Interstitial nephritis (otherwise known as tubulointerstitial nephropathy, tubulointerstitial nephritis) belongs to the category of immunoinflammatory diseases and is a pathological process that affects a special type of connective tissue in the kidneys - interstitial. In this case, as a result of inflammation, the tubular apparatus of the nephrons is affected.
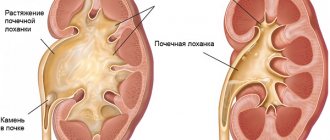
Despite the similarity with a fairly large number of nephropathic diseases, interstitial nephritis stands out as a separate nosological unit, which meets a number of specific diagnostic criteria, but nevertheless still remains little known to practitioners. As with pyelonephritis, the interstitial (loose fibrous connective) tissue and renal tubules are affected, however, no destructive changes are noted in the kidney tissues, and the renal cups and pelvis (that part of the organ that is responsible for removing ready urine from it) are not affected by the pathological process. Due to the absence of pronounced pathognostic symptoms of interstitial nephritis, as well as the laboratory criteria inherent specifically to this disease, clinical diagnosis in most cases is a rather difficult task, therefore, the most convincing method for determining the disease is currently considered to be taking a biopsy sample through a puncture (puncture of the test subject). formation with a hollow medical needle).
Certain diagnostic difficulties do not make it possible to speak with confidence about the prevalence of the disease, but in the medical literature of the last few decades there has been a persistent tendency towards an increase in the incidence of its occurrence. The reason for this is considered not only to be the modernization of diagnostic methods and medical equipment, but also to a more intense influence on the kidneys of factors that determine the development of interstitial nephritis.
General information
A feature of interstitial nephritis is the involvement of blood vessels and tubular structures in the process without involvement of the pyelocaliceal system and destruction of the organ. Since tubular dysfunction is of significant importance in the pathogenesis, the pathology was given another name - tubulointerstitial nephritis (TIN). According to research data, the acute version of the disease accounts for up to 20% of cases of organ damage, and the chronic version accounts for up to 12%.
The main cause of tubulointerstitial nephritis is considered to be congenital kidney defects. Another process is determined by the penetration of pathogenic microflora into the body, metal intoxication, and injuries. Tubulointerstitial nephritis is most often provoked by the following factors:
- long-term use (Sedalgina, Analgina, Pentalgina);
- uric acid diathesis;
- abnormalities in the development of renal structures.
The prolonged course of the pathology is accompanied by changes in the tissues of the organ, which is fraught with acute renal failure.
Regardless of what triggered tubulointerstitial nephritis, it must be treated adequately and on time. This is the only way to prevent complications. Do not hesitate to consult a doctor or try to eliminate the pathology yourself.
Treatment options
There is practically no treatment for the acute form of the disease at home. Even with a favorable course of nephritis, when there are no severe manifestations, hospitalization is recommended. In a hospital setting, the patient will be under constant supervision, which will help prevent the development of complications.
The disease can be treated only after the factors that caused it have been eliminated. It is necessary to discontinue those drugs that could provoke such a condition - antibiotics, non-steroidal anti-inflammatory drugs, etc.
Often this action alone helps eliminate the main symptoms of the disease. But recommendations still include strict bed rest for at least the first 2-3 weeks.
Diet plays an important role. When sick, the amount of salt is limited. The protein content in the diet is being reviewed - such recommendations are developed on an individual basis, depending on the level of azotemia (high levels of nitrogenous metabolic products in the blood) in a person. Smoked meats, canned food, fatty meats and fish, salty and spicy foods are prohibited.
Treatment of interstitial nephritis begins with the abolition of medications that provoked the disease. Then it is necessary to speed up the elimination of this drug from the body. At the same time, symptomatic treatment is carried out. With the “abortive” form, it is usually enough to take a course of calcium gluconate, rutin and vitamin C.
The patient must be treated inpatiently, strictly observing bed rest. In addition to basic therapy, it is important to maintain normal electrolyte levels and monitor the acid-base balance.
If the disease is severe, it is necessary to reduce swelling as soon as possible. For this purpose, glucocorticoids and antihistamines are prescribed. Sometimes drug overdoses and intoxications occur. In such cases, the medicine is quickly eliminated from the body using one of the available methods:
- hemosorption;
- antidotes;
- hemodialysis.
Treatment of chronic interstitial nephritis is primarily aimed at eliminating the causes that provoked the disease. The patient is prescribed restorative therapy, medications and vitamins. For necrosis, special medications are used:
- Trental;
- salurtiki;
- Heparin;
- antibiotics.
If treatment does not produce results within two days, the patient is prescribed glucocorticosteroids - hormonal drugs. It is important for the patient to ensure high-quality hydration: increase the volume of water and liquid injected into the vein with increased urination, and reduce with decreased urination.
Quite often, when tubulointerstitial nephritis is detected, treatment involves stopping the use of those medications that may have caused the development of this pathology.
Further, if improvement does not occur after stopping the medications for several days, hormonal glucocosteroid drugs may be included in the treatment process.
Particularly important during periods of treatment of a patient with tubulointerstitial nephritis is an increase in water consumption at times of increased fluid release from the body against the background of polyuria. In the absence of such a phenomenon, the daily fluid rate is reduced.
Drugs are prescribed taking into account the functionality of the kidneys. Excluding those medications that, when used, can disrupt the functioning of the organ.
If the disease has gone far enough that the patient is diagnosed with acute renal failure, characterized by partial or complete failure of both kidneys. A procedure is prescribed to cleanse the body of toxic substances, hemodialysis, which involves connecting the patient to an “artificial kidney” machine.
Causes
There are many factors influencing changes in kidney function and the appearance of TIN. Non-purulent interstitial inflammation of the organ is caused by:
- Systemic processes and metabolic disorders - sarcoidosis, Sjogren's syndrome, hyperuricemia.
- Bacterial and viral pathologies - diphtheria, streptococcal infection, leptospirosis, cytomegalovirus.
- Obstruction of the urinary tract.
- Granulomatous diseases.
- Intoxication.
- Exposure to ionizing radiation;
- Taking certain medications - diuretics, NSAIDs (non-steroidal anti-inflammatory drugs), sulfonamide and fluoroquinolone antibiotics. The disease can develop as a result of the use of Cephalotin, Allopurinol. Ampicillin, Ibuprofen, Captopril, Penicillin, Phenytoin.
Since the signs of TIN are similar to the manifestations of other nephrological processes, if you have suspicious symptoms, you should go to the hospital.
Causes of the disease
Interstitial nephritis can be the result of a fairly wide range of pathological conditions.
Factors contributing to the development of acute interstitial nephritis:
- the presence of infectious processes in the body;
- lymphoproliferative pathologies;
- diathesis of an allergic nature;
- introduction of protein preparations into the body;
- chemical intoxication of the body. substances;
- diseases that affect connective tissue.
Factors contributing to the occurrence of chronic interstitial nephritis:
- autoimmune diseases:
- chronic intoxication of the body;
- diseases during which granulomatous inflammation develops. For example, sarcoidosis or tuberculosis;
- disturbances in the development of kidney tissue;
- taking painkillers and non-preventive medications for a long period of time;
- various anomalies of the urinary system;
- congenital disorders of oxalate and urate metabolism.
Pathogenesis
Tubulointerstitial nephritis is often provoked by blood diseases, intoxication, rejection of transplants by the body, and systemic pathologies. Due to the influence of one or another factor, the intermediate tissue of the kidney swells, the vessels contract (with spasm), which leads to ischemia of the organ.
Tubulointerstitial nephritis is accompanied by increased blood pressure and an increase in the concentration of creatinine in the blood. Following ischemia, necrosis of the renal papillae often occurs. Deterioration of the tubules and interstitium leads to a significant increase in urine volume. Tubulointerstitial nephritis is also characterized by damage to the medulla, which is accompanied by the formation of additional foci of inflammation, as well as disruption of the parenchyma.
With the prolonged presence of damaging agents and persistent ischemia against the background of blood flow disorders, the appearance of irreversible changes in the epithelium is noted (connective tissue fibers replace functional ones).
Tubulointerstitial nephritis, if left untreated, leads to serious complications. To prevent them, you need to consult a doctor at the first alarming symptom and undergo an examination.
Diagnosis and treatment of interstitial cystitis in women
Have you been trying to cure your KIDNEYS for many years?
Head of the Institute of Nephrology: “You will be amazed at how easy it is to heal your kidneys just by taking it every day...
Read more "
Interstitial cystitis is a chronic form of inflammation of the bladder. The disease is accompanied by damage to the mucous membrane of the organ, as a result of which urine components penetrate into the intermediate tissue (interstitial), irritate the nerve endings, causing acute pain and the urge to urinate.
Causes and symptoms of the disease
Scientists have not fully elucidated the cause of the development of pathology. The provoking factor is considered to be a weakened immune system, a deficiency of glycosaminoglycans that cover the inner wall of the bladder. As a result, irritants can penetrate the mucous membrane, causing symptoms of interstitial cystitis. Women suffer from the disease 10 times more often than men. Children and older people are less susceptible to developing pathology.
Characteristic features:
- frequent urge and urination in small portions;
- cutting pain in the lower abdomen;
- burning sensation in the urethra;
- feeling of incomplete emptying of the bladder;
- urge to go to the toilet at night;
- blood in the urine;
- urine is cloudy, with an unpleasant odor;
- pain in the pelvis, radiating to the lumbar region;
- painful sexual intercourse, decreased libido;
- increased body temperature;
- nausea, vomiting;
- general malaise;
- increased symptoms before the onset of menstruation.
Irritants penetrate the bladder wall and cause the release of histamine from mast cells, which leads to irritation of tissues and nerve endings. The chronic process leads to the formation of scars on the walls of the bladder, which provokes a decrease in the elasticity and overall functioning of the organ. Symptoms of cystitis can manifest themselves in different ways, sometimes the urge to go to the toilet occurs every 20-30 minutes, and the feeling of fullness of the bladder persists even after visiting the restroom.
The filling of the bladder is accompanied by ruptures of the mucous membrane and interstitial tissue, in this place a blood clot forms and fibrin accumulates. Such lesions are called Hunner's ulcers, which are most often localized in the upper part of the bladder.
Sometimes the painful symptoms of interstitial cystitis go away without any treatment, and remission remains for a long time. But most often the disease is progressive.
Diagnosis of interstitial cystitis
Interstitial cystitis is quite difficult to diagnose, since the disease does not have pronounced symptoms for a long time. One effective method is cystoscopy. This is an instrumental examination of the bladder using a cystoscope equipped with a video camera. The analysis helps to assess the condition of the mucous membrane, identify the presence of inflammation, ulcers, scars; if necessary, a piece of tissue is immediately taken for cytological examination.
Another method for diagnosing interstitial cystitis is hydrodistension. The bladder is filled with fluid and the elasticity of the walls of the organ is checked. The disease is confirmed if the extensibility is low, cracks and hemorrhages appear. For medicinal purposes, antibiotics and vitamins are injected into the bladder cavity.
A potassium test is performed together with cystoscopy. Potassium chloride is injected into the cavity of the bladder; the drug does not cause pain in healthy people. But with sprains or ulcers, the remedy penetrates into the intervening tissue, the urge to urinate appears and the lower abdomen begins to hurt severely.
Traditional methods of treating interstitial cystitis
Therapy is aimed at eliminating the inflammatory process, relieving pain and restoring bladder function.
Non-steroidal anti-inflammatory drugs are used for this:
- Moment;
- Indomethacin;
- Diclofenac.
Since damage to the mucous membrane during interstitial cystitis provokes an allergic reaction, patients are prescribed antihistamines (Diazolin, Suprastin). To relieve inflammation, broad-spectrum antibiotics are taken in combination with antifungal agents.
Strengthens the mucous membrane Elmiron, sodium pentosan polysulfate, these drugs prevent the development of thrombosis and tissue scarring. Treatment is long-term and can take up to 6 months.
Conventional anesthetics are ineffective for interstitial cystitis, since the pain syndrome is caused by irritation of the nerve endings. Therefore, patients are prescribed antidepressants and anticonvulsants. Additional methods of therapy include physiotherapeutic procedures:
- electromyostimulation;
- massage;
- exercises to strengthen the pelvic floor muscles.
To strengthen the immune system, it is useful to take vitamin and mineral complexes (Duovit, Complevit), immunomodulating drugs (Echinacea, Imudon), herbal teas, decoctions and infusions.
The folk way to cleanse the kidneys! Our grandmothers were treated using this recipe...
Cleaning your kidneys is easy! You need to add it during meals...
Patients must follow a special diet that excludes foods rich in potassium: legumes, apricots, bananas, melon. It is also recommended to limit the amount of food that can irritate the bladder mucosa:
- alcohol;
- carbonated drinks;
- coffee;
- hot spices.
It is necessary to increase the volume of fluid consumed; during the day you need to drink 2-3 liters of clean, still water.
Surgical method of therapy
Surgical treatment of interstitial cystitis is indicated when there is a significant decrease in bladder volume against the background of progressive pathology. Partial excision or augmentation cystoplasty of the urinary organ is performed. The doctor forms a new bladder from part of the small or large intestine, the reservoir is connected to the urethra or an artificial outlet of urine is formed on the anterior wall of the abdominal cavity.
In such cases, the patient needs to empty the new bladder several times a day using a catheter, since the natural urge disappears after the operation. It is important to perform the procedures regularly to avoid rupture of an overfilled bladder.
Treatment of cystitis with traditional medicine recipes
In addition to traditional therapy, folk remedies can be used. For their preparation, medicinal herbs are used that have anti-inflammatory, strengthening and diuretic properties.
Recipe for interstitial cystitis
Take the root in equal proportions:
- cinquefoil;
- horsetail;
- licorice;
- large plantain.
One tablespoon of the mixture is poured into 0.5 liters of boiling water and left for 2 hours. Then the broth is filtered and taken 1/3 cup 3 times a day.
Recipe for cystitis from the newspaper “Doctor I-Bolit”: you will need St. John’s wort oil, you can buy it at the pharmacy, 1 kg of potatoes. Root vegetables must be washed and boiled in their skins; after cooking, they are kneaded and transferred to a bucket. A woman needs to sit on top and wrap herself in a warm blanket; she should steam for 30–40 minutes. Then St. John's wort oil is smeared on the lower abdomen above the pubis, cling film is applied, covered with a towel and left until the morning. The procedure is done every evening before bed for 5 days.
Interstitial cystitis can be treated using the following recipe: 2 tablespoons of elderberry inflorescences are poured into 250 ml of boiling water, kept in a steam bath for 15 minutes, then wrapped and left for 2 hours. The broth is filtered and taken 1 tablespoon 3 times a day 30 minutes before meals. Therapy is carried out for 14 days, after which they take a break for 1 week and repeat the treatment again.
Interstitial cystitis is a chronic progressive disease of the urinary system. Without timely treatment, the disease leads to bladder atrophy and incontinence. Therapy is performed by taking medications and performing physiotherapeutic procedures. In severe cases, surgery is indicated. In addition to the main treatment, you can use traditional medicine recipes.
Classification
There are several types of interstitial inflammation. Each has its own manifestations. A doctor can distinguish this disease from pyelonephritis, for example, or say exactly in what form it occurs.
Table - TIN classification
| Kinds | Description | |
| According to the nature of the flow | Spicy | Acute tubulointerstitial nephritis is characterized by the following symptoms:
|
| Chronic | When acute interstitial nephritis transitions to chronic, tissue fibrosis occurs. The pathology is accompanied by death of the tubules and damage to the glomeruli | |
| By mechanism of appearance | Primary | The development of acute tubulointerstitial nephritis occurs independently. Other pathologies do not affect the occurrence of inflammation |
| Secondary | Triggered by other failures. Often develops against the background of diseases such as diabetes, gout, leukemia | |
| By etiology | Autoimmune | The appearance is due to malfunctions of the immune system. |
| Toxic-allergic | Provoked by prolonged exposure to irritants, chemicals | |
| Idiopathic | The etiology of acute interstitial nephritis has not been established | |
| Post-infectious | Occurs as a complication of a previous illness | |
| According to clinical manifestations | Expanded form | Accompanied by pronounced symptoms |
| Heavy | Acute tubulointerstitial nephritis is characterized by prolonged anuria and renal failure. If hemodialysis is not performed, the patient may die | |
| Abortive | Symptoms subside. The disease does not threaten human life | |
| Focal | The signs are mild. Oliguria is present. The patient is recovering quickly. |
Causes of interstitial nephritis
Interstitial nephritis is a nonspecific inflammatory disease of the connective tissue of the kidneys, in which the inflammatory process (generalized or local) secondarily involves other structures of the kidney - tubules, vessels, and subsequently the glomeruli.
Interstitial nephritis often has a transient course and is primarily caused by damage to tubulointerstitial tissue due to its hypoxia and edema. However, in some cases, the disease takes a protracted course, the mass of functional tubules decreases, foci of sclerosis and necrosis appear, and chronic renal failure develops. Over the past decades, there has been a tendency towards an increase in the frequency of this disease among the adult population, which is associated not only with improved methods for diagnosing interstitial nephritis, but also with the expansion of the influence of disease-causing factors on the kidneys (in particular drugs). Interstitial nephritis is the cause of 20-40% of all cases of chronic renal failure and 10-25% of acute renal failure. The development of the disease is not related to gender and age. In Ukraine, the prevalence of interstitial nephritis is 0.7 per 100 thousand population.
There are acute and chronic interstitial nephritis. Acute, in turn, is divided into post-infectious, toxic-allergic and idiopathic. Typically, acute interstitial nephritis is the leading cause of “unknown renal failure” when urine output is maintained and the kidneys are of normal size.
The causes of interstitial nephritis are quite varied. Primary interstitial nephritis (nephritis that occurs in the intact kidney) can develop after the use of antibiotics, which cause damage to both the proximal and distal tubules. If it is caused by analgesics or non-steroidal anti-inflammatory drugs, then the distal tubules are more affected. Sulfonamide drugs, infectious diseases, and immunological disorders cause diffuse damage to the medulla and papillae.
With secondary interstitial nephritis, inflammatory changes in the interstitial tissue develop against the background of previous kidney diseases, their causes are:
- myeloma nephropathy,
- amyloidosis,
- sickle cell anemia,
- gout, diabetes insipidus,
- transplanted kidney.
Chronic interstitial nephritis can be a consequence of untreated or undiagnosed acute interstitial nephritis, but more often develops without previous acute interstitial nephritis. In such cases, the reasons for its occurrence may be:
- drug, household and industrial intoxication,
- radiation impacts,
- metabolic disorders,
- infections,
- immune changes in the body, etc.
At the same time, the leading role in the occurrence of chronic interstitial nephritis belongs to the long-term use (abuse) of drugs, among which the first place in importance is occupied by analgesics (phenacetin, analgin, butadione, etc.), and in recent years - NSAIDs (indomethacin, methindole, voltaren, acetylsalicylic acid, brufen, etc.). The presence of a causal relationship between the occurrence of chronic interstitial nephritis and the abuse of phenacetin is now considered a generally accepted fact.
Depending on the predominant localization of the pathological process, kidney function also changes. If the proximal tubules are damaged, aminaciduria, glucosuria, microglobulinuria, bicarbonaturia are observed, and proximal tubular acidosis may develop. If the distal tubules are predominantly affected, renal acidosis may also occur due to decreased sodium reabsorption and secretion.
If the entire medulla and papillae are affected, the ability of the kidney to concentrate urine is impaired, and this leads to the development of “renal” diabetes insipidus with severe polyuria and nocturia. However, isolated damage to the proximal and distal tubules of the medulla and papillae is rarely observed and therefore clinical manifestations are often mixed. The main pathogenetic mechanisms for the development of interstitial nephritis are as follows:
- immunocomplex - deposition of immune complexes in the basement membrane of the tubules;
- autoimmune - formation of antibodies to the tubular basement membrane;
- cytotoxic damage to this membrane, tubular epithelium and blood vessels with the development of irreversible ischemic damage to the medulla;
- damage caused by cellular immune reactions.
Often in the development of interstitial nephritis, depending on the nature of the process (acute or chronic), these mechanisms are combined. The pathogenesis of acute interstitial nephritis can be represented as follows:
- a foreign substance (antibiotic, chemical agent, bacterial toxin, pathological proteins formed during fever, as well as serum and vaccine proteins), penetrating into the bloodstream, enters the kidneys, where it passes through the glomerular filter and enters the lumen of the tubule;
- here reabsorption and damage to the basal membranes occurs, destruction of their protein structures;
- due to the interaction of foreign substances with protein particles of basement membranes, complete antigens are formed;
- they are also formed in the interstitial tissue under the influence of the same substances penetrating into it through the walls of the renal tubules;
- subsequently, immune reactions of interaction of antigens with antibodies occur with the participation of immunoglobulins and complement with the formation of immune complexes and their deposition on the basement membranes of the tubules and in the interstitium;
- an inflammatory process and histomorphological changes develop in the renal tissue, characteristic of acute interstitial nephritis;
- a reflex spasm of blood vessels occurs, as well as their compression due to the development of inflammatory edema of the interstitial tissue, accompanied by a decrease in renal blood flow and ischemia of the kidneys, including in the cortical layer, which is one of the reasons for the decrease in glomerular filtration rate and, as a consequence, an increase in the level of blood urea and creatinine;
- swelling of the interstitial tissue is accompanied by an increase in intrarenal pressure, including intratubular pressure, which adversely affects the process of glomerular filtration and is one of the most important reasons for the decrease in its rate.
However, structural changes in the glomerular capillaries themselves are usually not detected. Damage to the tubules, especially the distal parts, including the tubular epithelium, with simultaneous swelling of the interstitium leads to a significant decrease in the reabsorption of water and osmotically active substances and is accompanied by the development of polyuria and hyposthenuria. In addition, prolonged compression of the peritubular capillaries aggravates disturbances of tubular functions, contributing to the development of tubular acidosis, decreased protein reabsorption and the appearance of proteinuria. Violation of tubular functions occurs in the first days from the onset of the disease and persists for 2-3 months or more.
The pathogenesis of chronic interstitial nephritis has features depending on the cause of the disease. Thus, some drugs (salicylates, caffeine, etc.) directly damage tubular epithelial cells, leading to dystrophic changes in them with subsequent rejection. There is no convincing evidence of a direct nephrotoxic effect of phenacetin on the tubular structures of the kidneys. There is an opinion that in the pathogenesis of phenacetin nephritis, the damaging effect on renal tissue is not of phenacetin itself, but of its intermediate metabolic products - paracetamol and P-phenetidine, as well as hemoglobin degradation products.
With prolonged action of analgesics and NSAIDs on renal tissue, profound shifts in enzyme activity occur, which lead to metabolic disorders and hypoxia in the interstitial tissue and sustainable changes in the structure and function of the tubular apparatus of the kidneys.
In addition, analgesics can cause necrotic changes in the renal medulla, primarily in the area of the renal papillae. In the origin of chronic interstitial nephritis, the state of reactivity of the body and its sensitivity to drugs are also essential. The possibility of autoimmune genesis of chronic interstitial nephritis cannot be ruled out due to the formed complex “drug + kidney tissue protein,” which has antigenic properties.
The main changes in nephritis are observed in the interstitial tissue. Characteristic is the alternation of affected areas, often radially located, with areas of unchanged parenchyma with a clearly visible border. Changes in the tubules and rarely in the glomeruli are found only in areas where there is infiltration and sclerosis of the interstitial tissue. The nature of these elements depends on the etiology of the disease (polynuclear cells, lymphocytes, histiocytes, fibroblasts). Tubular degeneration of the renal glomeruli develops, as well as large vessels at all stages of development of acute interstitial nephritis remain intact and only in the case of a severe inflammatory process can they experience compression due to pronounced swelling of the surrounding tissues.
With a favorable course of acute interstitial nephritis, the described pathological changes in the renal tissue begin to reverse, usually within 3-4 months. In the chronic course of chronic interstitial nephritis, as the disease progresses, a gradual decrease in the size and weight of the kidneys is observed (often up to 50-70 g). Their surface becomes uneven, but without pronounced tuberosity. The fibrous capsule is difficult to separate from the renal tissue due to the formation of adhesions and adhesions. On the section, thinning of the cortical layer, pallor and atrophy of the papillae, and the phenomenon of papillary necrosis are noted. Microscopically, the earliest histomorphological changes are found in the inner layer of the medulla and papilla. The renal vessels usually do not experience significant changes or are completely intact. However, in vessels located in areas of renal tissue that have been fibrously changed, hyperplasia of the middle and inner membranes is found, and sometimes hyalinosis is found in arterioles. This leads to the development of arteriolosclerosis, which largely affects medium-sized arterioles, an acute inflammatory process leads to melting of the papillae, and the presence of obstruction leads to their smoothing. In the presence of chronic interstitial, especially toxic nephritis, it can develop into necrosis of the papillae.
Taking into account the peculiarities of the clinical picture of the disease during its course, the following variants (forms) of acute interstitial nephritis are distinguished:
- an expanded form, which is characterized by the main clinical symptoms and laboratory signs of this disease;
- a variant of acute interstitial nephritis, proceeds according to the type of “banal” renal failure with prolonged anuria and increasing hyperazotemia, with the phasic development of the pathological process characteristic of acute renal failure and a very severe course, requiring the use of program hemodialysis;
- “abortive” form with the absence of anuria phase, early development of polyuria, slight and short-term hyperazotemia, favorable course and rapid (within 1-1.5 months) restoration of renal concentration function;
- “focal” form, in which the clinical symptoms of acute interstitial nephritis are mild, erased, changes in urine are minimal and inconsistent, hyperazotemia is either absent or insignificant and passes quickly; characteristic acute occurrence of polyuria with hyposthenuria, rapid restoration of renal concentration function and disappearance of pathological changes in the urine;
- acute interstitial nephritis due to another renal disease.
Symptoms
TIN does not always begin acutely. The pathology is insidious and can proceed hidden for a long time until it becomes chronic. Interstitial nephritis is accompanied by the following symptoms:
- malaise;
- drowsiness;
- loss of appetite;
- pale skin;
- a sharp increase in body temperature;
- fever;
- chills;
- decreased volume of urine excreted;
- cephalalgia (headache);
- pre-fainting states;
- discomfort in the lower back;
- increased sweating;
- muscle aches;
- arterial hypertension.
Clinical manifestations of interstitial inflammation include eosinophilia, fever, and skin rash. Fever is detected in almost all patients, rash in half of patients. It occurs on the trunk and proximal limbs. The symptom is accompanied by itching.
Kinds
Nephritis is divided into two main types - according to the clinical picture and the mechanism of development.
Main classification:
- Expanded form (it identifies all the specific symptoms and test indicators characteristic of interstitial nephritis).
- Renal failure with prolonged urinary retention and impaired nitrogen function of the kidneys. The pathological process develops in phases, has a severe course and requires the patient to be connected to hemodialysis.
- In the abortive form, urinary retention is not observed, and the nitrogen excretion function is slightly impaired. Such interstitial nephritis is characterized by a favorable course with restoration of kidney functionality.
- Focal inflammation manifests itself in the form of mild symptoms. An increased content of metabolic products with impaired nitrogen excretion function is practically not observed. In other cases it may be insignificant. Focal lesions are characterized by increased urine production, which ends quickly. Kidney functions are gradually restored. This type of jade is the most favorable for the patient.
According to the development mechanism:
- damage associated with an immune reaction;
- autoimmune disorders or the introduction of external foreign microorganisms.
By type of occurrence:
- primary (development begins in a healthy organ);
- secondary (occurs after various diseases of the excretory system and kidneys).
Features of the course in children
Pathology is often diagnosed in children. It often develops in infants. The disease primarily affects premature infants. The main cause of TIN symptoms is exposure to toxic substances in the body. It happens that pathology develops after taking medications or vaccination.
Interstitial inflammation is accompanied by edema, urination disorders, and malaise. The levels of urea and creatinine in the blood increase. Almost always TIN is detected in the acute period. The transition to a chronic form is a rare phenomenon and is caused by inappropriate therapy.
Treatment of the disease
Treatment of interstitial nephritis must begin after the cause of its development in the human body has been established.
Considering the fact that the disease most often develops while taking certain synthetic medications, in this case the only method of treatment is to identify and stop taking the drug that triggered the development of the disease. If there is no effect within 3 days, it is indicated to take glucocorticosteroids.
It is important to provide the patient with the most optimal hydration regimen. If the amount of urine he excretes increases, then the volume of fluid he receives intravenously or consumes independently also increases accordingly. If the volume of urine decreases, the amount of fluid administered also decreases.
If a patient develops acute renal failure, hemodialysis must be performed urgently.
During treatment, it is important that the patient receives sufficient amounts of vitamins, proteins and carbohydrates, so doctors prescribe him a special diet.
Complications
Tubulointerstitial nephritis can be successfully treated. The main thing is to go to a medical facility in time and start therapy. Ignoring the manifestations of the disease and refusing to use medications can lead to the development of a chronic form. Changes in the functioning of structures are accompanied by a decrease in the number of nephrons and the development of renal failure. Tubulointerstitial nephritis, along with serious disruptions in the urinary system, leads to disability. People with complications require replacement treatment.
Due to the activation of the renin-angiotensin-aldosterone system (against the background of inflammation), arterial hypertension develops. When the synthesis of erythropoietin is impaired (if tubulointerstitial nephritis occurs in a chronic manner), severe anemia develops.
Types of disease
The classification of the disease is based on the course of the pathological process in the body. Experts distinguish two forms of interstitial nephritis - acute and chronic. In the first case, it is very easy to diagnose the problem, since the symptoms of the disease are clearly expressed, and an inflammatory process is observed in the body.
Signs of interstitial nephritis on a histological specimen
The chronic type of this disease is primarily due to an incompletely cured acute process. In this case, the patient may experience progression of kidney fibrosis and damage to the glomeruli with further tubular atrophy.
But it has long been known that inflammation of the renal glomeruli leads to the fact that the paired organ is not able to perform its key task - to cleanse the blood of waste products. “Thanks to” this, toxins and waste accumulate in the kidneys, poisoning the body.
Chronic interstitial nephritis (with further development) causes a decrease in the number of renal elements, which then leads to a deterioration in their functioning. If you are negligent in your health, the latent form of the disease can develop into nephrosclerosis and kidney failure. Most often, children are susceptible to this type of disease.
If treated promptly, the development of kidney failure can be avoided.
Diagnostics
If tubulointerstitial nephritis is suspected, in addition to examination, questioning, and analysis of the patient’s complaints, the following is prescribed:
- Biochemical blood test - to study urea and creatinine levels.
- Biochemistry of urine. An informative technique allows you to detect proteinuria and microhematuria.
- Complete blood count - to determine the concentration of red blood cells and leukocytes.
- Rehberg tests - to assess glomerular filtration rate.
- Research according to Zimnitsky - to study the ability of the kidneys to concentrate urine.
- Urine culture - to identify pathogenic microflora.
If there is a suspicion of acute tubulointerstitial nephritis, ultrasound is prescribed. The size of the kidneys increases slightly, and cortical echogenicity increases. In chronic disease, the organ, on the contrary, is reduced.
Renal biopsy is indicated for acute tubulointerstitial nephritis. Examination of a piece of tissue makes it possible to detect swelling of the interstitium.
Differential diagnosis is carried out in order to distinguish glomerulonephritis, pyelonephritis, urolithiasis from chronic or acute tubulointerstitial nephritis.
Features of prevention
In order to maintain kidney health after treatment, it is necessary to follow preventive measures:
- To drink a lot of water.
- Do not abuse medications, including painkillers.
- There are foods with B vitamins.
- Limit salt in your diet.
- Have your urine tested regularly.
- Treat foci of chronic infections.
- Avoid hypothermia.
- Dose physical activity.
The interstitial form of nephritis requires immediate contact with a specialist and initiation of treatment. The patient will temporarily lose his ability to work (for 3-4 months), but in the future this will allow him to recover and fully recover.
In order not to provoke complications of the disease in the future, it is very important to contact your doctor in a timely manner. For example, the following recommendations can provide good prevention:
- Drink the optimal amount of liquid.
- Take medications strictly as prescribed.
- Consult a doctor for any form of kidney ailment.
- Maintain only a healthy lifestyle.
- To undergo medical examinations in a timely manner for chronic or acute cases from 2 to 5 times a year based on the established diagnosis.
- Dress warmly.
It is important to know that the chronic form of this disease, due to the absence of clear symptoms, is always the most difficult to treat. Therefore, to prevent this from happening, it is important to undergo a full rehabilitation course when an acute form is detected. However, this does not mean that there are no restrictions after treatment. They exist, this means moderate physical activity and work only in environmentally friendly conditions.
If this form of the disease has been recorded in a child, then in order to avoid an allergic reaction, such children are not allowed to be vaccinated for 12-24 months. What parents are required to notify the class teacher or kindergarten teacher about.
Related publications
Treatment
Tubulointerstitial nephritis is a dangerous pathology that requires competent therapy. Treatment consists of eliminating provoking factors and normalizing kidney function. Treatment regimen for interstitial inflammation:
- Elimination of causes leading to the development of the disease or its transition to a chronic form.
- Discontinuation of medications that provoked the onset of symptoms.
- Maintaining a physiologically complete diet (in the absence of symptoms). It provides the patient with proteins, carbohydrates and fats, and enriches the body with vitamins and minerals.
- Limiting salt (especially if you have problems with blood pressure).
- Symptomatic therapy includes taking Enalapril. The drug helps to reduce the concentration of proteinuria and restore renal circulation.
- Use of steroids (if tubulointerstitial nephritis occurs with complications).
- The use of drugs to improve microcirculation (Curantil, Troxevasin).
- The use of Asparkam is a drug that prevents the leaching of Ca and K from the blood, as well as the occurrence of seizures.
If tubulointerstitial nephritis is complicated by renal failure, Prednisolone is prescribed. For renal dysfunction, treatment with Methylprednisolone is indicated. When the disease is accompanied by an increase in creatinine concentration, oligoanuria, hemodialysis is used.
Tubulointerstitial nephritis can be treated with alternative medicine, but only after consultation with the doctor. Herbal compositions ensure stabilization of the balance of lymph formation and drainage. In addition to pharmaceutical drugs, the use of infusions of mint and lingonberry is recommended. A decoction of oats and also primrose helps with pathology. You need to take natural medicine for 15 days, then take a break for 2 weeks. The general course is six months.
The infusions are prepared simply. Take 20 g of raw materials and 500 ml of boiling water. Place the container in a warm place for an hour. Take 100 ml three times a day. To make a decoction, the raw material is boiled for 15 minutes and only then infused.
Diet
Symptoms in the chronic form of interstitial nephritis, as a rule, are not always present. Therefore, during periods of remission, patients with this diagnosis are prescribed a nutritious diet with optimal consumption of proteins, fats, vitamins and energy value.
Where the use of a normal amount of table salt is not prohibited, unless in case of high blood pressure, swelling from salt, one should generally avoid it.
Here, if necessary, especially when symptoms of a chronic disease appear. It is recommended to establish oxalate-calcium metabolism. For example, a diet based on cabbage and potatoes may be suitable.
You should use foods with allergens with caution. This also includes products that, when consumed, can provoke irritation of the tubular apparatus of the kidneys. Therefore, smoked, spicy seasonings, and citrus fruits must be abandoned.
If the doctor has noted a decrease in the consumption of protein foods, then replenish the protein reserves in the body, possibly with the help of a plant-dairy diet. But the amount of liquid consumed should be at least 2000 ml. In case of acute interstitial nephritis, it will also be useful to arrange fasting diets. Based on pumpkin or apple days.
Diet
Proper nutrition during interstitial inflammation helps normalize kidney function. Principles of a therapeutic diet:
- Compliance with the drinking regime (2 liters of water per day, no less).
- Reducing salt.
- Refusal to eat fatty, fried, smoked foods.
- Exclusion of citrus fruits and spices.
It is recommended to enrich the diet with vegetarian soups, lean veal, and beef. Patients need to eat more:
- dairy products;
- potatoes;
- cabbage;
- vegetable salads.
If you are ill, you should avoid eating mushrooms, fish, canned meat, caviar, cheeses, legumes, and chocolate.
Prevention
Like any other disease, interstitial nephritis is easier to prevent than to cure.
Experts recommend adhering to the following rules:
- Do not take serious medications (such as antibiotics) without consulting your doctor. The same applies to diuretics;
- try to eat right. Avoid eating fatty and fried foods;
- if you have a genetic predisposition to the disease or suffer from other kidney diseases, it is recommended to test your urine for each disease;
- For normal kidney function, it is very important to adhere to the drinking regime. Drink 1.5 to 2 liters of water daily. You can determine the required volume of liquid using the following form: 30 ml of water for every 10 kg of weight;
- If possible, try to avoid taking antibiotics and pain medications;
- The functioning of the kidneys is closely related to the functioning of the entire genitourinary system. Therefore, you should not expose your body to additional risk in the form of hypothermia. It has been proven that one of the complications that arose against the background of untreated cystitis is precisely the development of such an ailment as nephritis;
- try to avoid stress and increased fatigue.
Peculiarities
A fairly common disease, characterized by an acute or chronic infectious-inflammatory process.
Despite the similarity of the disease with pyelonephritis, there are significant differences between these diseases. So, with interstitial nephritis, the kidney tissue is not destroyed. The inflammatory process affects only the connective tissues of the organ. They form a kind of kidney frame and do not extend to the cups and pelvis.
This disease can affect people of all ages. The disease can also be diagnosed in young children. Although the highest incidence rate is among the working population aged 25-52 years.