial ischemia with potassium tellurite.
The focus of myocardial ischemia after incubation in a solution of potassium tellurite remained light (arrows), the intact myocardium turned black (preparation by Filippov and L.V. Kaktursky). See also fig. 5-45.
Figure 15-26. Electron diffraction pattern. Myocardial ischemia (myocardial infarction about 3 hours old).
Vacuolization and swelling of mitochondria (M) with clearing of their matrix and destruction of cristae. Dilation of the tubules of the sarcoplasmic reticulum (SR). Mf – myofibrils (from [1]).
a b
Rice. 15-27. Microslides (a, b). Myocardial infarction, about 6 hours old (ischemic stage of myocardial infarction).
Histological examination (a) shows only a wavy course, contractural changes and fragmentation of cardiomyocytes, stromal edema and vascular congestion. The method of polarization microscopy (b) reveals cardiomyocytes in a state of necrosis (light); b — polarization microscopy method; x 100 (see also Fig. 5-46).
a b
Rice. 15-28. Macropreparations (a, b). Acute (primary) myocardial infarction about 1 (a) and 2 (b, c) days old.”
A large transmural focus of necrosis of irregular geometric shape, lighter than the intact myocardium, surrounded by small punctate hemorrhages, more pronounced on the 2nd day (preparations by N.O. Kryukov).
a b
Rice. 15-29. Macropreparations (a, b). Acute (primary) myocardial infarction about 3 days old.
A large transmural focus of necrosis of irregular geometric shape, variegated appearance, yellowish or greenish-gray color with pinpoint hemorrhages, flabby consistency, sinks into the section, surrounded by a red hemorrhagic rim (b - preparation by I.N. Shestakova). See also fig. 1-22, 5-45.
a b
Rice. 15-30. Microslides (a, b). Myocardial infarction about 3 days old (necrosis stage).
In the necrosis zone, cardiomyocytes are fragmented, partially lysed, do not contain nuclei, many with bright eosinophilic cytoplasm, others, on the contrary, are weakly stained. Pronounced leukocyte infiltration, congestion of the microcirculatory bed with minor hemorrhages; x 100 (see also Fig. 1-23).
a b
Rice. 15-31, a, b. Macropreparations “Acute (primary) myocardial infarction about 12 (a) and 15 (b) days old.”
Large transmural focus of necrosis of irregular geometric shape, variegated appearance, with foci of yellowish-gray and red color, flabby consistency, sinking in the section, with growths of granulation tissue of grayish-red color and with layers of mature connective tissue of gray color (preparations by N.O. Kryukov ).
a b
Rice. 15-32. Microslides (a, b). Myocardial infarction about 7 days old (stage of necrosis with the beginning of organization).
In the zone of necrosis, disintegration, lysis and resorption of necrotic, brightly eosinophilic cardiomyocytes by macrophages, leukocyte-macrophage infiltration is pronounced. From the zone of demarcation inflammation, granulation (young connective) tissue grows into the focus of necrosis; x 100 (see also Fig. 5-49, 9-29).
a b
Rice. 15-33. Macropreparations (a, b). Acute (primary) myocardial infarction, complicated by the development of an acute cardiac aneurysm.
In the area of the apex of the heart there is a spherical protrusion; on the section, the wall of the left ventricle in this place is thinned, represented by transmural mottled yellow-red foci of necrosis. From the endocardium – red parietal thrombi (b). Preparations by N.O. Kryukov.
Rice. 15-34. Macropreparation. Fibrinous pericarditis in acute (primary) myocardial infarction complicated by acute cardiac aneurysm.
On the epicardium there are dull yellowish and reddish fibrin filaments and films, easily detachable without damaging the serous membrane.
a b
Rice. 15-35. Macropreparations (a, b). Acute (primary) myocardial infarction, complicated by myomalacia and rupture of the left ventricular wall
; a — preparation by I.N. Shestakova.
a b
Rice. 15-36. Macropreparations (a, b). Hemotamponade of the pericardial cavity due to rupture of the wall of the left ventricle during myocardial infarction.
Rupture of the wall of the left ventricle (a), blood clots and dark liquid blood in the pericardial cavity (a, b); a – preparation by A.N. Kuzin and B.A. Kolontarev (see also Fig. 4-33).
a b
Rice. 15-37. Macropreparations (a, b). Large-focal (post-infarction) cardiosclerosis.
The size and weight of the heart are increased, the walls are thickened, the volume of the papillary and trabecular muscles of the left ventricle is increased, the heart cavities are expanded, the myocardium has a flabby consistency, and a clayey appearance on the section (eccentric myocardial hypertrophy). In the wall of the left ventricle there is a large transmural scar of irregular geometric shape, white color, dense consistency (1); b – preparation by N.O. Kryukov). See also Figure 9-9.
a b
Rice. 15-38. Microslides (a, b). Large-focal (post-infarction) cardiosclerosis.”
In the myocardium there is a large focus of scar (mature connective) tissue, with weakly expressed lymphomacrophage infiltration, a small number of siderophages, and full-blooded vessels. Hypertrophy of perifocally located cardiomyocytes is pronounced. When stained according to Van Gieson, connective tissue is colored red, cardiomyocytes are yellow; b - van Gieson picrofuchsin staining, a - x 100, b - x 400 (see also Fig. 9-10).
a b
Rice. 15-39. Macropreparations (a, b). Repeated myocardial infarction about 3 days ago.
Large foci of necrosis of irregular geometric shape, variegated appearance, yellowish-gray color with red spots, flabby consistency, sunken in the section, surrounded by a red hemorrhagic rim (1). Nearby there are large, irregularly shaped post-infarction scars of a grayish-white color (2). Preparations by N.O. Kryukov (see also Fig. ...).
a b
Rice. 15-40. Macropreparations (a, b). Chronic cardiac aneurysm - 1.
The size and weight of the heart are increased mainly due to its left ventricle. Part of its wall forms a sac-like protrusion (aneurysm). The epicardium in the area of the aneurysm is often sclerotic. As a result of fibrinous pericarditis, pericardial adhesions may form (b).
a b
Rice. 15-41. Macropreparations (a, b). Chronic cardiac aneurysm - 2.
The size and weight of the heart are increased mainly due to its left ventricle. Part of its wall forms a sac-like protrusion (aneurysm). Its wall is represented by dense connective (scar) tissue (post-infarction transmural scar), thinned, the endocardium and epicardium are sclerotic, grayish-white in color. The myocardium of the left ventricle outside the aneurysm is thickened (hypertrophied).
a b
Rice. 15-42. Macropreparations (a, b). Parietal thrombus in the cavity of a chronic cardiac aneurysm.
The size and weight of the heart are increased mainly due to its left ventricle. Part of its wall forms a sac-like protrusion (aneurysm). Its wall is represented by dense connective (scar) tissue (post-infarction transmural scar), thinned, the endocardium and epicardium are sclerotic, grayish-white in color. The myocardium of the left ventricle outside the aneurysm is thickened (hypertrophied). In the cavity of a chronic aneurysm, parietal thrombi often form (and - preparation by I.N. Shestakova). See. also Fig. 5-9.
Rice. 15-43. Macropreparation. Diffuse small-focal (atherosclerotic) cardiosclerosis.
The size and weight of the heart are increased mainly due to its left ventricle. The walls of the left ventricle are thickened. On the section in the myocardium there are many thin whitish connective tissue foci and layers (preparation by N.O. Kryukov).
| | | next lecture ==> | |
| Anemia. Polycythemia. Tumors of hematopoietic and lymphoid tissues | | | Finding individuality from the first days of life |
Treatment of pathology
A wrinkled kidney, the treatment of which must be carried out strictly under the supervision of a doctor and only according to his prescriptions, requires a thorough approach to therapy.
A wrinkled kidney, the treatment of which must be carried out strictly under the supervision of a doctor and only according to his prescriptions, requires a thorough approach to therapy. In the early stages of shrinkage, the patient may be prescribed a diet for a shriveled kidney. In this case, diet therapy should be based on the identified metabolic failures in the patient’s body. Basically, the principles of diet therapy look like this:
- Critical restriction of salt in the patient's diet. 1-3 grams per day is acceptable.
- Limiting fluid intake. Together with the first courses, the volume should be no more than 1.5 liters. This tactic helps prevent edema and hypertension.
- Limiting the consumption of animal protein. In this case, it is advisable to switch to soy and vegetable protein. It is possible to combine vegetable protein with keto acid or essential amino acids.
- Reduced phosphorus intake into the body. Moreover, if you have to increase the protein concentration, it is forbidden to introduce foods containing phosphorus into the diet (sea fish, fatty meats, milk, nuts and cocoa).
- Compliance with caloric intake. There should be at least 30 kcal per kg of weight of an elderly patient. Moreover, if the patient moves and has at least some exercise, then the calorie content is increased to 40 kcal/kg of weight. If the intake of protein in the diet is extremely reduced, then the daily calorie content should reach 48 kcal/kg.
- Introduction of polyunsaturated acids into the diet in sufficient quantities. In this case, it is good to take fish oil.
- Control over the introduction of magnesium and potassium into the diet. Products containing them are soaked in water for at least 30 minutes before use.
- Taking multivitamins. In this case, it is better to prescribe water-soluble complexes, since fat-soluble ones are retained in the tissues of the patient’s body.
- Monitoring hemoglobin levels. If necessary, the patient is prescribed erythropoietin.
Eligible Products
Acceptable products for pathology - salt-free bakery products
- Salt-free bakery products;
- Lean meats prepared exclusively by boiling or steaming;
- Cereal porridges;
- First courses with vegetable broth;
- Fruits and vegetables in any form;
- Oils (vegetable, unsalted butter);
- Juices, fruit compotes, tea.
Prohibited products:
- First courses with fish and meat broths;
- Meat and fish of fatty varieties;
- Mushrooms in any form;
- Marinades, pickles, smoked meats;
- All spicy foods and seasonings;
- Parsley, asparagus, rhubarb, radish, onion/garlic, spinach and sorrel;
- Chocolate and cocoa;
- Coffee.
Surgical treatment
If the drying out of the urinary organ is already at the last stage, then only surgical intervention (kidney removal) is indicated. In this case, there is simply nothing to treat. The method of performing the operation is chosen by the doctor depending on the patient’s condition:
- Endoscopy. The kidney is removed through one small puncture in the lumbar region.
- Laparoscopy. Removal of the organ through several small punctures in the peritoneum.
- Strip operation. Complete dissection of tissue on the way to the kidney from the lumbar side.
Treatment
The question of what to do when a kidney shrinks worries the vast majority of those who are faced with nephrosclerosis. The answer to this is clear - the disease must be treated immediately. However, treatment should be carried out taking into account both the symptoms of the disease and the reasons that led to its development.
Thus, nephrosclerosis, accompanied by increased blood pressure without renal failure, is treated with a salt-free diet. The patient is recommended:
- limiting the amount of salt and liquid consumed;
- taking blood pressure lowering medications, vitamins, and medications whose active ingredients are polyunsaturated acids.
If renal failure develops, the doctor can discontinue blood pressure-lowering medications that interfere with blood flow in the parenchyma and reduce the functionality of the organ.
If azotemia is detected, patients are recommended to eat a diet that limits the consumption of animal proteins (any meat and broths made from it) and is aimed at reducing the level of nitrogen toxins, and if the level of cholesterol in the blood increases, patients are prescribed statins.
With the development of unilateral pathology (shrinkage of one kidney while the structures of the second are intact), the restoration of lost functionality is carried out at the expense of a healthy organ.
If both kidneys shrink and renal failure develops, the patient may need:
- embolization of the renal arteries and nephrectomy (subsequently such patients require hemodialysis);
- organ transplantation from a donor.
For anemia that has developed as a result of dialysis, patients are prescribed artificial erythropoietin preparations.
Characteristic signs of pathology
Most often, nephrosclerosis is diagnosed accidentally during examination for other pathologies or during a routine examination.
Interestingly, difficulties also arise due to the activation of the compensatory functions of the second kidney (that is, it begins to work with double activity, and the person does not feel any deviations). When pathological processes have already reached a severe stage, the following symptoms may be observed:
nagging dull pain in the lumbar region; drowsiness and weakness; frequent urination at night; puffiness appears on the face in the morning; increased blood pressure, which is difficult to normalize with medications; Foreign impurities and blood particles are visible to the naked eye in the urine.
Nonspecific symptoms may occur in the form of frequent headaches or cardiac dysfunction.
If at least several of the listed signs are detected, you must contact a nephrologist and undergo an examination.
What to do for nephrosclerosis
At the initial stage, treatment of a wrinkled kidney is carried out comprehensively. Includes taking medications and following a diet. If conservative treatment is ineffective, surgery is prescribed.
Surgical intervention
Nephrectomy is a surgical intervention that involves removing part of the kidney or the entire organ with significant shrinkage. It is carried out using the following methods:
- Laparoscopy - during the operation, the surgeon makes 3 punctures in the tissues of the abdominal cavity, through which special instruments are inserted for surgical manipulations. The operation is monitored using an endoscope equipped with a camera, which is also inserted through a puncture in the skin.
- Percutaneous nephrectomy is a surgical procedure in which a urologist surgeon removes part of an organ through minor punctures in the lumbar region.
- Open abdominal surgery is used extremely rarely. Removal occurs by layer-by-layer incision of the tissues of the abdominal wall.
Drug treatment
Drug therapy is aimed at relieving symptoms, which can improve the patient’s general condition and prevent the progression of kidney shrinkage. For this purpose the following are appointed:
- anticoagulants – prevent blood clotting and thrombosis, which allows normalizing the functioning of the cardiovascular system (Heparin, Fraxiparin, Warfarin);
- potassium-containing agents to restore metabolic processes in the body (Panangin, Asparkam);
- antiplatelet agents – restore normal functioning of the vascular system and heart muscle, prevent the formation of blood clots (Pentoxifyline, Curantil, Trental);
- vitamin complexes and iron-containing medicines to restore the vitamin-mineral balance and the content of microelements (Vitrum, Duovit, Ferrum Lek);
- sorbents cleanse the body of toxic compounds (Polysorb, Enerosgel);
- ACE inhibitors or angiotensin receptor blockers to reduce intrarenal and blood pressure (Captopril, Vasopren);
- antispasmodic and analgesic drugs – relieve pain and eliminate vasospasm;
- uroseptics for the treatment and prevention of infectious pathologies;
- antibacterial drugs – suppress the activity of pathogenic flora in the infectious-inflammatory etiology of nephrosclerosis;
- diuretics - to restore diuresis (Indapamide, Furosemide).
Diet
To reduce the load on the kidneys and restore their normal functioning, treatment table No. 7 is prescribed, in accordance with the recommendations, which requires:
- reduce daily salt intake to 3 g;
- drink no more than 1.5 liters of liquid per day;
- limit the amount of animal protein;
- reduce phosphorus intake;
- reduce caloric intake;
- consume a sufficient amount of polyunsaturated acids;
- restriction of magnesium and potassium in the diet.
The patient can eat unleavened baked goods, lean meat and fish, cereals, vegetables, fruits, vegetable broths, oils of vegetable and animal origin, juices, compotes, teas. You should avoid fatty meat and fish, mushrooms and broths based on them, spices, seasonings, herbs, cocoa-containing products, and caffeine.
As a rule, diagnosing a wrinkled kidney has an unfavorable prognosis, which is caused by a disruption in its functioning. The pathology is treated surgically; in the initial stages, symptomatic therapy is acceptable.
Kidney infarction
The concept of heart attack still has strong associations with the heart. However, statistics over the past few decades show a rapid increase in the number of cases of renal infarction. This is explained by the spread of infectious diseases, the presence of bad habits among a huge number of people, as well as chronic diseases.
What it is
Kidney infarction is a urological pathology in which, as a result of impaired blood supply (ischemia) to the organ, tissue death occurs. As a rule, the reason for blocking the lumen in the trunk of the renal artery is a parietal thrombus of the atrium or ventricle. This type of heart attack is especially dangerous for people who have lost one kidney or already have serious diseases of the body’s filtration apparatus.
Forms of the disease
Depending on the causes, there are three forms of renal infarction:
- ischemic, or arterial;
- hemorrhagic or venous;
- combined (combines signs of arterial and venous);
- uric acid.
The first form is typical for older people, and the latter for newborns.
Causes
As a rule, an ischemic renal infarction (also called a “white” infarction) is the result of a clot blocking the artery leading to the kidney. The blood supply to the organ suddenly stops or slows down, and the reverse flow of blood becomes impossible. First of all, people suffering from cardiovascular diseases are at risk, which include:
Causes of pain in the kidney area
- mitral valve disease;
- atrial fibrillation;
- myocardial infarction;
- atherosclerosis;
- periarteritis nodosa;
- ascending aortic thrombosis;
- thromboembolism;
- DIC (disseminated intravascular coagulation) - expressed by increased thrombus formation in the vessels;
- infective endocarditis;
- connective tissue diseases;
- sickle cell anemia;
- aneurysm;
- thrombosis of the central vein of the adrenal glands.
Due to a blood clot, blood flow suddenly stops and an organ infarction may develop.
Those who have undergone surgery on the renal artery may also develop ischemic (anemic). Subsequently, a blood clot forms at the site of the injury, which blocks the blood flow to the organ.
Very rare, but there are cases when a blood clot develops after angiography - a study that is used specifically to diagnose kidney infarction, as well as coronary angioplasty - an operation to dilate blood vessels.
There are situations when, during an open operation to remove a tumor or stop bleeding, the surgeon deliberately provokes a kidney infarction.
Tumors that put pressure on the vessels and arteries of the kidney, radiation and chemotherapy, bacterial endocarditis (damage to the inner lining of the heart, aortic and heart valves) are also on the list of causes of renal infarction.
Ischemic renal infarction is called “white” because a microscopic specimen of the organ looks like a triangle or a cone of white color and dense consistency, with a bright red border around the perimeter. This is dry coagulative necrosis. The area of damage is directly related to the size of the vessel: if it is a renal artery, then its blockage results in total necrosis, if smaller arteries, the cortical layer or the entire tissue of the organ dies.
Hemorrhagic, or “red”, infarction occurs in rare cases. It is characterized by a violation of the outflow of blood, which causes its accumulation in the organ. The blood stagnates, and red blood cells begin to penetrate the walls of blood vessels. The microscopic specimen of the organ is distinguished by its rich red color and clear boundaries.
Uric acid renal infarction is diagnosed in a large number of newborns. The reasons are birth stress and the restructuring of metabolic processes. Uric acid accumulates in the hyaline casts that fill the urinary tubules. But this is a physiological norm, and after a certain amount of time the process of urine excretion returns to normal. Cases where uric acid infarction still occurs ten days after the birth of the child are considered pathological.
Less commonly, this type is diagnosed in adults, but then the cause is serious pathological processes that are accompanied by tissue breakdown.
When small vessels are clogged and the affected area is small, a person may not notice anything, that is, there are no symptoms of a kidney infarction.
If the lumen of a large vessel has been closed, the patient will experience the following symptoms:
- pain in the lumbar region;
- high blood pressure;
- increased body temperature (usually up to 38 degrees Celsius);
- chills;
- nausea or vomiting;
- pain on palpation.
Venous necrosis of the organ begins slowly and is severe. The painful process is complemented by the release of blood clots in the urine, which can even interfere with the removal of fluid from the bladder. The organ is increased in size.
Arterial necrosis always begins suddenly. The symptoms are similar to those listed above, but the amount of blood during urination is insignificant, and palpation is painless.
Blood in the urine is one of the signs of a kidney infarction
Symptoms of uric acid infarction are:
- rare urination;
- change in urine color (it becomes dark and cloudy).
The appearance of these signs in a baby should not be frightening, since this does not worsen his well-being, but an adult should be very concerned about this state of affairs, since it signals serious problems in the body.
Diagnosis of the disease is considered difficult, since its symptoms are similar to those of other pathologies (peritonitis, renal colic, dissection of the aortic aneurysm), so the patient is prescribed a comprehensive examination, including:
- visual inspection;
- a survey about the location, nature of the pain, as well as the time of its onset;
- general blood and urine tests, which in the latter should reveal an increase in protein levels and the presence of blood. Hematuria and proteinuria in advanced form are clearly visible even with the naked eye in urine samples. In the blood, a general analysis will reveal moderate leukocytosis;
- cytoscopy. It is prescribed for hematuria, if its origin is not entirely clear, and helps to exclude glomerulonephritis - inflammation of the capillary glomeruli that separate fluid from the blood, which upon further processing becomes urine;
- a biochemical analysis of blood and urine is necessary to detect an increase in the level of the hormone lactate dehydrogenase, which is involved in the process of glucose metabolism;
- coagulogram - a blood test to determine the quality of clotting;
- ultrasound examination of the organ;
- computed tomography;
- Dopplerography;
- angiography (performed less and less often, and only when there is no obstruction to blood flow);
- radioisotope research;
- radiography with contrast.
Dopplerography allows you to see exactly where the vessel is blocked
In the case of uric acid infarction of the kidney in an infant, treatment consists of increasing the amount of fluid consumed by the child. But only a doctor can determine and prescribe the required volume.
In case of ischemic infarction, hospitalization of the patient is necessary. Previously, treatment consisted only of surgery, but today there are effective drug regimens that can treat the disease without the use of a scalpel.
The treatment regimen includes the use of drugs that reduce blood clotting and thus prevent the formation of blood clots. If the presence of a blood clot is detected, the patient is given medications that dissolve the dangerous clot within several hours after a kidney infarction. To restore coagulation later, direct-acting anticoagulants are prescribed.
In the first hours after a heart attack (which is why it is important to see a doctor as soon as possible), balloon angioplasty is performed: a catheter is inserted into the femoral artery and advanced to the part of the kidney where the blocked artery is located. The balloon is then inflated and eliminates the clot. Blood circulation is instantly restored.
In case of severe pain, the patient is given narcotic painkillers, since conventional ones are ineffective.
To restore kidney function, streptokinase thrombolytics are used, but only when there is no hematuria and no blood in the urine.
After balloon angioplasty, the kidney receives the required volume of blood
In case of arterial infarction, bed rest is prescribed. Kidney function will improve with effective therapy, but, unfortunately, the patient’s internal organs will no longer function at the same level. Therefore, from now on, a person will need to carefully monitor his health.
Complications
After a heart attack, the kidney cannot fully perform its functions. In addition, there is a risk of developing nephrosclerosis or acute failure.
Also, primary urine may stop accumulating in the organ, which will disrupt metabolism and begin intoxication of the body.
Prevention
To reduce the likelihood of a renal infarction, you first need to adjust your nutrition system: reduce the consumption of fatty, salty, spicy foods.
It is recommended to include in your diet foods that help strengthen the walls of blood vessels. These are: dried fruits, apples with honey, rosehip decoction, carrot juice, cranberries, herbal preparations (their composition must be agreed with the attending physician).
If a patient has atherosclerosis, he is required to be prescribed medications containing acetylsalicylic acid, which thins the blood and helps prevent blood clots. An important point: it is contraindicated for people with stomach ulcers.
You shouldn’t test your body’s strength and expect it to “go away on its own.” One disease has different outcomes for different people, so at the first symptoms of a kidney infarction, you should consult a doctor and start treatment as soon as possible. You also need to monitor your diet and the amount of salt you consume.
2pochki.com
Forecasts
Despite the fact that nephrosclerosis cannot be cured, it is possible to stop the development of the disease and eliminate the accompanying manifestations. However, this must be done immediately after the first symptoms appear - only then will the treatment be effective.
- Analysis of the history of the disease and complaints - when (how long ago) for the first time and what exactly the symptoms appeared, how they developed over time, whether the patient consulted a doctor, what examination was carried out and with what results.
- Analysis of the life history - the presence of chronic kidney diseases, bad habits, any diseases of the genitourinary system (including sexually transmitted diseases), what are the working and living conditions (for example, frequent drafts).
- Analysis of family history - whether kidney disease or cancer occurred in close relatives of the patient.
- Medical examination and palpation (feeling) of the kidney area. Allows you to detect pain, changes in the skin (for example, redness, rashes) in the kidney area.
- Laboratory methods to determine signs of inflammation in the body: general urine analysis;
- general blood analysis;
- blood chemistry.
- Ultrasound examination (ultrasound) of the kidneys - examination of organs and tissues using ultrasonic waves (sound vibrations of superaudible frequency);
A consultation with a urologist is also possible.
Description of drugs in Lesson No. 01.02
Description of drugs in Pathological Anatomy in Lesson No. 1,2
(This is an indicative description, not a cathedral one, some drugs may be missing, as is the description of previous years)
LESSON No. 1 HISTORY OF THE DEPARTMENT OF PAT. ANATOMY OF MMA NAMED AFTER I.M.SECHENOV
See lectures
LESSON No. 2 NECROSIS. APOPTOSIS.
Electronogram No. 20 ISCHEMIC INFARCTION OF THE SPLEN
There is swelling of mitochondria with destruction of the crypts, with the appearance of calcium deposits on them. Destruction of lysosomes.
Microslide No. 7 NECROSIS OF THE EPITHELIUM OF THE CONVOLVED PROXIMAL AND DISTAL TUBULES OF THE KIDNEY. HEMATOXYLIN-EOSIN STAINING
Distal prox tubules are unchanged. The epithelium and glomeruli contain nuclei. The cytoplasm is coagulated and homogeneous in some places. Destruction of the basement membrane (tubulorrhexis) is observed. Karyopyknosis, karyolysis, and plasmorrhexis are noted. The capillaries of the glomerular loop are anemic, and the vessels of the medulla of the kidney are full-blooded
Microslide No. 6 ISCHEMIC RENAL INFARCTION. HEM COLORS. – EOD.
The necrosis zone is represented by structureless masses, surrounded by a zone of demarcation inflammation, represented by full-blooded vessels with dilated lumens and polymorphonuclear leukocytes. In the focus of necrosis, the tissue structure is disturbed, the nucleus is not stained, with signs of karyopyknosis, karyorrhexis, and karyolysis.
Microslide No. 8 NECROSIS OF LYMPH FOLLICULS. NODES (SURROUNDING GEM.-EOZ.)
A homogeneous structureless mass is determined in the center of the follicle. Along the periphery there are single lymphocytes of small sizes (as part of karyopyknosis). There are many randomly located clumps of formatin (karyorrhexis)
Microslide PANCREONECROSIS (OCR. HEM.-EOS.)
The glandular tissue is represented by a structureless mass, containing single nuclei in the composition of karyopyknosis. Contains chromatin clumps
Microslide No. 215 ISCHEMIA ZONE IN THE MYOCARDIUM. CHIC REACTION.
The presence of glycogen - cardiomyocytes - crimson areas. Lack of glycogen - light areas.
Macro specimen ISCHEMIC INFARCTION OF THE SPLEN
The shape and dimensions have not been changed. The color is heterogeneous - in general it is brown-red, but from the gate to the periphery of the organ there is a 1-2 cm strip of paler color. The focus of necrosis is triangular in shape, dense in consistency, the base faces the capsule. On the capsule in the area of the infarction there are rough deposits of fibrin. D-z: Acute ischemic infarction of the spleen
Macroscopic specimen of BRAIN INFARCTION. FOCUS OF GRAY SOFTENING.
The lesion is located in the occipital region of the left hemisphere, grayish in color, irregular in shape, flabby consistency. Occurred due to a blood clot or embolism of cerebral vessels.
Macro specimen of GANGRENE TOE
Dry gangrene. The fabrics are black (due to iron sulfide deposits). Reduced in volume, with a well-defined zone of demarcation inflammation.
Macro-drug of GUNS GANGRENE
Gangrene is wet. The intestinal wall is thickened, edematous, flabby consistency, black-red in color. The serous membrane is dull with fibrin deposits. Thrombosis of the superior mesenteric artery.
Macrodrug TUBERCULOSIS LYMPH. KNOTS
In the lymph area there is a zone of caseous (cheesy) necrosis. Yellowish-gray color, dense consistency, crumbling.
Macropreparation PETRIFICATIONS IN THE LUNG (for tuberculosis)
Round shape, whitish-gray color, rocky density (due to calcium deposition)
studfiles.net
Side effects of the pathology
Against the background of a developing pathological process, which leads to chronic renal failure, the patient's body's metabolic processes are disrupted.
Against the background of a developing pathological process, which leads to chronic renal failure, the patient's body's metabolic processes are disrupted. Namely:
- Protein metabolism disorder. The patient's body suffers from azotemia - saturation with protein breakdown products.
- Hormonal disbalance. Lack of insulin and somatostatin lead to increased protein breakdown.
- Disturbance of carbohydrate metabolism. In this case, glucose is not utilized normally.
- Failure in fat metabolism. In this case, atherosclerotic changes will not keep you waiting.
- Failures in water-electrolyte balance and mineral metabolism disorders. One and the other are closely interconnected. This may be due to excess concentrations of phosphorus, calcium, magnesium and other trace elements in the body.
Recommended diet for illness
A salt-free diet involves excluding the following foods from consumption: meat, fish, citrus fruits. Hot, sour, salty and spicy foods are prohibited. It is also necessary to completely abandon coffee drinks and pure coffee, smoked meats and sausages, chocolate, sorrel, onions and garlic, spinach and asparagus.
It is necessary to control the daily volume of fluid. It should not exceed one and a half liters, including first courses.
Consumption of animal protein should be kept to a minimum. Ideally, it should be replaced with vegetable or soy. The calorie content of food should be high, containing polyunsaturated acids. Consumption of foods containing phosphorus, potassium and magnesium should be reduced.
Disease prevention
To save yourself from the possible development of kidney infarction, it is necessary to promptly and efficiently treat the diseases that cause it. Provoking pathologies include:
- atherosclerosis;
- myocardial infarction;
- heart defects.
It is important to constantly monitor blood pressure levels if you are prone to vascular kidney damage. Before starting treatment, you should consult with your doctor, who, if necessary, will help you choose therapy so that it comprehensively eliminates all possible risks. In addition, you need to eat right, lead an active lifestyle and give up all bad habits.
Clinical picture of the pathology
As a rule, the symptoms of the pathological process are expressed in lower back pain
As a rule, the symptoms of the pathological process are expressed by three main syndromes:
- Urinary syndrome. This phenomenon is characterized by increased urination at night and at the same time the daily volume of urine increases. Blood can be observed in the urine constantly or periodically.
- Pain syndrome. In particular, this pain is nagging and constant, localized in the lumbar region.
- Hypertensive syndrome. Against the background of all the processes occurring in the urinary system, the patient experiences an uncontrolled and uncorrectable increase in pressure.
- In addition, when conducting a general analysis of urine, protein will be detected in it, and its specific gravity will be low.
Microspecimen of myocardium for hemorrhagic infarction
Forum about health and beauty
In the spring, when the first truly warm days arrive, a tick ready to attack can be waiting for us on any blade of grass or branch. He is ready to bite into his victim at any time of the day. Greatest to
Enlarged lymph nodes in the neck are one of the consequences of a cold or acute viral infection that affects the respiratory tract. Because of this, the lymph nodes in the neck become inflamed and increase in size. Yes
Medicine. Medicine is a system of scientific knowledge and practical activities, the goals of which are to strengthen and preserve health, prolong people’s lives, prevent and treat diseases