| Addison's disease | |
| Darkening of the skin on the legs of a white person with Addison's disease | |
| ICD-10 | 27.127.1-27.227.2 |
| ICD-10-CM | E27.1 |
| ICD-9 | 255.4255.4 |
| ICD-9-CM | 255.41 |
| OMIM | 103230 and 240200 |
| DiseasesDB | 222 |
| MedlinePlus | 000378 |
| eMedicine | med/42 |
| MeSH | D000224 |
| Media files on Wikimedia Commons | |
Addison's disease
(
chronic adrenal insufficiency
, or
hypocortisolism
, English Addison's disease) is a rare endocrine disease, as a result of which the adrenal glands lose the ability to produce sufficient amounts of hormones, primarily cortisol.
This pathological condition was first described by British physician Thomas Addison in his 1855 publication entitled Constitutional and Local Effects of Diseases of the Adrenal Cortex
.
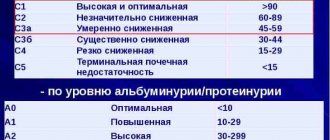
Classification[ | ]
Addison's disease may result from:
Primary insufficiency of the adrenal cortex, primary glandular (in which the adrenal cortex itself is damaged or poorly functioning) - autoimmune aggression, tuberculosis, hypoplasia, tumors or metastases in the adrenal glands, genetic defects in hormone synthesis, decreased sensitivity of the adrenal glands to ACTH.
Secondary adrenal insufficiency, hypothalamic-pituitary - in which the anterior pituitary gland produces insufficient adrenocorticotropic hormone to adequately stimulate the adrenal cortex. Tumors, ischemia, trauma, irradiation of the hypothalamic-pituitary region
Iatrogenic form - after long-term use of exogenous corticosteroids, atrophy of the adrenal glands and rupture of the hypothalamic-pituitary-adrenal connection occurs. When steroids are suddenly stopped, withdrawal syndrome develops.
Etiology and pathogenesis
The pathogenesis of PCNN is based on an absolute deficiency of corticosteroids. The most severe metabolic changes develop due to deficiency of the main mineralocorticoid - aldosterone . This deficiency results in loss of sodium and water through the kidneys and gastrointestinal tract. As a result, dehydration, hypotension and gastrointestinal disorders develop. In severe cases, with the development of severe hyponatremia and hypoosmolarity, transmembrane homeostasis is disrupted with the subsequent development of cellular dehydration. The most severe changes in this regard are observed in the central nervous system and may include progressive impairment of consciousness, coma and death of the patient. In parallel with the loss of sodium and water, potassium retention occurs. In its most obvious form, hyperkalemia is manifested by a disorder of the heart - hyperkalemic myocardial dystrophy. Deficiency of cortisol , the main adaptogenic hormone of the human body, leads to a decrease in resistance to various endo- and exogenous stressors (most often infections), against the background of which decompensation of the disease occurs. Of fundamental importance is the loss of such a function of cortisol as stimulation of gluconeogenesis and glycogenolysis in the liver, as well as the permissive effects of cortisol on thyroid hormones and catecholamines.
Clinical picture[ | ]
Addison's disease usually develops slowly over months or years, and symptoms may go unnoticed or not appear until stress or illness occurs that dramatically increases the body's need for glucocorticoids.
The most common symptoms of Addison's disease are:
- Chronic fatigue, gradually worsening over time;
- Muscle weakness;
- Loss of weight and appetite;
- Nausea, vomiting, diarrhea, abdominal pain;
- Low blood pressure, which decreases further when standing (orthostatic hypotension);
- Hyperpigmentation of the skin in patches in areas exposed to sunlight, known as Addison's melasma;
- Dysphoria, irritability, short temper, dissatisfaction with everything;
- Depression;
- Craving for salty and sour foods, as well as their combinations, thirst, drinking plenty of fluids;
- Hypoglycemia, low blood glucose levels;
- In women, menstruation becomes irregular or disappears; in men, impotence develops;
- Tetany (especially after drinking milk) due to excess phosphates;
- Paresthesia and sensory disturbances in the limbs, sometimes even to the point of paralysis, due to excess potassium;
- Increased number of eosinophils in the blood;
- Excessive amount of urine;
- Hypovolemia (decrease in circulating blood volume);
- Dehydration (dehydration of the body);
- Tremor (shaking of hands, head);
- Tachycardia (rapid heartbeat);
- Anxiety, restlessness, internal tension;
- Dysphagia (swallowing problems).
Tertiary adrenal insufficiency
Chronic deficiency of this type is characterized by the absence of pigment spots. The clinical picture includes weakness throughout the body, attacks of hypoglycemia 2-3 hours after eating.
This condition may occur due to drug therapy administered through suppressive dosage of glucocorticoids; malignant tumors; excessive exposure.
In any case, the patient will have to undergo a diagnostic examination at the clinic. To compensate for the lack of vital substances, the doctor prescribes glucocorticoid hormones and mineralocosticosteroids. Treatment must be supervised.
Addisonian crisis[ | ]
Main article: Addisonian crisis
In some cases, symptoms of Addison's disease can occur unexpectedly quickly. The condition of acute adrenal insufficiency is called “Addisonian crisis” and is extremely dangerous, threatening the patient’s life. The development of Addisonian crisis is most likely in case of untimely recognition of Addison's disease, in patients who did not receive treatment, or who received an inadequately small, insufficient dose of corticosteroids, or in cases where the dose of glucocorticoids was not promptly increased due to illness, stress, surgery, and so on. Thus, any acute illness, blood loss, trauma, surgery or infection can aggravate existing adrenal insufficiency and lead to Addisonian crisis.
In previously diagnosed and adequately treated patients, Addisonian crisis can occur as a result of abrupt cessation of corticosteroid treatment or a sharp reduction in their dose, or when the body's need for glucocorticoids increases (surgery, infections, stress, injury, shock).
Addisonian crisis can also occur in patients who do not suffer from Addison's disease, but who are receiving or have received in the recent past long-term treatment with glucocorticoids for other diseases (inflammatory, allergic, autoimmune, etc.) with a sharp reduction in the dose or sudden withdrawal of glucocorticoids, as well as with an increase the body's needs for glucocorticoids. The reason for this is the inhibition of the secretion of ACTH and endogenous glucocorticoids by exogenous glucocorticoids, the gradually developing functional atrophy of the adrenal cortex during long-term glucocorticoid treatment, as well as a decrease in the sensitivity of tissue receptors to glucocorticoids (desensitization) during therapy with supraphysiological doses, which leads to the patient’s dependence on the intake of exogenous glucocorticoids into the body (“steroid addiction”).
Symptoms of Addisonian crisis[ | ]
- Sudden severe pain in the legs, lower back, or abdomen;
- Severe vomiting, diarrhea, leading to dehydration and the development of shock;
- a sharp decrease in blood pressure;
- loss of consciousness;
- Acute psychosis or confusion, delirium;
- a sharp decrease in blood glucose levels;
- Hyponatremia, hyperkalemia, hypercalcemia, hyperphosphatemia;
- Brown plaque on the tongue and teeth due to hemolysis and the development of iron deficiency.
Prevention
According to statistics, more than eighty percent of cases of the disease are caused by stress or depression, so it is very important for the health of the body to avoid situations that cause such a reaction. It is very important to maintain a healthy lifestyle, eat right, and undergo periodic examinations.
If you suspect that your adrenal glands or kidneys are hurting, it is very important not to self-medicate or ignore the first symptoms of the disease. Only timely treatment will make it possible to nip the development of the disease in the bud.
Prevalence[ | ]
The prevalence of Addison's disease in the human population is estimated to be approximately 1:100,000 population.[1] According to other data, the prevalence of Addison's disease per 1 million population is 40-60 cases in the USA, 39 cases in the UK and 60 cases in Denmark[2]
Determining the exact number of patients with adrenal insufficiency is problematic at best, since many patients with relatively mild symptoms never seek medical attention and remain undiagnosed.[3]
Addison's disease can develop in people of any gender, any ethnicity, and at any age. However, the onset of the disease is most typical in adults between 30 and 50 years of age. Some studies suggest that women are slightly more likely than men to develop Addison's disease, and it tends to be more severe in women. Studies have not found any association between ethnic origin and the incidence of Addison's disease.[2]
Hypercorticism symptoms in women
- The most common symptom that occurs in almost all patients with this pathological condition is obesity. It is characterized by an uneven distribution of fat relative to the human body. Most of them are found in the face, neck, chest and abdomen.
At the same time, the legs have practically no deposits. The face is characterized by rounded contours, as it is also called moon-shaped, the skin has a purple tint. - Itsenko-Cushing syndrome causes symptoms in women (photo attached) in the form of increased facial hair, menstrual irregularities, and infertility.
- As a result of atrophic processes in the muscles, the formation of hernias occurs, including the white line of the abdomen, enlargement of the abdomen due to muscle hypotonia, sloping buttocks, wasting of the muscles of the thighs and legs.
- The skin has a marbled tint and hyperpigmented areas are visible.
- As a result of osteoporosis, various curvatures of the spinal column are formed in the form of scoliosis and kyphosis. Frequent fractures are observed.
- Due to the involvement of the myocardium in the process, cardiomyopathies, extrasystoles, hypertensive disorders, and heart failure are observed.
Treatment[ | ]
Hormone replacement therapy is prescribed to treat Addison's disease. If there is a lack of cortisol, hydrocortisone is prescribed; with a reduced content of the mineral corticosteroid aldosterone - fludrocortisone acetate tablets (Florinef, Cortineff). You may need to reduce your salt intake while taking fludrocortisone. Typically, patients with secondary adrenal insufficiency do not need to take mineralcorticosteroids because this adrenal function is preserved. The dose of the drug is selected individually for each patient and is usually 50-200 mcg (0.05 - 0.2 mg).
During Addisonian crisis, there is a drop in blood pressure and blood glucose levels, as well as an increase in potassium levels, which can threaten the patient's life. Typically, during Addisonian crisis, intravenous hydrocortisone, saline (0.9% NaCl) and dextrose (sugar) are administered. In this case, a sharp improvement usually occurs. When the patient is able to drink and take medications by mouth, the amount of hydrocortisone is reduced, maintaining only a maintenance dose. If there is a lack of aldosterone, maintenance therapy with fludrocortisone acetate is prescribed.
Itsenko-Cushing syndrome: treatment
The main goals of treatment for PUI are:
- Select the regimen and dose of glucocorticoids so that they best correspond to the physiological and circadian rhythm of cortisol
- Avoid the development of adrenal crisis
- Avoid chronic overdose and its long-term undesirable effects (osteoporosis, increased cardiovascular risks, metabolic syndrome)
- Improve the patient’s quality of life by ensuring his psychosocial adaptation
- Hydrocortisone therapy is recommended.
Level of strength of recommendation B. Level of certainty of evidence 1.
Therapy for this pathological condition depends on the pathogenetic level of its occurrence.
If drug-induced hypercortisolism is identified, then the main direction is to discontinue glucocorticoid drugs. Drugs that suppress the secretion of glucocorticoids are also prescribed.
When diagnosed with Cushing's disease, treatment, as with adrenal tumors, is carried out in the form of removal of the tumor. In the absence of the possibility of surgical correction, in some cases doctors are forced to resort to removal of the adrenal glands. In some cases, combined treatment with radiation and chemotherapy is carried out.
Of course, in addition to etiotropic therapy, treatment is necessary aimed at relieving the symptoms caused by such hormonal disorders and their consequences. Such treatment may include the prescription of antihypertensive drugs, cardiac glycosides in the event of heart failure, hypoglycemic treatment, immunomodulators to increase the body's protective properties. That is, maintaining the basic vital functions of the human body.
Heredity[ | ]
There are several different causes that can lead to the development of Addison's disease, and some of them have a hereditary component. The most common cause of Addison's disease in the United States and Western Europe is autoimmune destruction of the adrenal cortex. The tendency to develop this autoimmune aggression against the tissues of one's own adrenal glands is most likely inherited as a complex genetic defect. This means that for the development of such a condition, an “orchestra” of several different genes is needed, interacting with as yet unidentified environmental factors.
2.5. Differential diagnosis
Algorithm for differential diagnosis of primary CIU
In order to determine the nosological form of CNN, it is necessary to evaluate:
- Age of manifestation of adrenal insufficiency
- Presence of glucocorticoid and mineralocorticoid components
- Family history
- Presence of other clinical components
In the absence of additional clinical components that suggest the etiology of CIU, it is necessary:
- All boys with the onset of CLI after the age of three years should have a VLCFA (very long chain fatty acid) study to rule out X-linked adrenoleukodystrophy [BI]
- For patients of both sexes with the onset of the disease after the age of three years, conduct a study of antibodies to 21-hydroxylase [BI]
- Conduct genetic studies to identify mutations in known genes responsible for the development of adrenal insufficiency [BIII]
Table 2. Hereditary variants of primary CNN.
| Primary CNN (age of manifestation) |
| Diagnosis | Gene |
| After 3 years |
| Autoimmune polyglandular syndrome type 1 | AIRE |
| Autoimmune polyglandular syndrome type 2 | ||
| X-linked adrenoleukodystrophy | A.L.D. | |
| Familial isolated glucocorticoid deficiency | MC2R, MRAP, MCM4, NNT, STAR ALADIN | |
| Up to 3 years |
| Congenital dysfunction of the adrenal cortex | StAR, CYP11A1 3bGDM, CYP17, CYP21, CYP11B1, POR, |
| Allgrove syndrome (Triple A) | ALADIN | |
| Smith-Lemli-Opitz syndrome | DHCR7 | |
| Congenital X-linked adrenal hypoplasia | DAX gene, X chromosome deletion | |
| IMAGe syndrome |
Links[ | ]
- Addison's disease // Encyclopedic Dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907.
- [da-med.ru/diseases/cat-87/d-169/ Da-med.ru ::: Addison's disease (Bronze disease)]
- Addison disease – Geneva Foundation for Medical Education and Research
- Overview of Addison's Disease from the Mayo Clinic
- Addison's Disease Research Today — monthly online journal summarizing recent primary literature on Addison's disease
- National Adrenal Diseases Foundation
- eMedicine/WebMD article on Addison's disease
- Addison's information from MedicineNet
- "Addison's Disease: The Facts You Need to Know (MedHelp.org)
- The Addison & Cushing International Federation (ACIF)
- Addison's disease info from SeekWellness.com
- Information about Addison's disease in canines (dogs)
- More information about Addisonian crisis for children over 4 years old https://www.youtube.com/watch?v=MNVPMEV4heQ
- More information about Addisonian crisis for children over 12 years old https://www.youtube.com/watch?v=brtP2DqZiEk
Bibliography
UI – adrenal insufficiency
CFI - chronic adrenal insufficiency
PNF – primary adrenal insufficiency
CRH – corticotropin releasing hormone
ACTH – adrenocorticotropic hormone
PRA – plasma renin activity
VCFA - very long chain fatty acids
APS – autoimmune polyendocrine syndrome
CAI – congenital dysfunction of the adrenal cortex
- Orlova E.M., Kareva M.A. "Primary adrenal insufficiency in children: clinical options, diagnosis, treatment." Methodological manual for doctors 2008
- Handbook of a pediatric endocrinologist/Dedov II, Peterkova VA, Shiryaeva TYu, Bezlepkina OB, Kareva MA, Kuraeva, Nagaeva EV, Orlova EM, Strebkova NA. – M: Littera, 2011 – 528 p.
- Pediatric Adrenal Diseases Workshop, Turin, May 2010 Ghizzoni L. (Turin) Cappa M. Chrousos GP Loche S. Maghnie M, Karger, 2011
- Husebye ES, Allolio B, Arlt W, Badenhoop K, Bensing S, Betterle C, Falorni A, Gan EH, Hulting AL, Kasperlik-Zaluska A, K?mpe O, L?v?s K, Meyer G, Pearce SH. Consensus statement on the diagnosis, treatment and follow-up of patients with primary adrenal insufficiency. J Intern Med. 2014 Feb;275(2):104-15
- Grossman A, Johannsson G, Quinkler M, Zelissen P. Therapy of endocrine disease: Perspectives on the management of adrenal insufficiency: clinical insights from across Europe. Eur J Endocrinol. 2013 Oct 21;169(6):R165-75
- Horn MA, Erichsen MM, Wolff AS, M?nsson JE, Husebye ES, Tallaksen CM, Skjeldal OH.
Screening for X-linked adrenoleukodystrophy among adult men with Addison’s disease. Clin Endocrinol (Oxf). 2013 Sep;79(3):316-20
- Meyer G, Hackemann A, Penna-Martinez M, Badenhoop K. What affects the quality of life in autoimmune Addison’s disease? Horm Metab Res. 2013 Feb;45(2):92-5
- Engelen M, Kemp S, de Visser M, van Geel BM, Wanders RJ, Aubourg P, Poll-The BT X-linked adrenoleukodystrophy (X-ALD): clinical presentation and guidelines for diagnosis, follow-up and management. Orphanet J Rare Dis. 2012 Aug 13;7:5
- Meimaridou E, Hughes CR, Kowalczyk J, Chan LF, Clark AJ, Metherell LA ACTH resistance: genes and mechanisms. Endocr Dev. 2013;24:57-