Streptococcus agalactiae
is a bacterial pathogen that can cause various diseases in humans. But its asymptomatic carriage is much more common.
Pregnant women are carriers of streptococcus
can lead to abortions in late pregnancy, inflammatory diseases of the genital organs, and complications such as postpartum sepsis. Children born from sick mothers or from women carrying the bacteria may develop pneumonia, meningitis or sepsis. In order to determine the degree of possible infection of the fetus, it is necessary to perform PCR to detect the DNA of streptococcus agalactia.
Using PCR, the DNA of Streptococcus agalactia is determined in the urine
or in a scraping from the vagina before childbirth in the thirty-fifth week of pregnancy for antibiotic therapy, if necessary.
PCR diagnostics
allows you to determine intrauterine streptococcal infection in the fetus.
When DNA of streptococcus agalactia is detected by PCR in the spinal cord, its etiological role in the development of meningitis is confirmed.
The detection of streptococcus agalactia DNA in biomaterial proves that it is the causative agent of sepsis or bacteremia.
The main indications for PCR diagnostics of urine
if Streptococcus agalactia is suspected, the following are:
- Thirty-fifth week of pregnancy - urine or vaginal scraping is examined.
- Presence of streptococcal infection in obstetric history.
- Examination of blood and cerebrospinal fluid if meningitis, sepsis or bacteremia is suspected.
- The presence of symptoms of cystitis, urethritis, pyelonephritis, orchitis, epididymitis, prostatitis.
The material for the study is the first portion of morning urine.
. Women take the test before menstruation or two days after it. Men are advised not to urinate for three hours before taking the test.
PCR method detects urinary tract infections
caused by streptococcus agalactia.
The result of the study is entered into the response form and expressed in copies/ml of sample. A negative result is recorded as not detected.
The study is carried out within three working days
.
Antibacterial drugs and contamination of biomaterial before analysis can affect the results of the study.
It is important to note that about forty percent of people are carriers of this infection, so it is necessary to use additional laboratory and instrumental research methods in the diagnosis of streptococcal infection.
Source: medcentr-Endomedlab.ru
Urine examination for streptococci
One of the most informative tests for streptococcus infection is bacteriological urine culture
One of the most informative tests for infections of internal organs is bacteriological urine culture
. This study is carried out during pregnancy registration and in the third trimester.
Using the results of the analysis, it is possible to determine the presence of an infection that can be transmitted in utero or infect the child at birth. In order for the result to be as accurate as possible, the following rules must be followed:
- Stop taking diuretics and choleretic drugs 3 days before the test.
- Eliminate heavy, salty and smoked foods from the menu one day before.
- Collect only the midstream portion of morning urine in a sterile container.
- Before collecting the analysis, it is necessary to perform genital hygiene and insert a cotton swab into the vagina.
- The test must be taken within two hours after collection.
Streptococcus agalactia in urine during pregnancy is determined by inoculating the material on a nutrient medium - a solution of 5% blood agar. In order for the bacterium to grow, it is provided with an optimal temperature for development of 37 degrees.
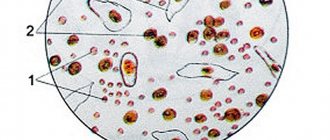
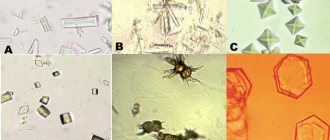
If streptococci are present, they form colonies of grayish plaques that are examined under a microscope. Next, the bacteria are sent to test tubes to determine their characteristics and sensitivity to antibiotics.
On average, a urine test for streptococci takes 7 days to prepare. The advantage of the study is high accuracy, exclusion of erroneous results and false reactions.
Laboratory diagnostic methods
Routinely, pregnant women undergo smears from the cervical canal. This research method allows you to determine the degree of vaginal cleanliness and establish the first deviations from the norm. If coccal flora predominates in the smear, a culture test is necessary, which is the main method for diagnosing the infection.
For sowing, liquid or solid nutrient media are used. In some laboratories they add substances that inhibit the growth of other microorganisms. This increases the excretion of streptococcus by 50%.
For sowing, material is taken from the vagina and anorectal area. It is recommended to take discharge from several areas of the mucous membrane at the same time. This also increases the likelihood of identifying the pathogen. Detection of 10 to 3 CFU/ml is a normal variant.
Since the role of streptococcus agalactia in infection of a newborn is very large, a system of screening tests has been developed to detect agalactia. To do this, they use the determination of microorganism antigens in latex agglutination, ELISA, and coagglutination. These methods are fast but have some disadvantages. If the examination is carried out during labor, vaginal discharge may be mixed with amniotic fluid and blood. This reduces the sensitivity of the tests.
PCR diagnostics is also used. With its help, you can isolate Streptococcus agalactia in urine discharged from the vagina and from the skin of a newborn. During the study, the DNA of the pathogen is determined. Recent developments in this area make it possible to study virulence genes. Identification of such a genetic composition indicates a high probability of infection of a newborn with a severe form of the disease.
For pregnant women, the study is carried out at 35-37 weeks. The PCR method allows you to identify qualitatively and quantitatively streptococcus in the material under study. Identifying the number of microorganisms allows us to judge the contamination of the area under study. The disadvantage of this method is that it is impossible to identify living representatives of the genus and determine their resistance to antibiotics.
Why is streptococcus agalactia dangerous during pregnancy?
In women, this type of streptococcus often causes an infection of the genitourinary system. Inflammatory processes occur due to decreased immunity and the proliferation of a large colony of streptococcus.
Urogenital diseases can be recognized by such signs as pain in the lower abdomen, itching, increased body temperature, and copious vaginal discharge.
Streptococcus agalactia during pregnancy often causes infections of the genitourinary system
Often streptococcus
causes the following diseases:
- Urethritis
is an inflammatory process of the urethral mucosa. In the absence of adequate treatment, urethritis leads to cystitis and inflammation of the appendages. - Cervicitis
is an infectious inflammation of the cervix. Complications of the disease can include cervical erosion, dysplasia and cancer. - Endometritis
- inflammation of the uterine mucosa is the most dangerous disease, as it can be accompanied by uterine bleeding, placental insufficiency and miscarriage.
With a large number of streptococcus colonies, inflammation of the membranes is possible, which invariably leads to premature birth, pathology of fetal development, and disruption of pregnancy. If a pregnant woman does not undergo drug treatment before the birth of the child, there is a risk of infection of the baby during childbirth.
As a rule, weakened and premature babies with pathologies are at risk.
Streptococcus agalactia during pregnancy can cause dangerous infectious diseases in infants immediately after birth or a few days later.
Streptoderma
– affects the upper layers of the skin and can cause deep erosions. The infection can be recognized by flat blisters with clear and then purulent contents. The pustule is accompanied by severe itching, which causes anxiety for the baby.
Vulgar ecthyma
– deep skin lesions with ulcers. Purulent blisters with yellow crusts form on the skin, under which a painful ulcer appears. The baby's body temperature is elevated, the general condition is lethargic and drowsy. Complications may include lymphadenitis and lymphangitis.
Streptococcus agalactia during pregnancy can cause serious infectious diseases in infants immediately after birth
Sepsis
– a dangerous development of streptococcal infection, which can lead to death. Symptoms of the disease are persistent fever and increased body temperature. If left untreated, toxic shock develops with damage to internal organs.
Meningitis
– the inflammatory process of the membranes of the brain is manifested by pallor of the skin, fever, and rash on the skin. Complications may include toxic shock and developmental delay.
Pneumonia
– develops as a result of damage to the alveoli of the lungs. Characteristic signs: shortness of breath, cough, vomiting, refusal to eat. The infection has a severe course, but with timely drug treatment, the favorable outcome increases significantly.
Necrotizing fasciitis
– Streptococci affect connective tissues and organs. A characteristic sign of the disease are numerous ulcers and purulent wounds. The disease is diagnosed in children extremely rarely.
Any disease caused by streptococcal infection is severe and poses a great threat to the baby’s life.
Only with timely treatment and proper medical care does a newborn have a chance to survive.
But unfortunately, not every child recovers completely; many of them have pathologies and suffer from central nervous system disorders.
If a woman has been diagnosed with streptococcus in her urine during pregnancy, treatment should be started as soon as possible
, especially if the infection is diagnosed after 30 weeks. Penicillin or ampicillin is used for therapy.
These drugs are absolutely safe for the expectant mother and baby and do not cause any adverse reactions. Before starting treatment with a penicillin-based antibiotic, it is necessary to test for an allergic reaction.
Ampicillin
The human body is regularly exposed to various bacterial infections that need to be promptly diagnosed and treated. Expectant mothers should pay special attention to their own health even at the stage of pregnancy planning.
, since they put not only their health, but also the life of the unborn child at great risk.
In order to avoid infection with streptococcus, it is necessary to ensure regular hygiene of the genital organs, strengthen the immune system, promptly treat diseases of the urinary system and listen to the recommendations of the supervising gynecologist.
An actively developing infection - streptococcus in the urine - can lead to irreversible consequences, although, at first glance, the bacterium seems harmless. In small quantities it does not harm an adult (for example, streptococcus agalactiae). But if the immune system is weakened and the colony increases, complications will arise. Only antibiotics can overcome such consequences. The difficulty lies in the symptoms of the disease, invisible in the early stages, which appear much later. In this regard, doctors recommend regular urine tests to determine the infection.
What is the danger of infection?
Streptococcus agalactia is detected in 20% of women during pregnancy. Lack of timely treatment can lead to the development of the following complications:
- urinary tract infection;
- spontaneous abortion;
- postpartum endometritis;
- chorioamnionitis;
- sepsis of the neonatal period;
- pneumonia of the newborn;
- endocarditis;
- meningitis.
For a woman, in most cases, the infection will be hidden; in a newborn, it often causes complications.
What it is?
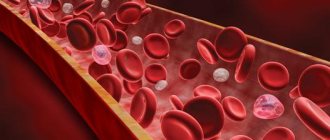
The infection can live in urine. The infection is almost always caused by beta-hemolytic streptococcus, which destroys red blood cells.
Harmful streptococcal infections appear when the immune system is severely weakened, a large number of bacteria enter the body at once, or hypothermia of bodily organs occurs. In other words, it is almost impossible to avoid streptococci, but you can monitor the number of colonies through basic personal hygiene and a healthy lifestyle.
If the environment is favorable for bacteria, an inflammatory or infectious process may develop.
Most
often, infection occurs through airborne droplets.
But infection is possible:
- during dental operations;
- placental route (from mother to child);
- through chronic bronchitis.
How does the pathogen get into the urine?
Streptococcus enters the bladder from the skin through the urethra. There are also options when it is transferred into the urine from the colon (the so-called fecal pathogen). From the anus, bacteria move into the urethra. The next chain is the bladder and above. This “ascending” path is more often typical for women due to its anatomical feature.
Symptoms of streptococcus in urine
There are no exact symptoms for streptococcal infection. It all depends on the area of the body affected by the infection. Symptoms of infection are associated with the fact that the bacterium, in the process of its life activity, releases toxins that are harmful to the body. Hence the unpleasant sensations. The most common signs are skin rashes, increased or decreased temperature, and unstable blood pressure. A dull pain appears in the kidney area, and problematic urination is observed. A urine test reveals unhealthy elevated levels of creatinine and hemoglobin.
If redness is already clearly visible, pus forms on the affected area of the body, and pain is felt when pressing, it means that the infection is in its peak stage. It is important to remember about the threat of toxins entering the bloodstream with infection, as a result of which there is a high probability of a person going into shock. As soon as the first, indirect symptoms of the disease appear, you need to immediately get tested.
Symptoms of the presence of bacteria in urine
An increased content of streptococci in the urine can cause manifestations of pathologies in various organs and systems of the human body. A person infected with streptococcal bacteria experiences the following symptoms:
- the urge to go to the toilet becomes more frequent;
- body temperature increases or decreases;
- lymph nodes in the groin area enlarge;
- the skin breaks out in a rash;
- there is pain and burning sensation during urination;
- acute abdominal pain;
- the color of urine changes, it becomes cloudy;
- redness appears in the area affected by bacteria;
- a whitish coating resembling flakes forms on the mucous membranes of the oral cavity;
- the patient suffers from attacks of nausea and vomiting;
- blood pressure levels decrease or increase;
- There is aching pain in the lower back.
Some patients complain of developing an allergic reaction. And it arises as a result of the interaction of the body with the waste products of streptococcus bacteria. The allergy manifests itself as a rash on top covered with yellow crusts. It may contain pus. During infection with streptococcus, autoimmune processes are often provoked, which cause destruction in the joints, heart and kidneys.
If treatment for streptococcal infection is not started in a timely manner, its further development can lead to endometritis, urethritis, vaginal candidiasis, inflammation in the bladder and prostate gland. Further, pus may be discharged through the urethra. In this case, the patient feels severe pain in the lower abdomen, and may also be bothered by the lumbar region, swelling and itching of the genitals.
Why is it dangerous?
When an adult is affected
Streptococcal infection causes a number of diseases if treatment is not started in time.
If left untreated, it can lead to inflammation of the bladder, resulting in urethritis. True, such processes occur only with weakened immunity. Urethritis affects both women and men.
Symptoms of urethritis are:
- pain and/or discharge during urination;
- itching and burning in the excretory canal.
If urethritis is not treated, then there is a high probability of cystitis, prostatitis, disturbance of the vaginal microflora, orchitis, balanitis, vesiculitis. Such consequences are possible after a sore throat caused by streptococcal infection in the respiratory tract. After passing through the urinary system, the bacterium can enter the kidneys and cause the disease glomerulonephritis.
What to do during pregnancy?
During pregnancy, 20% of women are diagnosed with this infection in the urine (even fecal streptococcus). Doctors say that the cause of the disease is tight synthetic underwear, improper intimate hygiene, unprotected sex (fecal matter is transmitted this way), and unsterile personal hygiene items. Such a high percentage of pregnant women suffering from streptococci is simply explained. During pregnancy, the body is weakened, immunity drops, which gives rise to the active development of infection.
With weakened immunity, the infection develops faster.
However, pregnant women should not overlook or take the treatment of the disease lightly. Complications include allergies, purulent otitis, sepsis, problems of the genitourinary and cardiovascular systems. As a rule, women learn about streptococcus based on the results of laboratory tests of urine or smear. In order for the research to give the correct result, it is necessary to pass the analysis correctly. A woman must wash herself before donating urine and cover her vagina with a sterile tampon. The container must be sterile; a disposable container is ideal. When a disease is detected, the woman is prescribed treatment, which consists of a course of antibiotics, and the doctor monitors the progress of the pregnancy.
Streptococcus bacteria do not pose a danger to a healthy adult, since the immune system successfully suppresses their reproduction. Streptococcus in the urine indicates an infectious disease that can have serious consequences, including death. Therefore, it is important to identify and properly treat the disease in a timely manner. Self-medication is dangerous not only due to lack of effectiveness, but also due to false negative test results. This, in turn, leads to untimely treatment and threatens complications of an existing disease.
Urine tests for staphylococcal infections
If the analysis reveals a high level of streptococci in the urine, then we can say with confidence that the person is infected, and at the same time he has a disease caused by streptococcal bacteria. Bacteria can lead to sore throat, tonsillitis, pharyngitis, urethritis, bronchitis, pneumonia, prostatitis, meningitis, cystitis, sepsis, periodontitis and pyelonephritis.
What does streptococcus indicate and threaten?
What kind of bacteria is this?
Hemolytic streptococcus is widespread and easily transmitted from an infected person or animal, through unwashed fruits or vegetables (fecal species), personal hygiene products (towels, toothbrushes), by airborne droplets, and can be inhaled with dust. There are alpha, beta and gamma coccal pathogens, which differ in the reactions they cause in the body. The most dangerous group of bacteria for humans is beta bacteria. In particular, this group includes the common species Streptococcus agalactiae, which causes irreversible damage to the nervous system of infants and sepsis in women in labor.
Why do streptococci appear in urine?
Bacteria appear during examination if there is an infection or if urine is collected incorrectly for analysis. The pathogen begins to actively grow when the immune system is weakened, under stress, or as a concomitant disease. Most often, colonies settle in the throat, intestines or genitourinary system. The presence of bacteria in the urine indicates a urinary tract infection. This may be a primary infection or the consequences of other diseases caused by streptococcus, for example:
The infection can be detected in urine after a sore throat.
- tonsillitis;
- scarlet fever;
- urethritis;
- sepsis;
- bronchitis;
- pneumonia;
- meningitis;
- periodontitis;
- pyelonephritis and others.
Symptoms
Streptococcal bacteria release toxic substances during their life processes, causing purulent rashes to appear on the skin. You feel weakness, nausea, fever, and swollen lymph nodes. In this case, there is a frequent urge to go to the toilet, pain when urinating, aching in the lower back or pain in the lower abdomen. The urine becomes cloudy, with bloody spots.
What is the danger?
Untreated streptococcal infections threaten autoimmune diseases, blood poisoning, irreversible changes in the structure of the kidneys, and kidney failure. Since bacteria are transmitted, among other things, through sexual contact, there is a high risk of infecting a partner during unprotected sexual intercourse. In pregnant women, bacteriuria must be treated before childbirth, since when a child passes through the genital tract, it will certainly become infected. There is also a risk of intrauterine infection.
Threat to an adult
The risk group includes office workers.
Illnesses caused by streptococcus affect people with weakened immune systems. Often these are office workers who are exposed to stress and lead a sedentary lifestyle in rooms with poor ventilation systems. Bacteria are part of dust and can be inhaled, causing damage to the respiratory tract (bronchitis, pneumonia, pharyngitis, sore throat), otitis media. If the body's defense system cannot limit the bacterial colony to one focus of infection, general blood poisoning develops.
Risk during pregnancy
Due to changes in hormonal levels and a general decrease in immunity, they are especially susceptible to the influence of bacteria. Streptococcus in the urine during pregnancy occurs in a third of pregnant women. Due to the structure of the genital organs, fecal streptococcus is often found in them. The main threat during this period is infection of the child in the womb or during childbirth. Therefore, pregnant women should regularly undergo urine tests and closely monitor their well-being. Often the course of pregnancy is complicated by pyelonephritis, cystitis; in especially severe cases, these bacteria can cause miscarriage.
The microflora of the human body is inhabited by a huge mass of different bacteria. Streptococcus actively multiplies in the urine in conditions of weakened immunity or during hypothermia, infecting the urinary tract. In an environment favorable to infection, the inflammatory process begins to develop.
Streptococcus in the vaginal microflora
Most of the normal vaginal flora is lactobacilli.
Opportunistic flora include streptococci, staphylococci, candida, gardnerella, ureaplasma and mycoplasma. If the number of these microorganisms does not exceed the norm, the condition of the vagina will be satisfactory. One of the causative agents of nonspecific inflammation is Streptococcus agalactia. The group of streptococci includes a large number of different microorganisms with similar morphological characteristics. Based on the type of growth on a nutrient medium, hemolytic, non-hemolytic and greening microorganisms are distinguished.
Streptococci of groups B and D, as well as viridans, are found in the vaginal environment. Agalactia is a beta-hemolytic streptococcus from group B. The norm for streptococci is 10 to 4 CFU/ml.
The colonization of streptococci in the vaginal environment occurs during puberty, especially at the beginning of sexual activity. Self-infection from the anal folds is also possible if, while washing, you direct movements away from the anus.
At-risk groups:
- women who have suffered premature birth;
- increased temperature during childbirth;
- anhydrous period of more than 18 hours;
- birth of a premature baby;
- underweight infants;
- C-section;
- the presence of bacteria in the urine.
During childbirth, a woman can infect her newborn. Streptococci are also transmitted through household means through shared hygiene items. A man can become infected during oral or anal intercourse.
While there are few streptococci in the vaginal environment, lactobacilli predominate. In large quantities, they can suppress the growth of opportunistic flora and protect against inflammation. Streptococcus is activated when there is an imbalance in the vaginal microflora.
Causes of microflora imbalance:
- hormonal changes;
- weakened immunity;
- failure to comply with personal hygiene rules;
- douching;
- severe systemic pathologies (diabetes mellitus).
During pregnancy, inflammation develops due to two factors at once (immunity and hormones). An increase in progesterone levels negatively affects local immunity, which is necessary to maintain pregnancy. However, against this background, latent infections of the genitourinary system often worsen.
A man becomes infected during unprotected sexual intercourse. He becomes a carrier and transmits streptococcus to his sexual partners.
Ways of infection with streptococcus
The stable presence of numerous colonies of microorganisms in the female genital organs and poor intimate hygiene are the main causes of the disease. Streptococcal bacteria usually do not detect themselves, but can be actively transmitted through handshakes, kisses, and sexual contact.
You can become infected with a pathogenic microorganism:
- by airborne droplets;
- for chronic bronchitis;
- during dental operations;
- through the placenta (from mother to child);
- after eating expired dairy products;
- during unprotected sexual intercourse;
- in kindergartens through toys and dishes;
- after exacerbation of infectious diseases.
Streptococci enter the bladder through the urethra from the skin. Women are also characterized by the transfer of bacteria from the colon (due to the peculiarities of their anatomical structure).
Infection of pregnant women
Streptococci are often detected in urine during pregnancy. They appear when:
- unprotected sex;
- neglect of the rules of intimate hygiene;
- wearing underwear made of synthetic fabrics.
This bacterium is almost always present in the vagina. Since the pregnant woman’s body is weakened, the infectious bacteria develops very quickly, which can cause some complications:
- allergies;
- sepsis;
- disease of the genitourinary organs;
- problems with the heart and blood vessels.
A newborn baby may develop meningitis, pneumonia, sepsis, and a neurological disorder is possible. The bacterium is especially dangerous for premature babies.
Signs of infection appear after the baby is born. The skin is pale, the baby's breathing is uneven, the body temperature is elevated, and vomiting may occur. Not all children recover completely. Most suffer from central nervous system disorders.
The most common signs of streptococcus:
- skin rashes;
- unstable pressure;
- tingling in the kidney area;
- painful urination.
A urine test always shows significantly elevated hemoglobin or creatinine levels.
Signs of a child becoming infected with streptococcal infection
Signs of early and late infection may appear. In the first case, fever, increased drowsiness in the first week of life, and problems with the respiratory system appear. Early onset of the disease occurs in 50% of newborns and sometimes leads to sepsis, pneumonia and meningitis.
With a late onset of infection, cough, problems with eating, high body temperature, convulsions or drowsiness, and nasal congestion are observed. These symptoms occur between 7 days and 3 months after birth and often provoke meningitis and sepsis.
In 99% of cases, infected newborns have no symptoms of the disease. For this reason, doctors recommend establishing GBS colonization through laboratory diagnostics. The test material is obtained by taking samples from the baby’s throat, external auditory canal, navel, and rectum. The presence of pathogenic microorganisms can be detected by examining the amniotic fluid.
Testing urine for infection in pregnant women
Bacteriological urine culture is considered the most informative. The examination is prescribed by a gynecologist when a pregnant woman is registered, as well as in the 3rd trimester. This is necessary to identify an infection that can be transmitted to a child at birth or even in utero.
To get the most accurate result, you need to follow some rules:
- 3 days before the day of the test, you must stop taking choleretic and diuretic drugs;
- do not eat salty or smoked foods before donating urine;
- before collecting urine, perform genital hygiene and insert a tampon into the vagina;
- collect only the second portion of morning urine in a sterile container;
- the test must be performed within 2 hours after urine collection.
If bacteria are present in the urine during pregnancy, they gather in colonies. A specialist examines them under a microscope. After this, they are sent in test tubes to determine their sensitivity to antibiotics. The analysis takes 7 days to prepare. The absolute norm is the complete absence of microorganisms in the urine.
Treatment of the disease
If streptococcus is detected in the urine during pregnancy, then treatment should be started immediately. It consists of several stages:
- Antibacterial therapy.
- Strengthening the immune system.
- Bringing intestinal microflora back to normal after antibiotic treatment.
- Detoxification of the body.
- Symptomatic therapy.
The main course of treatment for streptococcus consists of taking penicillin drugs. Penicillin or Ampicillin is prescribed. The drugs are safe for both mother and child and do not cause side effects. But still, an allergy test must be carried out before starting medication treatment.
To restore intestinal microflora, the following are additionally prescribed:
- Linux;
- Acipol;
- Bifiform;
- Cetrin;
- Zodak.
During the treatment period, excessive physical activity should not be allowed. In case of high intoxication, bed rest is required.
Treatment using folk remedies is possible, but only with the permission of a specialist.
If a staphylococcal infection is not treated, a pregnant woman may experience rupture of the membranes, premature birth, or intrauterine fetal death. Prevention of streptococcus is very simple: maintaining personal hygiene, preventing colds, strengthening the immune system. With timely treatment, you can get a normal outcome and avoid unwanted complications.
Source: narutoshinobilife.ru
Local therapy for streptococcus
Local therapy includes vaginal tablets and suppositories. Before childbirth, it is imperative to sanitize the vagina to reduce the chances of infection of the child. If the concentration of streptococcus exceeds 10 to the 8th degree and sanitation was not carried out, antibacterial therapy is required during childbirth. Sanitation of the birth canal and antibiotics help reduce the likelihood of infection of the child to 1-2%.
Recommended drugs:
- Fluomizin. Vaginal tablets effective for bacterial vaginosis. The tablet should be inserted into the vagina before bedtime (6 days). Microorganisms rarely develop resistance to the drug, but using the drug for less than 6 days leads to its ineffectiveness the next time. Contraindications to Fluomizin: allergies to components, ulcers of the vaginal mucosa, age under 18 years.
- Terzhinan. The drug is used in the treatment of bacterial and fungal infections. Thanks to prednisolone in its composition, Terzhinan has anti-inflammatory properties and reduces swelling of the mucous membrane. Pregnant women can use Terzhinan from the second trimester, during lactation only with the permission of a doctor. Before use, the tablet is moistened. During menstruation, therapy is not stopped. The course of treatment is 10 days.
- Hexicon. The suppositories contain chlorhexidine bigluconate, due to which they have an antimicrobial and antiseptic effect. Hexicon is effective for vaginosis and colpitis. Can be used during pregnancy and breastfeeding. To treat streptococcus, use 1 suppository 1-2 times a day for 7-10 days (for pregnant women 5-10 days).
Causes of appearance and possible complications
The disease appears due to weakened immunity, infection occurs through airborne droplets. In addition, the routes of transmission of streptococcal infection can be as follows:
- During dental procedures.
- Due to bronchitis, which is chronic.
- Through the placenta.
Such bacteria enter the urine through the urethra, passing from the skin. It is not uncommon for the pathogen to enter the urethra through the anus from the colon. This route of transmission is typical for women due to the structure of their genital organs. If left untreated, streptococcus can cause serious complications.
The most common of these is urethritis, which appears only if the patient's bladder is in a weakened state. Signs of this disease are burning and severe itching in the urinary canal. As well as discharge and pain when urinating.
In addition, prostatitis, cystitis, vesiculitis, balanitis may appear, or the microflora in the vagina may be disrupted. They can occur after a prolonged sore throat, which was provoked by the appearance of streptococcal pathogens in the respiratory tract. Also, bacteria can enter the kidneys from the urinary system and cause glomerulonephritis.
Epidemiology
Streptococcus agalactiae is widespread in nature. In the human body, they colonize the mucous membranes of the intestines, nose, pharynx, excretory and reproductive systems. From 15 to 40% of women of reproductive age are bacteria carriers.
There are three options for streptococcus to stay in the vagina:
- The harmless existence of bacteria in the body,
- Bacterial vaginosis,
- pathological process.
If there are few bacteria in a smear from the cervical canal, but there are a lot of lactobacilli, they talk about the first option. When the number of streptococci exceeds the number of lactic acid bacteria, and the number of leukocytes in the field of view is within 50, this is a sign of vaginal dysbiosis. If there are much more leukocytes, then there is an inflammatory process occurring in the form of cervicitis, colpitis, endometritis.
Ways of spread of infection:
- Contact - through common household objects, with a kiss, hug,
- Self-infection - germs from the anal area can penetrate the vagina,
- Vertical - infection of the fetus during pregnancy or newborn during childbirth,
- Sexual - during coitus without a condom,
- Airborne - when sneezing, coughing, close contact with a sick person,
- Food - when consuming contaminated food products,
- Hematogenous introduction of infection from the primary foci - the kidneys or nasopharynx.
Newborns become infected in the first hours and days after birth. This can happen earlier: in the pre- and intranatal period.
Streptococcus agalactiae is characterized by autumn-winter seasonality. These microorganisms are activated at a time when the body is weakened by viruses. Against the background of ARVI, a secondary bacterial infection most often develops.
Symptoms of the disease
As a rule, there are no exact symptoms for this disease. Everything will depend on how large the affected area is on the patient’s body. During its life, this pathogen releases toxins harmful to the body, which lead to unpleasant sensations in the patient. The most typical signs are:
- Increase or decrease in temperature level.
- Skin rashes.
- Blood pressure surges.
- Problems with urination.
- Rashes on the skin.
- Painful sensations in the kidney area.
First, the patient develops redness in areas of the skin, which develops into a purulent infection. If you apply light pressure to the affected area, you may feel pain. This condition indicates that the disease has entered an acute stage.
Patients with streptococcus should remember that if they do not consult a doctor promptly, toxins may enter their blood, which can provoke a state of shock. Therefore, experts recommend that at the first symptoms of such a disease, immediately contact a medical facility for diagnosis and treatment.
Streptococcus in pregnant women and children
During pregnancy, such an infection is diagnosed in a large number of women. The following can provoke the appearance of such a disease:
- Unprotected sexual intercourse (can cause fecal streptococcus).
- Failure to maintain intimate hygiene.
- Tight synthetic underwear.
Pregnant women are the main category of people who are exposed to this type of infection. The immune forces of the expectant mother are weakened during this period, which allows the infection to freely penetrate into the exhausted body and spread within it.
Experts recommend that women undergo tests and examinations throughout pregnancy to identify the causative agents of this disease. If it is detected, its treatment must be taken seriously. Untreated streptococcus can develop into purulent otitis media, sepsis, allergies, or problems with the cardiovascular and genitourinary systems.
In order for urine tests to give the correct result, it is necessary to carefully prepare for such a laboratory analysis. To do this, before donating urine, a woman needs to rinse her genitals thoroughly and cover her vagina with a sterile tampon. Urine is best placed in a sterile container from a pharmacy. If bacteria are detected, the pregnant woman will be prescribed a course of antibiotic therapy. In addition, the specialist will monitor her health even more carefully.
The most dangerous type of streptococcus in newly born children is agalactia. It can be fatal due to the infection's effect on the nervous system. In the mother's womb, such an infection is dangerous due to premature rupture of the membranes and other pathological conditions.
Without proper therapeutic measures, transmission of this bacterium to a child may result in meningitis, sepsis or pneumonia. Therefore, it is important to identify the presence of such a disease in a mother or her unborn baby as early as possible, and immediately begin a course of treatment. Antibiotics are used for this.
Influence
The bacillus has an extremely negative effect not only on the body of pregnant women, but also on the development of the baby.
Why is streptococcus dangerous during pregnancy?
For the baby
Infection of the membranes and the fetus itself often causes intrauterine growth retardation and intrauterine infection of the fetus. It can even cause miscarriages and stillbirths.
Intrauterine infection is realized by the occurrence of congenital pneumonia, neuroinfection, and in 5% of cases it ends in death.
Diagnosis and treatment
The sooner streptococcus is detected in the urine, the more effective treatment measures will be. To find the causative agents of this disease, special tests have been developed that can show results for the presence of bacteria within half an hour. As a rule, in medical institutions, in addition to tests, they use analysis of a selected sample.
If streptococcus is detected, doctors will refer the patient for testing for nephritis and urethritis. In children, such infections can be detected both early and late. In the first case, they will experience breathing problems, fever and drowsiness. As for the late stage, it is characterized by the appearance of convulsions, fever, lack of appetite, cough and nasal congestion.
But sometimes streptococcus does not produce such pronounced symptoms, so experts recommend diagnostics in a laboratory to detect bacteria.
In a urine test for such an infection, a large amount of hemoglobin and creatinine will be present.
Doctors use antibiotics to treat streptococcal infections. To ensure that such therapy does not harm the patient’s body, the treatment is supplemented with drugs that restore the microflora. If, as a result of exposure to streptococcus, the patient develops severe poisoning of the body, the medical institution will prescribe him to refuse any physical activity and adhere to bed rest.
When prescribing medications, the doctor will take into account the fact that urine is very sensitive to antibiotic drugs. Therefore, as a rule, complex measures are used in the treatment of such a disease. The course of antibiotic treatment ranges from 10 to 14 days. As preventive measures, experts advise paying close attention to your health, paying attention to your immune system and maintaining personal hygiene. Also, it should be remembered that it is possible to get rid of a streptococcal infection and avoid subsequent complications only if the patient consults a doctor in time.
Source: MochaAnaliz.com
Bacteria danger factors
The microorganism has a negative effect due to toxic enzymes and pathogenic factors. This is a kind of weapon of the bacterium, which it uses to colonize the human body:
- streptolysin destroys surrounding tissue;
- leukocidin is able to destroy immune cells, which allows the microorganism to invade the body;
- necrotoxin can cause tissue necrosis;
- hyaluronidase and amylase promote the introduction of streptococcus into surrounding tissues.
Thanks to a set of these factors, Streptococcus agalactia causes numerous diseases in the human body. Most often in adults, this microorganism causes a urinary tract infection.
The greatest number of negative consequences of streptococcus agalactia threatens a pregnant woman and a newborn child. The presence of infection can cause the following complications:
- bacteremia during or after childbirth;
- premature discharge of amniotic fluid;
- postpartum inflammation of the inner lining of the uterus (endometritis);
- chorioamnionitis – inflammation of the membranes;
- spontaneous abortion at any stage of pregnancy;
- sepsis, meningitis, neonatal endocarditis;
- premature onset of labor.
What does streptococcus indicate and threaten?
What kind of bacteria is this?
Hemolytic streptococcus is widespread and easily transmitted from an infected person or animal, through unwashed fruits or vegetables (fecal species), personal hygiene products (towels, toothbrushes), by airborne droplets, and can be inhaled with dust. There are alpha, beta and gamma coccal pathogens, which differ in the reactions they cause in the body. The most dangerous group of bacteria for humans is beta bacteria. In particular, this group includes the common species Streptococcus agalactiae, which causes irreversible damage to the nervous system of infants and sepsis in women in labor.
Return to contents
Why do streptococci appear in urine?
Bacteria appear during examination if there is an infection or if urine is collected incorrectly for analysis. The pathogen begins to actively grow when the immune system is weakened, under stress, or as a concomitant disease. Most often, colonies settle in the throat, intestines or genitourinary system. The presence of bacteria in the urine indicates a urinary tract infection. This may be a primary infection or the consequences of other diseases caused by streptococcus, for example:
The infection can be detected in urine after a sore throat.
- tonsillitis;
- scarlet fever;
- urethritis;
- sepsis;
- bronchitis;
- pneumonia;
- meningitis;
- periodontitis;
- pyelonephritis and others.
Return to contents
Symptoms
Streptococcal bacteria release toxic substances during their life processes, causing purulent rashes to appear on the skin. You feel weakness, nausea, fever, and swollen lymph nodes. In this case, there is a frequent urge to go to the toilet, pain when urinating, aching in the lower back or pain in the lower abdomen. The urine becomes cloudy, with bloody spots.
Return to contents
What is the danger?
Untreated streptococcal infections threaten autoimmune diseases, blood poisoning, irreversible changes in the structure of the kidneys, and kidney failure. Since bacteria are transmitted, among other things, through sexual contact, there is a high risk of infecting a partner during unprotected sexual intercourse. In pregnant women, bacteriuria must be treated before childbirth, since when a child passes through the genital tract, it will certainly become infected. There is also a risk of intrauterine infection.
Return to contents
Threat to an adult
The risk group includes office workers.
Illnesses caused by streptococcus affect people with weakened immune systems. Often these are office workers who are exposed to stress and lead a sedentary lifestyle in rooms with poor ventilation systems. Bacteria are part of dust and can be inhaled, causing damage to the respiratory tract (bronchitis, pneumonia, pharyngitis, sore throat), otitis media. If the body's defense system cannot limit the bacterial colony to one focus of infection, general blood poisoning develops.
Return to contents
Risk during pregnancy
Due to changes in hormonal levels and a general decrease in immunity, they are especially susceptible to the influence of bacteria. Streptococcus in the urine during pregnancy occurs in a third of pregnant women. Due to the structure of the genital organs, fecal streptococcus is often found in them. The main threat during this period is infection of the child in the womb or during childbirth. Therefore, pregnant women should regularly undergo urine tests and closely monitor their well-being. Often the course of pregnancy is complicated by pyelonephritis, cystitis; in especially severe cases, these bacteria can cause miscarriage.
Return to contents
Illnesses in a child
Although cases of infection in children are quite rare (about 2%), most of them are fatal or have serious consequences for the health and development of the child.
The consequence of infection of a child can be cerebral palsy.
A baby can become infected in the womb or during the birth canal. In this case, the child develops such dangerous diseases as:
- respiratory tract diseases, in particular pneumonia;
- cerebral palsy;
- blood poisoning - sepsis;
- deafness and other hearing impairments;
- meningitis;
- retardation in mental and physical development.
Return to contents
Prevention
You can start therapy with nitrofurantoin, which acts on many types of gram-negative and gram-positive bacteria. In pregnant women, a vaginal smear is obtained to detect streptococcus. If it is detected, ampicillin is prescribed, which accumulates in very high concentrations in the urine, and in fairly high concentrations in the wall and secretions of the vagina. Carriage of group B streptococcus in a pregnant woman must be reflected in the medical documentation in order to administer ampicillin during childbirth to prevent infection of the newborn.
Treating a pregnant woman with ampicillin or another suitable antibacterial drug does not guarantee the eradication of S. agalactiae from the vagina. A pregnant woman should be warned that this bacterium is constantly present in the rectum, therefore, in order to reduce vaginal contamination, personal hygiene should be carefully observed. In addition, S. agalactiae can be transmitted sexually.
Streptococcus agalactiae (S. agalactiae) infection. Neonatal incidence of S. Agalactiae infection, its clinical manifestations. Methods of specific immunoprophylaxis of S. Agalactiae infection.
Sadova N.V., Zaplatnikov A.L., Shipulina O.Yu., Podkopaev V.N., Fomina S.G., Skachkova T.S., Domonova
E.A., Safonova A.P.
One of the common bacterial diseases of the perinatal period is infection caused by Streptococcus agalactiae (S. agalactiae). In women during pregnancy, S. agalactiae; the infection can be either asymptomatic or clinically significant with the development of bacteremia, endometritis, chorioamnionitis, inflammation of the urinary and birth tract, and in newborns it can manifest as localized and invasive lesions.
S. agalactiae is a member of group B streptococci, which are gram-positive, encapsulated, non-spore-forming facultative anaerobes. The main virulence factor of S. agalactiae is the polysaccharide capsule. Of the protein pathogenicity factors, C5a peptidase, beta-hemolysin, C proteins (alpha- and beta-), hyaluronidase, Sip protein, CAMP factor (B-protein), as well as a complex of proteases, hemolysin, adhesins, etc. are especially noted.
It has been established that 15–40% of women are carriers of S. agalactiae, which colonizes the mucous membranes of the vagina or rectum. The birth of children from S. agalactiae-infected women is accompanied in 50% by vertical transmission of the pathogen. Transmission of the infection from an infected mother usually occurs shortly before childbirth or immediately during childbirth. In the postnatal period, especially in the immediate hours and days after birth, the child can also become infected, but this happens much less frequently compared to pre- and intranatal contamination. It has been noted that S. agalactiae infection of newborns does not always lead to the development of an infectious process. Risk factors for infection in a child born from an S. agalactiae-infected woman are: the age of the pregnant woman (12 hours), intrauterine growth retardation and the presence of S. agalactiae infection in previously born children.
Until recently, the neonatal incidence of S. agalactiae infection was 1–4 per 1000 live births, among which in 75% of cases the manifestation occurred on days 1–7 of life. At the same time, per 100 infected pregnant women, 1 child was born with severe S. agalactiae infection. Thanks to the active use of recommendations for the prevention of S. agalactiae infection in obstetric practice, it was possible to significantly reduce the level of infection of newborns, as well as the frequency of invasive forms of the disease in children in the first month of life. Thus, in countries where antibacterial prophylaxis of perinatal S. agalactiae infection is carried out, the incidence in the early neonatal period has been reduced by more than 80%, and neonatal morbidity rates in general do not exceed 0.3 cases per 1000 live births.
Clinical manifestations of perinatal S. agalactiae infection in women are postpartum infections of the endometrium, urinary tract, brain, as well as sepsis and complications of cesarean section. In newborns, localized and invasive forms of perinatal S. agalactiae infection are isolated. Moreover, depending on the time of manifestation, diseases with an early (before the 7th day of life) and late (after the 7th day of life) onset are distinguished. S. agalactiae – infection in newborns most often occurs in the form of invasive forms with bacteremia, damage to the lungs and meninges. Often, the disease becomes septic in nature, especially in premature and low birth weight infants, in whom sepsis is noted in 77–88% of all cases of S. agalactiae infection. It is in this group of patients that S. agalactiae infection is most severe and often ends in death. It should be especially noted that in the vast majority of cases, children are born in a normal condition, but after a few hours the clinical picture changes dramatically.
The manifestation of early forms, as a rule, debuts with cyanosis and respiratory disorders (apnea, tachypnea). A fulminant form of the disease is also possible, in which all the signs of septic shock appear very quickly. In clinical blood tests, leukopenia is often detected. With a late onset (after the 7th day of life), S. agalactiae infection can also occur in the form of sepsis or meningitis. Clinically, tension in the fontanelles, fever, depression of consciousness up to coma, and tonic-clonic convulsions are more often recorded. Other manifestations of infection are less common: omphalitis, otitis, sinusitis, conjunctivitis, arthritis, osteomyelitis, skin lesions, urinary system, endocarditis, myocarditis.
Due to the low specificity of clinical manifestations of S. agalactiae infection in newborns, laboratory diagnostic methods (classical bacteriological, serological, molecular biological) are of particular importance in verifying the etiology of the disease. Bacterioscopy reveals typical gram-positive cocci forming short chains. To detect S. agalactiae in biological fluids of the body (in blood, cerebrospinal fluid, urine, tracheo-bronchial aspirate) by bacteriological culture, it is necessary to use media enriched with blood or serum, because The isolation of S. agalactiae on conventional media, as a rule, does not exceed 10–12%. Serological diagnostic methods are important only in terms of retrospective confirmation of the diagnosis, as well as for identifying the intensity of passive immunity received transplacentally from the mother. At the same time, high-risk factors for S. agalactiae infection in the neonatal period include indications of seronegativity or low titers of specific antibodies in infected pregnant women.
In recent years, molecular biological diagnostic methods have become increasingly important. The speed of obtaining results when using polymerase chain reaction (PCR), combined with high sensitivity and specificity, makes PCR an indispensable method for verifying infectious diseases, especially in neonatological practice. Thus, in a pilot study, we studied the sensitivity of PCR in detecting the S. agalactiae genome in comparison with the bacteriological culture method. In a study of tracheal aspirate in 62 newborns in the neonatal intensive care unit due to severe infections of the neonatal period, in 9 children (14.5%) the genome of S. agalactiae was detected by PCR, while in parallel studies Bacteriological culture results were negative. Probably, the negative results of the bacteriological study were due to massive antibiotic therapy administered to children from the first days of life, which could lead to a change in the cultural and morphological characteristics of the pathogen and a decrease in the number of viable microorganisms.
Methods for specific immunoprophylaxis of S. agalactiae infection have not yet been developed, therefore antibiotic prophylaxis (AB prophylaxis) is used to prevent perinatal S. agalactiae infection. CDC recommendations developed in 2002 provide for mandatory screening for S. agalactiae carriage of all pregnant women at 35–37 weeks. When a pathogen is isolated from the vagina and/or anus, a woman is prescribed antibiotics during childbirth in cases where there are certain risk factors. Risk factors include the following conditions: the previous child suffered an invasive S. agalactiae infection, S. agalactiae bacteriuria occurred during the current pregnancy, threat of premature birth (up to 37 weeks), anhydrous interval of more than 12 hours, fever during childbirth .
If one of the above risk factors is detected in an S. agalactia-infected woman, an antibiotic is prescribed to prevent perinatal S. agalactiae infection during childbirth.
For AB prophylaxis, it is recommended to use benzylpenicillin, which is administered intravenously at a dose of 5 million units from the moment of the onset of labor, subsequently moving to a dose of 2.5 million units every 4 hours until the end of labor. An alternative to benzylpenicillin is ampicillin, which is also administered intravenously, initially at a dose of 2 g per injection, and then 1 g every 4 hours. If you are allergic to penicillins, they are replaced with clindamycin or erythromycin, but more often in these cases cefazolin is recommended (initially 2 g per intravenous injection, then 1 g every 8 hours intravenously until the end of labor). If there is a high risk of developing anaphylaxis due to beta-lactam antibiotics, vancomycin can be used, which is recommended to be administered intravenously, 1 g every 12 hours until the end of labor. Analysis of the results of the studies showed that thanks to AB prevention, it was possible to significantly reduce not only the neonatal incidence of S. agalactiae infection (regression by more than 80%), but also the frequency of development of invasive forms, which determined a significant improvement in the prognosis of the disease.
In cases where the woman did not undergo AB prophylaxis for S. agalactiae infection during childbirth, and the newborn has risk factors (the mother is a carrier of S. agalactiae, the mother’s age is less than 20 years, a complicated obstetric history, premature birth, fever in childbirth, a long anhydrous period, S. agalactiae infections in previously born children, as well as signs of intrauterine growth retardation in the child himself), etiotropic therapy should be started as quickly as possible. The choice of initial AB therapy is carried out empirically. Due to the fact that S. agalactiae is highly sensitive to beta-lactam antibiotics, ampicillin is the drug of choice if S. agalactiae infection is suspected. However, given that the clinical picture is nonspecific and there is a possibility of a different etiology of the disease, ampicillin is combined with gentamicin. In this case, the preferred route of administration of antibiotics is intravenous. In cases where neonatal S. agalactiae sepsis develops, ampicillin is prescribed at a rate of 200 mg/kg/day. For meningitis, the dose of antibiotics is increased, and ampicillin is administered at the rate of 300 mg/kg/day. When S. agalactiae and its genome are isolated, treatment is continued with the selected combination of antibiotics until the condition improves, and then switched to ampicillin monotherapy. For non-invasive forms of S. agalactiae infection, the duration of monotherapy is 10 days, for S. agalactiae - uncomplicated meningitis - 14 days, for S. agalactiae - arthritis and osteomyelitis - 3-4 weeks, for S. agalactiae - endocartitis and S. agalactiae - ventriculitis – at least 4 weeks.
Thus, there are now every opportunity to reduce morbidity and mortality from perinatal S. agalactiae infection. To do this, it is necessary to screen all pregnant women at 35–37 weeks for S. agalactiae carriage. If it is confirmed and there are risk factors (the previous child suffered S. agalactiae infection in the neonatal period, the woman has S. agalactiae bacteriuria, premature birth, a long anhydrous period, fever during childbirth), the woman during childbirth should be prescribed antibiotics to prevent perinatal S. agalactiae–contamination of her child. Strict implementation of these recommendations can reliably reduce the risk of vertical infection and significantly reduce the frequency of invasive forms of S. agalactiae diseases in newborns.
Literature
- Ohanyan K.A. The course and outcome of pregnancy during colonization of the genitourinary tract of women with group B and D streptococci. Abstract. diss. Ph.D. honey. Sciences. – St. Petersburg, 2008, 24
- Pokrovsky V.I., Pozdeev O.K. Family Streptococcaceae/ Medical microbiology. GEOTAR Medicine, M, 1999: 193–206.
- Shabalov N.P. Intrauterine infections/ Neonatology. In 2 volumes - St. Petersburg: Special literature, 1996, T. 2: 43–76.
- Baltimore RS Huie SM, Meek JI, Schuchat A. Early–onset neonatal sepsis in the era of group B streptococcal prevention. 2001. Vol. 108:1094–8.
- Boyer KM: Neonatal group in streptococcal infections // Current Opinion Pediatrics, 1995, 7: 13–18.
- Centers for Disease Control and Prevention(CDC). Prevention of perinatal group In streptococcal disease: Revised Guidelines from CDC // Morb. Mortal. Wkly Rep. 2002.Vol.51: 10–22
- Kenyon SL, Taylor PJ., Tarnow–Mordi W. Broad–spectrum antibiotics for preterm, prelabor rupture of fetal membranes, ORACLE Collaborative Group // Lancet. Vol. 357:979–88.
- Red Book: Report of the Committee on Infectious Diseases. 27h ed. Elk Grove Village, IL: American Academy of Pediatrics, 2006; 992.
- Weisner AM, Johnson AP, Lamagni TL et al. Characterization of group In streptococci recovered from infants with invasive disease in England and Wales // Clin Infect Dis. 2004. Vol. 38:1203–1208.
- Nandyal RR. Update on group B streptococcal infections: perinatal and neonatal periods. J Perinat Neonatal Nurs. 2008, 22, 3: 230-37. 11. Shulyak B.F. Group B streptococcus infection, methods of its laboratory diagnosis and prevention. Medical alphabet. 2010, no. 2: 47–53
- Gardam MA, Low DE, Saginur R. Group B streptococcal necrotizing fasciitis and streptococcal toxic shock-like syndrome in adults. Arch Intern Med 1998, 158:1704–08.
- Sendi P., Johansson L., Norrby–Teglund A. Invasive group B Streptococcal disease in non– pregnant adults: a review with emphasis on skin and soft–tissue infections. 2008, 36, 2, 100–11.
- Dmitriev A.V., Shakleina E.V. Molecular epidemiology of pathogenic group B streptococci // Zh. microb. epidemiol. and immunol. 2003: 83–92.
- Fischetti VA Gram–Positive Pathogens, American Society Microbiology, Washington, DC, 2000. 511 p.
- Jacobsson K. A Novel family of fibrinogen–binding proteins in Streptococcus agalactiae // Vet. 2003. Vol. 96: 103–113.
- Eidelshtein I.A., Sekhin S.V., Ivanchik N.V. et al. Validation of a test system based on real-time PCR for the detection of Streptococcus agalactiae in comparison with the microbiological method. Molecular diagnostics. M., 2010, 3: 346–348.
A huge variety of bacteria surrounds humans. Some of them cause serious diseases, others constitute the normal microflora of the skin, mucous membranes, gastrointestinal tract, and genitourinary system. Such bacteria include Streptococcus agalactia.
The balance of microbial activity is the key to health. In addition to beneficial properties, various bacteria also have negative factors in cohabitation with humans. Some of the representatives of opportunistic flora become causative agents of purulent infections under certain conditions.
The activation of such bacteria is especially dangerous in people with reduced immunity. In particular, streptococcus can cause serious illness in pregnant women and newborns.
The microbe is a gram-positive bacteria. That is, with special Gram staining for microscopy, it does not lose color after washing. This property is used to identify bacteria. Most gram-positive bacteria are causative agents of infections in humans.
The type of streptococcus agalactia is presented as spherical or ellipsoidal structures that are arranged in pairs or in the form of chains. This specific growth of bacteria allows them to be differentiated from other microbes.
Depending on the polysaccharide antigens, certain streptococci are characterized by certain serogroups that allow precise identification of the pathogen. There are 20 serogroups of streptococci, Agalactia belongs to serogroup B.
This representative of the opportunistic human microflora is a facultative anaerobic microorganism. This means that the bacteria do not need oxygen to function, but under certain conditions the microbe adapts to a type of respiration in which it uses it.
Agalactia is a beta-hemolytic bacteria. When grown on blood agar (nutrient medium), they carry out complete hemolysis (destruction of red blood cells - erythrocytes). The main factor of pathogenicity (the ability to cause disease) is the polysaccharide capsule, which interferes with the process of phagocytosis - the capture and destruction of bacteria by the body's protective cells.
Necessary tests
To diagnose streptococcus, it is necessary to undergo a series of tests. A smear from the mucous membrane of the affected organ will be informative:
- for angina - from the tonsils;
- for sinusitis - from the nose;
- for urethritis - from the urethra in men, and in women also from the vagina.
For bronchitis and pneumonia, sputum discharge is analyzed. If meningitis is suspected, cerebrospinal fluid sampling is necessary. For all diseases, a urine test is performed. For correct results, urine should be collected in the morning after hygiene procedures. The collection is carried out in a sterile container, separating the middle portion. To prevent the vaginal microflora in women from affecting the indicators, it is recommended to close the vagina with a sterile cotton swab. If it is suspected that bacteria have entered the test material from the outside, a repeat analysis is carried out using a catheter.
Return to contents