Congenital occlusion:
- ureter
- ureteropelvic junction
- ureterovesical orifice
Congenital dilatation of the ureter
Deviation of the ureter or ureteral orifice
Displacement of the ureter or ureteral orifice
Abnormal implantation of the ureter or ureteral orifice
Ureteral anomaly NOS
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are clickable links to such studies.
If you believe that any of our content is inaccurate, out of date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes of kidney duplication
Kidney duplication occurs when two foci of induction of differentiation are formed in the metanephrogenic blastema. In this case, two pyelocaliceal systems are formed, but complete separation of the blastemas does not occur, and therefore the kidney is covered with a common fibrous capsule. Each half of the doubled kidney has its own blood supply. The renal vessels can depart separately from the aorta, or they can arise through a common trunk, dividing at the renal sinus or nearby. Some intrarenal arteries pass from one half to the other, which can be of great importance during partial nephrectomy.
[9], [10]
Content
Definition and general information [edit]
The absence of an organ is encountered with a frequency of 1 in 1000 newborns. Bilateral renal agenesis is observed 4 times less often than unilateral one and predominantly in males (in a ratio of 3:1).
Approximately 56% of cases are noted on the left. Inheritance is autosomal dominant.
Etiology and pathogenesis[edit]
Unilateral renal agenesis can be caused by mutations in a number of genes: RET (10q11.2), BMP4 (14q22-q23), FRAS1 (4q21.21), FREM1 (9p22.3) or UPK3A (22q13.31), PAX2 (10q24. 31), HNF1B (17q12), DSTYK (1q32). Unilateral renal agenesis can occur as part of a variety of multiorgan syndromes, including Kallmann syndrome, branchio-otorenal syndrome, DiGeorge syndrome, Fraser syndrome, MURCS association, Poland syndrome, renal cyst-diabetes syndrome, and Williams syndrome.
Maternal diabetes or the use of certain medications during pregnancy can also cause kidney failure.
Symptoms of kidney duplication
Most often the upper half is underdeveloped; very rarely both halves are functionally the same or the lower half is underdeveloped. The underdeveloped half in its morphological structure resembles kidney dysplasia. The presence of parenchymal renal dysplasia in combination with urodynamic disturbances due to splitting of the ureter creates the preconditions for the occurrence of diseases in the abnormal kidney.
Most often, the symptoms of kidney duplication duplicate the symptoms of the following diseases: chronic (53.3%) and acute (19.8%) pyelonephritis, urolithiasis (30.8%), hydronephrosis of one half (19.7%). Kidney duplication can be suspected by ultrasound, especially with dilatation of the upper urinary tract.
[11], [12], [13], [14], [15], [16]
Horseshoe kidney: ICD-10 code, causes of pathology in a child, symptoms, diagnosis, treatment
The kidneys are a vital organic structure that performs a complex job. They cleanse the blood of toxic substances, remove excess fluid, and regulate blood pressure. Every year, the number of kidney pathologies is steadily increasing, which doctors associate with deteriorating environmental conditions, poor-quality products containing chemical additives, etc. One of the fairly common congenital anomalies is the horseshoe kidney.
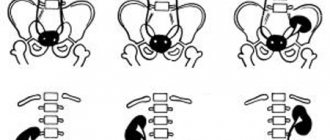
Horseshoe kidney
A horseshoe kidney is an abnormal congenital condition, the essence of which is the fusion of the upper or lower renal poles, due to which an isthmus is formed. The ICD-10 code is Q63.1. Typically, such an anomaly is accompanied by various pathological processes such as pyelonephritis, hydronephrosis, urolithiasis, etc. According to statistics, the horseshoe kidney occupies about 15% of the total number of anomalies of renal structures.
Most often, fusion of the lower poles occurs, as a result of which the kidney takes a U-shape (in 90% of cases). Each kidney has its own supply vessels and ureter. Almost every horseshoe kidney (≈89%) has an unusual cup structure and an abnormal vascular network with impaired blood circulation.
Much less often, the kidneys are fused by the upper poles, middle parts or opposite poles. Such forms also have a lot of associated pathologies.
The photo shows a normal and horseshoe kidney
Causes
The reason for the formation of a horseshoe kidney is disembryogenesis. The horseshoe kidney is formed during intrauterine development. Normally, in a fetus, kidney formation occurs in three stages: the prebud, the primary kidney, and then the secondary kidney. During the secondary kidney phase, the organ migrates to its bed in the lumbar region. The kidney is finally formed and fixed after the birth of the child.
The formation of a horseshoe kidney occurs when the process of organ migration is disrupted.
The reasons for such violations are the following factors:
- Aggressive environmental environment;
- Drug abuse;
- Pathologies of a genetic nature;
- Infectious lesions of the mother;
- Unhealthy habits of both or one of the parents;
- Chronic pathologies;
- Exposure to chemicals.
But more often than not, the true cause of the abnormal development of the organ cannot be determined. Pathology is more common in boys (2.5 times). In the general pediatric population, a horseshoe kidney is found in 1 in 500 newborns.
Quite often, a horseshoe kidney does not manifest itself in any way, but some children experience complications associated with the cardiovascular, genitourinary or nervous system. Symptoms may differ slightly depending on the concomitant damage to a particular organ.
In general, the following manifestations are distinguished:
- Pain syndrome that occurs in the umbilical zone during extension or flexion of the body. Pain can radiate to the lower abdomen, epigastrium or lower back after physical activity.
- Constipation resulting from compression of the mesenteric nerve plexuses by the isthmus of the fused organ.
- For a similar reason, the patient may be bothered by spasmodic intestinal pain or peristalsis disturbances.
- Constant pain causes hysteria, neurasthenia and emotional instability.
- Intrarenal increase in pressure resulting from compression of the vascular passages by the body of the abnormal kidney. This condition is often accompanied by blood in the urine.
- If compression of the inferior vena cava occurs, it leads to ascites and hyperedema of the lower half of the body, legs, and varicose veins.
- In the female population, a horseshoe kidney can lead to premature birth or menstrual irregularities.
It happens that an abnormal organ does not cause any problems and is asymptomatic, but is discovered during a random examination. If the fused organ is affected by any pathological process, then the clinical picture consists of symptoms of the lesion. In addition, the affected kidney can be combined with other congenital defects such as polycystic renal disease, spina bifida, skeletal abnormalities, hydrocephalus, etc.
Concomitant diseases and complications
The horseshoe kidney is often accompanied by complications caused by impaired urinary outflow:
- Hydronephrosis – 41.7% of cases.
- Urolithiasis – observed in 23.6% of cases.
- Pyelonephritis – 19.4%
- Arterial hypertension – 15.2%.
The horseshoe kidney is characterized by impaired urinary outflow, which is usually associated with improper location of the ureter. Also, impaired urinary outflow can be a consequence of blockage of the lumen with a stone.
When this happens, urine begins to accumulate in the calyces and pelvis. Since it is not excreted anywhere, the kidney enlarges, and the pyelocaliceal system begins to compress the parenchyma of the organ and its nephrons.
This leads to disturbances in the renal circulation, the occurrence of atrophic processes, which subsequently lead to necrosis. When irreversible death of nephrons occurs, partial or complete loss of renal function occurs.
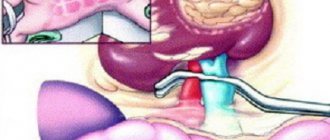
Hydronephrotic transformation or hydronephrosis develops, which can only be treated with surgical methods. The kidney is divided and positioned as close as possible to the physiological norm.
Hydronephrosis
Hydronephrosis is far from the only complication of a horseshoe kidney. For example, tumor formations and renal cancer often form in the isthmus that forms. Urodynamic disorders contribute to the loss of salt sediment, from which stones are subsequently formed and urolithiasis develops. Treatment is based on diet therapy, medication and instrumental surgery.
An abnormal kidney is often accompanied by congenital pathologies such as:
- Spina bifida - most often manifests itself in adolescents, a protrusion appears on the spinal column, radicular pain, similar to sciatica;
- Polycystic disease is a congenital anomaly of the kidneys, manifested by cystic degeneration of the organ parenchyma, which leads to a pathological decrease in renal functionality.
A horseshoe-shaped kidney increases the patient’s susceptibility to inflammatory pathologies, which include pyelonephritis, an infectious inflammatory process of bacterial origin. The causative agents of this complication are fungi, Proteus, staphylococcal or streptococcal components, and E. coli. These pathogens usually ascend to the kidney through the urinary tract from the rectal tissues or genitals.
During an attack of pyelonephritis, patients experience sudden lumbar pain and a sharp rise in temperature. And the horseshoe-shaped structure of the organ is fraught with the spread of the infectious process to the parenchymal structures of the kidney. The basis of treatment is antibiotic therapy with monitoring of antibiotic sensitivity.
If there is a suspicion of the presence of a horseshoe kidney, the patient is referred to undergo procedures such as ultrasound, electronic urography, computed tomography, etc.
- Based on the results of a urographic examination, a specialist can draw conclusions about the low location of the organ, its insufficient mobility, shadowing from the isthmus, shadow layering on the contour of the spine.
- Retrograde pyelography allows you to visualize the abnormal location of the organ, isthmus, silhouette of the kidney or its pelvis.
- Angiography is performed to study the location of the renal vasculature. In addition, such diagnostics allows us to identify the presence of additional vessels, the thickness and exact location of the isthmus.
- Ultrasound diagnostics (ultrasound) helps in identifying abnormal position of the renal pelvis, changes in the renal calyceal structures, and impaired blood circulation in the abnormal kidney.
- When performing nephroscintigraphy, an accumulation of a contrast radionuclide substance is recorded in the shape of a horseshoe, as if encircling the spine.
In the video, diagnostics of a horseshoe kidney using ultrasound:
Treatment
If the patient has no complaints, the kidneys function without failures, then the patient is simply constantly under the supervision of a nephrologist, who periodically prescribes the necessary preventive measures and diagnoses the condition of the renal structures. If the condition begins to deteriorate slightly, then the necessary therapy is prescribed.
If the deterioration is more serious, such as stone formation, tumors, hydronephrosis, then surgical treatment tactics are used. Urodynamic disturbances are eliminated by classical dissection of the isthmus and fixation of organs in their physiologically appropriate place.
The appearance of stones in the kidneys becomes an indication for lithotripsy, nephrolithotomy, pyelolithotomy or nephrolithotripsy. These surgical techniques are considered the most modern and are carried out under the control of special devices.
Horseshoe kidney is the most common developmental anomaly of the urinary system. The most serious disorders occur if there is compression of nearby organs. The most favorable prognosis is for patients in whom the anomaly was discovered in early childhood, and then an operation was performed to separate the kidneys.
Rate this article:
gidmed.com
Forms
[17], [18], [19], [20], [21], [22]
Accessory (third) kidney
An accessory (third) kidney is one of the rarest anomalies of this organ. The defect is almost always one-sided. Its origin is similar to that of the duplication bud, but too rapid differentiation leads to complete separation of the two metanephrogenic blastemas and the formation of two kidneys. The accessory kidney always has its own fibrous capsule, blood supply system, pyelocaliceal system and ureter, which often opens with an additional third orifice into the bladder below and medial to the two main orifices, but can also merge with the ureter of the main kidney like a split ureter (ureter fisus).
The essence of pathology
Kidney duplication in itself is not a dangerous anomaly .
Its key feature is a general deterioration in the filtering function of the urinary system, as well as an increased risk of chronic kidney disease.
Most often, doubling is unilateral, only in 5–7% of cases is it bilateral. Affects either the upper or lower lobe of the organ, extremely rarely – both at once. ICD-10 code – Q63.0-63.1.
What is this pathology? In most cases, the formation of an additional pelvis and, as a consequence, a second ureter. In a healthy person, one ureter comes out of each kidney, and with a double kidney, there are two, which can unite directly on the bladder or outside it.
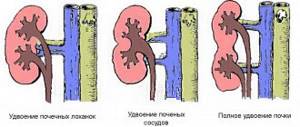
It is customary to distinguish 3 variations of kidney doubling:
- doubling of the pelvis;
- doubling of renal vessels;
- complete doubling of the kidney (the organ is divided into 2 independent systems with its own vessels and pelvis).
The first 2 options are usually referred to as incomplete doubling (see photo). And such a pathology is considered more complex and dangerous, since it is almost impossible to divide an organ without disrupting the functionality of its second part.
But with complete doubling of the kidney, one of its sides may subsequently atrophy (that is, stop functioning).
Treatment and prognosis
Treatment as such is not required for renal aplasia. The patient is necessarily prescribed a lifelong diet, the purpose of which is to reduce the load on the healthy kidney. If the pathology is accompanied by persistent hypertension, then treatment with mild diuretics is necessary.
It is also necessary to take preventive measures against bacterial kidney infections. The immune system also requires support so that the likelihood of viral agents or pathogenic bacteria entering the body is minimal. In particularly severe cases, transplantation is necessary.
In patients with renal aplasia, disability can be established when the functionality of a single kidney decreases, which is accompanied by severe symptoms of renal failure. Although disability for such a pathology is not always granted, patients are released from the army and immediately enlisted in the reserves.
Our readers successfully use Intoxic to get rid of parasites. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
Renal agenesis is ten times less common than pyelonephritis or hydronephrosis, but the pathology causes discomfort to the patient. The defect appears during embryonic development and consists in the absence of one bean-shaped organ or two natural filters in the fetus.
To prevent a serious defect, it is important to know what factors increase the risk of renal agenesis. Doctors explain how a congenital defect occurs and what to do if a child has only one kidney. Factors that provoke damage to the urinary tract of the embryo, methods of treatment and prevention of agenesis, possible complications are described in the article.
- general information
- Reasons for the development of pathology
- Types and forms of the disease
- Unilateral (ureter preserved)
- Unilateral (no ureter)
- Bilateral agenesis
- Diagnostics
- Characteristic signs and symptoms
- General rules and methods of treatment
- Renal agenesis in adults and children
general information
Kidney aplasia is the absence of one or both natural filters in the body. Without bean-shaped organs, it is impossible to remove fluid and decay products; when toxic substances accumulate above permissible limits, severe intoxication and death occur.
Diagnosis of pathology
Diagnosis of kidney duplication includes:
- ultrasound examination (allows you to establish the very fact of the presence of pathology and outline the contours of the organ);
- renal perfusion (study of the kidney blood flow system and vascular conductivity);
- angiography (performed using X-rays, also necessary to study blood flow);
- computer and magnetic resonance imaging (allows you to visualize an abnormal organ and establish the exact structure of its structure);
- comprehensive urine analysis (provides additional information to form a clinical picture of the patient).
Only after all the above studies can be established the exact type of pathology and, if necessary, a surgical treatment plan can be drawn up.