Kidney tests – a set of blood tests (not urine) aimed at assessing kidney function.
Indeed, when conducting kidney tests, biochemical studies of the blood are taken into account. If the kidney is sick, it means that it does not fulfill its main cleansing role and the level of so-called toxins increases.
Kidney tests are taken as part of a comprehensive diagnosis of diseases, often together with liver tests. In the price list of the laboratory, along with rheumatic tests, the research package often bears the same name - kidney tests.
How to decipher a biochemical blood test in adults?
Decoding a biochemical blood test is a comparison of the results obtained with normal values. The analysis form contains a complete list of indicators determined by the biochemical laboratory and their reference values.
Biochemical analysis is prescribed for diagnosis:
- Pathologies of the gynecological system.
- Diseases of the circulatory system (leukemia).
- Kidney, liver failure (hereditary pathologies).
- Disturbances in the functioning of the heart muscle (heart attack, stroke).
- Diseases in the musculoskeletal system (arthritis, arthrosis, osteoporosis).
- Diseases of the thyroid gland (diabetes mellitus).
- Deviations in the functioning of the stomach, intestines, pancreas.
Sometimes it is enough to establish a final diagnosis based on deviations from the norm in one or more parameters, but more often, for a full diagnosis, other results of additional research methods and an assessment of the clinical picture of the disease are required.
Instead of an afterword
Kidney tests are necessary for the diagnosis of acute and chronic kidney diseases. But, indicators from a group of kidney tests may indicate many other diseases - joints, muscles, endocrine glands.
Creatinine, urea and uric acid are the three main indicators of kidney tests. At the same time, for a complete diagnosis of diseases, tests such as cystatin C may be needed, as well as ultrasound, CT, MRI, and urography.
You need to prescribe and read tests with understanding and knowledge. Seek advice from a doctor; only a specialist can do this correctly. Don't self-medicate!
Be healthy!
Preparing for analysis
The reliability of the blood test may well be affected by its preparation and implementation. Therefore, it is worth noting the main points of preparation in order to receive normal research results without false deviations.
- Eliminate heavy foods (fried, fatty and spicy foods) from your diet at least 24 hours before blood sampling - it is best to stick to a balanced diet several days before the test.
- Reduce the consumption of coffee, strong tea, psychostimulants to a minimum - 12 hours before donating blood, you should not take substances that affect the central nervous system (caffeine, alcohol).
- Provide comfortable conditions for your emotional state, avoid stress and physical activity.
- On the day of blood collection, you should not eat before the procedure.
Indications for the study
Any patient is referred for such an examination, since kidney diseases are considered quite common. The main goal is to detect the problem in order to begin timely treatment. It is necessary to clarify under what circumstances kidney tests may be prescribed:
- The patient is taking medications that cause organ damage and have a detrimental effect on substances contained in the kidneys.
- There is a risk of hereditary factors. This confirms that the illnesses of relatives could be passed on to you by inheritance. Such problems should not be left unchecked, as subsequent generations are also at risk if the problem is not identified and eradicated in a timely manner.
- When the body is affected by diabetes mellitus, kidney failure occurs, blood pressure constantly rises, and pyelonephritis appears in a chronic form.
- During pregnancy, expectant mothers are recommended to undergo this type of examination in order to avoid various tendencies to difficulties in the ureteral system.
Even without supervision from specialists, you should independently monitor the normal functioning of your organs. When violations are detected, you should immediately consult a doctor.
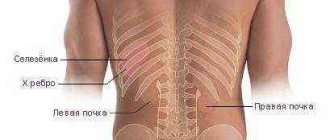
Signs of kidney dysfunction are:
- frequent and prolonged pain in the head;
- swelling appearing on the face;
- sensations of chills or fever, nagging pain in the lumbar region;
- deviations from normal body temperature without obvious reasons;
- increased pressure in the arteries.
The patient’s general well-being deteriorates, the level of performance of the body decreases, which is exhausted not only physically, but also morally.
But even in the case of the simultaneous presence of all signs, it is prohibited to establish a diagnosis and begin independent treatment - you should consult a specialist. After deciphering the kidney profile, it is allowed to take the necessary measures.
Each analysis requires at least some preparation, otherwise the indicators will be distorted or completely inaccurate. It must be remembered that blood will be tested. Before a kidney test, a certain list of measures should be followed:
- For a couple of weeks, you should stop taking medications that can distort the readings. The doctor tells the patient what medications are allowed to be taken and what is strictly prohibited.
- Before testing, you must adhere to a certain diet for a week, limiting yourself to fried and fatty foods.
- Two days before the test, stop drinking alcoholic beverages and also avoid smoking. Physical activity is also contraindicated.
- You cannot eat food twelve hours before, because the analysis is done on an empty stomach. You can only drink filtered water.
- For thirty minutes, the patient needs to rest so that no traces of physical or mental stress remain in the body - blood is donated in a calm state.
After delivery, the analysis is processed within 24 hours, its results can be clarified with the attending physician. They perform diagnostics and determine your next steps, which will be aimed at adhering to the therapeutic course. How to collect urine
Biochemical blood test: normal indicators
For convenience, the norms of biochemical blood test indicators in adults are shown in the table:
| Analysis: | Men: | Women: |
| Total protein | 64-84 g/l. | 64-84 g/l. |
| Hemoglobin | 130-160 g/l | 120-150 g/l. |
| Haptoglobin | 150-2000 mg/l | 150-2000 mg/l |
| Glucose | 3.30-5.50 mmol/l. | 3.30-5.50 mmol/l. |
| Urea | 2.5-8.3 mmol/l. | 2.5-8.3 mmol/l. |
| Creatinine | 62-115 µmol/l | 53-97 µmol/l. |
| Cholesterol | 3.5-6.5 mmol/l. | 3.5-6.5 mmol/l. |
| Bilirubin | 5-20 µmol/l. | 5-20 µmol/l. |
| AlAT (ALT) | up to 45 units/l. | up to 31 units/l. |
| ASAT (AST) | up to 45 units/l. | up to 31 units/l. |
| Lipase | 0-190 units/l. | 0-190 units/l. |
| Alpha amylase | 28-100 units/l. | 28-100 units/l. |
| Pancreatic amylase | 0-50 units/l. | 0-50 units/l. |
Each of the criteria indicated in the table reflects the condition of one or more human organs, and the combination of some of them allows in some cases to make an accurate diagnosis or direct the diagnostic process in the right direction.
Below we will look at what each of these tests shows using the example of deciphering a biochemical blood test in adults.
The most common kidney diseases and their symptoms
There are many diseases that cause kidney problems, but some are particularly common.
Urolithiasis disease
The main symptom of this disease is renal colic. It is a consequence of the passage of a stone from the kidney into the ureter, which leads to disruption of the outflow of urine and injury to the walls of the urinary tract. Acute pain can spread to the entire pelvic area, and sometimes to the inner thigh.
A person suffering from renal colic cannot find a position in which the pain would subside. There is an admixture of blood in the urine, sometimes sand is noticeable.
Inflammation (cystitis, pyelonephritis)
The most common diseases accompanied by inflammation of the kidneys and urinary tract are cystitis and pyelonephritis.
With these ailments, the patient experiences high fever, lethargy and decreased appetite.
The pain can be either aching or sharp. There is a feeling of heaviness in the lumbar region. Often cystitis and pyelonephritis are accompanied by frequent and painful urination.
Infections (glomerulonephritis)
Glomerulonephritis is an infectious disease. In the first stages of the disease, blood is noticeable in the urine, and as the disease progresses, anuria (cessation of urine production) may occur. With glomerulonephritis, the electrolyte balance is disturbed, extensive swelling develops, but there is no pain characteristic of renal diseases. The most serious complication is swelling of the brain and lungs.
Total protein
Total protein is the total concentration of proteins found in the blood. Proteins take part in all biochemical reactions of the body - they transport various substances, act as catalysts for reactions, and participate in immune defense.
Normal levels of protein in the blood are 64-84 g/l. If the protein is higher than this, the body may be susceptible to infection. In addition, the cause of increased protein may be arthritis, rheumatism, or the onset of cancer. With a low protein content in the blood, the likelihood of liver disease increases many times, as well as problems with the intestines and kidneys. The most difficult diagnosis for low protein is cancer.
See in more detail: why protein is elevated in the blood.
Preventive measures
The kidneys are the natural filter of our body, so it is very important to take care of their condition and prevent the development of possible pathologies in advance.
To do this, it is enough to follow simple tips and recommendations, mainly related to your daily diet and lifestyle.
Here is a list of preventive measures that will help avoid the development of kidney diseases:
- Limit the amount of foods in your diet that are high in protein, which can cause kidney stones. The protein norm per day for an adult is 0.7 grams per kg of weight.
- It is necessary to stop drinking alcoholic beverages.
- Eat more foods that are good for your kidneys: berries (lingonberries, cranberries, strawberries, blueberries), watermelon and melon, rose hips, fresh herbs, vegetables (cabbage, cucumbers, pumpkin, bell peppers), apples, fish (preferably sea).
- Maintain drinking regime. If you do not have chronic kidney disease, drink up to 1.5 liters of water per day, in hot weather, in case of dehydration (diarrhea and vomiting), and during intense exercise, this volume increases.
- Avoid any hypothermia, as it increases the load on the kidneys.
- Play sports (but don’t overexert yourself; dancing and yoga are good for preventing kidney disease).
- Temper yourself and strengthen your immune system.
- Watch your weight.
The kidneys are a fairly sensitive organ, so you should treat them with special attention.
If you notice any symptoms that indicate the development of kidney disease, be sure to consult a doctor. Remember that the disease is easier to treat at the initial stage.
Sometimes the presence of pathologies of the urinary system can be suspected independently. If you see white flakes in your urine, you need to see a doctor for a diagnosis. Could this phenomenon be normal?
Why your kidneys hurt during pregnancy and what can be done as treatment, you will find out by following the link.
Albumen
This protein is produced by the liver and is considered the main protein in the blood plasma. In general, experts distinguish albumins as a separate protein group, called protein fractions.
An increase in the concentration of albumin in the blood (hyperalbuminemia) may be associated with the following pathologies:
- dehydration, or dehydration (loss of fluid from the body through vomiting, diarrhea, profuse sweating);
- extensive burns.
A reduced albumin level is observed in smoking patients and in women during pregnancy and breastfeeding. In other people, a decrease in albumin may indicate various liver pathologies (for example, cirrhosis, hepatitis, or oncology), or intestinal inflammation of an infectious nature (sepsis). In addition, in case of heart failure or cancer, burns or fever, various injuries or drug overdose, the albumin in the blood will be lower than normal.
Video on the topic
Refers to additional methods for diagnosing diseases. Modern medicine has a large arsenal of laboratory tests, one of the most important is a biochemical blood test.
They are used to obtain more detailed data on the functioning of the entire organism or a specific organ, since the biochemical changes at the slightest disturbance in their functions. This popular laboratory diagnostic method provides a lot of information for the doctor and has a high degree of reliability. Analysis of biochemical parameters is used to diagnose diseases of many organs and systems in therapy, gynecology, and surgery. The modern one includes several dozen different indicators. Let us consider only those of them that are most important in the correct diagnosis of diseases of organs and systems.
Biochemical for diseases of the heart and blood vessels
In patients with atherosclerosis, which causes the development of coronary artery disease, hypertension and other pathologies of the heart and blood vessels, the level of cholesterol and beta lipoproteins is determined.
An informative diagnostic test for damage to the heart muscle is an increase in the activity of the enzymes creatine phosphokinase, aspartate aminotransferase, alanine aminotransferase, and lactate dehydrogenase.
To determine the degree of inflammation activity in rheumatism, myocarditis and other inflammatory diseases, protein fractions - albumins and globulins - are determined.
Biochemical blood parameters in diseases of the digestive tract
Biochemical indicators occupy a vital place in the diagnosis of liver diseases. They are not very specific and do not provide an accurate diagnosis, but their results make it possible to assess the functional state of the liver and the degree of its impairment. The main indicators of the functional state of the liver are pigment, carbohydrate, protein, enzyme and The study of pigment metabolism involves determining the content of total, direct and indirect. The state of carbohydrate metabolism is indicated by the amount of sialic acids, seromucoid and lactic acid. Protein metabolism is characterized by blood and its fractions. Indicators characterizing liver function also include total lipids, cholesterol, triglycerides, and lipoproteins.
Biochemical blood parameters in kidney diseases
The most important indicator of kidney function, which is determined by a biochemical blood test, is creatinine. The state of the functional capacity of the kidneys is also judged by the level of urea.
In assessing the work of other organs, this analysis is not of great importance.
Patient preparation and technique for taking a blood test for biochemistry
Preparing a patient for a biochemical test is not difficult. Usually this test is taken in the morning, the patient must come on an empty stomach, so before taking the test you must not eat anything for 6-8 hours.
To determine biochemical parameters, 5-10 ml of blood is taken from the patient’s ulnar vein. Typically, test results are ready within 24 hours after donating blood.
Biochemical blood parameters should be determined even if there are no special deviations from health. Analysis indicators will help assess the functioning of the entire body and promptly identify possible deviations in the functioning of a particular organ. Carrying out a blood test for biochemistry will help you take the necessary measures before symptoms of a certain disease appear, which will be much more difficult to treat at an advanced clinical stage.
General blood analysis
for kidney diseases is one of the main tools for diagnosing the clinical picture of the disease. Many kidney diseases, especially in the acute period or in the acute phase of a chronic course, are accompanied by changes in the peripheral blood picture and its biochemical parameters.
What do the general blood test indicators mean?
Leukocytes (WBC, white blood cells or white blood cells)
- are responsible for neutralizing infection and cellular immunity of the body against viruses and bacteria. There are 5 types of leukocytes: granulocytes (neutrophils, eosinophils, basophils), monocytes and lymphocytes.
Normal leukocyte count
in the blood: (4-9) x 10^9/l.
Increased number of white blood cells (leukocytosis)
- a sign of an inflammatory process.
A change in the picture of white blood in a number of kidney diseases is expressed primarily by an increase in the content of leukocytes.
Moderate or severe leukocytosis is observed with pyelonephritis
, to a lesser extent in
acute and exacerbation of chronic glomerulonephritis
,
subacute (extracapillary) nephritis
, with secondary kidney damage in patients with
periarteritis nodosa
,
rheumatism
,
hemorrhagic capillary toxicosis
,
rheumatoid arthritis
, etc.
At the same time for lupus nephritis
(in patients with SLE - systemic lupus erythematosus) leukopenia or normal white blood cell counts are characteristic.
Slight or moderate leukocytosis is often observed in chronic renal failure
of various etiologies. It is often accompanied by a shift in the leukocyte count to the left, and sometimes by eosinophilia.
ESR - erythrocyte sedimentation rate
.
An important indicator of the presence and activity of the inflammatory process in the kidneys is ESR. Erythrocyte sedimentation rate (ESR) is a nonspecific indicator of the pathological condition of the body.
Normal ESR
in different categories of patients:
- newborns - 0-2 mm/h;
- children under 6 years old - 12-17 mm/h;
- men under 60 years old - up to 8 mm/h;
- women under 60 years old - up to 12 mm/h;
- men over 60 years old - up to 15 mm/h;
- women over 60 years old - up to 20 mm/h.
Increase in ESR
indicates
inflammation, acute infection
or
poisoning
.
It can be increased in all primary and secondary kidney lesions. Moreover, in patients with secondary kidney damage (for example, with diffuse connective tissue diseases, myeloma, etc.), a significant increase in ESR is due to the underlying disease. ESR reaches a high level in nephrotic syndrome
of various origins.
Red blood cells (RBC, red blood cells)
- blood elements containing hemoglobin, red blood cells, which participate in the transport of oxygen to tissues and support biological oxidation processes in the body.
Normal red blood cell count
in blood:
- men - (4.0-5.1) x 10^{12}/l
- women - (3.7-4.7) x 10^{12}/l
- children - (3.80-4.90) x 10^{12}/l
A decrease in the number of red blood cells indicates anemia (anemia). Slight or moderate anemia is often found in patients with chronic pyelonephritis
, with nephrotic syndrome.
Increased (erythrocytosis) number of red blood cells
happens when:
- neoplasms;
- hydrocele of the renal pelvis;
- the influence of corticosteroids;
- Cushing's disease and syndrome;
- Polycythemia vera disease;
- treatment with steroids.
A slight relative increase in the number of red blood cells may be associated with blood thickening due to a burn, diarrhea, or taking diuretics.
Decreased red blood cell count
observed when:
- blood loss;
- anemia;
- pregnancy;
- hydremia (intravenous administration of large amounts of fluid, that is, infusion therapy)
- with the outflow of tissue fluid into the bloodstream while reducing edema (therapy with diuretics).
- reducing the intensity of red blood cell formation in the bone marrow;
- accelerated destruction of red blood cells.
Hemoglobin (Hb, HGB)
- carries oxygen from the lungs to the organs and tissues of the body. Low hemoglobin indicates anemia (anemia).
Normal hemoglobin content
in blood:
- men - 135-160 g/l (grams per liter);
- women - 120-140 g/l.
Anemia that gradually increases and reaches a significant degree in some cases is characteristic of chronic and acute renal failure
, as well as subacute (extracapillary)
nephritis
.
Increase in hemoglobin
noted when:
- primary and secondary erythremia;
- dehydration (false effect due to hemoconcentration);
- excessive smoking (formation of functionally inactive HbCO).
Decreased hemoglobin
detected when:
- anemia;
- overhydration (a false effect due to hemodilution - “dilution” of the blood, increasing the volume of plasma relative to the volume of the totality of formed elements).
Platelets (PLT)
- participate in the process of blood clotting.
A decrease in platelet count
indicates poor blood clotting. A natural decrease in platelet levels is observed during menstruation and pregnancy, and an increase after physical activity. In case of kidney disease, the blood clotting factor should be taken into account when prescribing certain drugs that affect the prothrombin index.
Eosinophils (eosinophilic granulocytes)
- a type of leukocyte.
An increase in the content of eosinophils
may indicate allergic diseases and the presence of worms.
In addition to a general blood test, kidney disease may require additional studies to provide a more complete picture of the clinical picture of the disease.
As nonspecific laboratory tests that reflect the inflammatory process in the kidneys and the degree of its activity, biochemical blood parameters such as C-reactive protein, DPA test, the content of sialic acids, fibrinogen, cholesterol, total protein and protein fractions
, which are most pronounced in the acute phase of the disease or during its exacerbation during the chronic course, as well as in nephrotic syndrome. These indicators are determined using generally accepted methods.
Changes in blood electrolyte composition
In case of acute or chronic renal failure, as well as long-term use of diuretics, monitoring of the electrolyte composition of the blood is required, in particular the concentration of potassium, sodium, calcium and chlorine ions in it.
Glucose (sugar)
The most common indicator of carbohydrate metabolism is blood sugar. Its short-term increase occurs during emotional arousal, stress reactions, pain attacks, and after eating. The norm is 3.5-5.5 mmol/l (glucose tolerance test, sugar load test).
- Sugar is elevated - diabetes, endocrine disorders, pancreatitis, pancreatic tumor, cerebral hemorrhage, chronic liver and kidney damage, myocardial infarction, cystic fibrosis.
- Sugar is low - damage to the liver and pancreas, hypothyroidism, stomach or adrenal cancer, arsenic poisoning or certain medications, alcohol intoxication.
What tests to take for kidney disease: types
With the help of a general examination of urine, severe kidney diseases can be identified.
Checking the chemical characteristics of urine, examining it under a microscope for pathological impurities - the OAM method. Urine tests can determine the number of good blood cells, white blood cells, as well as the color, acidity and transparency of biological fluid. This type of examination also identifies pathogenic contaminants. A general urine test is done to diagnose pyelonephritis, glomerulonephritis, urolithiasis and urethritis. Using this method, the following indicators are checked in patients:
- amylase;
- glucose;
- creatinine;
- uric acid;
- urea;
- microalbumin.
General blood analysis
Tests can detect abnormalities in liver and kidney disease. Research is effective in identifying disorders in the musculoskeletal and endocrine systems. Blood tests are also performed to diagnose kidney disease. Nitrogenous compounds of metabolism are excreted by paired organs. A fairly high level indicates that the kidneys are not coping with their work, and the doctor diagnoses failure. Blood counts or special tests help him with this. Biochemistry for kidney diseases carefully examines the composition of the components to determine the degree of chronic, inflammatory processes and pathologies in the kidneys.
Renal and functional tests, their indicators
Creatinine level
Creatinine levels are low in people who eat more plant foods.
The component is considered the end product of protein metabolism. Creatinine is a nitrogen substance that is not affected by physical or psychological stress or food. With a good lifestyle, the level of the substance in the blood is constant and varies depending on muscle mass. Deviations may indicate disturbances in metabolic processes or excessive use of medications. Low levels of the substance in the river indicate the consumption of only plant foods, and are typical for people with a lack of muscle mass. The following factors provoke an upward change in results.
Kidney disease is a fairly common ailment of the human genitourinary system. The main cause of kidney disease is infection, most often E. coli. According to statistics, about 4% of our country's population suffers from kidney disease. It is noted that women are susceptible to more diseases than men. There is an explanation for this. As you know, most of the diseases of the kidneys and genitourinary system occur due to various infections that enter our body through the urethra. Due to the structure of the female genital organs, the risk of infection in women is very high. The kidneys are the filter of our body. Thanks to them, every minute our blood is cleansed of harmful microbes and bacteria. If kidney function is impaired, the entire body will suffer. A timely visit to a doctor will prevent kidney disease from progressing and prevent the risk of various complications.
Uric acid
The main breakdown product of the main component of nucleic acids - purine bases. Since it is not used further in metabolic processes, it is excreted unchanged by the kidneys. The normal level in blood plasma is 0.16-0.44 mmol/l.
An increase in uric acid levels in the blood indicates:
- renal failure;
- leukemia, lymphoma;
- prolonged fasting;
- alcohol abuse;
- overdose of salicylates and diuretics.
A decrease in the level of uric acid in the blood can be observed during treatment with piperazine drugs, allopurinol, prebenecid, ACTH, sometimes with hepatitis, anemia.
See in more detail: why uric acid in the blood is elevated.
Renal test norms
Reference values, i.e. Each laboratory has its own standards. But they do not differ much, so below are the international standards (in mol/l) and units of measurement for kidney samples :
1. creatinine
- newborns up to 28 days – 12-48
- infants up to 1 year – 21-55
- children from 1 to 15 years old – 27-88
- women – 44-104
- men – 44-110
2. urea
- newborns – 1.7-5.0
- infants – 1.4-5.4
- children – 1.8-6.7
- men – 2.8-8.0
- women – 2.0-6.7
3. uric acid
- newborns – 143-340
- infants – 120-340
- children – 140-340
- men – 220-420
- women – 140-340
Urea
It is a consequence of the breakdown of proteins. The permissible amount of this substance in a person’s blood changes with age. Often, the level of urea goes through the roof in patients who have pathologies in their kidneys: doctors prescribe a similar blood test to diagnose and predict the disease.
A decrease in the level of urea in the blood can be triggered by reasons that are physiological (pregnancy, fasting, excessive exercise), or pathological (celiac disease, cirrhosis of the liver, heavy metal poisoning).
See in more detail: why urea in the blood is elevated.
Checking your kidneys at home
Interestingly, you can do a simple kidney examination yourself. It is enough to collect your morning urine in a clean white or transparent container and evaluate its clarity, color and smell.
Urine of a healthy person:
- transparent, without foreign matter;
- straw-yellow color;
- has a slight odor.
If you find foam, flakes, sediment in it, a color change to brown or reddish, or a strong odor, you must undergo a medical examination. Symptoms of pathology of the urinary system (lower back pain, difficulty urinating, signs of intoxication) are another indication for prescribing tests.
Creatinine
This substance, like urea, is a product of protein metabolism and is also excreted by the kidneys. Creatinine is a product of metabolic processes occurring in skeletal muscles, and to a lesser extent in the brain. Accordingly, its level will depend on the condition of the kidneys and muscles.
Increased creatinine is observed in renal failure, severe injuries with muscle damage, increased thyroid function, and after the use of certain anti-inflammatory and antibacterial agents. Moderately high creatinine is found in athletes.
See in more detail: why creatinine is elevated in the blood.
Renal tests and renal function tests - differences
Even though these two concepts sound very similar, they show different things. The first are blood indicators that the doctor looks at and only then draws conclusions. The second ones are calculated using a formula based on knowledge of the indicators of kidney tests, when the result is obvious.
Renal function tests are more accurate and evaluate the kidney's ability to concentrate and dilute urine. After all, if you don’t do this, then it turns out that urine is poorly filtered blood. Also, renal function tests are more complex - the level of creatinine in the blood and urine is measured, age, weight, and gender are taken into account. For analysis, samples can be taken directly from the ureters or renal artery.
The Zimnitsky test and the test with antidiuretic hormone are also aimed at assessing the concentration-dilution (sorry) activity of the kidneys. But they measure the specific gravity of urine, its quantity, osmolarity of blood and urine.
Kidney function tests include:
- glomerular filtration rate
- creatinine clearance
- inulin clearance
So, the main difference between renal function tests and simple renal tests is the presence of calculations and formulas.
Aspartate aminotransferase (AST, AST)
A cellular enzyme involved in amino acid metabolism. AST is found in the tissues of the heart, liver, kidneys, nervous tissue, skeletal muscles and other organs. An AST blood test may show an increase in AST in the blood if the body has a disease such as:
- myocardial infarction;
- viral, toxic, alcoholic hepatitis;
- angina pectoris;
- acute pancreatitis;
- liver cancer;
- acute rheumatic carditis;
- heavy physical activity;
- heart failure.
AST is elevated in skeletal muscle injuries, burns, heat stroke, and as a result of cardiac surgery.
See more details: why AST is elevated.
What does the analysis show?
From the analysis readings, the levels of certain substances are established, then the doctor studies the patient’s indicators and compiles a transcript:
- Urea. This is the final product of the digestive process, which determines the performance of the kidneys. If necessary, subsequent diagnostics are performed to identify diseases that may occur in the organs of the ureteric system.
- Uric acid. It is removed along with urine as a result of the breakdown of proteins and nucleotides of complex shape. Its level in the blood should not exceed the normal value. Otherwise, this may confirm that the body is affected by kidney disease.
- Creatine. Its indicator is considered the most important. In the case of normal metabolism, the element is completely removed simultaneously with urine. Its accumulation in the blood in large quantities causes pathology.
- Electrolytes. A number of chemical elements that are contained inside cells. This is another important indicator of the performance of the urinary system.
The slightest non-compliance with standards is considered a prerequisite for the emergence of serious diseases. They should be identified and treated early.
Cholesterol
A component of fat metabolism, it is involved in the construction of cell membranes, the synthesis of sex hormones and vitamin D. There is total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
Degrees of increased cholesterol in the blood:
- 5.2-6.5 mmol/l – mild degree of increase in the substance, a risk zone for atherosclerosis;
- 6.5-8.0 mmol/l – a moderate increase, which is corrected by diet;
- over 8.0 mmol/l – a high level requiring drug intervention.
An increase in cholesterol levels in the serum or blood plasma is an argument in favor of atherosclerosis, hypothyroidism (low activity of the thyroid gland), chronic hepatitis, decompensated diabetes mellitus, obstructive jaundice.
This indicator decreases when:
- malignant liver tumors;
- cirrhosis of the liver;
- rheumatoid arthritis;
- hyperfunction of the thyroid and parathyroid glands;
- starvation;
- malabsorption of substances;
- chronic obstructive pulmonary diseases.
Bilirubin
Bilirubin is a yellow-red pigment that is formed when hemoglobin breaks down in the spleen, liver and bone marrow. Its normal level in the blood of children and adults is 3.4–20.5 µmol/l.
If the table with the examination results contains an elevated level of bilirubin, then the doctor can diagnose one of the following diseases in adults:
- cholelithiasis;
- pancreatic tumors;
- inflammatory diseases of the biliary tract.
If bilirubin is below normal, then the patient may have one of the following diseases:
- acute viral hepatitis;
- bacterial liver damage (leptospirosis, brucellosis, etc.);
- toxic hepatitis;
- medicinal product;
- neoplasms in the liver and primary biliary cirrhosis;
- hemolytic anemia of various etiologies.
Bilirubin, formed as a result of the breakdown of hemoglobin (indirect), is released into the blood, where it binds to albumin and is transported to the liver. In liver cells, bilirubin combines with glucuronic acid. This bilirubin bound to glucuronic acid is called direct bilirubin.
See in more detail: why bilirubin is increased in the blood.
Hardware diagnostics of kidneys
To find out whether the kidneys are sick and whether they are working well, in addition to urine and blood tests, hardware diagnostics are performed, which provides additional information about the condition of the internal organs and allows an accurate diagnosis. Most often they resort to the following diagnostic methods:
- Survey radiography - provides information about the shape, contours, size and location of these organs, and also allows you to identify stones. The nature of the change in the listed parameters is determined by the type of disease.
- Ultrasound examination - determines the size of the kidneys, the thickness of the parenchyma, the condition of the pelvis, cups and other parts of the urinary system. The type of changes is characteristic of various diseases. For example, acute pyelonephritis causes an enlargement of the kidney, thickening of the parenchyma, and with chronic pyelonephritis its size decreases, the ratio of the thickness of the parenchyma to the area of the pyelocaliceal complex decreases, and other changes are observed.
- Radionuclide renography allows you to evaluate the functions of the urinary system, renal artery patency, trauma, renal obstruction; identify congenital anomalies of the urinary system, acute and chronic renal failure, and urinary tract infections.
- Cystoscopy - examination of the mucous membrane of the bladder using a cystoscope allows you to identify stones and other foreign bodies, as well as tumors of the bladder, assess the condition of its inner lining, and determine which kidney secretes blood or pus. The examination of the urethral mucosa is called urethroscopy.
- Biopsy - analysis of a small piece of organ tissue is performed to determine the nature and extent of structural tissue damage, such as glomerular or tubular disease.
- Computed tomography – performs detailed visualization and reveals pathology of the kidneys, bladder, adrenal glands; allows you to diagnose urolithiasis, cysts, polycystic disease, exclude oncopathology, and study the functionality of organs.
Having compared the patient's complaints, the results of examination, tests and other types of diagnostics, the urologist - a specialist in diseases of the urinary system - makes a diagnosis. Making a diagnosis requires a mandatory in-person consultation with a doctor! Tests and other types of studies are repeated during treatment to monitor its effectiveness.
Laboratory tests play an important role in the diagnosis of kidney pathology. They allow you to reliably assess the functional state of the urinary organs and even judge the prognosis of the disease. In our review, we will try to figure out what tests you need to take first in order to check your kidneys and get a complete picture of their work.
Amylase
Breaks down carbohydrates from food and ensures their digestion. Contained in the salivary glands and pancreas. There is alpha-amylysis (diastase) and pancreatic amylase.
- alpha-amylase rate: 28-100 units/l.
- pancreatic amylase rate: 0-50 units/l.
A high amylase content in a biochemical blood test indicates: peritonitis, pancreatitis, diabetes mellitus, pancreatic cyst, stone, cholecystitis or renal failure.
Decreased alpha-amylase: thyrotoxicosis; myocardial infarction; complete necrosis of the pancreas; toxicosis of pregnant women.
Deviations from the norm
Change in creatinine level
An increased level of creatinine, which is included in the biochemical blood test, can be caused by:
- Medicines can increase creatinine levels.
syndrome of impairment of all renal functions;
- acromegaly (dysfunction of the anterior pituitary gland) and gigantism;
- muscle damage, both mechanical and surgical;
- taking toxic medications (sulfonamides, some groups of antibiotics);
- radiation sickness;
- increased content in the bloodstream of glucose, ketone bodies, as well as medications - vitamins (ascorbic acid), antibiotics (cefazolin), painkillers (ibuprofen);
- unbalanced diet;
- endocrine pathologies;
- dehydration.
- starvation;
- decrease in muscle mass;
- taking corticosteroid drugs;
- 1st and 2nd trimester of pregnancy;
- plant-based (vegetarian) diet;
- overhydration;
- muscular dystrophy.
Reduced creatinine levels are often associated with the following conditions:
Return to contents
Change in urea concentration level
An increase in urea concentration is possible:
- Impaired renal excretory function affects the level of urea in the blood.
when the excretory function of the kidneys is weakened, which is caused by glomerulonephritis, pyelonephritis, the use of nephrotoxic medications;
Low urea concentration titers are provoked by:
- impaired synthesis of urea by the liver in various types of hepatitis and cirrhosis;
- hepatic coma;
- poisoning with phosphorus compounds, arsenic;
- a certain period of pregnancy;
- diet therapy;
- overhydration;
- clinical condition after hemodialysis.
Return to contents
Change in uric acid concentration
High titers of uric acid in the blood are associated with the following conditions:
- High levels of uric acid are characteristic of kidney failure.
gout;
A decrease in the amount of uric acid occurs due to:
- hepatocerebral dystrophy;
- Fanconi syndrome (proximal tubule dysfunction);
- Hodgkin's disease (malignant disease of lymphoid tissue);
- taking toxic drugs;
- xanthinuria;
- pathology of the proximal tubules of the kidneys;
- low purine diet.
Return to contents
Potassium
Another important intracellular electrolyte. Its normal content in the body ranges from 3.5 to 5.5 mmol per liter.
Reduced potassium content:
- excess hormones of the adrenal cortex (including taking dosage forms of cortisone);
- chronic fasting (failure to receive potassium from food);
- prolonged vomiting, diarrhea (loss with intestinal juice);
- renal dysfunction;
- cystic fibrosis.
Increased potassium content:
- dehydration;
- acute renal failure (impaired renal excretion); ,
- adrenal insufficiency.
- cell damage (hemolysis - destruction of blood cells, severe starvation, convulsions, severe injuries).
The condition when potassium is elevated is called hyperkalemia, and when it is low, hypokalemia.
Creatinine level
All tests included in the kidney tests are considered as a whole. This allows you to get a complete picture of the condition of the kidneys and related organs. Each indicator has its own significance for diagnosis. Often the results obtained differ slightly in different laboratories. The numbers also vary depending on gender and age.
The level of a healthy person is constant. Normal values are 44–130 µmol/L. This parameter reflects muscle activity. Increased performance may reveal:
- The presence of a number of diseases: chronic pyelonerit, polycystic kidney disease, renal artery stenosis, etc.;
- the use of medications, long-term use of which lead to kidney destruction: aspirin, penicillins, antitumor drugs, etc.;
- shock due to dehydration, blood loss, due to pain and other conditions accompanying acute renal failure;
- excessive physical activity and large consumption of meat products (athletes, etc.);
- serious damage to muscle tissue, for example, in accidents, falls, etc.
If kidney tests show a decrease in levels, the following conditions are possible:
- Increased intensity of blood flow in the kidneys - when taking glucocorticoid drugs;
- pathology in pregnant women - preeclampsia and serious deterioration of filtration;
- long stay without movement, for example, on a bed during illness, when the volume of muscle tissue noticeably decreases (atrophies).
- nephritis;
- tumors, neoplasms;
- anemia;
- glomerulonephritis;
- ulcers, bleeding, etc.
Sodium
Sodium does not directly participate in metabolism. It is completely abundant in the extracellular fluid. Its main function is to maintain osmotic pressure and pH. Sodium excretion occurs in the urine and is controlled by the adrenal hormone aldosterone.
Sodium reduction:
- decreased concentration due to increased fluid volume (diabetes mellitus, chronic heart disease)
- failure, liver cirrhosis, nephrotic syndrome, edema).
- loss of an element (abuse of diuretics, kidney pathology, adrenal insufficiency).
Increased sodium content:
- increased function of the adrenal cortex;
- excess salt intake;
- loss of extracellular fluid (profuse sweat, severe vomiting and diarrhea, increased urination in diabetes insipidus);
- violation of the central regulation of water-salt metabolism (pathology of the hypothalamus, coma).
An increase in a microelement is called hypernatremia, and a decrease is called hyponatremia.
Main symptoms
If a person has any problems with their kidneys, they will experience the following symptoms:
regular increase in blood (arterial) pressure; change in the color of urine, the appearance of impurities in it (including blood) and an unpleasant odor; constant urge to urinate (especially at night); decrease or increase in the volume of urine produced; pain when urinating; sharp or nagging pain in the lumbar region; swelling of the legs and face; constant thirst and decreased appetite; the appearance of shortness of breath.
If the above symptoms appear, it is recommended to undergo examination. With its help, the onset of disease development can be detected in a timely manner. Also, a prerequisite for examination may be taking medications that interfere with kidney function (Acyclovir, Biseptol, diuretics, etc.).
Pain in the lumbar region becomes more intense after hypothermia or with the development of a viral disease.