Home Genitourinary diseases Difficulty urinating
- Types of disease
- Causes
- Diagnosis and treatment
Hematuria code according to ICD 10 is a serious illness characterized by the presence of blood in the urine. Modern medicine knows about two hundred reasons why blood may be present in urine, some of them may indicate simple malfunctions in the body, while others are signs of the development of dangerous diseases. For this reason, one cannot help but pay attention to the presence of blood or even blood clots in the urine. First, you need to immediately contact a medical institution, where a specialist will conduct a diagnosis and draw up a treatment plan.
brief information
1.1 Definition
Hematuria is a condition characterized by blood in the urine more than the physiological norm.
Hematuria - release of red blood cells:
>3 on urine sediment microscopy in 2 out of 3 tests; >1000 in 1 ml of average urine according to Nechiporenko.
1.2 Etiology and pathogenesis
Causes of hematuria:
- urinary tract tumors
- BPH
- ICD
- PCa
- injuries
- inflammatory processes of the urinary tract
- kidney disease (glomerulonephritis)
Categories of risk factors
Nephrological disease:
- proteinuria >0.5 g/day;
- signs of renal failure;
- altered red blood cells in the sediment;
- cylindruria;
- elevated serum creatinine.
Urological disease:
- smoking;
- occupational hazards (dyes, etc.);
- over 40 years old;
- history of symptoms or urological disease;
- history of urinary disorders;
- recurrent UTIs;
- long-term use of analgesics;
- history of pain radiating to the pelvic area;
- long-term history of the presence of a foreign body.
1.3 Epidemiology
The prevalence of microhematuria ranges from 2.4 to 31.1%, more often in men over 60 years of age and in smokers/former smokers.
Age-specific prevalence of microhematuria:
- up to 12 years 1–4%;
- men 18–33 years old 5.2%;
- over 50 years old men 4–18%, women 14%;
- over 75 years old men 13%, women 9%.
With hematuria, diseases requiring treatment are identified in 3.4–56%.
1.4 Coding according to ICD 10
N02 – Recurrent and persistent hematuria
R31 – Nonspecific hematuria
1.5 Classification
By intensity:
- macrohematuria - visible blood, more than 0.5 ml of blood in 500 ml of urine;
- microhematuria – more than 3 red blood cells in the field of view.
By etiology:
- extraglomerular origin (tubulointerstitial diseases);
- glomerular origin.
Types and degrees
The classification of hemorrhoids depends on the location, size and number of nodes (bumps) formed. There are internal, external and mixed hemorrhoids, and according to the degree of manifestation of symptoms, four stages of this disease are distinguished.
Classification of hemorrhoids:
- The first stage is characterized by bloody discharge from the anus, periodic pain and difficulty defecating.
- In the second stage, changes affect internal hemorrhoids, which can fall out during bowel movements, but spontaneously retract.
- In the third stage, prolapse of hemorrhoids is almost constant; in some cases, self-reduction is acceptable.
- The fourth stage is characterized by a strong increase in hemorrhoids, inflammation of the anus and nearby tissues.
As the disease progresses, pain and bleeding increase, symptoms of anemia and intoxication of the body appear.
Chronic hemorrhoids affect all aspects of life; from the inflammatory process in the anus, the infection can be transmitted to the abdominal organs, digestion, and genitourinary system.
Diagnostics
“Benign” causes of asymptomatic microhematuria that do not require a full examination:
- strength exercises,
- chronic kidney disease,
- infectious or viral diseases,
- menstruation,
- injuries,
- recent urological manipulations.
If pathologies are identified, appropriate treatment is carried out, with a repeat examination upon completion.
Examination for asymptomatic microhematuria to exclude “benign” causes:
- careful collection of anamnesis,
- physical examination,
- laboratory research.
2.1 Complaints and anamnesis
Diagnosis of hematuria is based on complaints of blood admixture or detection of formed elements in the analysis.
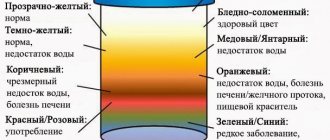
Change the color of urine
medicines:
- pink - pyramidon;
- saffron yellow - nitroxoline;
- brown - senna;
- raspberry - phenolphthalein;
- red-brown - madder.
products:
- raspberry - beets;
- brown - rhubarb.
diseases and conditions:
- brick - acute porphyria;
- red-brown - myoglobinuria with prolonged compartment syndrome.
Blood clots:
- vermiform - from the upper urinary tract;
- large shapeless ones - the bladder.
Blood staining:
- only the initial portion - initial hematuria after injury, inflammation or tumor of the urethra;
- all portions - total hematuria in diseases of the urinary system and prostate;
- at the end of urination - terminal hematuria with pathology of the bladder neck, cystitis, urethrotrigonitis, prostatitis, pathology of the seminal tubercle.
Localization of pain syndrome:
- in the lumbar region on the affected side to hematuria - a stone in the ureter;
- pain after hematuria - obstruction of the ureter by clots;
- difficulty urinating after the appearance of blood in the urine - bladder tamponade.
It is necessary to clarify:
- conditions contributing to the appearance of hematuria;
- travel to tropical countries (schistosomiasis, malaria);
- family history of hereditary diseases (Fabry disease, Alport disease, etc.);
- previously suffered tonsillitis, urolithiasis, bladder tumor, etc.;
- taking medications (aminoglycosides, amitriptyline, NSAIDs, penicillins, diuretics, contraceptives, antimalarials, anticonvulsants, cyclophosphamide, antiplatelet agents, anticoagulant).
The intensity of hematuria does not correlate with the severity of the disease.
2.2 Physical examination
Note:
- hemorrhagic rashes in diseases of the hemostatic system, hemorrhagic fever with renal syndrome;
- edema, increased blood pressure in nephrological diseases;
- increased body temperature during infections;
- enlarged lymph nodes due to infections, blood diseases, cancer.
Recommended:
- palpation of the abdomen to detect an enlarged liver, spleen, tumor of the abdominal cavity and retroperitoneal space;
- digital rectal examination of men;
- vaginal examination;
- examination of the external urethral opening.
2.3 Laboratory diagnostics
In the absence of any obvious benign disease, a properly collected urine sample is examined.
A positive blood dipstick test does not allow a diagnosis of asymptomatic microhematuria, but is a reason for urine microscopy.
The main diagnostic method is a general urine test .
To make a diagnosis, microscopic examination of urinary sediment .
In case of questionable proteinuria, studies on the selectivity of proteinuria are necessary.
Phase-contrast microscopy of sediment allows topical diagnostics:
- unchanged red blood cells in pathology of the lower urinary tract, ureter or pyelocaliceal system;
- altered red blood cells and casts in nephrological disease;
- leukocyturia and pyuria - UTI.
If changes are detected in urine analysis, a bacteriological study with determination of sensitivity to antibiotics is indicated.
Pyuria with repeated negative results of bacteriological examination is an indication for a urine test for Mycobacterium tuberculosis, a chest x-ray and consultation with a phthisiatrician.
The first morning urine, as well as urine after heavy physical or sexual activity, is not suitable for diagnosing microhematuria.
Performing a 3-glass test:
- with isolated hematuria in the first portion - the source is in the urethra;
- with isolated hematuria in the third portion - in the neck of the bladder.
A clinical blood test is recommended to detect anemia.
Biochemical blood test : total protein, glucose, creatinine, urea, PSA.
At the first hospitalization, renal function is assessed by GFR, creatinine and urea levels.
cytology for persistent microhematuria and difficulties with standard diagnosis or risk factors for carcinoma in situ.
It is not recommended to include the assessment of markers in urine in the diagnostic algorithm.
2.4 Instrumental diagnostics
Ultrasound of the kidneys, bladder, prostate gland for gross hematuria.
MSCT to detect urinary tract pathology.
If MSCT is not possible, excretory urography .
If MSCT is contraindicated, an alternative method is magnetic resonance (MR) urography .
Regardless of age, cystoscopy .
To exclude urological causes of asymptomatic microhematuria after 35 years, cystoscopy is recommended.
Blue light fluorescence cystoscopy is not recommended for asymptomatic microhematuria.
Ureteropyeloscopy will reveal tumors of the ureter or renal pelvis.
If there is a tumor, a biopsy is performed .
2.5 Other diagnostics
Consultation with a urologist and nephrologist for microhematuria due to anticoagulants.
Symptoms (signs)
Clinical manifestations
• Caused by the underlying disease.
• Complaints about the release of red (brown, dark, “coffee”, “tea” colored) urine - gross hematuria •• Hematuria at the beginning of urination (initial) - damage to the initial part of the urethra •• Hematuria at the end of urination (terminal) - damage to the prostate, cervical part of the bladder, internal opening of the urethra •• Total hematuria (in all portions of urine) - diseases of the bladder, ureters, renal pelvis.
Treatment
The goal is to eliminate the cause of hematuria.
3.1 Conservative treatment
For ongoing hematuria, hemostatic drugs .
For hematological diseases, treatment with blood components or transfusion of fresh frozen plasma is recommended, depending on the defect in the hemostatic system.
For infectious and inflammatory diseases of the urinary system, antibacterial, anti-inflammatory and infusion-detoxification therapy is carried out.
For nephrological diseases, pathogenetic therapy with glucocorticoids and cytostatics is recommended.
3.2 Surgical treatment
The goal is to completely stop the bleeding.
Indications:
- recurrent hematuria caused by urological diseases requiring surgical intervention (tumors, strictures, stones);
- macrohematuria leading to anemia, bladder tamponade - emergency surgery.
Treatment of the underlying disease causing hematuria is recommended.
In case of relieved hematuria, planned surgical treatment of the underlying disease is performed.
If bleeding continues, emergency surgery is required.
For hematuria complicated by tamponade, it is recommended to wash the bladder of clots.
For incurable disease and ongoing bleeding, minimally invasive surgical methods are preferred.
Causes of hemorrhoids
Most often, hemorrhoidal bleeding is a consequence of damage to internal hemorrhoids during defecation. This is mainly observed with prolonged constipation and excessive straining. Hemorrhoidal bleeding is preceded by thinning of the walls of the node, which is a consequence of blood stagnation and disruption of local venous blood flow. As a result, small tears and erosions form, which lead to bleeding. Among the etiological factors, one can also identify a violation of the outflow of blood through the venules from the cavernous bodies in the walls of the rectum, the presence of branched cavernous bodies, congenital functional underdevelopment of connective tissue, changes in the innervation of the venous wall.
Risk factors that can lead to the development of hemorrhoidal bleeding include increased pressure in the vein system due to constipation, prolonged sitting or standing, heavy physical work, or pregnancy. Regular abuse of alcoholic beverages and spicy foods can also lead to this condition. Hemorrhoidal bleeding also develops against the background of liver cirrhosis with concomitant portal hypertension.
Experts identify the following causes of the disease:
- Obesity;
- Great physical activity;
- Physical inactivity;
- Hereditary predisposition;
- Nervous tension;
- Problems with blood flow in the rectum;
- Chronic constipation;
- Inflammation and tumors in the intestines and liver;
- Infectious infection;
- Frequent sexual intercourse through the anus;
- Smoking.
The main cause of the disease is considered to be an increased or congenital tendency to form blood clots, as well as vascular pathology. Due to the increased blood flow to the rectum and weakened outflow, it fills and stretches the damaged veins, which ultimately leads to the formation of a node that grows and becomes inflamed over time.
In women, hemorrhoids are often caused by pregnancy and childbirth (in almost every second woman after childbirth, doctors diagnose various forms of this disease). And since it is difficult to treat during pregnancy (this is associated with a risk to the fetus when using various drugs), a woman should visit a proctologist even at the stage of pregnancy planning.